Operatieve behandeling
Uitgangsvraag
Wat is de aanbevolen operatieve behandeling bij patiënten met chronische posttraumatische anterieure schouderinstabiliteit?
De uitgangsvraag omvat de volgende deelvragen:
- Wat is de aanbevolen operatieve behandeling voor patiënten met schouder instabiliteit met 2 of meer luxaties: wekedelen procedure of ossale procedure?
- Wat is de aanbevolen operatieve procedure (open of arthroscopisch) bij patiënten met chronische posttraumatische anterieure instabiliteit en een indicatie voor operatieve behandeling?
- Wat is de aanbevolen operatieve behandeling voor patiënten met schouder instabiliteit na eerder operatief ingrijpen: wekedelen procedure of ossale procedure?
Aanbeveling
Wekedelen of ossale procedure
Overweeg bij jongere patiënten met chronische posttraumatische anterieure instabiliteit (2 of meer luxaties), waarbij er geen sprake is van botverlies aan humerale of glenoïd zijde een wekedelen procedure te verrichten.
Indien er tevens sprake is van een geïsoleerde Hill Sachs laesie, kan nog een remplissage aan de ingreep worden toegevoegd.
Overweeg een ossale procedure te verrichten bij:
- jongere patiënten die aan contactsport doen, 2 of meer luxaties hebben gehad en botverlies van het glenoïd hebben;
- twijfel over de mate en relevantie van botverlies aan glenoïd.
Arthroscopische of open benadering
Kies, als er een indicatie gesteld is voor een Bankart procedure, tussen een arthroscopische of open benadering op basis van opleiding en ervaring van de operateur. Er lijkt een kleinere recidiefkans te zijn bij een open Bankart procedure.
Kies, als er een indicatie gesteld is voor een Latarjet procedure, tussen een open of arthroscopische benadering op basis van opleiding en ervaring van de operateur.
Na eerder ingrijpen
Overweeg bij patiënten met een recidief schouderluxatie na eerdere geïsoleerde Bankart procedure en aanwezigheid van een Hill Sachs laesie, zonder botverlies aan de glenoïd zijde, een recidief weke delen procedure met daarbij een remplissage danwel een ossale procedure te verrichten.
Verricht bij overige patiënten met een recidief schouderluxatie na eerdere wekedelen procedure(s), met of zonder Hill Sachs laesie maar met (twijfel over) botverlies van glenoïd, bij voorkeur een ossale procedure.
Overwegingen
Balans tussen gewenste en ongewenste effecten en kwaliteit van bewijs
Bij een operatieve behandeling van chronische posttraumatische anterieure schouderinstabiliteit zijn er meerdere keuzes die moeten worden gemaakt, waaronder de keuze tussen een wekedelen of een ossale procedure en de keuze tussen een open of arthroscopische benadering. Deze keuzes kunnen verschillen per patiëntengroep, waaronder patiënten die een eerdere ingreep hebben ondergaan. Er werd literatuuronderzoek verricht naar chirurgische behandeling van chronische posttraumatische anterieure schouderinstabiliteit met als doel antwoord te kunnen geven op een aantal vragen.
1. Wat is de aanbevolen operatieve behandeling voor patiënten met schouder instabiliteit met 2 of meer luxaties: wekedelen procedure of ossale procedure?
Met het literatuuronderzoek werden vier prospectieve studies geïncludeerd die de vergelijking maakten tussen twee procedures: een wekedelen procedure (arthroscopische Bankart procedure) en een ossale procedure (open stabilisatie volgens Bristow en/of Latarjet) bij patiënten met schouderinstabiliteit na 2 of meer luxaties. Voor de cruciale uitkomstmaten reluxatie en complicaties was de bewijskracht laag. De gevonden studies suggereren dat een wekedelen procedure niet tot nauwelijks effect heeft op reluxatiekans. De multicenter RCT van Kukkonen (2021) laat weliswaar meer reluxaties zien in de patiënten die een arthroscopische Bankart procedure ondergingen t.o.v. patiënten behandeld met een ossale procedure. Echter werden in Kukkonen (2021) uitsluitend jongvolwassen mannen waren geïncludeerd (16-25 jaar). Ook werd er in de geïncludeerde studies een laag complicatierisico gerapporteerd voor beide ingrepen, zowel bij patiënten die een wekedelen procedure ondergingen, als patiënten die behandeld werden met een ossale procedure werden geen complicaties gevonden. Samengevat lijkt het risico op reluxatie en complicaties vergelijkbaar voor beide ingrepen.
De belangrijke uitkomstmaat aanhoudende vrees werd alleen gerapporteerd in de RCT van Kukkonen (2021). Deze studie laat zien dat meer patiënten aanhoudende vrees ervaarden na een arthroscopische Bankart, dan na een open Latarjet. De bewijskracht voor dit gevonden effect is laag. De belangrijke uitkomstmaten aanhoudende instabiliteit en subluxatie werden alleen gerapporteerd in de studie van Russo (2017). In deze studie werden beide uitkomstmaten slechts gerapporteerd voor de totale studiepopulatie, waardoor er geen conclusies getrokken konden worden over de effecten op aanhoudende instabiliteit en subluxatie na een wekedelen procedure of ossale procedure.
2. Wat is de aanbevolen chirurgische procedure (open of arthroscopisch) bij patiënten met traumatische anterieure instabiliteit en een indicatie voor operatieve behandeling?
Met het literatuuronderzoek werd onderscheid gemaakt tussen een open- of arthroscopische wekedelen procedure, en een open- of arthroscopische ossale procedure.
Voor de wekedelen ingrepen (Bankart procedure), die in Nederland doorgaans arthroscopisch worden uitgevoerd, werd met het literatuuronderzoek een systematische review gevonden, met daarin vijf gerandomiseerde trials, en één aanvullende gerandomiseerde studie werden gevonden. Deze onderzoeken suggereren dat een artroscopisch procedure een groter risico geeft op reluxatie dan een open procedure. De arthroscopische Bankart procedure geeft daarentegen mogelijk wel een lager risico op complicaties, daarnaast laat het gevonden bewijs een kortere operatieduur zien voor een arthroscopische Bankart procedure.
Hoewel het risico op een recidief lager blijkt bij een open Bankart procedure, dient de kanttekening te worden geplaatst dat de meerderheid van de geïncludeerde studies van oudere datum is. Arthroscopische technieken zijn de afgelopen jaren verbeterd, waarmee het aannemelijk is dat de resultaten van de ingreep ook zijn verbeterd.
Voor de ossale (Latarjet) procedure werden geen gerandomiseerde studies gevonden, enkel observationeel onderzoek. Dit onderzoek heeft van nature een lage bewijskracht. Omdat er geen sprake is van randomisatie, is het niet gegarandeerd dat de karakteristieken van de patiënten die een artroscopische Latarjet ondergingen vergelijkbaar zijn met de karakteristieken van de patiënten die een open Latarjet ondergingen. In de geïncludeerde studies hing de keuze voor het type ingreep veelal af van de keuze van de operateur, of was de tijdsperiode waar de ingreep werd uitgevoerd een bepalende factor. Voor de uitkomsten reluxatie, complicaties en operatieduur, werden gepoolde effecten gevonden die mogelijk in het voordeel zijn van de arthroscopische ossale procedure. De betrouwbaarheidsintervallen van de gepoolde effecten zijn echter zo breed, dat we onzeker zijn over het daadwerkelijke effect. Dit kan zowel in het voordeel van een arthroscopische ossale procedure liggen, als in het voordeel van een open ossale procedure, of er kan sprake zijn van geen verschil.
Het feit dat er naar de ossale ingrepen geen gerandomiseerde studies zijn gedaan, kan mogelijk worden verklaard door het feit dat dit type ingreep pas de laatste jaren steeds meer aandacht heeft gekregen. Met name de arthroscopische Latarjet is een relatief nieuwe techniek met een forse leercurve. Doorgaans duurt het arthroscopisch uitvoeren van een Latarjet procedure dan ook langer dan een open Latarjet. Dit sluit aan bij de resultaten uit de geïncludeerde studies.
3. Wat zijn de (on)gunstige effecten van een wekedelen procedure vergeleken met een ossale procedure voor patiënten met schouder instabiliteit en een recidief na eerder operatief ingrijpen?
Met het literatuuronderzoek werden twee onderzoeken geïncludeerd die een wekedelen procedure vergeleken met een ossale procedure, nadat een eerdere operatieve procedure om schouderinstabiliteit te herstellen, gefaald heeft. De twee studies die werden gevonden hebben een retrospectief karakter. Dit type onderzoek kenmerkt heeft een lage bewijskracht, waardoor er veel onzekerheid bestaat over de gevonden effecten of de vooraf gedefinieerde uitkomstmaten. In beide studies werden de drie uitkomstmaten reluxatie, subluxatie en persisterende instabiliteit, gezamenlijk gerapporteerd, waardoor er geen conclusie kon worden getrokken over het risico op één van deze individuele uitkomsten. Waar Calvo (2021) nauwelijks tot geen verschil in risico op reluxatie/subluxatie/persisterende stabiliteit suggereert, suggereert Elamo (2020) een mogelijk verhoogd risico op het optreden van deze uitkomsten na een wekedelen procedure. Ook voor de belangrijke uitkomstmaat complicaties werden tegenstrijdige resultaten gevonden. Vanwege deze tegenstrijdigheid (inconsistentie), is het op basis van deze gevonden resultaten onduidelijk wat het daadwerkelijke effect is van een wekedelen procedure of ossale procedure op de gedefinieerde uitkomsten. Bovendien was het bewijs afkomstig uit observationele onderzoeken met een (zeer) lage bewijskracht. Voor de uitkomstmaat aanhoudende angst voor luxatie werd geen bewijs gevonden.
Keuze van behandeling
Grofweg zou men kunnen zeggen dat er vier scenario’s zijn voor patiënten met chronische posttraumatische anterieure schouderinstabiliteit:
- Er is alleen sprake van schade aan de wekedelen (labrum, kapsel).
- Er is schade aan de wekedelen en bot verlies aan glenoïd zijde.
- Er is schade aan de wekedelen en bot verlies aan humerale zijde (Hill-Sachs laesie).
- Er is schade aan de wekedelen en zowel bot verlies aan glenoïd als humerale zijde (bipolair botverlies).
In de ideale wereld zou er voor ieder scenario een ‘custom-made’ chirurgische oplossing zijn, dit blijkt in praktijk helaas lastig.
Bij het maken van de behandelkeuze zijn verschillende factoren waar rekening mee moet worden gehouden, waaronder:
- Het risico op reluxatie en recidief instabiliteit.
- Het risico op complicaties.
- Mate van glenoïd botverlies.
- Aanwezigheid van Hill-Sachs laesie.
Risico op reluxatie en recidief instabiliteit
Ongeacht de mate van weke delen en ossale schade, is het aannemelijk dat een ossale procedure een kleinere kans op reluxatie en recidief instabiliteit kent dan een wekedelen procedure. Dit wordt ondersteund door de meta-analyse van Imam (2021), waarin de gerandomiseerde studie van Zarezade (2014) was geïncludeerd, naast zes observationele onderzoeken. Een meta-analyse van deze trials (n = 3275 patiënten), suggereert een hogere kans op recidief luxatie na de Bankart procedure wanneer vergeleken met stabilisatie volgens Latarjet (RR: 2.74, 95% BI 1,48 tot 5,06). Eenzelfde conclusie wordt getrokken in de meest recente meta-analyse van Hoseinzadeh (2024) op basis van 21 studies waarvan 3 RCT’s. De auteurs achten de kans op een recidief instabiliteit na een Bankart procedure tot 3.08 keer groter in vergelijking met een ingreep volgens Latarjet. Met toename van lengte van follow-up, tussen de 5 en 10 jaar postoperatief, lijkt het voordeel van de Latarjet procedure op dit vlak toe te nemen. Kanttekening bij deze studie echter is dat de mate van glenoïd bot verlies niet specifiek benoemd wordt. De resultaten van beide systematische reviews moeten met zorg worden geïnterpreteerd, aangezien deze voor het grootste deel afkomstig zijn van observationele studies. De mogelijke lagere kans op reluxatie en recidief instabiliteit maakt dat een ossale procedure de voorkeur heeft bij patiënten met een eerder gefaalde (wekedelen)procedure.
Deze resultaten ten faveure van ossale procedures willen echter niet zeggen dat iedere patiënt met symptomatische, recidiverende schouder luxaties (na een eerder gefaalde procedure) een ossale procedure moet ondergaan. In de behandelbeslissing moeten verschillende factoren worden meegenomen waaronder de wens van de patiënt, mogelijk oorzaak van falen (technische fouten, hypermobiliteit), het risico op complicaties en de mate botverlies.
Risico op complicaties
Een reden om géén ossale procedure uit te voeren kunnen liggen in de hogere kans op peri- en postoperatieve complicaties. De studies geïncludeerd in de literatuursamenvatting suggereren een laag complicatie risico na beide ingrepen. Desalniettemin acht de werkgroep het aannemelijk, mede ondersteund door systematische literatuur reviews en meta-analyses van observationele onderzoeken, dat met name de kans op postoperatieve neuropraxie, implantaat gerelateerde complicaties en haematoomvorming groter zijn na een (arthroscopische) bot blok procedure (Williams, 2018; Hoseinzadeh, 2024). Daarnaast kunnen ook bot resorptie op langere termijn en pseudo-artrose een punt van zorg zijn (Rutgers 2023). Systematische literatuur onderzoeken waarin alleen complicaties na arthroscopische wekedelen procedures (193 observationele onderzoeken, n = 14019 Bankart ingrepen; Rodriguez, 2023) of de Latarjet procedures (35 observationele onderzoeken, n = 2560 Latarjet ingrepen; Choo 2023) worden beschreven, laten zien dat het risico op complicaties na Latarjet 16.1%, is, en 0.7% na een wekedelen procedure. Er moet terughoudendheid zijn met het vergelijken van deze cijfers, aangezien hier een indirecte vergelijking wordt gemaakt. Het is bijvoorbeeld onduidelijk of de patiënten in beide studies vergelijkbaar waren.
Mate van botverlies
Een andere reden om niet te kiezen voor een ossale procedure is dat er niet bij alle patiënten sprake hoeft te zijn van botverlies, zowel aan glenoïd als humerale zijde. De literatuur laat veel ruimte voor discussie met betrekking tot (1) de optimale manier van het berekenen van bot verlies aan glenoïd zijde (Gowd, 2018; Weil, 2022) en (2) welk percentage van botverlies het kritieke omslagpunt zou moeten vormen om te besluiten tot het verrichten van een ossale procedure (Cognetti, 2024; Hoyt, 2024). Aan humerale zijde wordt het belang van bot verlies vaak beschreven volgens het vrij complexe ‘on-track / off-track’ principe om het belang van de Hill-Sachs laesie met het oog op recidief instabiliteit te duiden (Di Giacomo, 2014). Zie ook de module Meetmethoden Glenoïdaal botverlies.
Het blijkt dus lastig om een exacte maat van botverlies aan glenoïd zijde te benoemen als omslagpunt voor de keuze voor een ossale procedure. Daarom werd verder gekeken naar specifieke risicofactoren die de kans op een recidief na een (arthroscopische) wekedelen procedure vergroten en dus bij kunnen dragen in de besluitvorming. Een klinische preoperatieve score die hierin kan helpen is de Instability Severity Index Score (ISIS; Balg, 2007). Hoe hoger deze score, hoe hoger de kans op recidief instabiliteit na een wekedelen procedure. In een systematisch review naar risicofactoren geassocieerd met een verhoogde recidiefkans (29 observationele studies geïncludeerd, n = 4582 schouders) kwam een ISIS score van >3 tevens naar voren als risico factor. Andere factoren die hierin geïdentificeerd werden als negatieve risico factor waren: leeftijd jonger dan 20 jaar, deelname aan competitieve sport, aanwezigheid van een Hill-Sachs laesie, aanwezigheid van glenoïd botverlies, aanwezigheid van een ALPSA-laesie (anterior labrum periosteal sleeve avulsion), meer dan 1 luxatie preoperatief, en tot slot meer dan 6 maanden tussen luxatie en operatie (Verweij 2021). Dit sluit aan bij de resultaten die gevonden werden in de RCT van Kukkonen (2021), waarin in een populatie van mannelijke jongvolwassenen (16 - 25 jaar) een hogere recidief kans gevonden werd dan in de andere trials.
Aanwezigheid Hills-Sachs Laesie
Tot slot nog een nuance met betrekking tot de aanwezigheid van een Hill-Sachs laesie; het toevoegen van een Hill-Sachs remplissage (capsulomyodese van de infraspinatus) aan een Bankart procedure laat vaak goede resultaten met lage recidief kans zien postoperatief (Locher 2016; Hurley,2020). Dit geldt ook voor patiënten waarbij een eerdere (wekedelen) procedure is gefaald. In een meta-analyse naar het verschil tussen Bankart repair + remplissage (BRR) en Latarjet, waarin één prospectief observationeel onderzoek en drie retrospectieve onderzoeken zijn geïncludeerd (totaal 379 patiënten), wordt een vergelijkbaar recidief percentage gezien (RR = 0.72; 95% CI: 0.37 tot 1.41) en vergelijkbare PROM’s uitkomsten (Haroun, 2020). Echter werd er ook een lagere complicatie risico gerapporteerd voor de BRR groep (RR, 7.37; 95% CI: 2 tot 27 en RR voor re-interventie: RR= 0.79; 95% CI: 0.1 tot 3.47). Er is beperkt bewijs om dit te ondersteunen bij een eerder gefaalde wekedelen procedure (Sinha 2021). In het geval van bipolair botverlies is er nog discussie welke maat van botverlies aan glenoïd zijde te accepteren is om deze ingreep uit te voeren, net als in het geval van unipolair botverlies aan glenoïd zijde.
Aangezien de arthroscopische Bankart procedure momenteel de gouden standaard is, zou het interessant kunnen zijn om een open Bankart procedure te vergelijken met een open danwel arthroscopische Latarjet procedure. Onderzoeken waarin deze vergelijking werd gemaakt, werden echter niet gevonden.
Kwaliteit van bewijs
De overall bewijskracht voor de eerste deelvragen was laag (GRADE low).
Er is afgewaardeerd vanwege ernstige
- Risk of Bias: methodologische beperkingen, waaronder gebrek aan blindering of onduidelijkheid van randomisatie.
- Imprecisie: onnauwkeurigheid, omdat het betrouwbaarheidsinterval een of meerdere grenzen van klinische relevantie overschrijdt.
Voor de analyse bij patiënten met eerder operatief ingrijpen was de overall bewijskracht zeer laag (GRADE very low). Dit betekent dat we zeer onzeker zijn over het gevonden geschatte effect van de cruciale uitkomstmaten.
Er is afgewaardeerd vanwege zeer ernstige:
- Risk of bias: methodologische beperkingen. Bewijs afkomstig uit retrospectief onderzoek, waarin niet gecorrigeerd werd voor confounders. Ook was de keuze voor de manier van ingrijpen niet (adequaat) gerapporteerd.
- Inconsistentie: tegenstrijdige resultaten.
Omdat de literatuur onvoldoende richting kan geven aan de besluitvorming omtrent chirurgisch ingrijpen bij schouderinstabiliteit, zijn de aanbevelingen gebaseerd op aanvullende argumenten waaronder expert opinie, waar mogelijk aangevuld met (indirecte) literatuur. Dit betreft zowel de keuze voor een wekedelen of ossale behandeling, als de keuze voor arthroscopisch of open ingrijpen en de behandelkeuze voor patiënten waarbij eerdere behandeling faalde.
Waarden en voorkeuren van patiënten (en eventueel hun naasten/verzorgers)
De patiënt is gebaat bij een ingreep met weinig risico’s en een grote kans op herstel. Over het algemeen wordt een arthroscopische Bankart procedure als een ingreep met een relatief laag risico beschouwd. Wel gaat dit mogelijk gepaard met een hogere kans op een secundaire revisie/ingreep op later tijdstip, gezien een mogelijk grotere recidief kans op instabiliteit in vergelijking met een ossale procedure. Ook suggereert de RCT van Kukkonen (2021) een hoger risico op ‘aanhoudende vrees’ na een arthroscopische Bankart procedure, wat nadelig kan zijn voor de patiënt. Gemiddeld genomen mag worden aangenomen dat de hersteltijd na een operatie vergelijkbaar zal zijn. Het is van belang om bovenstaande factoren vooraf met de patiënt te bespreken, bijvoorbeeld in de vorm van samen beslissen of een informed consent.
Kostenaspecten
De kosten van de primaire interventies, weke delen en ossale, mogen als vergelijkbaar beschouwd worden. Implantaatkosten zullen weinig verschillen, daarnaast zijn allebei in dagbehandeling uit te voeren. De Bankart procedure (met remplissage) duurt mogelijk langer om uit te voeren, het valt te beargumenteren dat dit hogere kosten met zich meebrengt (bijv. personele kosten). Daarnaast is de duur van een arthroscopische Bankart procedure mogelijk korter dan een open Bankart procedure wat een gunstig effect op de kosten zou kunnen hebben. Voor de Latarjet procedure geldt dat een arthroscopische Latarjet procedure doorgaans langer duurt dan een open Latarjet procedure en een leercurve heeft, wat redenen kunnen zijn om te kiezen voor een open Latarjet.
Deze argumenten spelen geen rol bij de behandelkeuze voor een individuele patiënt. Het spreekt voor zich de dat kosten per individuele patiënt op kunnen lopen indien er een revisie operatie uitgevoerd dient te worden. Er zijn kosten-effectiviteitsanalyses gepubliceerd uit verschillende zorg systemen met tegengestelde uitkomsten, hierbij dient de kanttekening te worden gemaakt dat de groepen patiënten die vergeleken zijn niet exact hetzelfde zijn (Min, 2018; Pugliese, 2023).
Gelijkheid ((health) equity/equitable)
De interventie leidt niet tot een toe- of afname van gezondheidsgelijkheid.
Aanvaardbaarheid
Ethische aanvaardbaarheid
De interventie lijkt aanvaardbaar voor de betrokkenen. Er zijn geen ethische bezwaren.
Duurzaamheid
Bij de interventie spelen duurzaamheidsaspecten niet direct een rol.
Haalbaarheid
De interventies zijn over het algemeen al standaardzorg in de praktijk. Hierbij lijkt de arthroscopische Bankart procedure, zeker in Nederland, nog altijd als het meest te worden toegepast. Mogelijk zou op basis van bekende literatuur en bovenstaande uiteenzetting een ossale procedure vaker de voorkeur kunnen genieten. Specifiek in het geval van twijfel over de mate van botverlies aan glenoïd zijde.
De doorslaggevende factor in de keuze voor een open- of arthroscopische procedure zijn ervaring en opleiding van operateur. In Nederland worden Bankart ingrepen doorgaans arthroscopisch uitgevoerd en de Latarjet procedures meestal open. Gezien de uitkomsten van een open Bankart procedure en arthroscopische Latarjet, lijken beiden ingrepen zowel arthroscopisch als open te kunnen worden uitgevoerd. Voor de Latarjet procedure geldt overigens wel dat een arthroscopische benadering langer duurt dan een open benadering, dit kan een reden zij om te kiezen voor een open Latarjet. Ook de leercurve t.a.v. het uitvoeren van een arthroscopische Latarjet speelt hierbij een rol.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
Wekedelen of ossale procedure
Er zijn aanwijzingen dat de kans op recidief anterieure instabiliteit of luxatie en aanhoudende vrees over het algemeen kleiner is na een ossale procedure dan na een wekedelen procedure. In de literatuur is niet duidelijk welke hoeveelheid botverlies aan glenoïd zijde het kritieke omslagpunt vormt, noch is er consensus over de meetmethode, om richting te geven om een wekedelen of ossale procedure te verrichten. Bij twijfel over de mate van botverlies aan glenoïd zijde, heeft behandeling middels Latarjet de voorkeur. De Instability Severity Index Score is een klinische score die kan helpen in de besluitvorming, aangezien een hogere ISIS geassocieerd is met een verhoogde recidief kans na een wekedelen procedure. Andere risicofactoren die helpend kunnen zijn in de behandelbeslissing zijn leeftijd van de patiënt, deelname aan competitieve sport, aanwezigheid Hill-sachs laesie, aanwezigheid glenoïd botverlies, aanwezigheid ALPSA-laesie, meer dan 1 luxatie preoperatief, > 6 maanden tussen luxatie en operatie.
Arthroscopische of open benadering
De kans op reluxatie is mogelijk kleiner na een open Bankart procedure in vergelijking met een arthroscopische Bankart procedure. Echter lijkt de complicatie kans hoger en de operatietijd langer na een open Bankart procedure. Daarnaast biedt de arthroscopische procedure de mogelijkheid om een remplissage toe te voegen wat een gunstig effect kan hebben op het verlagen van de recidief kans in vergelijking met een geïsoleerde Bankart procedure. De uitkomsten na een open versus arthroscopische Latarjet procedure zijn vergelijkbaar behoudens langere operatietijd en leercurve van de arthroscopische benadering.
Na eerder ingrijpen
De overweging tussen een wekedelen procedure versus ossale procedure is in de situatie van een eerder gefaalde wekedelen procedure vergelijkbaar met die van een recidiverende anterieure instabiliteit. Gezien er sprake is van een eerder gefaalde weke delen interventie zou in de meeste gevallen een ossale procedure de voorkeur hebben.
Eindoordeel:
Zwakke aanbeveling voor een wekedele procedure en ossale procedure bij patiënten met chronische posttraumatische anterieure schouderinstabiliteit.
Onderbouwing
Achtergrond
In the literature, multiple surgical techniques have been described to treat patients with habitual shoulder instability. These can roughly be divided into procedures that involve the repair of soft tissues (labrum, capsule) and procedures that also involve an osseous procedure to increase the surface of the glenoid (fixing a bone block to the front of the glenoid). Both types of procedures have advantages and disadvantages, and there is still much debate about which type of procedure is best for which patient. Generally, it is assumed that there is a higher risk of recurrent instability after a soft tissue procedure compared to an osseous procedure. However, it is assumed that the osseous procedure carries a higher risk of complications, and not every patient requires such an extensive procedure to adequately stabilize the shoulder. It is unclear if these assumptions are true. Factors such as the number of previous dislocations and the presence of bone loss from the glenoid and/or humerus play an important role in the treatment decision. Both types of procedures have been described as either arthroscopic or open surgeries. The arthroscopic Bankart procedure, an anterior soft tissue reconstruction of the capsuloligamentous structures of the shoulder, is considered the most performed surgical treatment for this patient group. At the same time, good outcomes have also been reported in the past with open Bankart repair. However, there is increasing evidence that a osseous procedure, in which the coracoid process is osteotomized and fixed to the anterior glenoid rim (Latarjet procedure), may lead to lower recurrence rates of instability but potentially more complications. In recent years, this procedure has also been increasingly performed arthroscopically. It is questioned whether an arthroscopic approach or open surgery results in better outcomes for patients with anterior shoulder instability.
Conclusies / Summary of Findings
Summary of findings
Click here to see these tables in a document
Question 1. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with shoulder instability who suffered 2 or more dislocations and/or with less than 25% bone loss?
|
Outcome
|
Study results and measurements |
Absolute effect estimates |
Certainty of the Evidence (Quality of evidence) |
Conclusions |
|
|
Osseous procedure |
Soft tissue procedure |
||||
|
(re)dislocation (critical)
|
Risk difference: 0.04 (95%-BI -0.09 — 0.17) Based on data from 222 patients in 3 studies
|
27 per 1000* |
98 per 1000 |
Low Due to very serious risk of bias1
|
Soft tissue procedure may result in little to no difference in (re)dislocation when compared with osseous procedure in patients with shoulder instability with two or more luxations with <25% bone loss.
Source: Zarezade (2014), Kukkonen (2021), and Abouelsoud (2015) |
|
Difference: 71 more per 1000
|
|||||
|
Complications (critical)
|
Risk difference 0.00 (95%-CI -0.03 — 0.03) Based on data from 262 patients in 4 studies |
0 per 1000* |
0 per 1000 |
Low Due to very serious risk of bias1
|
Soft tissue procedure may result in little to no difference in complications when compared with osseous procedure in patients with shoulder instability with two or more luxations with <25% bone loss.
Source: Zarezade (2014), Kukkonen (2021), Russo (2016), and Abouelsoud (2015 |
|
Difference: -
|
|||||
|
Persistent apprehension (important) |
Relative Risk 2.18 (95%-CI 0.96 — 4.91) Based op data van 121 patients in 1 study |
119 per 1000* |
259 per 1000 |
Low Due to serious risk of bias, due to serious imprecision2 |
Soft tissue procedure may result in an increase in persistent apprehension when compared with bony procedure in patients with shoulder instability with two or more luxations with <25% bone loss.
Source: Kukkonen (2021) |
|
Difference: 140 morer per 1000 (95% CI 5 lower – 465 more)
|
|||||
|
Subluxation (important)
|
Based on data from 40 patients in 1 study |
Persistent instability was only reported in one study (Russo, 2017). The outcome was only reported for the total study population, not per treatment arm. It was reported that: “three months post-operatively, one patient had a shoulder subluxation” |
No GRADE |
It was not possible to draw conclusions or grade the level of evidence, due to the absence of comparative data.
Source: - |
|
|
Persistent instability (important) |
Based on data from 40 patients in 1 study |
Persistent instability was only reported in one study (Russo, 2017). The outcome was only reported for the total study population, not per treatment arm. It was reported that: “Shoulder stiffness occurred in one female patients with restoration of ROM after 14 months, and in one patient a posterior instability was reported at two years of follow-up. |
No GRADE |
It was not possible to draw conclusions or grade the level of evidence, due to the absence of comparative data.
Source: - |
|
1. Risk of Bias: very serious. Due to uncertainty whether randomization was performed.
2. Risk of Bias: serious. Due to lack of blinding
Imprecision: serious. Due to overlap of the upper limit of the 95% confidence interval with the minimal clinically important difference.
Question 2a. and 2b.
What are the (un)beneficial effects of an arthroscopic soft tissue (Bankart) procedure, compared with an open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid)?
|
Outcome
|
Study results and measurements |
Absolute effect estimates |
Certainty of the evidence (Quality of evidence) |
Summary |
|
|
Open Bankart |
Arthroscopic Bankart |
||||
|
Redislocation
|
Relative risk: 1.83 (CI 95% 1.16 - 2.89) Based on data from 750 participants in 6 studies
|
67 per 1000 |
123 per 1000 |
Low Due to serious risk of bias, due to serious imprecision1 |
Arthroscopic Bankart repair might increase the risk of redislocation when compared with open Bankart repair in patients with shoulder instability. |
|
Difference: 56 more per 1000 (CI 95% 11 more - 127 more) |
|||||
|
Complications
|
Relative risk: 0.7 (CI 95% 0.27 - 1.8) Based on data from 364 participants in 1 studies
|
55 per 1000 |
38 per 1000 |
Very low Due to serious risk of bias, due to very serious imprecision2 |
The evidence is very uncertain about the effect of arthroscopic Bankart repair on complications, when compared with open Bankart Repair in patients with shoulder instability. |
|
Difference: 17 fewer per 1000 (CI 95% 40 fewer - 44 more) |
|||||
|
Subluxation |
Based on data of 0 participants in 0 studies |
- |
No GRADE (no evidence was found) |
No evidence was found regarding the effect of postoperative functional activity when compared with postoperative immobilization in patients with shoulder instability that was operatively treated. |
|
|
Surgical duration
|
Based on data from 592 participants in 3 studies
|
Difference: MD 41.90 lower (CI 95% 64.24 lower - 19.57 lower) |
Low Due to serious risk of bias, due to serious imprecision3 |
Arthroscopic Bankart repair might reduce the surgical duration when compared with open Bankart repair in patients with shoulder instability.
|
|
|
Persisting apprehension |
Based on data of 0 participants in 0 studies |
- |
No GRADE (no evidence was found) |
No evidence was found regarding the effect of postoperative functional activity when compared with postoperative immobilization in patients with shoulder instability that was operatively treated. |
|
|
2b. What are the (un)beneficial effects of an arthroscopic osseous (Bristow-Latarjet) procedure compared with an open osseous (Bristow-Latarjet) procedure in patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid)? |
|||||
|
Redislocation
|
Relative risk: 0.78 (CI 95% 0.23 - 2.62) Based on data from 716 participants in 9 studies
|
16 per 1000 |
12 per 1000 |
Very Low Due to serious risk of bias, due to very serious imprecision4
|
The evidence is very uncertain about the effect of arthroscopic open Coracoid transfer surgery on redislocation when compared with open coracoid transfer surgery in patients with shoulder instability. |
|
Difference: 4 fewer per 1000 (CI 95% 12 fewer - 26 more) |
|||||
|
Complicaties post-operative
|
Relative risk: 0.81 (CI 95% 0.47 - 1.41) Based on data from 1100 participants in 10 studies
|
95 per 1000 |
77 per 1000 |
Very Low Due to serious risk of bias, due to very serious imprecision4
|
The evidence is very uncertain about the effect of arthroscopic open Coracoid transfer surgery on surgical duration when compared with open coracoid transfer surgery in patients with shoulder instability. |
|
Difference: 18 fewer per 1000 (CI 95% 50 fewer - 39 more) |
|||||
|
(Re)dislocation and subluxation (postoperative instability)
|
Relative risk: 0.71 (95% CI 0.33 to 1.52) Based on data from 1322 participants in 13 studies |
25 per 1000 |
18 per 1000 |
Very Low Due to serious risk of bias, due to very serious imprecision4
|
The evidence is very uncertain about the effect of arthroscopic open Coracoid transfer surgery on surgical duration when compared with open coracoid transfer surgery in patients with shoulder instability.. |
|
Difference:7 fewer per 1000 (CI 95% 17 fewer – 13 more) |
|||||
|
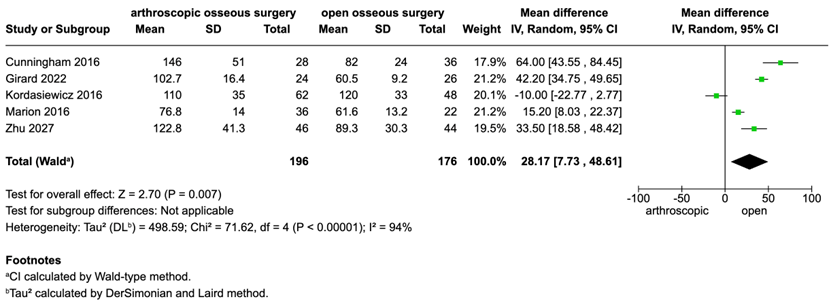
Surgical duration
|
Based on data from 372 participants in 5 studies
|
|
|
Very Low Due to serious risk of bias, due to very serious imprecision4
|
The evidence is very uncertain about the effect of arthroscopic open Coracoid transfer surgery on surgical duration when compared with open coracoid transfer surgery in patients with shoulder instability. |
|
Difference: MD 28.17 lower (CI 95% 7.73 lower - 48.61 higher) |
|||||
|
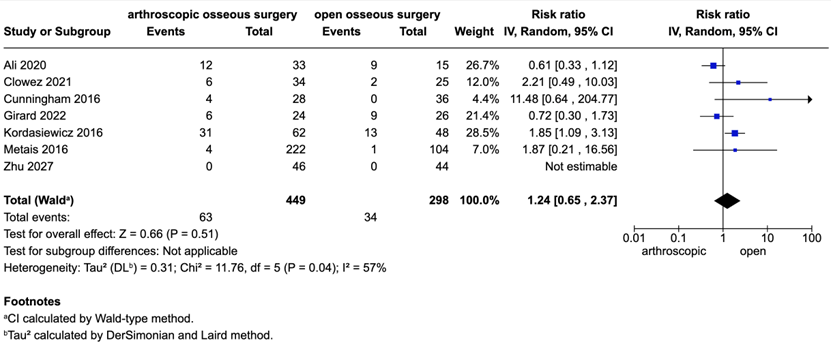
Persisting apprehension
|
Relative risk: 1.24 (CI 95% 0.65 - 2.37) Based on data from 747 participants in 7 studies
|
114 per 1000 |
141 per 1000 |
Very Low Due to serious risk of bias, due to very serious imprecision4
|
The evidence is very uncertain about the effect of arthroscopic open Coracoid transfer surgery on surgical duration when compared with open coracoid transfer surgery in patients with shoulder instability. |
|
Difference: 27 more per 1000 (CI 95% 40 fewer - 156 more) |
|||||
1. Risk of bias: serious. Lack of blinding. Imprecision: serious. overlap of the lower limit of the 95% confidence interval with the minimal clinically important difference.
2. Risk of bias: serious. Lack of blinding. Imprecision: serious. overlap of the both limits of the 95% confidence interval with the minimal clinically important difference.
3. Risk of bias: serious. Lack of blinding. Imprecision: serious. overlap of the upper limit of the 95% confidence interval with the minimal clinically important difference.
4. Risk of Bias: serious. Due to lack of correction for confounding factors (not clear if intervention and control group were comparable). Imprecision: very serious. Due to overlap of both limits of the 95% confidence interval with the minimal clinically important difference
Question 3. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with recurrent shoulder instability after previous surgery with <15 % bone loss?
|
Outcome
|
Study results and measurements |
Absolute effect estimates |
Certainty of the Evidence (Quality of evidence) |
Conclusions |
|
|
Osseous procedure |
Soft tissue procedure |
||||
|
Redislocation (critical)
persistent instability, subluxation (Important) |
RD: -0.06 (95% CI -0.27, 0.15). RD: 0.28 (95% CI 0.14 to 0.42). Based on data from 114 patients in 2 studies (not pooled) |
Calvo (2021): 179 per 1000
Elamo (2020): 0 per 1000
|
Calvo (2021): 118 per 1000
Elamo (2020): 283 per 1000
|
Very Low Due to serious risk of bias, Due to inconsistency1 |
The evidence is very uncertain about the effect of soft tissue procedure on redislocation, persistent instability and subluxation, when compared with osseous procedure in patients with recurrent shoulder instability after previous operative treatment with <15% bone loss.
Source: Calvo (2021), Elamo (2020) |
|
|
|||||
|
Complications (critical)
|
RR: 0.00 RR: 1.58 (95% CI 0.73, 3.42)
Based on data from 114 patients in 2 studies (not pooled) |
Calvo (2021): 0 per 1000
Elamo (2020): 261 per 1000
|
Calvo (2021): 0 per 1000
Elamo (2020): 413 per 1000
|
Very Low Due to serious risk of bias, Due to inconsistency1 |
The evidence is very uncertain about the effect of soft tissue procedures on complications when compared with osseous procedure in patients with recurrent shoulder instability after previous operative treatment with <15% bone loss.
Source: Calvo (2021), Elamo (2020) |
|
|
|||||
|
Persistent apprehension (important) |
No evidence |
- |
No GRADE |
No evidence was found regarding the effect of soft tissue procedure one persistent apprehension when compared with osseous procedure in patients with recurrent shoulder instability after previous operative treatment with <15% bone loss.
Source: - |
|
1. Risk of Bias: serious. Due to concerns regarding the selection of participants and lack of correction for confounding factors
Inconsistency: serious. Due to conflicting results
(Results were retrieved from observational studies, start GRADE low)
Samenvatting literatuur
Description of studies
1. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with shoulder instability who suffered 2 or more dislocations and/or with less than 25% bone loss?
A total of four studies was included in the analysis of the literature. Important study characteristics and results are summarized in Table 5. The assessment of the risk of bias is summarized in the risk of bias tables (under the tab ‘Evidence tabellen’).
Abouelsoud (2015) performed a prospective comparative study to compare the clinical outcome and cost-effectiveness or arthroscopic remplissage and open Latarjet procedures in cases or recurrent shoulder dislocation with large Hill-Sachs Lesion. The study was executed in a hospital in Egypt. Patients who showed recurrent anterior glenohumeral instability (i.e., subluxation and dislocation defined by more than three episodes within a 12-month period of conservative treatment) and the Hill–Sachs size assessed on preoperative MRI was 20–30 % of the humeral head size were included.
Kukkonen (2021) performed a multi-centre RCT to compare the success rates of arthroscopic Bankart and Open Latarjet procedure in the treatment of traumatic shoulder instability in young males. The study was executed in 8 public hospitals in Finland. Young adult male patients (age 16-25 years), with involuntary redislocation, subluxation or fear of shoulder dislocation after a primarily conservatively treated traumatic anteroinferior shoulder dislocation were included.
Russo (2017) compared the results of two techniques treating chronic shoulder instability with moderate glenoid loss: bone-block according to open Latarjet Patte procedure, and arthroscopic Bankart repair in association with subcapsularis augmentation. The study was executed in a hospital I Italy Inclusion criteria were clinical history of traumatic or atraumatic anterior shoulder instability, glenoid bone loss from 5 to 23% as assessed by CT scan according to the ‘‘Pico area method’’, and humeral bone loss (Hill-Sachs) wider than one-third of the humeral head, participation in sports, capsulolabral insufficiency, failure of arthroscopic stabilization, or dislocation with glenoid fracture (bony Bankart).
Zarezade (2014) performed a RCT in which Bankart arthroscopic procedure was compared with Open Bristow Procedure. The study was executed in an Iranian hospital. Inclusion criteria were patients aged 18-45, suffering from recurrent dislocation of the shoulder due to trauma, dislocation not healing following non-surgical treatments.
|
Author, year
|
Participants |
Comparison |
Follow-up |
Outcome measures |
Comments |
Risk of bias* |
|
Abouelsoud (2015) |
The study was conducted on 32 shoulders (and 32 patients).
I: 16 patients C: 16 patients
Mean age of the total study population was 28.2 years. Gender: 29 males and 3 females
All patients had a history of recurrent anterior shoulder instability.
Six patients were involved in non-violent sports, two in violent sports, and the rest not involved in sports.
Number of dislocations (total patient population) Minimum number of dislocations: 3 Some patients, the number of dislocations was (so) numerous that it could not be counted.
|
Intervention: Arthroscopic remplissage procedure with capsulolabral repair using four anchors.
Postoperative rehabilitation protocol was the same for both groups
Control Modified Latarjet procedure [Coracoid transfer procedure (modified Latarjet with coracoid osteotomy just anterior to coracoclavicular ligaments attachment)].
Postoperative rehabilitation protocol was the same for both groups |
Mean follow-up period of 31.31 months (range: 24–40 months). |
Reluxation Not reported
Complications
|
Author’s conclusion: “Open modified Latarjet and arthroscopic remplissage procedure with Bankart repair are equally effective in prevention of dislocation in patients with recurrent anterior shoulder dislocation and engaging Hill–Sachs lesion” |
High It seems that no randomization was performed
|
|
Kukkonen (2021) |
122 young males with traumatic shoulder anteroinferior instability were randomised.
I: 62 patients C: 59 patients
Age (years) The average age of patients was 21 years (range 16-25 years).
All young male patients between 16 and 25 years old.
Mean age (SD) (range) I: 21.4 (2.7) (16-25) C: 21.4 (2.7) (16-25)
Hyperlaxity (n) I: 11 C: 8
Significant Hill-Sachs lesion in CT (n) I: 19 C: 18 |
Intervention Arthroscopic Bankart for the treatment of traumatic shoulder instability in young males
Control: Open Latarjet procedure in the treatment of traumatic shoulder instability in young males. |
3 months, 6 months, 1 and 2 years postoperatively.
|
Recurrence of instability (dislocation at two-years follow-up).
Clinical apprehension
|
Author’s conclusion: “Arthroscopic Bankart operation carries a significant risk for short- term postoperative redislocations compared with open Latarjet operation, in the treatment of traumatic anteroinferior instability in young males. Patients should be counselled accordingly before deciding the surgical treatment.”
Drop- out rate 25%. Reason not reported.
% bone loss not reported |
Some concerns
|
|
Russo (2017) |
Ninety-one patients with moderate anterior glenoid bone loss underwent from 2011 to 2015. From these patients, two groups of 20 individuals each have been selected.
I: 20 patients C: 20 patients
One patient in each group presented a failed arthroscopic Bankart repair.
Baseline characteristics for the total study population:
Mean age: 23.4 years
Right shoulder involved: 19/40 patients (47.5%)
Gender, males 28/40 patients (70%) |
Intervention Arthroscopic Bankart repair associated with subscapularis augmentation
Control Open Latarjet procedure
|
The mean follow-up in the open Latarjet procedure group was 21 months (20–39 months),
In the arthroscopic Bankart repair group, the mean follow-up was 20 months (15–36 months).
|
Complications Persistent instability subluxations |
Author’s conclusion: “Arthroscopic subscapularis augmentation of Bankart repair is an effective procedure for the treatment of recurrent anterior shoulder instability with glenoid bone loss without any significant difference in comparison with the well-known open Latarjet procedure.”
|
High It seems that no randomization was performed
|
|
Zarezade (2014) |
Patients over the age of 18 and less than 45 years suffering from recurrent anterior shoulder dislocation due to trauma
40 patients were selected and randomly divided into two groups of 20 patients.
I: 18 patients C: 19 patients
Age (years) The average age of patients was 29.6 ± 4.6 years (range: 23-40).
I: 28.6 ± 4.5 C: 30.4 ± 4.8
Frequency of dislocations (N, %)
Less than 5 times: 11 (29.7%) 5-9 times: 5 (13.5%) More than 10 times: 12 (32.4%) Unknown number: 9 (24.3%) |
Intervention Arthroscopic Bankart repair
Control Open Bristow procedure
|
Mean follow-up time in these patients was 7.5 years and none of the patients had relapse.
Time period of measured outcomes not specified (solely mentioned mean follow-up duration of 7.5 years).
|
Outcomes Dislocation after surgery, Complications
|
Author’s conclusion: “The two mentioned techniques did not differ significantly, although some parameters such as level of performance, pain intensity, use of analgesics, and range of internal rotation showed more improvement in Bristow procedure. Therefore, if there is no contraindication for Bristow procedure, it is preferred to use this method” % bone loss not reported
|
Some concerns |
*For further details, see risk of bias table in the appendix
2a. What are the (un)beneficial effects of an arthroscopic soft tissue (Bankart) procedure, compared with an open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid)?
A total of one systematic review and one additional primary study were included in the analysis of the literature. Important study characteristics and results are summarized in Table 6. The assessment of the risk of bias is summarized in the risk of bias tables (under the tab ‘Evidence tabellen’).
Khatri (2018) performed a systematic review and meta-analysis to compare the results of traditional open Bankart repair and arthroscopic Bankart repair in traumatic anterior shoulder instability. The databased Medline, PubMed, Embase and Cochrane Library were searched for relevant articles until December 2017. All randomized controlled trials, published in English, comparing the open Bankart repair with arthroscopic Bankart repair were included in the study. Cadaveric studies, biomechanical studies and studies that provided insufficient information on the population characteristics, surgical procedure or outcome were excluded. In total five randomized controlled trials were included: Sperber (2001), Fabbriciani (2004), Bottoni (2006), Netto (2012), Mohatadi (2014). Risk of bias was assessed with the PEDro scale.
Gupta (2024) performed a randomized controlled trial to compare the outcomes of open versus arthroscopic surgical management for recurrent anterior shoulder instability. The study was executed in a hospital in India. Patients were either randomized to open (n = 182) or arthroscopic (n = 182) Bankart repair surgery.
2b. What are the (un)beneficial effects of an arthroscopic osseous (Bristow-Latarjet) procedure compared with an open osseous (Bristow-Latarjet) procedure in patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid)?
A total of one systematic review, five additional primary studies were included in the analysis of the literature. Important study characteristics and results are summarized in Table 6. The assessment of the risk of bias is summarized in the risk of bias tables (under the tab ‘Evidence tabellen’).
Deng (2023) conducted a systematic review to evaluate the clinical efficacy, postoperative revisions, and complications between the open Latarjet (OL) and arthroscopic Latarjet (AL) procedures for treating recurrent anterior shoulder instability. The review involved searching the MEDLINE/PubMed, Cochrane Library, and Embase databases from their inception to July 2022 to identify relevant studies comparing the OL and AL procedures. The inclusion criteria encompassed RCTs, prospective cohort studies, retrospective cohort studies, and case-control studies published in English. A total of 11 studies were included: Ali (2020), Bonnevialle (2021), Cunningham (2016), Hurley (2021), Kordasiewicz (2018, 2017), Marion (2017), Metais (2016), Nourissat (2016), Russo (2017), and Zhu (2017). The risk of bias in these studies was assessed using the Newcastle-Ottawa Scale.
For the purposes of these guideline the risk of bias was assessed for individual studies. If specific risk of bias assessments were not available, the NOS scores were used as an alternative.
Nascimento (2024) performed a multicenter retrospective cohort study of medical records and imaging studies of two groups of patients, with two years of follow-up, who underwent one of two variations of the Latarjet procedure: open approach with screws (open-screw group) or arthroscopic approach with cortical buttons (scope-button group). Exclusion criteria included previous shoulder surgery, except for a previous failed Bankart repair. The choice between open or arthroscopic Latarjet was based on surgeon experience and institutional capabilities, though specific criteria for selecting one technique over the other were not detailed. Both techniques were applied based on patient medical indications, such as glenoid bone loss or recurrence after a previous surgery. Surgeries were performed by experienced shoulder surgeons at two institutions, following standardized preoperative, surgical, and rehabilitation protocols.
Girard (2022) conducted a retrospective comparative study of two consecutive patient groups who underwent either arthroscopic or open bone block procedures for anterior shoulder instability. Only primary shoulder stabilization cases were included, with all patients having a minimum clinical follow-up of 12 months. The study included patients treated for chronic anterior instability with either arthroscopic Latarjet using double cortical buttons (group A) or open Latarjet with screws (group O). From January 1, 2018, to June 30, 2018, all patients were treated exclusively with the arthroscopic procedure, while from July 1, 2018, to December 31, 2018, all patients underwent the open procedure. This change was motivated by findings from a previous study that reported an unexpectedly long time to achieve bone block fusion in the arthroscopic group, prompting a technical shift for evaluation.
Gaujac (2024) performed a single-centre study to assess bone block positioning during the arthroscopic Latarjet procedure, comparing two fixation techniques: anterior screw fixation and posterior glenoid-guided system with double cortical button fixation. The study included patients with recurrent anterior shoulder instability. Group A consisted of patients who underwent surgery from July 2014 to June 2017 using the anterior screw fixation, while Group B had surgery from July 2017 to September 2019 with posterior fixation. All surgeries were performed by a single surgeon.
Tanaka (2024) conducted a retrospective study evaluating the impact of arthroscopic confirmation of coracoid fixation on bone union rates and clinical outcomes in rugby players undergoing the Bristow procedure. From 2010 to July 2017, the open Bristow procedure with Bankart repair was performed, while from August 2017 onward, a mini-open AS-assisted Bristow procedure with arthroscopic Bankart repair was used.
Clowez (2024) conducted a retrospective single-center cohort study evaluating patients who experienced anterior instability recurrence after arthroscopic Bankart repair and subsequently underwent revision with either a Bristow or Latarjet coracoid bone-block procedure, performed either open or arthroscopically. The study included patients with at least one glenohumeral instability event or persistent anteroinferior apprehension preventing return to sports, with a minimum follow-up of 24 months.
|
Study |
Participants |
Comparison |
Follow-up |
Outcome measures |
Comments |
Risk of bias (per outcome measure)* |
|
Question 2a arthroscopic versus open soft tissue (Bankart) surgery |
||||||
|
Included in systematic review Khatri, 2018 |
||||||
|
Bottoni (2006) |
N at baseline Intervention: 32 Control: 29
Age (mean, SD not provided) Intervention: 25.2 Control: 25.1 |
Intervention: Arthroscopic Bankart
Control: Open Bankart |
Intervention: 28.5 months
Control: 30 months |
Shoulder stability (defined as no episode of dislocation; data retrieved from original paper)
Surgical duration |
No blinding of subjects and clinicians, no intention to treat analysis |
|
|
Fabbriciani (2004) |
N at baseline Intervention: 30 Control: 30
Age (mean, SD not provided) Intervention: 24.5 Control: 26.8 |
Intervention: Arthroscopic Bankart
Control: Open Bankart |
Intervention: 24 months
Control: 24 months |
None |
None of the predefined outcomes was reported |
|
|
Mohatadi (2014) |
N at baseline Intervention: 98 Control: 98
Age (mean, SD not provided)
Intervention: 27.8 Control: 27.2 |
Intervention: Arthroscopic Bankart
Control: Open Bankart |
Intervention: 24 months
Control: 24 months |
Shoulder stability (defined as no episode of dislocation data; retrieved from original paper)
Surgical duration |
|
No blinding of subjects and assessors |
|
Netto (2012) |
N at baseline Intervention: 17 Control: 25
Age (mean, SD not provided) Intervention: 27.8 Control: 27.2 |
Intervention: Arthroscopic Bankart
Control: Open Bankart |
Intervention: 37.5 months
Control: 37.5 months |
Shoulder stability (defined as no episode of dislocation; data retrieved from original paper))
|
|
No blinding of subjects, clinicians and assessors No intention to treat analysis.
It was stated that Netto (2012) reported surgical time as an outcome. However when considering the original paper, data on this outcome could not be identified. |
|
Sperber (2001) |
N at baseline Intervention: 30 Control: 26
Age (mean, SD not provided) Intervention: 25 Control: 27.5 |
Intervention: Arthroscopic Bankart
Control: Open Bankart |
Intervention: 24 months
Control: 24 months |
Shoulder stability (defined as no episode of dislocation; data retrieved from original paper))
|
|
No blinding of subjects, clinicians and assessors No intention to treat analysis |
|
Individual studies |
||||||
|
Gupta (2024) |
N at baseline Intervention: 182 Control: 182
Age (mean, SD) Intervention: 30.2, 7.9 Control: 29.5, 8.1
Sex (n female, %) Intervention: 54, 30% Control: 52, 29%
Previous dislocations (mean, SD) Intervention: 3.4, 1.3 Control: 3.5, 1.2 |
Intervention: Arthroscopic Bankart surgery (Group II)
Control: Open Bankart surgery (Group I) |
3-, 6- and 12-months follow-up |
Redislocation
Surgical duration
Intraoperative complications
|
It was stated that outcomes were assessed at 3-, 6- and 12-months follow-up. Only outcomes at 12 months follow-up were presented. |
Information on allocation and. randomization procedures was not available.
It was stated that surgeons were blinded
Probably selective outcome reporting. |
|
Question 2b. arthroscopic versus open osseous procedure |
||||||
|
Studies included in the systematic review Deng, 2024 |
||||||
|
Ali (2020) |
N at baseline-end Intervention: 37-33 Control: 25-15
Age (mean, SD) Intervention: 30 (7) Control: 28 (10)
|
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
24 months follow-up |
Apprehension, complications (post-operative), (re)dislocation
|
|
|
|
Bonnevialle (2021) |
N at baseline-end Intervention: 17-17 Control: 22-22
Age (mean, SD) Intervention: 22.3 (5.3) Control: 21.2 (4.8)
Sex (n male) Intervention: 14 Control: 21 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
2 weeks, 1.5 and every 3 months follow-up |
None |
None of the predefined outcomes was reported |
|
|
Cunningham (2016) |
N at baseline-end Intervention: 28-28 Control: 36-36
Age (mean, SD) Intervention: 26.0 (7.6) Control: 25.0 (9.2)
Sex (n male) Intervention: 24 Control: 34 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
7 months |
(re)dislocation and subluxation, post-operative complications, surgical duration, apprehension
|
|
|
|
Hurley1 (2021) |
N at baseline-end Intervention: 40-30 Control: 110-72
Age (mean, SD) Intervention: 32 (12.3) Control: 30 (10.0)
Sex (n male) Intervention: 25 Control: 32 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
12 months follow-up |
(re)dislocation and subluxation |
Dislocation and subluxations were defined as recurrent instability in the primary study
|
|
|
Hurley2 (2021) |
N at baseline-end Intervention: 40-40 Control: 110-110
Age (mean, SD) Intervention: 30.7 (11.5) Control: 28.4 (9.6)
Sex (n male, %) Intervention: 34 (85%) Control: 95 (86.4%) |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
3 months follow-up |
Post-operative complications
|
|
|
|
Kordasiewicz (2016) |
N at baseline-end Intervention: 66-62 Control: 55-48
Age (mean) Intervention: 26 Control: 28
Sex (n male) Intervention: 55 Control: 2 |
Intervention: arthroscopic Latarjet
Control: Open Latarjet
|
Only mean follow-up were presented
Intervention: 23.4 (mean)
Control: 54.2m (mean) |
(re)dislocation and subluxation, apprehension, surgical duration, complications
|
(re)dislocation and subluxation defined as recurrence in the primary study |
|
|
Marion (2016) |
N at baseline-end Intervention: 36-36 Control: 22-20
Age (mean, SD) Intervention: 27.3 (7.5) Control: 26.7 (7.8)
Sex (n male) Intervention: 29 Control: 16 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
24 months |
(re)dislocation and subluxation, post-operative complications, surgical duration
|
It was stated that there was a follow-up to 24 months. Only outcomes at 3-6 months follow-up were included in the meta-analysis.
|
|
|
Metais (2016) |
N at baseline-end Intervention: 222-77 Control: 104 -38 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
6, 12 months follow-up |
(re)dislocation and subluxation, post-operative complications, apprehension
|
It was stated that there was a follow-up 6, 12 months. Only outcomes at baseline were included in the meta-analysis. |
|
|
Nourissat (2016) |
N at baseline-end Intervention: 99-? Control: 85-?
|
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
1, 3, 6, 12 months follow-up |
None |
None of the predefined outcomes was reported |
|
|
Russo (2017) |
N at baseline-end Intervention: 21-21 Control: 25-21 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
12 months follow-up |
None |
None of the predefined outcomes was reported |
|
|
Zhu (2017) |
N at baseline-end Intervention: 46-? Control: 44-?
Age (mean, SD) Intervention: 32.1 (10.3) Control: 34.8 (11.5)
Sex (n male) Intervention: 26 Control: 32 |
Intervention: Arthroscopic Latarjet (AL group)
Control: Open latarjet (OL group) |
24 months follow-up |
(re)dislocation and subluxation, surgical duration, apprehension
|
|
|
|
Individual studies |
||||||
|
Nascimento (2024) |
N at baseline-end Intervention: 44-44 Control: 38-38
Age (mean, SD) Intervention: 32.5 (15.0) Control: 27.5 (12.0)
Sex (n male) Intervention: 38 Control: 36 |
Intervention: Arthroscopic Latarjet (scope-button group)
Control: Open latarjet (open-screw group) |
2 weeks, 3-, 6-, 12-, and 24-months follow-up |
Dislocation, subluxation
|
The open group included 2 patients (5.3%) with a previous Bankart repair, while the arthroscopic group included 13 patients (29.5%). |
|
|
Girard (2022) |
N at baseline-end Intervention: 24-24 Control: 26-26
Age (mean, SD) Intervention: 22.5 (6.8) Control: 25.5 (8.7)
Sex (n male) Intervention: 19 Control: 24 |
Intervention: Arthroscopic Latarjet (group A)
Control: Open Latarjet (group O) |
15, 45 days, 3, 6, 12 months follow-up |
Surgical duration, subluxation, dislocation, apprehension, Complications (intra-operative)
|
|
|
|
Gaujac (2024) |
N at baseline-end Intervention: 44-41 Control: 35-31
Age (mean, SD) Intervention: 27.8 (6.8) Control: 24.9 (7.2)
Sex (n female, %) Intervention: 41 Control: 31 |
Intervention: Arthroscopic Latarjet (group B)
Control: Open Latarjet (group A) |
24 months follow-up |
Complication (intra-operative, post-operative), dislocation or subluxation (recurrence) |
Recurrence of instability is defined by dislocation or subluxation. |
|
|
Tanaka (2024) |
N at baseline Intervention: 45 Control: 66
Age (mean, SD) Intervention: 17.4 Control: 18.4
Sex (n female, %) Intervention: 43 Control: 66 |
Intervention: Arthroscopy assisted (mini-open) Bristow procedure with ABR
Control: Open Bristow procedure with open Bankart repair |
24 months follow-up |
Dislocation I: 0 – C: 0 Subluxation: I: 1 – C: 2
Complications (post-operative I: 0 – C: 0 |
|
|
|
Clowez (2021) |
N at baseline Intervention: 34 Control: 25
Age (mean, SD) Total: 23 (5.9)
Sex (n female, %) Total: 8 |
Intervention: Arthroscopic procedure
Control: Open procedure |
24 months follow-up |
Apprehension I: 6 - C: 2 Subluxation I: 0 - C: 4 Dislocation I: 0 - C: 0 Complications (intra/post-operative) I: 0- C: 0 |
|
|
*For further details, see risk of bias table in the appendix
3. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with recurrent shoulder instability after previous surgery with <15 % bone loss?
A total of two studies were included in the analysis of the literature. Even though these studies did not match the inclusion criteria (wrong study design), the guideline development group considered these studies relevant for answering the research question. As a consequence, these studies were included in the summary of literature. Important study characteristics and results are summarized in Table 7. The assessment of the risk of bias is summarized in the risk of bias tables (under the tab ‘Evidence tabellen’).
Calvo (2021) performed a single centre retrospective study to evaluate results of revision surgery in patients with previous surgical stabilization failure and subcritical glenoid bone defects comparing repeated Bankart repair with Arthroscopic Latarjet Procedure. Bone defects were considered subcritical if they involved <15% of the articular glenoid surface.
Elamo (2020) retrospectively assessed and compared (patient-reported) outcomes and clinical results between arthroscopic revision Bankart surgery and open revision Latarjet operation, after failed arthroscopic primary Bankart repair stabilization.
|
Author, year
|
Participants |
Comparison |
Follow-up |
Outcome measures |
Comments |
Risk of bias* |
|
Calvo (2021) |
Total of 45 patients (mean age, 29.1 ± 8.9 years) with subcritical bone loss (<15% of articular surface) who had undergone revision anterior shoulder instability repair after failed Bankart repair.
Total participants: 45 patients Intervention: 17 Control: 28
Age (year) I: 29.6 ± 8.6 C: 28.7 ± 9.3 |
Intervention Revision surgery arthroscopic Bankart repair – after primary Bankart repair
Control Revision surgery arthroscopic Latarjet surgery – after primary Bankart repair |
Minimum of 2 years postoperatively |
Subluxation or redislocation (considered as recurrent instability),
complications
|
Author’s conclusion: “The most relevant finding of this study was that arthroscopic Latarjet did not obtain superior results compared with repeated arthroscopic Bankart repair in patients with recurrent anterior shoulder instability after Bankart repair and subcritical glenoid bone loss”
|
Some concerns, cases and controls not selected from same population;
“The revision technique was selected based on the practice of the senior surgeon, who chose the surgical technique according to current evidence in the literature . Therefore, before 2012 patients with recurrent postoperative instability were scheduled for revision Bankart repair if the bony Bankart lesion involved <15% of the glenoid articular surface and for Latarjet only if the defect was larger. After 2012, all patients (…) were scheduled for arthroscopic Latarjet regardless of the presence or absence of glenoid bone defect” |
|
Elamo (2020) |
Total number of 69 patients with revised primary Bankart procedures were identified.
N total at baseline: 69 Intervention: 46 Control: 23
Number of patients available for follow-up I: 30 C: 18
Agee at primary operation, yr I: 27.9 C: 26
Gender, male (n, %): I: 21 (81%) C: 13 (87%) |
Intervention Arthroscopic revision Bankart operation after failed arthroscopic primary Bankart stabilization
Control Open revision Latarjet operation after failed arthroscopic primary Bankart stabilization. |
Length of follow-up, yr.: I: 7.8 C: 3.5
Substantial loss-to follow-up (30 per cent drop out rate)
|
Recurrence of instability (requiring surgical intervention)
Persisting subluxation Persisting redislocation |
Author’s conclusion: “an open Latarjet procedure yield better results than an arthroscopic Bankart procedure in a revision setting after a failed primary arthroscopic Bankart procedure. The re-dislocation rate is high and patient-reported outcome measures are poor after an arthroscopic revision Bankart operation compared with an open revision Latarjet procedure”
The percentage of bone loss in the study population was not reported. |
Some concerns
Not clear how treatment decision was made. High loss to follow-up rate |
*For further details, see risk of bias table in the appendix
Results
1. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with shoulder instability who suffered 2 or more dislocations and/or with less than 25% bone loss?
(Re)dislocation
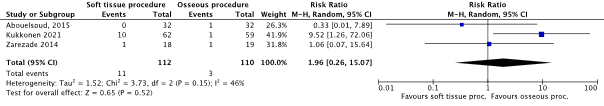
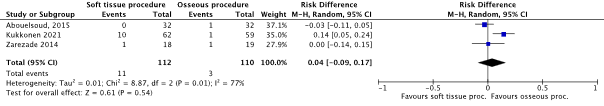
Three studies reported the outcome (re)dislocation after a soft tissue procedure or osseous procedure in patients with two or more dislocations (Abouelsoud, 2015; Kukkonen, 2021; Zarezade, 2014). The pooled number of patients experiencing (re)dislocation in the soft tissue procedure group was 11/112 (9.8%), compared to 3/110 (2.7%) of the patients undergoing osseous procedure. The pooled Risk Ratio was 1.96 (95% CI: 0.26 to 15.07), see Figure 1. The pooled Risk Difference was 0.04 (95% CI -0.09 to 0.17), see Figure 2.
Figure 1. Forest plot showing the effects of soft tissue procedure (Bankart repair) compared with osseous procedure (Latarjet or Bristow) on the outcome (re)dislocation
Pooled relative risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval
Figure 2. Forest plot showing the effects of soft tissue procedure (Bankart repair) compared with osseous procedure (Latarjet or Bristow) on the outcome (re)dislocation
Pooled Risk Difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval
Complications
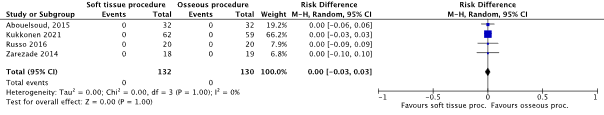
Four studies reported the outcome complications after a soft tissue procedure or osseous procedure in patients with two or more dislocations (Abouelsoud, 2015; Russo, 2016; Kukkonen, 2021; Zarezade, 2014). All studies reported that there were no (treatment-related) complications in either the soft tissue procedure group (0/132) or the osseous procedure group (0/130). See Figure 3.
Figure 3. Forest plot showing the effects of soft tissue procedure (Bankart repair) compared with osseous procedure (Latarjet or Bristow) on the outcome complications
Pooled Risk Difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval
Persistent instability
Russo (2016) reported on persistent instability for the total study population and stated ‘’Shoulder stiffness occurred in one female patient with restoration of ROM after 14 months, and in one patient a posterior instability was reported at two years of follow-up, but no further treatment was required.’’
Abouelsoud (2015), Kukkonen (2021) and Zarezade (2014), did not report on persistent instability.
Subluxation
Russo (2016) solely mentioned textually and for the total population of patients: ‘’ Three months postoperatively, one patient had a shoulder subluxation’’. As results were only available for the total study population, the GRADE approach could not be applied.
Abouelsoud (2015), Kukkonen (2021) and Zarezade (2014) did not report on subluxation.
Persistent apprehension
Kukkonen (2021) reported the outcome clinical apprehension. In the soft tissue procedure group (Bankart Repair), 16/62 patients (33%) had signs of clinical positive apprehension, compared to 7/59 patients (16%) undergoing osseous procedure (open Latarjet). The RR was 2.18 (95% CI 0.96 to 4.91).
Abouelsoud (2015), Russo (2016) and Zarezade (2016) did not report on persistent apprehension.
2a. What are the (un)beneficial effects of an arthroscopic soft tissue (Bankart) procedure, compared with an open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid)?
(Re)dislocation
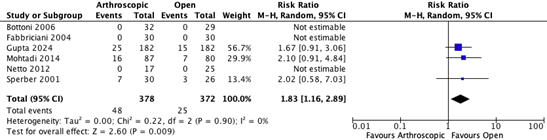
Five studies from the systematic review from Khatri (2018) and the RCT from Gupta (2024) reported the outcome redislocation (Bottoni, 2006; Fabbriciani, 2004; Gupta, 2024; Mohtadi, 2014; Netto, 2012; Sperber, 2001). The follow-up duration across these studies ranged from 3 to 37.5 months. In total 48/378 (12.7%) of the patients undergoing arthroscopic soft tissue surgery experienced redislocation, compared to 25/372 (6.6%) of the patients undergoing open soft tissue surgery. The pooled Risk Ratio (RR) was 1.83 (95% CI: 1.16 to 2.89), see Figure 4.
Figure 4. Forest plot showing the outcome redislocation for the comparison arthroscopic and open soft tissue surgery for shoulder instability
Risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Complications
Gupta (2024) reported intraoperative complications. Of the patients who underwent Arthroscopic Bankart surgery, 7/182 (3.8%) experienced intraoperative complications, compared to 10/182 (5.5%) patients of the open Bankart surgery group. The RR was 0.70 (95% CI: 0.27 to 1.80). It was not stated which intraoperative complications were observed.
Subluxation
None of the included studies reported the outcome subluxation after arthroscopic soft tissue (Bankart) surgery or open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability.
Surgical duration
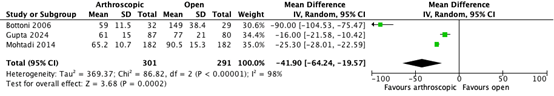
Two studies from the systematic review of Khatri (2018) and the RCT from Gupta (2024) reported the outcome ‘surgical duration’ (Bottoni, 2006; Mohtadi, 2014). The mean difference in surgical duration between the arthroscopic soft tissue surgery (n = 301) compared to the open soft tissue surgery (n = 291) is 41.90 minutes (95% CI -64.24 to – 19.57). See Figure 5.
Figure 5. Forest plot showing the outcome surgical duration for the comparison arthroscopic and open soft tissue surgery for shoulder instability
Risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Persisting apprehension.
None of the included studies reported the outcome persisting apprehension after arthroscopic soft tissue (Bankart) surgery or open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability.
2b. What are the (un)beneficial effects of an arthroscopic osseous (Bristow-Latarjet) procedure compared with an open osseous (Bristow-Latarjet) procedure in patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid)?
The predefined outcomes (re)dislocation and subluxation were reported as ‘postoperative instability’ in Deng (2024). Postoperative instability was defined as “all incidences of recurrent dislocations and subluxations.” Data from individual studies reporting on (re)dislocation and subluxation were combined and presented as the overall number of ‘postoperative instability’. ‘
Dislocation was specifically reported under the term ‘recurrence rate’, referring to the number of complete dislocations occurring after surgery. To maintain consistency, dislocation was categorized under ‘recurrence rate’ in the individual studies.
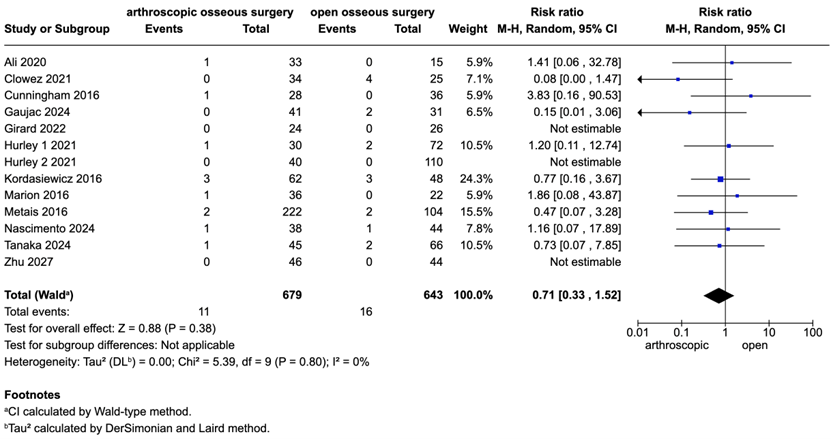
(Re)dislocation and subluxation (postoperative instability)
Eight studies from the systematic review of Deng (2024) reported postoperative instability at final follow-up (min. 3 months, max 24 months follow-up) in patients undergoing arthroscopic osseous surgery compared to open osseous surgery (Ali, 2020; Cunningham, 2016; Hurley, 2021; Kordasiewicz, 2017; Marion, 2016; Metais, 2016; Zhu, 2017). Additionally, five other studies (Gaujac, 2024; Girard, 2022; Nascimento, 2024; Tanaka, 2024; Clowez, 2021) provided data, which were pooled in a meta-analysis. Of the patients undergoing arthroscopic surgery 11/679 (1.6%) experienced postoperative instability compared to 16/643 (2.4%) of the patients undergoing open osseous surgery. The RR was 0.71 (95% CI 0.33 to 1.52), see Figure 6.
Figure 6. Forest plot showing the outcome postoperative instability for the comparison arthroscopic and open osseous surgery
Risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
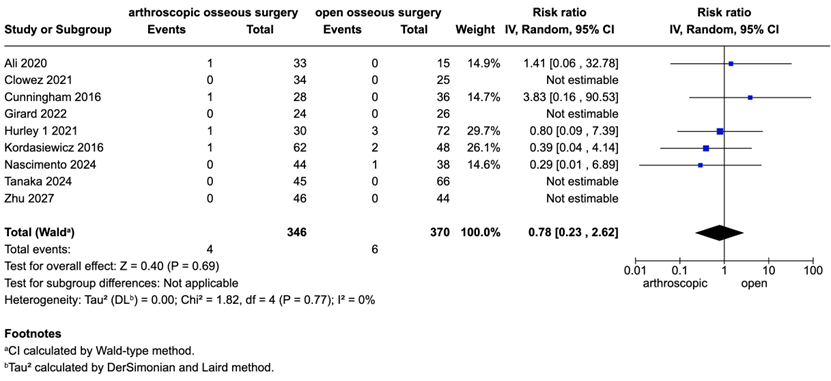
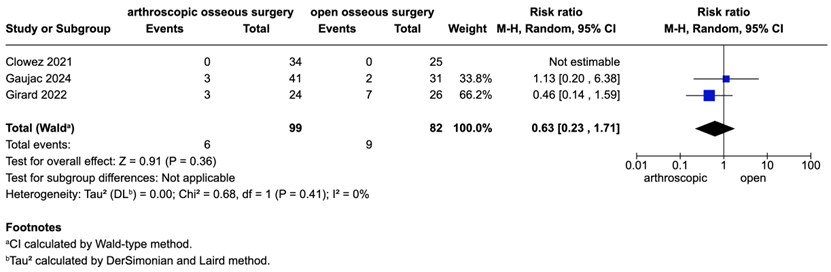
Redislocation (recurrence rate)
Five studies from the systematic review of Deng (2024) reported recurrence rates in patients undergoing arthroscopic surgery compared to open surgery (Ali, 2020; Cunningham, 2016; Hurley, 2021; Kordasiewicz, 2017; Zhu, 2017). Additionally, four other studies (Girard, 2022; Nascimento, 2024 Tanaka, 2024; Clowez, 2021) provided data, which were pooled in a meta-analysis. Of the patients undergoing arthrscopic osseous surgery 4/346 (1.2%) experienced recurrence compared to 6/370 (1.6%) of the patients undergoing open osseous surgery. The RR was 0.78 (95% CI 0.23 to 2.62), see Figure 7.
Figure 7. Forest plot showing the outcome redislocation for the comparison arthroscopic and open osseous surgery
Risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
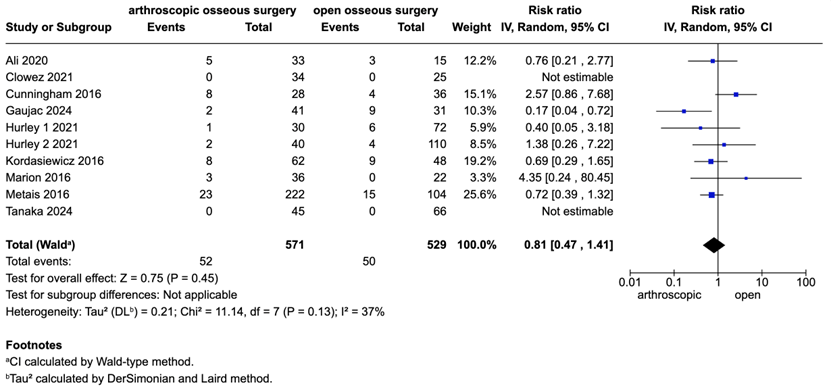
Complications (post-operative)
Seven studies from the systematic review of Deng (2024) reported the postoperative complication rate in patients undergoing arthroscopic surgery compared to open surgery (Ali, 2020; Cunningham, 2016; Hurley, 2021; Kordasiewicz, 2017; Marion, 2016; Metais, 2016). Additionally, four other studies (Gaujac, 2024; Girard, 2022; Tanaka, 2024; Clowez, 2021) provided data, which were pooled in a new meta-analysis.
Of the patients undergoing arthroscopic osseous surgery 52/571 (9.1%) experienced post-operative complications compared to 50/529 9.5%) of the patients undergoing open osseous surgery. The RR was 0.81 (95% CI 0.47 to 1.41), see Figure 8.
Figure 8. Forest plot showing the outcome complications (post-operative) for the comparison arthroscopic and open osseous surgery
Pooled risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Complications (intra-operative)
Three studies (Gaujac, 2024; Girard, 2022; Clowez, 2021) reported intra-operative complications in patients undergoing arthroscopic surgery compared to open surgery, which were pooled in a new meta-analysis. Of the patients undergoing arthroscopic osseous surgery 6/99 (6.1%) experienced intra-operative complications compared to 9/82 (11%) of the patients undergoing open osseous surgery. The RR was 0.63 (95% CI 0.23 to 1.71), see Figure 9.
Figure 9. Forest plot showing the outcome complications (intra-operative) for the comparison arthroscopic and open osseous surgery
Pooled risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Surgical duration
Four studies included in the systematic review by Deng (2024) compared operation times for arthroscopic versus open surgery (Cunningham, 2016; Kordasiewicz, 2017; Marion, 2016; Zhu, 2017), along with one additional study by Girard (2024). The results were pooled in a meta-analysis, showing showing a mean difference of 28.17 minutes in favor of open surgery, see Figure 10.
Figure 10. Forest plot showing the outcome surgical duration for the comparison arthroscopic and open osseous surgery
Pooled standardized mean difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Persisting apprehension
Five studies from the systematic review of Deng (2024) reported persistent apprehension at the last follow-up in patients who underwent arthroscopic surgery compared to those who underwent open surgery (Ali, 2020; Cunningham, 2016; Kordasiewicz, 2017; Metais, 2016; Zhu, 2017). Additionally, two studies (Girard, 2024; Clowez, 2021) provided data, and the results were pooled in a meta-analysis. Of the patients undergoing arthrscopic osseous surgery 63/449 (14%) had persisting apprehension compared to 34/298 (11.4%) of the patients undergoing open osseous surgery. The RR was 1.24 (95% CI 0.65 to 2.37), see Figure 11.
Figure 11. Forest plot showing the outcome persisting apprehension for the comparison arthroscopic and open osseous surgery
Pooled risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
3. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with recurrent shoulder instability after previous surgery with <15 % bone loss?
Calvo (2021) and Elamo (2020) reported respectively the outcomes recurrent instability and treatment failure.
- Calvo (2021) defined recurrent instability as the total number of redislocation and subluxation and recurrence of instability.
- Elamo (2020) defined treatment failure as recurrent instability requiring surgical intervention or persisting subluxations and/or dislocations.
In both studies, the occurrence of these outcomes was taken together and presented as an overall number for respectively recurrent instability and treatment failure. A subtotal for the specific outcomes was not presented, therefore it was not possible to report results for the individual predefined outcomes.
Redislocation / persistent instability / subluxation
Calvo (2021) reported the outcome recurrent instability (defined as redislocation or subluxation). Of the patients who underwent revisional arthroscopic Bankart repair, 2/17 (11.8%) experienced recurrent instability, compared to 5/28 (17.9%) patients who underwent revisional arthroscopic Latarjet surgery. The Risk Ratio (RR) was 0.66 (95% CI 0.14 to 3.03), Risk Difference (RD): -0.06 (95% CI -0.27, 0.15). See Table 3. Of the seven patients experiencing recurrent instability, two patients had dislocations and five patients had subluxations.
Elamo (2020) reported the outcome failure of intervention (defined as recurrence of instability requiring surgical intervention or persisting subluxations and/or dislocations). Of the patients who underwent revisional Arthroscopic Bankart surgery, 13/46 (28.3%) experienced failure of intervention, compared to 0/23 (0%) of the patients treated with revisional open Latarjet. The RD was 0.28 (95% CI 0.14 to 0.42). See Table 8.
Table 8. results for the outcome redislocation / persistent instability / subluxation
|
|
Soft tissue procedure (arthroscopic Bankart repair) |
Osseous procedure (arthroscopic/open Latarjet) |
Effect measure |
|
Calvo (2021) |
2/17 (11.8%) |
5/28 (17.9%) |
RD: -0.06 (95% CI -0.27, 0.15). |
|
Elamo (2020) |
13/46 (28.3%) |
0/23 (0% |
RD: 0.28 (95% CI 0.14 to 0.42). |
Complications
Calvo (2021) reported that there were no reported intra – or postoperative complications in the patients undergoing revisional arthroscopic repair (0/17) and patients undergoing revisional arthroscopic Latarjet (0/28). See Table 9.
Elamo (2020) reported the incidence of osteoarthritis at follow-up. After revisional arthroscopic Bankart repair, 19/46 (41.3%) patients experienced osteoarthritis, compared to 6/23 (26.1%) patients undergoing revisional open Latarjet procedure. The RR was 1.58 (95% CI 0.73, 3.42) and RD: 0.15 (95% CI -0.08, 0.38). See Table 4.
Table 9. results for the outcome complications
|
|
Soft tissue procedure (arthroscopic Bankart repair) |
Osseous procedure (arthroscopic/open Latarjet) |
Effect measure |
|
Calvo (2021) |
0/17 |
0/28 |
- |
|
Elamo (2020) |
19/46 (41.3%) |
6/23 (26.1%) |
RR: 1.58 (95% CI 0.73, 3.42) RD: 0.15 (95% CI -0.08, 0.38). |
Persistent apprehension
None of the included studies reported the outcome persistent apprehension.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following questions:
1. What are the benefits and harms of a soft tissue procedure compared to an osseous procedure for patients with shoulder instability who suffered 2 or more dislocations and/or with less than 25%bone loss?
Table 1. PICO 1
| Patients | Adult patients (> 18 years) with two or more dislocations with <25% bone loss |
| Intervention | Soft tissue procedure (e.g. Bankart) |
| Control | Osseous procedure (e.g. Latarjet) |
| Outcomes | Redislocation, complications, persistent instability, subluxation, persistent apprehension |
| Other selection criteria |
Study design:
|
2a. What are the benefits and harms of an arthroscopic soft tissue (Bankart) procedure, compared with an open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid)?
Table 2. PICO 2a
| Patients | Patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid) |
| Intervention | Arthroscopic soft tissue surgery (Bankart) |
| Control | Open soft tissue surgery (Bankart) |
| Outcomes | (Re)dislocation, subluxation, complications, surgical duration persisting apprehension |
| Other selection criteria |
Study design:
|
2b. What are the benefits and harms of an arthroscopic osseous (Bristow-Latarjet) procedure compared with an open osseous (Bristow-Latarjet) procedure in patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid)?
Table 3. PICO 2b
| Patients | Patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid) |
| Intervention | Arthroscopic osseous procedure (Bristow-Latarjet) |
| Control | Open coracoid transfer (Bristow-Latarjet) |
| Outcomes | (Re)dislocation, subluxation, complications, surgical duration, persisting apprehension |
| Other selection criteria |
Study design:
|
3. What are the benefits and harms of a soft tissue procedure compared to an osseous procedure for patients with recurrent shoulder instability after previous surgery with <15 % bone loss?
Table 4. PICO 3
| Patients | Patients (>18 years) with recurrent shoulder instability after previous operative treatment with <15% bone loss |
| Intervention | Soft tissue procedure (e.g. Bankart, hill sachs remplissage) |
| Control | Osseous procedure (e.g. Latarjet) |
| Outcomes |
Redislocation, complications, persistent instability, subluxation, persistent apprehension |
| Other selection criteria |
Study design:
|
Relevant outcome measures
The guideline development group considered (re)dislocation and complications as critical outcome measures for decision making; and persistent instability, subluxation, and persistent apprehension as important outcome measures for decision making.
A priori, the guideline development group did not define the outcome measures listed above but used the definitions used in the studies.
The guideline development group defined a threshold of 10% for continuous outcomes and for dichotomous outcomes of <0.80 and >1.25 as a minimal clinically (patient) important difference.
Search and select (Methods)
1. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with shoulder instability who suffered 2 or more dislocations and/or with less than 25% bone loss?
The databases Embase.com and Ovid/Medline were searched with relevant search terms until 20-12-2023. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 274 hits. Studies were selected based on the criteria described in Table 1. Twenty-three studies were initially selected based on title and abstract screening. After reading the full text, nineteen studies were excluded (see the table with reasons for exclusion under the tab ‘evidence tabellen’, and four studies were included.
2a. What are the (un)beneficial effects of an arthroscopic soft tissue (Bankart) procedure, compared with an open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid)?
A systematic literature search was performed by a medical information specialist using the following bibliographic databases: Embase.com and Ovid/Medline. Both databases were searched to 20th November 2024 for systematic reviews, RCTs and observational studies. Systematic searches were completed using a combination of controlled vocabulary/subject headings (e.g., Emtree-terms, MeSH) wherever they were available and natural language keywords. The overall search strategy was derived from three primary search concepts: (1) shoulder dislocation; (2) arthroscopic latarjet procedure; (3) open bankart repair. Duplicates were removed using EndNote software. After deduplication a total of 2651 records were imported for title/abstract screening.
Systematic reviews and randomized trials were selected based on the criteria described in Table 1 and Table 2 and 3. For question 2a, 33 studies were initially selected based on title and abstract screening. After reading the full text, 30 studies were excluded (see the table with reasons for exclusion under the tab ‘evidence tabellen’. One systematic review and one RCT were selected for question 3a and one systematic review (including observational research) was selected for question 3b.
2b. What are the (un)beneficial effects of an arthroscopic osseous (Bristow-Latarjet) procedure compared with an open osseous (Bristow-Latarjet) procedure in patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid)?
For question 2b no randomized controlled trials were found. Therefore, the observational studies published after the search data of the selected systematic review, were also screened for relevant publications. Titles and abstracts were screened using the ASReview software. The settings TF-IDF and Naïve bayes were used. Hurley (2021) was used as prior knowledge for inclusion. Sebastia-Forcada (2019) and Karpinski (2024) were used as prior knowledge for exclusions. The articles were screened by the guideline methodologist, using the following stopping rule: after 10% of the total set subsequent exclusions. Based on title and abstract, thirteen articles were initially selected. After screening the full-text articles, a total of five studies was included, and eight studies were excluded (see the table with reasons for exclusion under the tab Methods).”
3. What are the (un)beneficial effects of a soft tissue procedure compared to an osseous procedure for patients with recurrent shoulder instability after previous surgery with <15 % bone loss?
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms until 20-12-2023. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 274 hits. Studies were selected based on the criteria stated in Table 4. Twelve studies were initially selected based on title and abstract screening. After reading the full text, eleven studies were excluded (see the table with reasons for exclusion under the tab Methods) and one studies was considered relevant.
The systematic review from Lho (2023) was initially included. As this systematic review only included two relevant papers (Calvo, 2021; Elamo, 2020), the individual papers were included. The other studies included in the systematic review (Lho, 2023) were considered irrelevant because they did not make the correct comparison or did not include a control population.
Referenties
- Literatuur deelvraag 1
- Bakshi NK, Cibulas GA, Sekiya JK, Bedi A. A clinical comparison of linear- and surface area–based methods of measuring glenoid bone loss. Am J Sports Med. 2018;46(10):2472-2477.
- Balg F, Boileau P. The instability severity index score: a simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470-1477.
- Choo CH, Na SS, Choi BC, Kim DH. Complications related to Latarjet Shoulder Stabilization: a systematic review. Am J Sports Med. 2023 Jan;51(1):263-270.
- Di Giacomo G, Itoi E, Burkhart S. Evolving Concept of Bipolar Bone Loss and the Hill-Sachs Lesion: From “Engaging/Non-Engaging” Lesion to “On-Track/Off-Track” Lesion. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014;30(1):90-8. doi:10.1016/j.arthro.2013.10.004
- Gowd AK, Liu JN, Cabarcas BC, et al. Management of recurrent anterior shoulder instability with bipolar bone loss: a systematic review to assess critical bone loss amounts. Am J Sports Med.
- Clowez G, Gendre P, Boileau P. The Bristow-Latarjet procedure for revision of failed arthroscopic Bankart: a retrospective case series of 59 consecutive patients. J Shoulder Elbow Surg. 2021 Dec;30(12):e724-e731. doi: 10.1016/j.jse.2021.05.007. Epub 2021 Jun 2. PMID: 34087273.
- Hossein Zadeh R, Daliri M, Sadeghi M, Hossein Zadeh R, Sahebi M, Moradi A, Samei M, Ebrahimzadeh MH. Arthroscopic Bankart repair vs. Latarjet procedure for recurrent shoulder instability: a meta-analysis of clinical outcomes and complication rates in general and athletic populations. J Shoulder Elbow Surg. 2024 Aug 14:S1058-2746(24)00556-1. doi: 10.1016/j.jse.2024.06.024. Epub ahead of print. PMID: 39151667.
- Hurley ET, Toale JP, Davey MS, Colasanti CA, Pauzenberger L, Strauss EJ, Mullett H. Remplissage for anterior shoulder instability with Hill-Sachs lesions: a systematic review and meta-analysis.
- Imam MA, Shehata MSA, Martin A, Attia H, Sinokrot M, Bahbah EI, Gwilym S, Jacob J, Narvani AA, Meyer DC. Bankart Repair Versus Latarjet Procedure for Recurrent Anterior Shoulder Instability: A Systematic Review and Meta-analysis of 3275 Shoulders. Am J Sports Med. 2021 Jun;49(7):1945-1953. doi: 10.1177/0363546520962082. Epub 2020 Dec 2. Erratum in: Am J Sports Med. 2021 Jul;49(8):NP34. doi: 10.1177/03635465211024618. PMID: 33264030.] J Shoulder Elbow Surg. 2020 Dec;29(12):2487-2494. doi: 10.1016/j.jse.2020.06.021. Epub 2020 Jul 7.PMID: 32650087 Review.
- Locher J, Wilken F, Beitzel K, et al. Hill-Sachs off-track lesions as risk factor for recurrence of instability after arthroscopic Bankart repair. Arthroscopy. 2016;32(10):1993-1999.
- Min K, Fedorka C, Solberg MJ, Shaha SH, Higgins LD. The cost-effectiveness of the arthroscopic Bankart versus open Latarjet in the treatment of primary shoulder instability. J Shoulder Elbow Surg. 2018 Jun;27(6S):S2-S9. doi: 10.1016/j.jse.2017.11.013. Epub 2018 Jan 4. PMID: 29307674.
- Pugliese M, Loppini M, Vanni E, Longo UG, Castagna A. Cost-effectiveness analysis of arthroscopic Bankart repair versus open Latarjet reconstruction in anterior shoulder instability. Int Orthop. 2023 Jul;47(7):1771-1777. doi: 10.1007/s00264-023-05736-7. Epub 2023 Mar 28. Erratum in: Int Orthop. 2023 Jul;47(7):1885. doi: 10.1007/s00264-023-05811-z. PMID: 36973428.
- Rodriguez K, Hurley ET, Park CN, Clark B, Levin JM, Klifto CS, Dickens JF, Lau BC. Complications following arthroscopic bankart repair: a systematic review. J Shoulder Elbow Surg. 2024 Feb;33(2):435-440.
- Rutgers C, Verweij LPE, Schuit AA, Sierevelt IN, Jamaludin FS, van der Woude HJ, van den Bekerom MPJ. High resorption rates following glenoid augmentation procedures do not seem to lead to higher recurrence rates or worse clinical outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2023 Jul;31(7):2581-2592. doi: 10.1007/s00167-022-07267-x. Epub 2022 Dec 14. PMID: 36515733.
- Shaha JS, Cook JB, Song DJ, et al. Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43(7):1719-1725.
- Verweij LPE, van Spanning SH, Grillo A, Kerkhoffs GMMJ, Priester-Vink S, van Deurzen DFP, van den Bekerom MPJ. Age, participation in competitive sports, bony lesions, ALPSA lesions, > 1 preoperative dislocations, surgical delay and ISIS score > 3 are risk factors for recurrence following arthroscopic Bankart repair: a systematic review and meta-analysis of 4584 shoulders. Knee Surg Sports Traumatol Arthrosc. 2021 Dec;29(12):4004-4014. doi: 10.1007/s00167-021-06704-7. Epub 2021 Aug 22. PMID: 34420117; PMCID: PMC8595227.
- Weil S, Arnander M, Pearse Y, Tennent D. Reporting of glenoid bone loss measurement in clinical studies and the need for standardization : a systematic review. Bone Joint J. 2022 Jan;104-B(1):12-18. doi: 10.1302/0301-620X.104B1.BJJ-2021-0751.R1. PMID: 34969273.
- Williams HLM, Evans JP, Furness ND, Smith CD. It's Not All About Redislocation: A Systematic Review of Complications After Anterior Shoulder Stabilization Surgery. Am J Sports Med. 2019 Nov;47(13):3277-3283. doi: 10.1177/0363546518810711. Epub 2018 Dec 10. PMID: 30525905.
- Literatuur deelvraag 2
- Deng, Z. and Zheng, Y. and Su, J. and Chen, S. and Deng, Z. and Zhu, W. and Li, Y. and Lu, W. Open Versus Arthroscopic Latarjet for Recurrent Anterior Shoulder Instability: A Systematic Review and Meta-analysis. Orthopaedic Journal of Sports Medicine. 2023; 11 (5) :23259671231174476.
- Karpinski K, Akguen D, Gebauer H, Paksoy A, Lupetti M, Markova V, Zettinig O, Moroder P. Reliability of Manual Measurements Versus Semiautomated Software for Glenoid Bone Loss Quantification in Patients With Anterior Shoulder Instability. Orthop J Sports Med. 2024 Feb 12;12(2):23259671231222938. doi: 10.1177/23259671231222938. PMID: 38352173; PMCID: PMC10863483.
- Khatri, Kavin and Arora, Hobinder and Chaudhary, Sanjay and Goyal, Darsh Meta-Analysis of Randomized Controlled Trials Involving Anterior Shoulder Instability. The open orthopaedics journal. 2018; 12 :411-418.
- Sebastiá-Forcada E, Martínez-Rico S, Vizcaya-Moreno MF, Lizaur-Utrilla A. Prospective study on effectiveness and safety of arthroscopic Bankart using a single anterior portal for patients with anterior shoulder instability. Rev Esp Cir Ortop Traumatol (Engl Ed). 2019 Nov-Dec;63(6):431-438. English, Spanish. doi: 10.1016/j.recot.2019.05.002. Epub 2019 Jul 6. PMID: 31285179.
- Literatuur deelvraag 3
- Bakshi NK, Cibulas GA, Sekiya JK, Bedi A. A clinical comparison of linear- and surface area–based methods of measuring glenoid bone loss. Am J Sports Med. 2018;46(10):2472-2477.
- Balg F, Boileau P. The instability severity index score: a simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470-1477.
- Cognetti DJ, DeFoor MT, Hartzler RU, Sheean AJ. Glenoid augmentation for subcritical bone loss: a narrative review. Ann Jt. 2024 Apr 9;9:15. doi: 10.21037/aoj-23-36. PMID: 38690075; PMCID: PMC11058534.
- Choo CH, Na SS, Choi BC, Kim DH. Complications related to Latarjet Shoulder Stabilization: a systematic review. Am J Sports Med. 2023 Jan;51(1):263-270.
- Di Giacomo G, Itoi E, Burkhart S. Evolving Concept of Bipolar Bone Loss and the Hill-Sachs Lesion: From “Engaging/Non-Engaging” Lesion to “On-Track/Off-Track” Lesion. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014;30(1):90-8. doi:10.1016/j.arthro.2013.10.004.
- Gowd AK, Liu JN, Cabarcas BC, et al. Management of recurrent anterior shoulder instability with bipolar bone loss: a systematic review to assess critical bone loss amounts. Am J Sports Med.
- Haroun HK, Sobhy MH, Abdelrahman AA. Arthroscopic Bankart repair with remplissage versus Latarjet procedure for management of engaging Hill-Sachs lesions with subcritical glenoid bone loss in traumatic anterior shoulder instability: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020 Oct;29(10):2163-2174. doi: 10.1016/j.jse.2020.04.032. Epub 2020 Jun 9. PMID: 32807370.
- Hoyt BW, Tisherman RT, Popchak AJ, Dickens JF. Arthroscopic Bone Block Stabilization for Anterior Shoulder Instability with Subcritical Glenohumeral Bone Loss. Curr Rev Musculoskelet Med. 2024 Nov;17(11):465-475. doi: 10.1007/s12178-024-09921-y. Epub 2024 Aug 19. PMID: 39158663; PMCID: PMC11464743.
- Hurley ET, Toale JP, Davey MS, Colasanti CA, Pauzenberger L, Strauss EJ, Mullett H. Remplissage for anterior shoulder instability with Hill-Sachs lesions: a systematic review and meta-analysis.
- Locher J, Wilken F, Beitzel K, et al. Hill-Sachs off-track lesions as risk factor for recurrence of instability after arthroscopic Bankart repair. Arthroscopy. 2016;32(10):1993-1999.
- Rodriguez K, Hurley ET, Park CN, Clark B, Levin JM, Klifto CS, Dickens JF, Lau BC. Complications following arthroscopic bankart repair: a systematic review. J Shoulder Elbow Surg. 2024 Feb;33(2):435-440.
- Shaha JS, Cook JB, Song DJ, et al. Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43(7):1719-1725.
- Sinha S, Mehta N, Goyal R, Goyal A, Joshi D, Arya RK. Is Revision Bankart Repair with Remplissage a Viable Option for Failed Bankart Repair in Non-contact Sports Person Aiming to Return to Sports? Indian J Orthop. 2021 May 7;55(Suppl 2):359-365. doi: 10.1007/s43465-021-00415-4. PMID: 34306548; PMCID: PMC8275742.
- Weil S, Arnander M, Pearse Y, Tennent D. Reporting of glenoid bone loss measurement in clinical studies and the need for standardization : a systematic review. Bone Joint J. 2022 Jan;104-B(1):12-18. doi: 10.1302/0301-620X.104B1.BJJ-2021-0751.R1. PMID: 34969273.
Evidence tabellen
Risk of bias table for intervention studies (randomized controlled trials; based on Cochrane risk of bias tool and suggestions by the CLARITY Group at McMaster University), studies included for question 1
1. What are the benefits and harms of a soft tissue procedure compared to an osseous procedure for patients with shoulder instability who suffered 2 or more dislocations and/or with less than 25% bone loss?
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measure
LOW Some concerns HIGH
|
|
Abouelsoud (2015) |
Probably no
Reason: Besides in – and exclusion criteria they did not report on the allocation sequence. Solely stated that ‘’Odd number patients had a modified Latarjet procedure and even number patients had arthroscopic remplissage procedure with capsulolabral repair using four anchors.’’ This could suggest randomization however not specified. |
Probably no
Reason: Not reported |
Probably no
Reason: Not reported |
Probably yes
Reason:
Loss to follow-up over time not reported. |
Probably yes
Reason:
Study free of selective outcome reporting. |
Probably yes
Reason:
No other comments. |
High concerns of bias |
|
Kukkonen (2021) |
Probably yes
Reason: All patients were screened for the trial if they had been referred to the participating institutes with anteroinferior shoulder instability after an initial traumatic dislocation. The enrolled patients were randomised into either the arthroscopic Bankart or the Open Latarjet procedure. Further information not provided. |
Probably no
Reason:
Not reported |
Probably no
Reason:
Blinding not reported. Solely mentioned that all operations were carried out by experienced shoulder surgeons. Before commencing the trial, the surgeons held a wet-lab consensus meeting to decide how to perform both operations uniformly and in the best possible way. Additionally, a clinician or physiotherapist assessed the clinical outcomes. |
Probably yes
Reason:
Drop-out rate was 25% at two-year follow-up. Further not specified what the percentage of drop-out was in each study group. |
Probably yes
Reason:
Study free of selective outcome reporting. SSV, WOSI, Constant Score etc. solely presented in figures (Figure 5) à not quantified textually. |
Probably yes
Reason:
Small comment: funding source not reported. |
Some concerns of bias |
|
Russo (2017) |
Probably no
Reason:
From December 2011 to October 2015, 51 patients with anterior gleno-humeral instability underwent an open Latarjet procedure, and 40 to an ASA plus Bankart repair. Subsequently, 20 patients were selected from 51 patients treated with the Latarjet–Patte procedure with a minimum and maximum follow-up of 20 and 30 months, and the first 20 cases out of 40, treated with the Bankart plus ASA procedure, with a minimum follow-up of 12 months, were selected. |
Probably no
Reason:
Not reported |
Probably no
Reason:
Blinding not reported. Solely stated that clinical and radiological assessments were performed by one radiologist and two different shoulder surgeons. |
Probably yes
Reason:
Loss to follow-up over time not reported. |
Probably yes
Reason:
Study free of selective outcome reporting. |
Probably yes
Reason:
Funding source not reported, setting not reported (solely affiliations authors). |
High concerns of bias |
|
Zarezade (2014) |
Probably no
Reason:
Patients with recurrent anterior shoulder dislocation who were candidates for surgical treatment were randomly divided into two groups More information was not provided. |
Probably no
Reason:
Not reported
|
Probably no
Reason:
Not reported
|
Probably no
Reason:
In article it was stated that ‘’During the study, we excluded three patients as they were unavailable and not coming to our centers, two from Bankart group and one from Bristow group. Finally, these two groups with a population of 18 and 19, respectively, were compared with each other’’. |
Probably yes
Reason:
Study free of selective outcome reporting. |
Probably yes
Reason:
No other comments. |
Some concerns of Bias |
Table of excluded studies, question 1
|
Reference |
Reason for exclusion |
|
An VV, Sivakumar BS, Phan K, Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elbow Surg. 2016 May;25(5):853-63. doi: 10.1016/j.jse.2015.11.001. Epub 2016 Jan 19. PMID: 26809355. |
More recent and higher quality SR available (Imam, 2021) |
|
Bessière C, Trojani C, Carles M, Mehta SS, Boileau P. The open latarjet procedure is more reliable in terms of shoulder stability than arthroscopic bankart repair. Clin Orthop Relat Res. 2014 Aug;472(8):2345-51. doi: 10.1007/s11999-014-3550-9. PMID: 24615422; PMCID: PMC4079884. |
wrong design; retrospective cohort study |
|
Billaud A, Baverel L; ReSurg; SoFEC; Metais P. Arthroscopic Latarjet yields better union and prevention of instability compared to arthroscopic bony Bankart repair in shoulders with recurrent anterior instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2023 Dec;31(12):5994-6005. doi: 10.1007/s00167-023-07655-x. Epub 2023 Nov 18. PMID: 37980282. |
More recent and higher quality SR available (Imam, 2021) |
|
Bliven KCH, Parr GP. Outcomes of the Latarjet Procedure Compared With Bankart Repair for Recurrent Traumatic Anterior Shoulder Instability. J Athl Train. 2018 Feb;53(2):181-183. doi: 10.4085/1062-6050-232-16. Epub 2018 Jan 19. PMID: 29350555; PMCID: PMC5842908. |
wrong desing; commentary paper |
|
Davis WH, DiPasquale JA, Patel RK, Sandler AB, Scanaliato JP, Dunn JC, Parnes N. Arthroscopic Remplissage Combined With Bankart Repair Results in a Higher Rate of Return to Sport in Athletes Compared With Bankart Repair Alone or the Latarjet Procedure: A Systematic Review and Meta-analysis. Am J Sports Med. 2023 Oct;51(12):3304-3312. doi: 10.1177/03635465221138559. Epub 2023 Jan 9. PMID: 36622005. |
No relevant papers included, included papers had wrong design; retrospective studies or non-comparative |
|
Ernstbrunner L, De Nard B, Olthof M, Beeler S, Bouaicha S, Gerber C, Wieser K. Long-term Results of the Arthroscopic Bankart Repair for Recurrent Anterior Shoulder Instability in Patients Older Than 40 Years: A Comparison With the Open Latarjet Procedure. Am J Sports Med. 2020 Jul;48(9):2090-2096. doi: 10.1177/0363546520931090. Epub 2020 Jun 24. PMID: 32579397. |
wrong design; retrospective cohort study |
|
Haroun HK, Sobhy MH, Abdelrahman AA. Arthroscopic Bankart repair with remplissage versus Latarjet procedure for management of engaging Hill-Sachs lesions with subcritical glenoid bone loss in traumatic anterior shoulder instability: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020 Oct;29(10):2163-2174. doi: 10.1016/j.jse.2020.04.032. Epub 2020 Jun 9. PMID: 32807370. |
Not all included papers were relevant, relevant papers were included individually in the analysis of literature |
|
Hurley E, Anil U, Lim Fat D, Pauzenberger L, Strauss E, Mullett H. Operative Treatment of Anterior Shoulder Instability A Network Meta-Analysis. Bull Hosp Jt Dis (2013). 2020 Sep;78(3):202-209. PMID: 32857028. |
More recent and higher quality SR available (Imam, 2021) |
|
Hurley ET, Davey MS, Montgomery C, O'Doherty R, Gaafar M, Pauzenberger L, Mullett H. Arthroscopic Bankart Repair Versus Open Latarjet for Recurrent Shoulder Instability in Athletes. Orthop J Sports Med. 2021 Sep 8;9(9):23259671211023801. doi: 10.1177/23259671211023801. PMID: 34527752; PMCID: PMC8436306. |
wrong design; retrospective cohort study |
|
Imam MA, Shehata MSA, Martin A, Attia H, Sinokrot M, Bahbah EI, Gwilym S, Jacob J, Narvani AA, Meyer DC. Bankart Repair Versus Latarjet Procedure for Recurrent Anterior Shoulder Instability: A Systematic Review and Meta-analysis of 3275 Shoulders. Am J Sports Med. 2021 Jun;49(7):1945-1953. doi: 10.1177/0363546520962082. Epub 2020 Dec 2. Erratum in: Am J Sports Med. 2021 Jul;49(8):NP34. doi: 10.1177/03635465211024618. PMID: 33264030. |
Not all included papers were relevant, relevant papers were included individually in the analysis of literature |
|
Jeon YS, Jeong HY, Lee DK, Rhee YG. Borderline Glenoid Bone Defect in Anterior Shoulder Instability: Latarjet Procedure Versus Bankart Repair. Am J Sports Med. 2018 Jul;46(9):2170-2176. doi: 10.1177/0363546518776978. Epub 2018 Jun 7. PMID: 29879363. |
wrong design; retrospective cohort study |
|
Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014 Sep;30(9):1184-211. doi: 10.1016/j.arthro.2014.04.005. Epub 2014 Jun 4. PMID: 24907025. |
More recent and higher quality SR available (Imam, 2021) |
|
Mahirogullari M, Kuskucu M, Solakoglu C, Akmaz I, Pehlivan O, Kiral A, Kaplan H. Comparison of outcomes of two different surgeries in regarding to complications for chronic anterior shoulder instability. Arch Orthop Trauma Surg. 2006 Dec;126(10):674-9. doi: 10.1007/s00402-006-0190-x. Epub 2006 Jul 29. PMID: 16896744. |
More recent and higher quality SR available (Imam, 2021) |
|
Maiotti M, De Vita A, De Benedetto M, Cerciello S, Massoni C, Di Giunta A, Raffelini F, Lo Cascio R, Pirani P, Castricini R. Clinical outcomes and recurrence rate of 4 procedures for recurrent anterior shoulder instability: ASA, remplissage, open, and arthroscopic Latarjet: a multicenter study. J Shoulder Elbow Surg. 2023 May;32(5):931-938. doi: 10.1016/j.jse.2022.10.030. Epub 2022 Dec 5. PMID: 36470517. |
wrong design; retrospective cohort study |
|
Rai S, Tamang N, Sharma LK, Marasini RP, Singh JL, Khanal K, Ghimire Kc M, Sherchan B. Comparative study of arthroscopic Bankart repair versus open Latarjet procedure for recurrent shoulder dislocation. J Int Med Res. 2021 Apr;49(4):3000605211007328. doi: 10.1177/03000605211007328. PMID: 33845604; PMCID: PMC8047861. |
wrong design; retrospective cohort study |
|
Tucker A, Ma J, Sparavalo S, Coady CM, Wong I. Arthroscopic anatomic glenoid reconstruction has a lower rate of recurrent instability compared to arthroscopic Bankart repair while otherwise maintaining a similar complication and safety profile. J ISAKOS. 2022 Oct;7(5):113-117. doi: 10.1016/j.jisako.2022.05.003. Epub 2022 May 29. PMID: 35649503. |
wrong design; retrospective cohort study |
|
Wang, Yanjiao, Rui Wang, and Luning Sun. "Bankart pepair versus Bristow-Latarjet procedure for recurrent anterior instability of the shoulder: a meta-analysis." Chinese Journal of Tissue Engineering Research 25.21 2021: 3423. |
More recent and higher quality SR available (Imam, 2021) |
|
Wu D, Zhou Z, Song W, Chen D, Bai Z, Zhang X, Yu W, He Y. Arthroscopic Autologous Iliac Crest Grafting Results in Similar Outcomes and Low Recurrence Compared to Remplissage Plus Bankart Repair for Anterior Shoulder Instability With Bipolar Bone Defects. Arthroscopy. 2023 Jul;39(7):1600-1607. doi: 10.1016/j.arthro.2022.12.039. Epub 2023 Jan 25. PMID: 36708746. |
wrong design; retrospective cohort study |
|
Zimmermann SM, Scheyerer MJ, Farshad M, Catanzaro S, Rahm S, Gerber C. Long-Term Restoration of Anterior Shoulder Stability: A Retrospective Analysis of Arthroscopic Bankart Repair Versus Open Latarjet Procedure. J Bone Joint Surg Am. 2016 Dec 7;98(23):1954-1961. doi: 10.2106/JBJS.15.01398. PMID: 27926676. |
wrong design; retrospective cohort study |
Risk of bias table for intervention studies (randomized controlled trials; based on Cochrane risk of bias tool and suggestions by the CLARITY Group at McMaster University), studies included for question 2A
2a. What are the benefits and harms of an arthroscopic soft tissue (Bankart) procedure, compared with an open soft tissue (Bankart) surgery in patients with traumatic anterior shoulder instability (without clear bone loss of the glenoid)?
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measure
LOW Some concerns HIGH
|
|
Gupta, 2024 |
No information |
No information |
Definitely no
Reason: it was stated that surgeons were blinded. Patients, assessors and data-analysts were not blinded |
No information |
Probably no
Reason: it was stated that outcomes were assessed at 3, 6 and 12 months follow-up. Only outcomes at 12 months follow-up were presented. |
Probably yes;
Reason: no other sources of bias could be identified |
High;
No information on allocation and randomization procedure
Lack of blinding
Selective outcome reporting |
2b. What are the benefits and harms of an arthroscopic osseous (Bristow-Latarjet) procedure compared with an open osseous (Bristow-Latarjet) procedure in patients with traumatic anterior shoulder instability (with suspicion of bone loss of the anterior glenoid)?
|
Author Year |
Selection of participants
Was selection of exposed and non-exposed cohorts drawn from the same population?
|
Exposure
Can we be confident in the assessment of exposure?
|
Outcome of interest
Can we be confident that the outcome of interest was not present at start of study?
|
Confounding-assessment
Can we be confident in the assessment of confounding factors?
|
Confounding-analysis
Did the study match exposed and unexposed for all variables that are associated with the outcome of interest or did the statistical analysis adjust for these confounding variables? |
Assessment of outcome
Can we be confident in the assessment of outcome?
|
Follow up
Was the follow up of cohorts adequate? In particular, was outcome data complete or imputed?
|
Co-interventions
Were co-interventions similar between groups?
|
Overall Risk of bias
|
|
Nascimento (2024) |
Probably no
Reason: Although both groups met the same indication criteria for operation and followed the same postoperative protocol, they were treated in two different hospitals by different surgeons, which introduces a potential selection bias as they may not represent the exact same source population. |
Probably no
Reason: The type of surgical procedure was clearly documented in operative records and confirmed with postoperative imaging. However, the procedures were performed by different surgeons in different hospitals, which could introduce variability in how the procedures were executed. |
Definitely yes
Reason: The outcome was assessed postoperatively at defined intervals, and baseline measurements were recorded preoperatively. |
Definitely yes
Reason: The study identified potential confounders. Preoperative CTs and clinical records were systematically reviewed for these. Comprehensive confounder assessment was performed. |
Probably no
Reason: The study performed post hoc comparisons of baseline variables and multiple regression analysis to adjust for potential confounders. However, as this was a retrospective cohort study without matching, there remains a risk of residual confounding and bias. |
Definitely yes
Reason: Outcomes were evaluated at fixed postoperative time points using standardized, validated measures. The same evaluation protocol was followed for both groups.
|
Probably yes
Reason: Patients had scheduled follow-ups at 2 weeks, 3, 6, 12, and 24 months. The study specified a minimum follow-up of 24 months as an inclusion criterion. There’s no mention of missing data or imputation, implying complete follow-up data for included participants. |
Definitely yes
Reason: The postoperative rehabilitation protocol was standardized across both institutions, regardless of the surgical approach. |
High
|
|
Girard (2022) |
Definitely no
Reason: Patients were treated in two consecutive time periods: arthroscopic procedures from January to June 2018, and open procedures from July to December 2018. |
Probably yes
Reason: The type of surgical procedure (arthroscopic vs. open Latarjet) was clearly documented in operative reports, performed by the same experienced surgeon, and verified postoperatively. |
Definitely yes
Reason: All outcome measures were assessed postoperatively. Baseline clinical and radiological data were collected preoperatively. |
Probably no
Reason: Although baseline data were collected, there may still be unmeasured or uncontrolled confounders because no matching or advanced statistical adjustments were performed. |
Probably no
Reason: No matching or regression analysis; risk of residual confounding due to retrospective, time-based allocation. |
Definitely yes
Reason: Clinical and radiological outcomes were assessed by an independent observer blinded to the surgeon (for clinical follow-ups) and via standardized imaging protocols (CT at 6 months, repeated at 12 months if needed). |
Probably yes
Reason: all patients had at least 12 months of clinical follow-up, with predefined follow-up visits at day 15, day 45, 3 months, 6 months, and 1 year. |
Probably yes
Reason: Both groups received the same anesthesia protocol, perioperative medication regimen, and an identical, standardized rehabilitation protocol. |
High
|
|
Gaujac (2024) |
Probably no
Reason: Patients were treated in two time periods: 2014–2017 vs. 2017–2019, but were slected from the same center and single operator. |
Probably yes
Reason: The exposure (surgical technique: anterior drilling with screws vs. posterior drilling with buttons) is clearly defined and perfomed by a single operator. |
Defenitiy yes
Reason: The study involves surgery for recurrent anterior shoulder instability; all patients had this condition before surgery. |
Probably no
Reason: The groups were defined by time period, so temporal confounders may exist. There is no mention of baseline characteristic comparisons or additional confounder assessment. |
Definitely no
Reason: The groups were not matched or randomized, and no statistical adjustment for confounders was reported. |
Probably yes
Reason: Outcome measures were objective (CT scan with specific measurements), analyzed by two independent observers with good reproducibility. Observer 1 conducted blind measurements twice with a 2‐month gap. |
Probably yes
Reason: Follow-up was up to 24 months for complications and functional scores. There is no explicit statement about completeness or handling of missing data. |
Probably yes
Reason: Postoperative care and rehabilitation protocols were the same for both groups. |
High
|
|
Tanaka (2024) |
Probably yes
Reason: Both groups (open Bristow and AS-assisted Bristow) were drawn from the same center, during overlapping but sequential time periods. The cohorts represent consecutive series of patients undergoing surgery for anterior shoulder instability who were rugby players. |
Probably yes
Reason: Clearly documented with detailed surgical technique descriptions. The exposure is well-defined and reliably assessed by surgical records. |
Definitiely yes
Reason: The study focuses on postoperative outcomes. |
Probably no
Reason: The study collected baseline clinical scores and demographic data, but there is no detailed description of adjustment or matching for confounders such as age, activity level, severity of instability, or prior surgeries between groups. |
Definitely no
Reason: No clear evidence of matching or multivariate adjustment for confounders. The groups were compared using univariate statistical tests only (Mann-Whitney U and Fisher’s exact test). |
Probably no
Reason: Blinding of outcome assessors was not stated, so detection bias is possible. |
Probably no
Reason: Some patients were lost to follow-up (2 shoulders in AS-assisted group). |
Probably yes
Reason: Both groups had similar rehab protocols, with no reported differences in adjunct treatments, so co-interventions were likely comparable.
|
High |
|
Glowez (2024) |
Probably no
Reason: Only patients with failed Bankart repair treated by Bristow-Latarjet were included, but it is not clearly stated from what larger population these patients were selected.
|
Probably yes
Reason: Exposure is documented in surgical records. |
Probably yes
Reason: All patients had recurrent instability or symptoms after primary Bankart, so the outcome was new. |
Probably no
Reason: Some factors (sport type, bone loss severity) were assessed but not fully detailed. |
Definitely no
Reason: No matching or multivariate adjustment reported. |
Probably yes
Reason: Clinical and imaging outcomes assessed by two independent observers using validated tools. |
Probably yes
Reason: Minimum 24 months follow-up with no mention of missing data or imputation. |
No information
Reason: This was not explicitly stated. |
High |
Table of excluded studies question 2A and 2B
|
Reference |
Reason for exclusion |
|
Best MJ, Wang KY, Nayar SK, Agarwal AR, Kreulen RT, Sharma S, McFarland EG, Srikumaran U. Epidemiology of shoulder instability procedures: A comprehensive analysis of complications and costs. Shoulder Elbow. 2023 Aug;15(4):398-404. doi: 10.1177/17585732221116814. Epub 2022 Aug 4. PMID: 37538528; PMCID: PMC10395401. |
wrong comparison: latarjet, anterior bone block reconstruction, arthroscopic bankart, open bankart
|
|
Markes AR, Cevallos N, Lansdown DA, Ma CB, Feeley BT, Zhang AL. Risk for recurrent instability and reoperation following arthroscopic and open shoulder stabilization in a large cross-sectional population. JSES Int. 2022 Jul 5;6(5):730-735. doi: 10.1016/j.jseint.2022.06.004. PMID: 36081703; PMCID: PMC9446191. |
open versus arthrscopic stabilization surgery; not specified latarjet or Bankart
|
|
Bonnevialle N, Girard M, Dalmas Y, Martinel V, Faruch M, Mansat P. Short-Term Bone Fusion With Arthroscopic Double-Button Latarjet Versus Open-Screw Latarjet. Am J Sports Med. 2021 May;49(6):1596-1603. doi: 10.1177/03635465211001095. Epub 2021 Apr 8. PMID: 33830790. |
Relevant data not reported |
|
Prakash U, Kumar N. Open Versus Arthroscopic Surgical Management for Recurrent Anterior instability of the Shoulder: A Retrospective Analysis. International Journal of Pharmaceutical and Clinical Research 2024; 16(5); 1611-1614 |
Relevant data not reported |
|
Russo (2017) Russo A, Grasso A, Arrighi A, Pistorio A, Molfetta L. Accuracy of Coracoid Bone Graft Placement: Open versus Arthroscopic Latarjet. Joints. 2017 Jul 28;5(2):85-88. doi: 10.1055/s-0037-1603934. PMID: 29114636; PMCID: PMC5672875. |
No relevant outcomes reported |
|
Taverna E, Guarrella V, Cartolari R, Ufenast H, Broffoni L, Barea C, Garavaglia G. Arthroscopically-assisted Latarjet: an easy and reproducible technique for improving the accuracy of graft and screw placement. Shoulder Elbow. 2018 Apr;10(2):99-106. doi: 10.1177/1758573217706701. Epub 2017 May 15. PMID: 29560035; PMCID: PMC5851123. |
No relevant outcomes reported |
|
Abdul-Rassoul, H. and Galvin, J. W. and Curry, E. J. and Simon, J. and Li, X. Return to Sport After Surgical Treatment for Anterior Shoulder Instability: A Systematic Review. The American journal of sports medicine. 2019; 47 (6) :1507-1515 |
wrong outcome |
|
Ahmed AS, Gabig AM, Dawes A, Gottschalk MB, Lamplot JD, Wagner ER. Trends and projections in surgical stabilization of glenohumeral instability in the United States from 2009 to 2030: rise of the Latarjet procedure and fall of open Bankart repair. J Shoulder Elbow Surg. 2023 Aug;32(8):e387-e395. doi: 10.1016/j.jse.2023.03.011. Epub 2023 Apr 10. PMID: 37044304. |
wrong design: database analysis |
|
Bitar IJ, Marangoni LD, Bustos DG, Pezzutti L, Bitar LB. Open Bankart repair plus inferior capsular shift versus isolated arthroscopic Bankart repair in collision athletes with recurrent anterior shoulder instability: a prospective study. J Shoulder Elbow Surg. 2024 Dec;33(12):2572-2579. doi: 10.1016/j.jse.2024.03.041. Epub 2024 May 10. PMID: 38734129. |
wrong design: geen randomisatie |
|
Bottoni CR, Johnson JD, Zhou L, Raybin SG, Shaha JS, Cruz CA, Lindell KK, Thoma DC. Arthroscopic Versus Open Anterior Shoulder Stabilization: A Prospective Randomized Clinical Trial With 15-Year Follow-up With an Assessment of the Glenoid Being "On-Track" and "Off-Track" as a Predictor of Failure. Am J Sports Med. 2021 Jul;49(8):1999-2005. doi: 10.1177/03635465211018212. Epub 2021 Jun 8. Erratum in: Am J Sports Med. 2022 Feb;50(2):NP14-NP15. doi: 10.1177/03635465211067445. PMID: 34102075. |
wrong outcome: clinical failure, defined as single redislocation, surgery for recurrent dislocation, subjective instability |
|
Cerciello, S. and Corona, K. and Morris, B. J. and Santagada, D. A. and Maccauro, G. Early Outcomes and Perioperative Complications of the Arthroscopic Latarjet Procedure: Systematic Review and Meta-analysis. The American journal of sports medicine. 2019; 47 (9) :2232-2241 |
only case-series and case reports included |
|
Chen, L. and Xu, Z. and Peng, J. and Xing, F. and Wang, H. and Xiang, Z. Effectiveness and safety of arthroscopic versus open Bankart repair for recurrent anterior shoulder dislocation: a meta-analysis of clinical trial data. Archives of Orthopaedic and Trauma Surgery. 2015; 135 (4) :529-538 |
More recent and higher quality SR available |
|
Cho, Chul-Hyun and Na, Sang Soo and Choi, Byung-Chan and Kim, Du-Han Complications Related to Latarjet Shoulder Stabilization: A Systematic Review. The American journal of sports medicine. 2023; 51 (1) :263-270 |
wrong outcome: complication rate? |
|
Desmeules, F. and Barry, J. and Roy, J. S. and Vendittoli, P. A. and Rouleau, D. M. Surgical interventions for post-traumatic anterior shoulder instability in adults. Cochrane Database of Systematic Reviews. 2014; 2014 (5) :CD011092 |
Low quality SR: SR (no specific description of the included primary studies) |
|
Freedman, Kevin B. and Smith, Adam P. and Romeo, Anthony A. and Cole, Brian J. and Bach, Bernard R., Jr. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for Recurrent Anterior instability of the shoulder: a meta-analysis. The American journal of sports medicine. 2004; 32 (6) :1520-1527 |
More recent and higher quality SR available |
|
Gao, B. and DeFroda, S. and Bokshan, S. and Ready, L. V. and Sullivan, K. and Etzel, C. and Owens, B. D. Arthroscopic Versus Open Bankart Repairs in Recurrent Anterior Shoulder Instability: A Systematic Review of the Association Between Publication Date and Postoperative Recurrent Instability in Systematic Reviews. Arthroscopy - Journal of Arthroscopic and Related Surgery. 2020; 36 (3) :862-871 |
Wrong outcome; association between publication date and outcomes |
|
Hobby, J. and Griffin, D. and Dunbar, M. and Boileau, P. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. Journal of Bone and Joint Surgery - Series B. 2007; 89 (9) :1188-1196 |
SR of comparative studies (no RCT) + case series |
|
Hohmann, E. and Tetsworth, K. and Glatt, V. Open versus arthroscopic surgical treatment for anterior shoulder dislocation: a comparative systematic review and meta-analysis over the past 20 years. Journal of Shoulder and Elbow Surgery. 2017; 26 (10) :1873-1880 |
More recent and higher quality SR available |
|
Horner, N. S. and Moroz, P. A. and Bhullar, R. and Habib, A. and Simunovic, N. and Wong, I. and Bedi, A. and Ayeni, O. R. Open versus arthroscopic Latarjet procedures for the treatment of shoulder instability: A systematic review of comparative studies. BMC Musculoskeletal Disorders. 2018; 19 (1) :255 |
More recent and higher quality SR available |
|
Hurley, E. T. and Lim Fat, D. and Farrington, S. K. and Mullett, H. Open Versus Arthroscopic Latarjet Procedure for Anterior Shoulder Instability: A Systematic Review and Meta-analysis. The American journal of sports medicine. 2019; 47 (5) :1248-1253 |
More recent and higher quality SR available |
|
Kumar S, Ranjan V, Utkarsh. A Retrospective Comparative Study of Arthroscopic Versus Open Surgical Treatment for Recurrent Anterior Instability of the Shoulder. Int J Pharm Clin Res. 2024;16(2):1214-1217. citeturn0search1 |
wrong design: retrospective study |
|
Lee MS, Patel SM, Klug T, Moran J, Park N, Mahatme RJ, Fong S, Gillinov SM, Dawes A, Surucu S, Graf A, Jimenez AE. Over 89% of Patients Return to Work After Undergoing Arthroscopic or Open Latarjet Procedure for Anterior Shoulder Instability: A Systematic Review. Arthroscopy. 2024 Oct 9:S0749-8063(24)00781-3. doi: 10.1016/j.arthro.2024.09.056. Epub ahead of print. PMID: 39393429. |
wrong outcome: return to work |
|
Malahias, Michael-Alexander and Fandridis, Emmanouil and Chytas, Dimitrios and Chronopulos, Efstathios and Brilakis, Emmanouil and Antonogiannakis, Emmanouil Arthroscopic versus open Latarjet: a step-by-step comprehensive and systematic review. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2019; 29 (5) :957-966 |
More recent and higher quality SR available |
|
Miura, K. and Tsuda, E. and Tohyama, H. and Iwahori, Y. and Mae, T. and Mochizuki, Y. and Nakagawa, K. and Nakamae, A. and Nakamura, T. and Takao, M. and Uchida, S. and Muneta, T. and Ochi, M. Can arthroscopic Bankart repairs using suture anchors restore equivalent stability to open repairs in the management of traumatic anterior shoulder dislocation? A meta-analysis. Journal of Orthopaedic Science. 2018; 23 (6) :935-941 |
Higher quality SR available |
|
Mohtadi, N. G. H. and Bitar, I. J. and Sasyniuk, T. M. and Hollinshead, R. M. and Harper, W. P. Arthroscopic versus open repair for traumatic anterior shoulder instability: A meta-analysis. Arthroscopy - Journal of Arthroscopic and Related Surgery. 2005; 21 (6) :652-658 |
More recent and higher quality SR available |
|
Pan D, Suo Y, Chen Q, Hou D, Zhang L. Effect of open versus minimally invasive surgery on postoperative wound site complications in patients with recurrent shoulder instability: A meta-analysis. Int Wound J. 2023 Sep 26;21(2):e14412. doi: 10.1111/iwj.14412. Epub ahead of print. Retraction in: Int Wound J. 2025 Mar;22(3):e70353. doi: 10.1111/iwj.70353. PMID: 37751908; PMCID: PMC10824617. |
More recent and higher quality SR available |
|
Petrera, M. and Patella, V. and Patella, S. and Theodoropoulos, J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surgery, Sports Traumatology, Arthroscopy. 2010; 18 (12) :1742-1747 |
More recent and higher quality SR available |
|
Pulavarti, R. S. and Symes, T. H. and Rangan, A. Surgical interventions for anterior shoulder instability in adults. Cochrane Database of Systematic Reviews. 2009; (4) :CD005077 |
More recent and higher quality SR available |
|
Randelli, P. and Fossati, C. and Stoppani, C. and Evola, F. R. and De Girolamo, L. Open Latarjet versus arthroscopic Latarjet: clinical results and cost analysis. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2016; 24 (2) :526-532 |
wrong outcome: cost analysis |
|
Rollick, Natalie C. and Ono, Yohei and Kurji, Hafeez M. and Nelson, Atiba A. and Boorman, Richard S. and Thornton, Gail M. and Lo, Ian Ky Long-term outcomes of the Bankart and Latarjet repairs: a systematic review. Open access journal of sports medicine. 2017; 8 :97-105 |
Low quality SR: SR (no specific description of the included primary studies) |
|
Uchiyama Y, Handa A, Shimpuku E, Omi H, Hashimoto H, Imai T, Watanabe M. Open Bankart repair plus inferior capsular shift versus arthroscopic Bankart repair without augmentations for traumatic anterior shoulder instability: A prospective study. J Orthop Surg (Hong Kong). 2017 Sep-Dec;25(3):2309499017727947. doi: 10.1177/2309499017727947. PMID: 28946834. |
wrong design: geen randomisatie |
|
Wang, L. and Liu, Y. and Su, X. and Liu, S. A meta-analysis of arthroscopic versus open repair for treatment of bankart lesions in the shoulder. Medical Science Monitor. 2015; 21 :3028-3035 |
More recent and higher quality SR available |
|
Williams, H. L. M. and Evans, J. P. and Furness, N. D. and Smith, C. D. It's Not All About Redislocation: A Systematic Review of Complications After Anterior Shoulder Stabilization Surgery. The American journal of sports medicine. 2019; 47 (13) :3277-3283 |
Low quality SR: SR (no specific description of the included primary studies) |
|
Zhu Y, Jiang C, Song G. Arthroscopic Versus Open Latarjet in the Treatment of Recurrent Anterior Shoulder Dislocation With Marked Glenoid Bone Loss: A Prospective Comparative Study. Am J Sports Med. 2017 Jun;45(7):1645-1653. doi: 10.1177/0363546517693845. Epub 2017 Mar 28. PMID: 28351205. |
wrong design: geen randomisatie |
Risk of bias table for interventions studies (cohort studies based on risk of bias tool by the CLARITY Group at McMaster University), studies included for question 3
3. What are the benefits and harms of a soft tissue procedure compared to an osseous procedure for patients with recurrent shoulder instability after previous surgery with <15 % bone loss?
|
Author, year |
Selection of participants
Was selection of exposed and non-exposed cohorts drawn from the same population?
|
Exposure
Can we be confident in the assessment of exposure?
|
Outcome of interest
Can we be confident that the outcome of interest was not present at start of study?
|
Confounding-assessment
Can we be confident in the assessment of confounding factors?
|
Confounding-analysis
Did the study match exposed and unexposed for all variables that are associated with the outcome of interest or did the statistical analysis adjust for these confounding variables |
Assessment of outcome
Can we be confident in the assessment of outcome?
|
Follow up
Was the follow up of cohorts adequate? In particular, was outcome data complete or imputed?
|
Co-interventions
Were co-interventions similar between groups?
|
Overall Risk of bias
|
|
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Definitely yes, probably yes, probably no, definitely no |
Low, Some concerns, High |
|
|
Calvo, 2021 |
Definitely no
Reason: treatment decision was based on the period in which the patients underwent surgery (before 2012 Bankart and after 2012 Latarjet) |
Probably yes
Reason: one single senior surgeon performed all procedures, surgical data was collected |
Definitely yes
Reason: Post-operative outcomes |
No information |
Probably no
Reason: Select study population, but no matching or multivariate analysis |
Definitely yes
Reason: an independent examiner assessed the outcomes |
Definitely yes
Reason: There were no dropouts, and 2-year data were collected for all patients |
Definitely yes
Reason: patients followed the same postoperative protocol. |
Some concerns, due to the selection of participants, no correction for confounding factors |
|
Elamo 2020 |
Probably yes;
Reason: all patients treated in a single hospital between 2002 and 2013 |
Definitely yes;
Reason: data was retrieved from the patient history and medical records |
Definitely yes
Reason: Post-operative outcomes |
Definitely yes
Reason: Post-operative data |
Probably no
Reason: No matching or multivariate analysis |
Definitely yes
Reason: the patients were clinically examined by an independent investigator |
Definitely no
Reason: high loss-to-follow-up rate. Length of follow-up differed between intervention and control
Respectively n=16 and n=5 in the intervention and control group |
No information |
Some concerns, no correction for confounding factors, high loss to follow-up rate |
Table of excluded studies for question 3
|
Reference |
Reason for exclusion |
|
Lho, T., Lee, J., Oh, K. S., & Chung, S. W. (2023). Latarjet procedure for failed Bankart repair provides better stability and return to sports, but worse postoperative pain and external rotation limitations with more complications, compared to revision Bankart repair: a systematic review and meta‐analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 31(8), 3541-3558. |
SR and meta-analysis of 24 studies. The included studies in the SR with an adequate control group were: Elamo (2020), Calvo (2021), Werhtel et al., Flinkkilä et al., and Rossi et al.,. Werhtel et al., Flinkkilä et al., and Rossi et al. made the wrong comparison: a.o. to compare the postoperative outcomes of the Latarjet procedure when performed as primary surgery and as revision for a failed arthroscopic Bankart repair; to compare the results from Latarjet as a primary operation vs. revision surgery after a failed arthroscopic Bankart repair for posttraumatic anteroinferior shoulder instability. In addition, to assess the effect of preoperative bony pathology on outcome; and To compare return to sport, functional outcomes, and complications of the modified Latarjet performed as a primary or revision procedure in competitive athletes. |
|
Frank, R. M., Mellano, C., Shin, J. J., Feldheim, T. F., Mascarenhas, R., Yanke, A. B., ... & Verma, N. N. (2015). Clinical outcomes following revision anterior shoulder stabilization: arthroscopic revision stabilization versus Latarjet. Orthopaedic Journal of Sports Medicine, 3(7_suppl2), 2325967115S00048. |
Wrong study design |
|
Longo, U. G., Loppini, M., Rizzello, G., Ciuffreda, M., Berton, A., Maffulli, N., & Denaro, V. (2014). Remplissage, humeral osteochondral grafts, weber osteotomy, and shoulder arthroplasty for the management of humeral bone defects in shoulder instability: systematic review and quantitative synthesis of the literature. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 30(12), 1650-1666. |
In Boileau et al. (2012) (therapeutic study) patients with humeral-sidebone loss undergone previous surgery (Open Bristow-Latarjet procedure (6), open Bankart procedure(1), arthroscopic Bankart repair) Humeral-sidebone and Raiss (2014) also included patients with previous surgery however wrong design (retrospective study). Andere studies vergeleken ook bv de combinatie van remplis en bankart vs bankart alone (niet de I en C onze studie) |
|
Clowez, G., Gendre, P., & Boileau, P. (2021). The Bristow-Latarjet procedure for revision of failed arthroscopic Bankart: a retrospective case series of 59 consecutive patients. Journal of Shoulder and Elbow Surgery, 30(12), e724-e731. |
Wrong study design |
|
Agarwalla, A., Gowd, A. K., Liu, J. N., Garcia, G. H., Perry, A. K., Polce, E. M., ... & Verma, N. N. (2022). High rate of return to work by 3 months following Latarjet for anterior shoulder instability. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 38(3), 684-691. |
Wrong study design |
|
Ranalletta, M., Rossi, L. A., Bertona, A., Tanoira, I., Maignon, G. D., & Bongiovanni, S. L. (2018). Modified Latarjet procedure without capsulolabral repair for the treatment of failed previous operative stabilizations in athletes. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 34(5), 1421-1427. |
No comparison |
|
Flinkkilä, T., & Sirniö, K. (2015). Open Latarjet procedure for failed arthroscopic Bankart repair. Orthopaedics & Traumatology: Surgery & Research, 101(1), 35-38. |
Retrospective study and no comparison |
|
O'Neill, D. C., Christensen, G., Kawakami, J., Burks, R. T., Greis, P. E., Tashjian, R. Z., & Chalmers, P. N. (2020). Revision anterior glenohumeral instability: is arthroscopic treatment an option?. JSES international, 4(2), 287-291. |
Wrong study design |
|
Boileau, P., Richou, J., Lisai, A., Chuinard, C., & Bicknell, R. T. (2009). The role of arthroscopy in revision of failed open anterior stabilization of the shoulder. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 25(10), 1075-1084. |
Wrong study design |
|
Friedman, L. G. M., Griesser, M. J., Miniaci, A. A., & Jones, M. H. (2014). Recurrent instability after revision anterior shoulder stabilization surgery. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 30(3), 372-381. |
No comparison:, in all studies solely one procedure is mentioned > no comparison |
|
Werthel, J. D., Sabatier, V., Schoch, B., Amsallem, L., Nourissat, G., Valenti, P., ... & Hardy, A. (2020). Outcomes of the Latarjet procedure for the treatment of chronic anterior shoulder instability: patients with prior arthroscopic Bankart repair versus primary cases. The American journal of sports medicine, 48(1), 27-32. |
Wrong design: A multicenter retrospective comparative case-cohort analysis |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 17-02-2026
Beoordeeld op geldigheid : 17-02-2026
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd door de Stichting Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodules is in 2022 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met schouderinstabiliteit.
Werkgroep richtlijn schouderinstabiliteit
- Prof. Dr. M.P.J (Michel) Bekerom, orthopedisch chirurg OLVG en MC Jan van Gooijen, NOV – voorzitter richtlijnwerkgroep
- Dr. J.J.A.M. (Jos) van Raaij, orthopedisch chirurg, niet praktiserend, NOV
- Dr. O.A.J. (Olivier) van der Meijden, orthopedisch chirurg Albert Schweitzer Ziekenhuis, NOV
- Dr. A.R. (Alex) Poublon, orthopedisch chirurg Ziekenhuis Gelderse Vallei, NOV
- Dr. T.D.W. (Tjarco) Alta, orthopedisch chirurg Spaarne Gasthuis, NOV
- Dr. R.J. (Robert Jan) Derksen, traumachirurg, Zaans Medisch Centrum, NVvH
- MSc. F. (Femke) Boon, fysio-, manueel therapeut, extended scope specialist Schoudercentrum IBC, KNGF
- MSc. K.M.C. (Karin) Hekman, fysio-, manueel therapeut, extended scope specialist, Schoudercentrum IBC, KNGF
- Dr. I.D. (Iris) Kilsdonk, radioloog Deventer Ziekenhuis, NVvR
- Dr. H.J. (Henk-Jan) van der Woude, radioloog OLVG, NVvR
- Drs. H.K. (Rik) van der Kolk, sportarts OLVG, VSG
- Mevr. drs. G. (Gerardine) Willemsen-de Mey, patiëntvertegenwoordiger Nationale Vereniging ReumaZorg Nederland
Met ondersteuning van
- Dr. J. (Jacqueline) Jennen, adviseur Kennisinstituut van de Federatie Medisch Specialisten (tot december 2023)
- Dr. F. (Floor) Willeboordse, senior adviseur Kennisinstituut van de Federatie Medisch Speciaisten (tot januari 2025)
- Dr. M.S. (Matthijs) Ruiter, senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten (vanaf januari 2025)
- MSc. D.G. (Dian) Ossendrijver, adviseur kennisinstituut van de Federatie Medisch Specialisten (vanaf december 2023)
- Dr. M. (Michiel) Oerbekke, adviseur Kennisinstituut van de Federatie Medisch Specialisten
- Dr. J. (Jing) de Haan-Du, adviseur Kennisinstituut van de Federatie Medisch Specialisten
- E. (Esther) van Bijl, medisch informatiespecialist, kennisinstituut van de Federatie Medisch Specialisten
Belangenverklaringen
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten via secretariaat@kennisinstituut.nl.
Gemelde (neven)functies en belangen werkgroep
|
Naam |
Hoofdfunctie |
Neven werkzaamheden |
Persoonlijke financiële belangen |
Persoonlijke relaties |
Extern gefinancierd onderzoek |
Intellectuele belangen en reputatie |
Overige belangen |
Datum |
Restrictie |
|
Michel van den Bekerom (voorzitter) |
Orthopedisch chirurg, OLVG, Amsterdam |
Betaald onderwijs geven bij/voor: |
Geen |
Geen |
Onderzoek gesteund door: SECEC (European Society for surgery of the shoulder an the elbow), ZonMW, SNN (Smith and Nephew). Het OLVG ontvangt financiële support voor een shoulder and elbow clinical and research fellowship van van Smith en Nephew. Dit fellowship wordt mede (financieel) ondersteund door een firma die materiaal maakt dat gebruikt wordt voor schouderstabilisaties. Het betreft een overeenkomst tussen het OLVG en de firma vanwege educatieve doeleinden. |
Geen |
Het OLVG is voornemens om een consultancy contract met zimmer/biomet op te stellen zodat ik op vraag elders kan opereren. |
19-10-2022 |
Geen restricties
|
|
Jos van Raaij |
Orthopedisch chirurg, Martini ziekenhuis Groningen |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
11-07-2022 |
Geen restricties |
|
Olivier van der Meijden |
Orthopedisch chirurg |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
28-09-2023 |
Geen restricties |
|
Alexander Poublon |
Orthopedisch chirurg met aandachtsgebied schouder |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
06-10-2023 |
Geen restricties |
|
Tjarco Alta |
Orthopedisch Chirurg |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
28-09-2023 |
Geen restricties |
|
Karin Hekman |
Fysiotherapeut bij Schoudercentrum IBC |
Voorzitter Schoudernetwerk Nederland; onkostenvergoeding |
Ik behandel patiënten die schouderinstabiliteit hebben binnen het schoudercentrum en binnen MC Jan van Goyen, dit is de reden voor het plaatsnemen in deze expertise groep. |
Geen |
Geen |
Het enige voordeel dat deelname aan deze richtlijn oplevert is nog meer persoonlijke expertise wat mogelijk leidt tot een verdieping van de fysiotherapeutische toepassingen bij schouderinstabiliteit. Dit is voor het SchouderNetwerk Nederland van primair belang en kan leiden tot uitdragen van kennis naar de regionale netwerken. Als voorzitter van deze stichting voel ik mij hier verantwoordelijk voor. |
Geen |
09-10-2023 |
Geen restricties |
|
Femke Boon |
Fysio- manueel therapeut en Extended Scope specialist bij Schoudercentrum IBC locatie Amstelland |
- 2x/ maand elleboog-schouder orthopedie poli bij Medisch Centrum Jan van Goyen (betaald, gedetacheerd vanuit IBC) |
Werkzaam bij Schoudercentrum IBC Amstelland |
Geen |
Richtlijn ontwikkeling FMS primaire anterieure schouderluxaties |
Geen |
Geen |
4-10-2023 |
Geen restricties |
|
Iris Kilsdonk |
Deventer Ziekenhuis |
Bestuurslid NVvR, sectie muskuloskeletale radiologie |
Geen |
Geen |
Geen |
Geen |
Geen |
2-10-2023 |
Geen restricties |
|
Robert Jan Derksen |
Traumachirurg Zaans Medisch Centrum |
Bestuurslid NVT |
Geen |
Geen |
Geen |
Geen |
Geen |
28-08-2022 |
Geen restricties |
|
Rik van der Kolk |
Sportarts, OLVG |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
10-08-2022 |
Geen restricties |
|
Henk-Jan van der Woude |
Radioloog Onze Lieve Vrouwe Gasthuis Amsterdam |
Consulent Commissie voor Beentumoren, onbezoldigd |
Geen |
Geen |
Geen |
Geen |
Geen |
07-02-2023 |
Geen restricties |
Inbreng patiëntenperspectief
De werkgroep besteedde aandacht aan het patiëntenperspectief door het uitnodigen van de Patiëntenfederatie Nederland en de Nationale Vereniging ReumaZorg Nederland voor de knelpunteninventarisatie. Daarnaast nam een patiëntvertegenwoordiger van ReumaZorg Nederland deel aan de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voor commentaar voorgelegd aan Patiëntenfederatie Nederland en ReumaZorg Nederland en de eventueel aangeleverde commentaren zijn bekeken en verwerkt
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijnmodule voerde de werkgroep conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uit om te beoordelen of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling is de richtlijnmodule op verschillende domeinen getoetst (zie het stroomschema bij Werkwijze).
|
Module |
Uitkomst raming |
Toelichting |
|
Operatieve behandeling |
Geen financiële gevolgen |
Uit de toetsing volgt dat de aanbeveling(en) niet breed toepasbaar zijn (<5.000 patiënten) en zal daarom naar verwachting geen substantiële financiële gevolgen hebben voor de collectieve uitgaven.
|
Werkwijze
Voor meer details over de gebruikte richtlijnmethodologie verwijzen wij u naar de Werkwijze. Relevante informatie voor de ontwikkeling van deze richtlijn is hieronder weergegeven.
Zoekverantwoording
Question 1
Algemene informatie
|
Cluster/richtlijn: Schouderinstabiliteit Module 6 en 7 - Operatieve behandeling 1 en 2 |
|
|
Uitgangsvraag/modules: Wat is de indicatie voor een operatieve behandeling bij patiënten met schouderinstabiliteit? Wat is de indicatie voor een operatieve behandeling bij patiënten met recidief schouderinstabiliteit na eerdere operatieve behandeling? |
|
|
Database(s): Embase.com, Ovid/Medline |
Datum: 20-12-2023 |
|
Periode: vanaf 2003 |
Talen: geen restrictie |
|
Literatuurspecialist: Esther van der Bijl |
Rayyan review: https://rayyan.ai/reviews/879934 |
|
BMI-zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting: Voor deze vraag is gezocht op de elementen:
Vanwege de grote opbrengst is in overleg gezocht met de P AND I AND C.
→ Het sleutelartikel PMID 33172578 wordt niet gevonden met deze search. Het valt uit op studiedesign. |
|
|
Te gebruiken voor richtlijntekst: In de databases Embase.com en Ovid/Medline is op 20-12-2023 systematisch gezocht naar systematische reviews, RCTs en observationele studies over wekedelen procedures vergeleken met een ossale procedures voor patiënten met schouder instabiliteit. De literatuurzoekactie leverde 274 unieke treffers op. |
|
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SR |
42 |
36 |
46 |
|
RCT |
38 |
17 |
44 |
|
Observationeel |
161 |
151 |
185 |
|
Totaal |
241 |
204 |
275* |
*in Rayyan
Zoekstrategie - 20 december 2023
Embase.com
|
No. |
Query |
Results |
|
#1 |
'shoulder dislocation'/exp OR 'recurrent shoulder dislocation'/exp OR ('shoulder'/exp AND ('dislocation'/de OR 'recurrent dislocation'/exp OR 'subluxation'/exp OR 'joint dislocation'/exp OR 'bone erosion'/exp OR 'joint instability'/de)) OR ((('shoulder' OR 'gleno-humeral*' OR 'humer*' OR 'scapulohumer*') NEAR/3 ('dislocat*' OR 'diastasis' OR 'instabil*' OR 'luxat*' OR 'subluxat*')):ti,ab,kw) OR ('shoulder':ti,ab,kw AND (('bon*' NEAR/3 ('resorption' OR 'loss' OR 'erosion')):ti,ab,kw)) OR 'bankart lesion'/exp OR (('bankart' NEAR/3 ('fracture*' OR 'lesion*' OR 'tear*')):ti,ab,kw) OR (('hill-sachs' NEAR/3 'lesion*'):ti,ab,kw) OR ((('on track' OR 'off track') NEAR/6 ('hill sachs' OR 'bone loss' OR 'shoulder' OR 'lesion*')):ti,ab,kw) |
18193 |
|
#2 |
'soft tissue'/exp AND 'procedures'/exp OR 'bankart repair'/exp OR 'putti-platt operation'/exp OR 'slap repair'/exp OR ((('bankart' OR 'putti-platt' OR 'slap' OR 'superior labr* anterior posterior') NEAR/3 ('operation*' OR 'procedure*' OR 'repair*' OR 'surger*' OR 'technique')):ti,ab,kw) OR 'capsulolabral repair':ti,ab,kw OR 'remplissage':ti,ab,kw OR 'soft tissue procedure*':ti,ab,kw |
60633 |
|
#3 |
'latarjet procedure'/exp OR 'eden-hybinette procedure'/exp OR 'bone graft'/exp OR 'bone transplantation'/exp OR ((('bon*' OR 'osseous') NEAR/3 ('graft*' OR 'autograft*' OR 'allograft*' OR 'augmentation' OR 'block*' OR 'transplant*')):ti,ab,kw) OR ((('bristow-latarjet' OR 'latarjet' OR 'latarjet-bristow' OR 'eden hybbinette' OR 'hybbinette eden') NEAR/3 ('operation*' OR 'procedure*' OR 'surger*' OR 'technique' OR 'stabilizat*' OR 'repair')):ti,ab,kw) |
143704 |
|
#4 |
#1 AND #2 AND #3 |
561 |
|
#5 |
#4 AND [2003-2024]/py NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) |
417 |
|
#6 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
987412 |
|
#7 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
3939234 |
|
#8 |
'major clinical study'/de OR 'clinical study'/de OR 'case control study'/de OR 'family study'/de OR 'longitudinal study'/de OR 'retrospective study'/de OR 'prospective study'/de OR 'comparative study'/de OR 'cohort analysis'/de OR ((cohort NEAR/1 (study OR studies)):ab,ti) OR (('case control' NEAR/1 (study OR studies)):ab,ti) OR (('follow up' NEAR/1 (study OR studies)):ab,ti) OR (observational NEAR/1 (study OR studies)) OR ((epidemiologic NEAR/1 (study OR studies)):ab,ti) OR (('cross sectional' NEAR/1 (study OR studies)):ab,ti) |
7991815 |
|
#9 |
'case control study'/de OR 'comparative study'/exp OR 'control group'/de OR 'controlled study'/de OR 'controlled clinical trial'/de OR 'crossover procedure'/de OR 'double blind procedure'/de OR 'phase 2 clinical trial'/de OR 'phase 3 clinical trial'/de OR 'phase 4 clinical trial'/de OR 'pretest posttest design'/de OR 'pretest posttest control group design'/de OR 'quasi experimental study'/de OR 'single blind procedure'/de OR 'triple blind procedure'/de OR (((control OR controlled) NEAR/6 trial):ti,ab,kw) OR (((control OR controlled) NEAR/6 (study OR studies)):ti,ab,kw) OR (((control OR controlled) NEAR/1 active):ti,ab,kw) OR 'open label*':ti,ab,kw OR (((double OR two OR three OR multi OR trial) NEAR/1 (arm OR arms)):ti,ab,kw) OR ((allocat* NEAR/10 (arm OR arms)):ti,ab,kw) OR placebo*:ti,ab,kw OR 'sham-control*':ti,ab,kw OR (((single OR double OR triple OR assessor) NEAR/1 (blind* OR masked)):ti,ab,kw) OR nonrandom*:ti,ab,kw OR 'non-random*':ti,ab,kw OR 'quasi-experiment*':ti,ab,kw OR crossover:ti,ab,kw OR 'cross over':ti,ab,kw OR 'parallel group*':ti,ab,kw OR 'factorial trial':ti,ab,kw OR ((phase NEAR/5 (study OR trial)):ti,ab,kw) OR ((case* NEAR/6 (matched OR control*)):ti,ab,kw) OR ((match* NEAR/6 (pair OR pairs OR cohort* OR control* OR group* OR healthy OR age OR sex OR gender OR patient* OR subject* OR participant*)):ti,ab,kw) OR ((propensity NEAR/6 (scor* OR match*)):ti,ab,kw) OR versus:ti OR vs:ti OR compar*:ti OR ((compar* NEAR/1 study):ti,ab,kw) OR (('major clinical study'/de OR 'clinical study'/de OR 'cohort analysis'/de OR 'observational study'/de OR 'cross-sectional study'/de OR 'multicenter study'/de OR 'correlational study'/de OR 'follow up'/de OR cohort*:ti,ab,kw OR 'follow up':ti,ab,kw OR followup:ti,ab,kw OR longitudinal*:ti,ab,kw OR prospective*:ti,ab,kw OR retrospective*:ti,ab,kw OR observational*:ti,ab,kw OR 'cross sectional*':ti,ab,kw OR cross?ectional*:ti,ab,kw OR multicent*:ti,ab,kw OR 'multi-cent*':ti,ab,kw OR consecutive*:ti,ab,kw) AND (group:ti,ab,kw OR groups:ti,ab,kw OR subgroup*:ti,ab,kw OR versus:ti,ab,kw OR vs:ti,ab,kw OR compar*:ti,ab,kw OR 'odds ratio*':ab OR 'relative odds':ab OR 'risk ratio*':ab OR 'relative risk*':ab OR 'rate ratio':ab OR aor:ab OR arr:ab OR rrr:ab OR ((('or' OR 'rr') NEAR/6 ci):ab))) |
14679817 |
|
#10 |
#5 AND #6 – SR’s |
42 |
|
#11 |
#5 AND #7 NOT #10 – RCT’s |
38 |
|
#12 |
#5 AND (#8 OR #9) NOT (#10 OR #11) – Observationele studies |
161 |
|
#13 |
#10 OR #11 OR #12 |
241 |
Ovid/Medline
|
# |
Searches |
Results |
|
1 |
exp Shoulder Dislocation/ or (exp Shoulder Joint/ and exp Joint Instability/) or ((shoulder or gleno-humeral* or humer* or scapulohumer*) adj3 (dislocat* or diastasis or instabil* or luxat* or subluxat*)).ti,ab,kf. or (shoulder and (bon* adj3 (resorption or loss or erosion or tear))).ti,ab,kf. or (exp Bankart Lesions/ or (bankart adj3 (fracture* or lesion* or tear*)).ti,ab,kf.) or (hill-sachs adj3 lesion*).ti,ab,kf. or ((on track or off track) adj6 (hill sachs or bone loss or shoulder or lesion*)).ti,ab,kf. |
13289 |
|
2 |
(((bankart or putti-platt or slap or superior labr* anterior posterior) adj3 (operation* or procedure* or repair* or surger* or technique)) or capsulolabral repair or remplissage or soft tissue procedure*).ti,ab,kf. |
2645 |
|
3 |
Bone Transplantation/ or ((bon* or osseous) adj3 (graft* or autograft* or allograft* or augmentation or block* or transplant*)).ti,ab,kf. or ((bristow-latarjet or latarjet or latarjet-bristow or eden hybbinette or hybbinette eden) adj3 (operation* or procedure* or surger* or technique or stabilizat*)).ti,ab,kf. |
102551 |
|
4 |
1 and 2 and 3 |
369 |
|
5 |
limit 4 to yr="2003 -2024" |
355 |
|
6 |
5 not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
330 |
|
7 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
714934 |
|
8 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2670491 |
|
9 |
Epidemiologic studies/ or case control studies/ or exp cohort studies/ or Controlled Before-After Studies/ or Case control.tw. or cohort.tw. or Cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or Longitudinal.tw. or Retrospective*.tw. or prospective*.tw. or consecutive*.tw. or Cross sectional.tw. or Cross-sectional studies/ or historically controlled study/ or interrupted time series analysis/ [Onder exp cohort studies vallen ook longitudinale, prospectieve en retrospectieve studies] |
4610598 |
|
10 |
Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) |
5583617 |
|
11 |
6 and 7 – SR’s |
36 |
|
12 |
(6 and 8) not 11 – RCT’s |
17 |
|
13 |
(6 and (9 or 10)) not (11 or 12) – Observationele studies |
151 |
|
14 |
11 or 12 or 13 |
204 |
Question 2a. and 2b.
Algemene informatie
|
Cluster/richtlijn: Richtlijn Schouderinstabiliteit - Module Artroscopisch versus open |
|
|
Uitgangsvraag/modules: Wat is de aanbevolen chirurgische ingreep (open of arthroscopisch) bij patiënten met traumatische anterieure instabiliteit en een indicatie voor operatieve behandeling? |
|
|
Database(s): Embase.com, Ovid/Medline |
Datum: 20 november 2024 |
|
Periode: geen restrictie |
Talen: geen restrictie |
|
Literatuurspecialist: Esther van der Bijl |
Rayyan review: https://new.rayyan.ai/reviews/1234657/overview |
|
BMI-zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Deduplication: voor het ontdubbelen is gebruik gemaakt van http://dedupendnote.nl/ |
|
|
Toelichting: Voor deze vraag is gezocht op de elementen schouderinstabiliteit EN (Arthroscopische Latarjet OF Open Bankart repair).
De sleutelartikelen worden gevonden met deze search.
In overleg worden in eerste instantie alleen de SR’s aangeboden in Rayyan. 23-01-2025: gerandomiseerde studies worden aangeboden in Rayyan 20-02-2025: observationeel onderzoek wordt gescreend met ASreview |
|
Zoekopbrengst - 20 november 2024
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SR |
259 |
255 |
305* |
|
RCT |
401 |
224 |
478 |
|
Observationele studies |
1545 |
1577 |
1868 |
|
Totaal |
2205 |
2056 |
2651 |
*in Rayyan
Zoekstrategie - 20 november 2024
Embase.com
|
No. |
Query |
Results |
|
#1 |
'shoulder dislocation'/exp OR 'recurrent shoulder dislocation'/exp OR 'bankart lesion'/exp OR ('shoulder'/exp AND ('dislocation'/de OR 'recurrent dislocation'/exp OR 'subluxation'/exp OR 'joint dislocation'/exp OR 'bone erosion'/exp OR 'joint instability'/de)) OR ((('shoulder*' OR 'gleno-humer*' OR 'glenoid*' OR 'humer*' OR 'scapulohumer*' OR 'glenohumer*') NEAR/3 ('dislocat*' OR 'diastasis' OR 'instabil*' OR 'luxat*' OR 'subluxat*' OR 'defect*')):ti,ab,kw) OR (('shoulder*':ti,ab,kw OR glenoid*:ti,ab,kw OR 'gleno-humer*':ti,ab,kw OR 'humer*':ti,ab,kw OR 'scapulohumer*':ti,ab,kw OR 'glenohumer*':ti,ab,kw) AND (('bon*' NEAR/3 ('resorption*' OR 'loss*' OR 'erosion*')):ti,ab,kw)) OR ((('bankart' OR 'hill-sachs') NEAR/3 ('fracture*' OR 'lesion*' OR 'tear*')):ti,ab,kw) OR ((('on track' OR 'off track') NEAR/3 ('hill sachs' OR 'bone loss*' OR 'shoulder*' OR 'lesion*')):ti,ab,kw) |
21034 |
|
#2 |
'latarjet procedure'/exp OR 'arthroscopic latarjet procedure'/exp OR 'eden-hybinette procedure'/exp OR 'bone graft'/exp OR 'bone transplantation'/exp OR ((('bon*' OR 'osseous') NEAR/3 ('graft*' OR 'autograft*' OR 'allograft*' OR 'augmentation*' OR 'block*' OR 'transplant*')):ti,ab,kw) OR ((('bristow-latarjet' OR 'latarjet' OR 'latarjet-bristow' OR 'eden hybbinette' OR 'hybbinette eden') NEAR/3 ('operat*' OR 'procedure*' OR 'surger*' OR 'technique*' OR 'stabilizat*' OR stabilisat* OR 'repair*' OR surgic*)):ti,ab,kw) OR ((arthroscopic* NEAR/7 latarjet):ti,ab,kw) OR ((arthroscopic* NEAR/3 (stabilizat* OR stabilisat*) NEAR/3 surger*):ti,ab,kw) |
149011 |
|
#3 |
'soft tissue'/exp AND 'procedures'/exp OR 'bankart repair'/exp OR 'open bankart repair'/exp OR 'putti-platt operation'/exp OR 'slap repair'/exp OR ((('bankart' OR 'putti-platt' OR 'slap' OR 'superior labr* anterior posterior') NEAR/3 ('operat*' OR 'procedure*' OR 'repair*' OR 'surger*' OR 'technique*' OR surgic* OR 'stabilizat*')):ti,ab,kw) OR ((open NEAR/3 bankart):ti,ab,kw) OR 'capsulolabral repair*':ti,ab,kw OR 'remplissage':ti,ab,kw OR (('soft tissue*' NEAR/3 procedure*):ti,ab,kw) |
64673 |
|
#4 |
#2 OR #3 |
211043 |
|
#5 |
#1 AND #4 |
4605 |
|
#6 |
#5 NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) |
3720 |
|
#7 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
1078783 |
|
#8 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
4145676 |
|
#9 |
'major clinical study'/de OR 'clinical study'/de OR 'case control study'/de OR 'family study'/de OR 'longitudinal study'/de OR 'retrospective study'/de OR 'prospective study'/de OR 'comparative study'/de OR 'cohort analysis'/de OR ((cohort NEAR/1 (study OR studies)):ab,ti) OR (('case control' NEAR/1 (study OR studies)):ab,ti) OR (('follow up' NEAR/1 (study OR studies)):ab,ti) OR (observational NEAR/1 (study OR studies)) OR ((epidemiologic NEAR/1 (study OR studies)):ab,ti) OR (('cross sectional' NEAR/1 (study OR studies)):ab,ti) |
8498857 |
|
#10 |
'case control study'/de OR 'comparative study'/exp OR 'control group'/de OR 'controlled study'/de OR 'controlled clinical trial'/de OR 'crossover procedure'/de OR 'double blind procedure'/de OR 'phase 2 clinical trial'/de OR 'phase 3 clinical trial'/de OR 'phase 4 clinical trial'/de OR 'pretest posttest design'/de OR 'pretest posttest control group design'/de OR 'quasi experimental study'/de OR 'single blind procedure'/de OR 'triple blind procedure'/de OR (((control OR controlled) NEAR/6 trial):ti,ab,kw) OR (((control OR controlled) NEAR/6 (study OR studies)):ti,ab,kw) OR (((control OR controlled) NEAR/1 active):ti,ab,kw) OR 'open label*':ti,ab,kw OR (((double OR two OR three OR multi OR trial) NEAR/1 (arm OR arms)):ti,ab,kw) OR ((allocat* NEAR/10 (arm OR arms)):ti,ab,kw) OR placebo*:ti,ab,kw OR 'sham-control*':ti,ab,kw OR (((single OR double OR triple OR assessor) NEAR/1 (blind* OR masked)):ti,ab,kw) OR nonrandom*:ti,ab,kw OR 'non-random*':ti,ab,kw OR 'quasi-experiment*':ti,ab,kw OR crossover:ti,ab,kw OR 'cross over':ti,ab,kw OR 'parallel group*':ti,ab,kw OR 'factorial trial':ti,ab,kw OR ((phase NEAR/5 (study OR trial)):ti,ab,kw) OR ((case* NEAR/6 (matched OR control*)):ti,ab,kw) OR ((match* NEAR/6 (pair OR pairs OR cohort* OR control* OR group* OR healthy OR age OR sex OR gender OR patient* OR subject* OR participant*)):ti,ab,kw) OR ((propensity NEAR/6 (scor* OR match*)):ti,ab,kw) OR versus:ti OR vs:ti OR compar*:ti OR ((compar* NEAR/1 study):ti,ab,kw) OR (('major clinical study'/de OR 'clinical study'/de OR 'cohort analysis'/de OR 'observational study'/de OR 'cross-sectional study'/de OR 'multicenter study'/de OR 'correlational study'/de OR 'follow up'/de OR cohort*:ti,ab,kw OR 'follow up':ti,ab,kw OR followup:ti,ab,kw OR longitudinal*:ti,ab,kw OR prospective*:ti,ab,kw OR retrospective*:ti,ab,kw OR observational*:ti,ab,kw OR 'cross sectional*':ti,ab,kw OR cross?ectional*:ti,ab,kw OR multicent*:ti,ab,kw OR 'multi-cent*':ti,ab,kw OR consecutive*:ti,ab,kw) AND (group:ti,ab,kw OR groups:ti,ab,kw OR subgroup*:ti,ab,kw OR versus:ti,ab,kw OR vs:ti,ab,kw OR compar*:ti,ab,kw OR 'odds ratio*':ab OR 'relative odds':ab OR 'risk ratio*':ab OR 'relative risk*':ab OR 'rate ratio':ab OR aor:ab OR arr:ab OR rrr:ab OR ((('or' OR 'rr') NEAR/6 ci):ab))) |
15547564 |
|
#11 |
#6 AND #7 - SR |
259 |
|
#12 |
#6 AND #8 NOT #11 - RCT |
401 |
|
#13 |
#6 AND (#9 OR #10) NOT (#11 OR #12) - Observationeel |
1545 |
|
#14 |
#11 OR #12 OR #13 - Totaal |
2205 |
Ovid/Medline
|
# |
Searches |
Results |
|
1 |
exp Shoulder Dislocation/ or exp Bankart Lesions/ or (exp Shoulder Joint/ and exp Joint Instability/) or ((shoulder* or gleno-humer* or glenoid* or humer* or scapulohumer* or glenohumer*) adj3 (dislocat* or diastasis or instabil* or luxat* or subluxat* or defect*)).ti,ab,kf. or ((shoulder* or glenoid* or gleno-humer* or humer* or scapulohumer* or glenohumer*) and (bon* adj3 (resorption* or loss* or erosion*))).ti,ab,kf. or ((bankart or hill-sachs) adj3 (fracture* or lesion* or tear*)).ti,ab,kf. or ((on track or off track) adj3 (hill sachs or bone loss* or shoulder* or lesion*)).ti,ab,kf. |
15381 |
|
2 |
(exp Arthroscopy/ and (exp General Surgery/ or exp Orthopedics/)) or Bone Transplantation/ or ((bon* or osseous) adj3 (graft* or autograft* or allograft* or augmentation* or block* or transplant*)).ti,ab,kf. or ((bristow-latarjet or latarjet or latarjet-bristow or eden hybbinette or hybbinette eden) adj3 (operat* or procedure* or surger* or technique* or stabilizat* or stabilisat* or repair* or surgic*)).ti,ab,kf. or (arthroscopic* adj7 latarjet).ti,ab,kf. or (arthroscopic* adj3 (stabilizat* or stabilisat*) adj3 surger*).ti,ab,kf. |
106075 |
|
3 |
(((bankart or putti-platt or slap or superior labr* anterior posterior) adj3 (operat* or procedure* or repair* or surger* or technique* or surgic* or stabilizat*)) or (open adj3 bankart) or capsulolabral repair* or remplissage or (soft tissue* adj3 procedure*)).ti,ab,kf. |
3896 |
|
4 |
2 or 3 |
109351 |
|
5 |
1 and 4 |
3416 |
|
6 |
5 not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
3258 |
|
7 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
791524 |
|
8 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2808360 |
|
9 |
Epidemiologic studies/ or case control studies/ or exp cohort studies/ or Controlled Before-After Studies/ or Case control.tw. or cohort.tw. or Cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or Longitudinal.tw. or Retrospective*.tw. or prospective*.tw. or consecutive*.tw. or Cross sectional.tw. or Cross-sectional studies/ or historically controlled study/ or interrupted time series analysis/ [Onder exp cohort studies vallen ook longitudinale, prospectieve en retrospectieve studies] |
4887182 |
|
10 |
Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) |
5840342 |
|
11 |
6 and 7 - SR |
255 |
|
12 |
(6 and 8) not 11 - RCT |
224 |
|
13 |
(6 and (9 or 10)) not (11 or 12) - Observationeel |
1577 |
|
14 |
11 or 12 or 13 - Totaal |
2056 |
Question 3
Algemene informatie
|
Cluster/richtlijn: Schouderinstabiliteit Module 6 en 7 - Operatieve behandeling 1 en 2 |
|
|
Uitgangsvraag/modules: Wat is de indicatie voor een operatieve behandeling bij patiënten met schouderinstabiliteit? Wat is de indicatie voor een operatieve behandeling bij patiënten met recidief schouderinstabiliteit na eerdere operatieve behandeling? |
|
|
Database(s): Embase.com, Ovid/Medline |
Datum: 20-12-2023 |
|
Periode: vanaf 2003 |
Talen: geen restrictie |
|
Literatuurspecialist: Esther van der Bijl |
Rayyan review: https://rayyan.ai/reviews/879934 |
|
BMI-zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting: Voor deze vraag is gezocht op de elementen:
Vanwege de grote opbrengst is in overleg gezocht met de P AND I AND C.
→ Het sleutelartikel PMID 33172578 wordt niet gevonden met deze search. Het valt uit op studiedesign. |
|
|
Te gebruiken voor richtlijntekst: In de databases Embase.com en Ovid/Medline is op 20-12-2023 systematisch gezocht naar systematische reviews, RCTs en observationele studies over wekedelen procedures vergeleken met een ossale procedures voor patiënten met schouder instabiliteit. De literatuurzoekactie leverde 274 unieke treffers op. |
|
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SR |
42 |
36 |
46 |
|
RCT |
38 |
17 |
44 |
|
Observationeel |
161 |
151 |
185 |
|
Totaal |
241 |
204 |
275* |
*in Rayyan
Zoekstrategie - 20 december 2023
Embase.com
|
No. |
Query |
Results |
|
#1 |
'shoulder dislocation'/exp OR 'recurrent shoulder dislocation'/exp OR ('shoulder'/exp AND ('dislocation'/de OR 'recurrent dislocation'/exp OR 'subluxation'/exp OR 'joint dislocation'/exp OR 'bone erosion'/exp OR 'joint instability'/de)) OR ((('shoulder' OR 'gleno-humeral*' OR 'humer*' OR 'scapulohumer*') NEAR/3 ('dislocat*' OR 'diastasis' OR 'instabil*' OR 'luxat*' OR 'subluxat*')):ti,ab,kw) OR ('shoulder':ti,ab,kw AND (('bon*' NEAR/3 ('resorption' OR 'loss' OR 'erosion')):ti,ab,kw)) OR 'bankart lesion'/exp OR (('bankart' NEAR/3 ('fracture*' OR 'lesion*' OR 'tear*')):ti,ab,kw) OR (('hill-sachs' NEAR/3 'lesion*'):ti,ab,kw) OR ((('on track' OR 'off track') NEAR/6 ('hill sachs' OR 'bone loss' OR 'shoulder' OR 'lesion*')):ti,ab,kw) |
18193 |
|
#2 |
'soft tissue'/exp AND 'procedures'/exp OR 'bankart repair'/exp OR 'putti-platt operation'/exp OR 'slap repair'/exp OR ((('bankart' OR 'putti-platt' OR 'slap' OR 'superior labr* anterior posterior') NEAR/3 ('operation*' OR 'procedure*' OR 'repair*' OR 'surger*' OR 'technique')):ti,ab,kw) OR 'capsulolabral repair':ti,ab,kw OR 'remplissage':ti,ab,kw OR 'soft tissue procedure*':ti,ab,kw |
60633 |
|
#3 |
'latarjet procedure'/exp OR 'eden-hybinette procedure'/exp OR 'bone graft'/exp OR 'bone transplantation'/exp OR ((('bon*' OR 'osseous') NEAR/3 ('graft*' OR 'autograft*' OR 'allograft*' OR 'augmentation' OR 'block*' OR 'transplant*')):ti,ab,kw) OR ((('bristow-latarjet' OR 'latarjet' OR 'latarjet-bristow' OR 'eden hybbinette' OR 'hybbinette eden') NEAR/3 ('operation*' OR 'procedure*' OR 'surger*' OR 'technique' OR 'stabilizat*' OR 'repair')):ti,ab,kw) |
143704 |
|
#4 |
#1 AND #2 AND #3 |
561 |
|
#5 |
#4 AND [2003-2024]/py NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) |
417 |
|
#6 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
987412 |
|
#7 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
3939234 |
|
#8 |
'major clinical study'/de OR 'clinical study'/de OR 'case control study'/de OR 'family study'/de OR 'longitudinal study'/de OR 'retrospective study'/de OR 'prospective study'/de OR 'comparative study'/de OR 'cohort analysis'/de OR ((cohort NEAR/1 (study OR studies)):ab,ti) OR (('case control' NEAR/1 (study OR studies)):ab,ti) OR (('follow up' NEAR/1 (study OR studies)):ab,ti) OR (observational NEAR/1 (study OR studies)) OR ((epidemiologic NEAR/1 (study OR studies)):ab,ti) OR (('cross sectional' NEAR/1 (study OR studies)):ab,ti) |
7991815 |
|
#9 |
'case control study'/de OR 'comparative study'/exp OR 'control group'/de OR 'controlled study'/de OR 'controlled clinical trial'/de OR 'crossover procedure'/de OR 'double blind procedure'/de OR 'phase 2 clinical trial'/de OR 'phase 3 clinical trial'/de OR 'phase 4 clinical trial'/de OR 'pretest posttest design'/de OR 'pretest posttest control group design'/de OR 'quasi experimental study'/de OR 'single blind procedure'/de OR 'triple blind procedure'/de OR (((control OR controlled) NEAR/6 trial):ti,ab,kw) OR (((control OR controlled) NEAR/6 (study OR studies)):ti,ab,kw) OR (((control OR controlled) NEAR/1 active):ti,ab,kw) OR 'open label*':ti,ab,kw OR (((double OR two OR three OR multi OR trial) NEAR/1 (arm OR arms)):ti,ab,kw) OR ((allocat* NEAR/10 (arm OR arms)):ti,ab,kw) OR placebo*:ti,ab,kw OR 'sham-control*':ti,ab,kw OR (((single OR double OR triple OR assessor) NEAR/1 (blind* OR masked)):ti,ab,kw) OR nonrandom*:ti,ab,kw OR 'non-random*':ti,ab,kw OR 'quasi-experiment*':ti,ab,kw OR crossover:ti,ab,kw OR 'cross over':ti,ab,kw OR 'parallel group*':ti,ab,kw OR 'factorial trial':ti,ab,kw OR ((phase NEAR/5 (study OR trial)):ti,ab,kw) OR ((case* NEAR/6 (matched OR control*)):ti,ab,kw) OR ((match* NEAR/6 (pair OR pairs OR cohort* OR control* OR group* OR healthy OR age OR sex OR gender OR patient* OR subject* OR participant*)):ti,ab,kw) OR ((propensity NEAR/6 (scor* OR match*)):ti,ab,kw) OR versus:ti OR vs:ti OR compar*:ti OR ((compar* NEAR/1 study):ti,ab,kw) OR (('major clinical study'/de OR 'clinical study'/de OR 'cohort analysis'/de OR 'observational study'/de OR 'cross-sectional study'/de OR 'multicenter study'/de OR 'correlational study'/de OR 'follow up'/de OR cohort*:ti,ab,kw OR 'follow up':ti,ab,kw OR followup:ti,ab,kw OR longitudinal*:ti,ab,kw OR prospective*:ti,ab,kw OR retrospective*:ti,ab,kw OR observational*:ti,ab,kw OR 'cross sectional*':ti,ab,kw OR cross?ectional*:ti,ab,kw OR multicent*:ti,ab,kw OR 'multi-cent*':ti,ab,kw OR consecutive*:ti,ab,kw) AND (group:ti,ab,kw OR groups:ti,ab,kw OR subgroup*:ti,ab,kw OR versus:ti,ab,kw OR vs:ti,ab,kw OR compar*:ti,ab,kw OR 'odds ratio*':ab OR 'relative odds':ab OR 'risk ratio*':ab OR 'relative risk*':ab OR 'rate ratio':ab OR aor:ab OR arr:ab OR rrr:ab OR ((('or' OR 'rr') NEAR/6 ci):ab))) |
14679817 |
|
#10 |
#5 AND #6 – SR’s |
42 |
|
#11 |
#5 AND #7 NOT #10 – RCT’s |
38 |
|
#12 |
#5 AND (#8 OR #9) NOT (#10 OR #11) – Observationele studies |
161 |
|
#13 |
#10 OR #11 OR #12 |
241 |
Ovid/Medline
|
# |
Searches |
Results |
|
1 |
exp Shoulder Dislocation/ or (exp Shoulder Joint/ and exp Joint Instability/) or ((shoulder or gleno-humeral* or humer* or scapulohumer*) adj3 (dislocat* or diastasis or instabil* or luxat* or subluxat*)).ti,ab,kf. or (shoulder and (bon* adj3 (resorption or loss or erosion or tear))).ti,ab,kf. or (exp Bankart Lesions/ or (bankart adj3 (fracture* or lesion* or tear*)).ti,ab,kf.) or (hill-sachs adj3 lesion*).ti,ab,kf. or ((on track or off track) adj6 (hill sachs or bone loss or shoulder or lesion*)).ti,ab,kf. |
13289 |
|
2 |
(((bankart or putti-platt or slap or superior labr* anterior posterior) adj3 (operation* or procedure* or repair* or surger* or technique)) or capsulolabral repair or remplissage or soft tissue procedure*).ti,ab,kf. |
2645 |
|
3 |
Bone Transplantation/ or ((bon* or osseous) adj3 (graft* or autograft* or allograft* or augmentation or block* or transplant*)).ti,ab,kf. or ((bristow-latarjet or latarjet or latarjet-bristow or eden hybbinette or hybbinette eden) adj3 (operation* or procedure* or surger* or technique or stabilizat*)).ti,ab,kf. |
102551 |
|
4 |
1 and 2 and 3 |
369 |
|
5 |
limit 4 to yr="2003 -2024" |
355 |
|
6 |
5 not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
330 |
|
7 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
714934 |
|
8 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2670491 |
|
9 |
Epidemiologic studies/ or case control studies/ or exp cohort studies/ or Controlled Before-After Studies/ or Case control.tw. or cohort.tw. or Cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or Longitudinal.tw. or Retrospective*.tw. or prospective*.tw. or consecutive*.tw. or Cross sectional.tw. or Cross-sectional studies/ or historically controlled study/ or interrupted time series analysis/ [Onder exp cohort studies vallen ook longitudinale, prospectieve en retrospectieve studies] |
4610598 |
|
10 |
Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) |
5583617 |
|
11 |
6 and 7 – SR’s |
36 |
|
12 |
(6 and 8) not 11 – RCT’s |
17 |
|
13 |
(6 and (9 or 10)) not (11 or 12) – Observationele studies |
151 |
|
14 |
11 or 12 or 13 |
204 |