Fixatie na een ribfractuur
Uitgangsvraag
Wat is de plaats van fixatie van de ribben na een ribfractuur?
Aanbeveling
Overweeg fixatie bij een fladderthorax om de kans op pneumonie mogelijk te verkleinen.
Wees terughoudend met fixatie bij multipele ribfracturen. Overweeg fixatie van de ribben bij patiënten die niet ontwend kunnen worden van mechanische ventilatie ondanks adequate pijnstilling.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Er is literatuuronderzoek uitgevoerd naar de meerwaarde van rib fixatie ten opzichte van niet fixeren van de rib bij patiënten met multipele ribfracturen en patiënten met een fladderthorax. Er werden vijf studies geïncludeerd in de literatuuranalyse: één systematische review, waarin drie individuele gerandomiseerde studies aan de PICO voldeden en vier losse gerandomiseerde studies. De vier gerandomiseerde studies verschenen na de laatste searchdatum van de geïncludeerde systematische review en werden in de literatuuranalyse toegevoegd aan de drie gerandomiseerde studies uit de systematische review van Cataneo (2015). Mortaliteit werd als cruciale uitkomstmaat gedefinieerd. Pneumonie, vervormingen van de thorax, opname duur in het ziekenhuis, opnameduur op de intensive care, wondinfecties, technisch falen van de procedure, de duur van mechanische ventilatie, pijn, kwaliteit van leven en kosten werden als belangrijke uitkomstmaten voor klinische besluitvorming gedefinieerd. Waar mogelijk werden de resultaten van alle uitkomstmaten separaat geanalyseerd voor patiënten met (multipele) ribfracturen en voor patiënten met een fladderthorax.
Er werd geen klinisch relevant verschil gevonden in mortaliteit tussen het wel en niet fixeren van de ribfracturen, zowel bij patiënten met een fladderthorax als bij patiënten met multipele ribfracturen. Voor de uitkomstmaten pneumonie, opnameduur op de intensive care, de duur van mechanische ventilatie en pijn werden echter wel voor beide patiëntengroepen een klinisch relevant verschil gevonden in het voordeel van het fixeren van de rib. Voor wondinfecties en vervormingen van de thorax werden de resultaten beschrijvend weergegeven, omdat patiënten die werden toegewezen aan een niet operatieve fixatie van de ribben bij voorbaat geen risico lopen op wondinfecties of vervormingen van de borstkas. Het heeft zodoende geen meerwaarde om deze uitkomst te vergelijken tussen beiden interventies. Alleen voor pneumonie werd de bewijskracht gegradeerd op ‘laag GRADE’. Alle andere uitkomstmaten werden gegradeerd op ‘zeer laag GRADE’, waardoor het onduidelijk is of het gevonden effect het daadwerkelijke effect juist weerspiegelt. Het is belangrijk om hier onderzoek naar te doen.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Met betrekking tot twee belangrijke uitkomsten voor patiënten namelijk kwaliteit van leven en pijn werden geen klinische relevante verschillen gevonden tussen wel of niet fixeren van ribfracturen. Ook met betrekking tot wellicht blijvende thoraxdeformiteit kon geen voordeel van fixatie en daarmee (partiele) correctie van deformiteit worden aangetoond. Opgemerkt dient te worden dat de patiënt in de fase na het ongeval vooral is gericht op adequate pijnstilling en herstel van onbelemmerde ademhaling. Zie hiervoor module Pijnstilling van deze richtlijn, waarin de waarde van locoregionale pijnstillingmethoden bij patiënten met pijn na multipele ribfracturen na een gediagnosticeerd thoracaal letsel werd onderzocht. Problemen die later kunnen optreden zijn onder andere een grote deformiteit, cosmetische bezwaren of risico van ontstaan van non-unions of malunions van ribfracturen. Het is voor patiënten belangrijk dat ook deze problemen besproken worden bij de afweging om te fixeren of af te wachten. Het is voor patiënten van belang dat de voor- en nadelen volgens de principes van samen beslissen worden besproken en ook aandacht wordt besteed aan deze problematiek die later kan ontstaan.
Kosten (middelenbeslag)
Omdat het thoraxletsel het derde letsel is qua voorkomen al dan niet in combinatie met andere letsels, is het reëel te veronderstellen dat de absolute daarmee gepaard gaande kosten hoog zullen zijn voor de samenleving (Peek, 2022). Een Nederlandse studie naar de geassocieerde directe- en indirecte medische kosten van rib fixatie toonde €6.785,- directe kosten per patiënt en €22.886,- indirecte kosten per patiënt (Prins, 2022). Een Amerikaanse studie van Choi (2021) die de kosteneffectiviteit van ribfixatie bij patiënten met een fladder thorax versus geen fladder thorax evalueerde, toonde alleen kosteneffectiviteit in de gestabiliseerde fladderthorax groep onder de 65 jaar. Een retrospectieve studie van Bauman (2023) toonde een dekkingsbijdrage van €1045,- in de chirurgisch gestabiliseerde ribfracturen groep. Echter een beslissingsanalysemodel dat de kosten en uitkomsten van operatieve fixatie versus niet-operatieve behandeling voor ribfracturen van Swart (2017) vergeleek, toonde dat operatieve fixatie gepaard ging met hogere kosten dan niet-operatieve behandeling. Er zijn tot op heden geen kwalitatief goede gerandomiseerde vergelijkende kosteneffectiviteitsstudies op dit onderwerp.
Daar er tot op heden in de gehele groep van patiënten met ribfracturen geen uitgesproken voordeel met betrekking tot ribfixatie versus geen ribfixatie aantoonbaar is en ook niet in de duur van ziekenhuisopname en opnameduur op de IC, lijken de kosten bij het verrichten van ribfixatie verhoogd. Daarnaast komt technisch falen en zo nodige re-interventies alleen in de operatieve groep voor en deze zijn kostenverhogend.
Duurzaamheid
Een operatie heeft een grotere negatieve impact op het milieu in vergelijking met conservatieve behandeling. Vanuit dit oogpunt is het dus beter om af te zien van ribfixatie. Indien er voor operatie gekozen wordt, besteed dan aandacht aan het type operatie- en afdekmateriaal en aan het reduceren van het gebruik van disposables.
Aanvaardbaarheid, haalbaarheid en implementatie
Tot op heden is er onvoldoende bekend met betrekking tot de meerwaarde van een chirurgische ribfixatie ten opzichte van geen fixatie van de ribfracturen. Indien toch bij uitzondering of in studieverband wordt gekozen bij een patiënt een ribfractuur fixatie te verrichten, dan is dit op basis van bovengenoemde onderzoeken een relatief veilige operatie met een lage technische faalkans en infectiekans. Met betrekking tot toegankelijkheid en kennis- en kunde niveau, zijn er door de regionale samenwerking in Nederland tussen traumacentra, altijd locaties waar deze interventies door traumachirurgen kunnen worden verricht.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
De verrichte evaluatie van de plaats van ribfixatie na ribfracturen toont slechts ‘lage’ en ‘zeer lage’ bewijskracht op de belangrijkste beslissing karakteristieken. Toch lijkt er een gering verschil te zijn tussen het al dan niet aanwezig zijn van een klinisch relevante fladderthorax, welke de zuurstofopname capaciteit van patiënt beïnvloed, multipele ribfracturen zonder en met behoefte aan mechanische ondersteuning en enkelvoudige ribfracturen of niet verplaatste ribfracturen.
Voor de groep van de enkelvoudige ribfracturen of enkele niet verplaatste ribfracturen is geen duidelijk voordeel van ribfixatie aantoonbaar. Voor de groep met een fladderthorax lijkt er volgens dewerkgroep een gering voordeel te zijn in de studies met betrekking tot lagere incidentie van pneumonie, duur van ziekenhuisopname, pijn, vermijden van tracheostoma en borstkas deformiteit. De groep patiënten met multipele ribfracturen lijkt dit voordeel in nog lagere mate te hebben. Behalve als er geen ontwenning van mechanische ventilatie bij adequate pijnstilling of ernstige thorax deformiteit mogelijk is, ziet de werkgroep geen generale indicatie voor ribfixatie in deze specifieke populatie. Wel wil de werkgroep erop wijzen dat meerdere studies die deze vraag kunnen beantwoorden zijn verschenen of nog lopende zijn na de datum van de zoektocht die de basis vormt voor deze richtlijn.
Een chirurgische interventie draagt altijd risico’s bij zich, zo ook bij rib fixatie chirurgie. Technisch falen van materiaal of operateur is altijd mogelijk, net als het ontstaan van (wond)infecties. Bij de keuze voorafgaand aan het verrichten van een ribfixatie dienen daarom zorgvuldig de mogelijke contra-indicaties worden overwogen. Tevens dient de timing van interventie gebalanceerd te worden ten aanzien van eventuele andere letsels.
Onderbouwing
Achtergrond
Er is nog onvoldoende duidelijkheid over de plaats van operatieve fixatie in de behandeling van de verschillende vormen van ribfracturen na trauma. Ribfracturen zijn veel voorkomende fracturen. Ribfracturen worden veelal conservatief behandeld. Recente ontwikkelingen in fixatie technieken hebben in de laatste jaren geleid tot toegenomen interesse in de mogelijkheden tot fixatie van ribfracturen. Helaas is er tot heden onvoldoende bekend met betrekking tot de meerwaarde van een chirurgische ribfixatie ten opzichte van geen fixatie van ribfracturen, behoudens bij patiënten met een klinisch relevante fladderthorax waarbij fixatie enige meerwaarde lijkt te hebben (Leinicke, 2013). De fladderthorax wordt in deze module gedefinieerd als het letsel waarbij radiologisch drie of meer aaneengesloten ribben op ten minste twee plaatsen gebroken zijn. Niet elke radiologische fladderthorax is klinisch zichtbaar en/of klinisch relevant. Bij een klinisch zichtbare fladderthorax zorgen deze verwondingen ervoor dat het aangedane deel van de borstkaswand onafhankelijk van de rest van de borstkaswand beweegt. Een fladderthorax kan dan ook een aanzienlijke verstoring van de ademhalingsfysiologie veroorzaken (LNAZ, registratiehandleiding LTR-versie 2.0).
Conclusies / Summary of Findings
Mortality
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on mortality in comparison with no rib fixation in patients with flail chest trauma and in patients with non-flail chest trauma.
Sources: Cataneo, 2015; Granetzny, 2005; Marasco, 2013; Tanaka, 2002; Liu, 2019; Marasco, 2022; Meyer, 2023 |
Pneumonia
|
Low GRADE |
Rib fixation may result in a lower incidence of pneumonia in comparison with no rib fixation in patients with flail chest trauma.
Due to a lack of information in the included studies, it was not possible to draw a conclusion for the effect of rib fixation on pneumonia in patients with non-flail chest trauma.
Sources: Cataneo, 2015; Granetzny, 2005; Marasco, 2013; Tanaka, 2002; Liu, 2019 |
Wound infections
|
No GRADE |
It was not possible to conclude the predefined outcome wound infections in patients with flail chest trauma and non-flail trauma. Wound infection depends on patient selection for no rib fixation treatment.
Sources: Cataneo, 2015; Granetzny, 2005; Meyer, 2023 |
Chest deformity
|
No GRADE |
It was not possible to conclude the predefined outcome chest deformity in patients with flail chest trauma and non-flail trauma. Chest deformity depends on patient selection for no rib fixation treatment.
Sources: Cataneo, 2015; Granetzny, 2005; Liu, 2019 |
Tracheostomy
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on the need for a tracheostomy in comparison with no rib fixation in patients with flail chest trauma.
Due to a lack of information in the included studies, it was not possible to draw a conclusion for the effect of rib fixation on the need for tracheostomy in patients with non-flail chest trauma.
Sources: Cataneo, 2015; Marasco, 2013; Liu, 2019 |
Length of hospital stay
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on the length of hospital stay in comparison with no rib fixation in patients with flail chest trauma and in patients with non-flail chest trauma.
Sources: Liu, 2019; Marasco, 2022; Meyer, 2023 |
Length of ICU stay
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on the length of ICU stay in comparison with no rib fixation in patients with flail chest trauma and in patients with non-flail chest trauma.
Sources: Cataneo, 2015; Granetzny, 2005; Tanaka, 2002; Liu, 2019; Marasco, 2022 |
Technical failures
|
No GRADE |
Due to an absence of information in the included studies, it was not possible to draw any conclusions regarding the outcome technical success in patients with flail chest trauma or patients with non-flail chest trauma.
Source: - |
Duration of mechanical ventilation
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on the duration of mechanical ventilation in comparison with no rib fixation in patients with flail chest trauma.
Due to a lack of information in the included studies, it was not possible to draw a conclusion for the effect of rib fixation on the duration of mechanical ventilation in patients with non-flail chest trauma.
Sources: Cataneo, 2015; Granetzny, 2005; Tanaka, 2002; Liu, 2019 |
Pain
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on pain in comparison with no rib fixation in patients with flail chest trauma and in patients with non-flail chest trauma.
Sources: Liu, 2019; Marasco, 2022; Meyer, 2023; Pieracci, 2020 |
Quality of life
|
Very low GRADE |
The evidence is very uncertain about the effect of rib fixation on quality of life in comparison with no rib fixation in patients with non-flail chest trauma.
Due to a lack of information in the included studies, it was not possible to draw a conclusion for the effect of rib fixation on the requirement of mechanical ventilation in patients with chest trauma.
Sources: Marasco, 2022; Pieracci, 2020 |
Costs
|
No GRADE |
Due to an absence of information in the included studies, it was not possible to draw any conclusions regarding the outcome costs in patients with flail chest trauma and patients with non-flail chest trauma.
Source: - |
Samenvatting literatuur
Description of studies
The systematic (Cochrane) review of Cataneo (2015) aimed to evaluate the effectiveness and safety of surgical stabilization compared with clinical management for people with flail chest. Cataneo (2015) searched the electronic databases of the Cochrane Injuries Group Specialised Register, Cochrane Central Register of Controlled Trials, Ovid Medline, Embase, CINAHL, ISI Web of Science, clinicaltrials.gov, and International Clinical Trials Registery Platform up to the 12th of May 2014. Cataneo (2015) included the following studies: (1) randomized controlled trials, using a parallel design, comparing surgical stabilization (any type) with clinical management; (2) adult patients or children with flail chest; (3) any type of surgical intervention to stabilize flail chest with clinical management. Clinical management included any type of chest wall stabilization without surgical intervention such as straps or bags and any type of ventilatory assistance. In total, three randomized controlled trials comprising 123 patients were included (Granetzny, 2005; Marasco, 2013; Tanaka, 2002). Granetzny (2005) compared surgical fixation of fractured ribs with stainless steel wire or Kirschner wires, or both after 24 to 36 hours of intensive care unit admission with conservative treatment using strapping and packing in the form of dressing and fixing with an adhesive bandage, which was put adhesively to the flail segment within five centimetre anterior and posterior to the flail segment and one rib above and below it. This adhesive plaster was put in place for at least seven to ten days. Until the participants were operated upon, they were given the same treatment as the conservatively treated participants. In the study of Marasco (2013), only rib fractures between the levels of ribs three and ten were fixed. Ribs fractured more than once were usually addressed by fixing one fracture per rib, converting a flail segment to simple fractured ribs. Ribs with a single fracture were not fixed unless there was gross deformity mandating intervention. Anterior and lateral rib fractures were preferentially fixed over posterior rib fractures. This procedure was compared with non-surgical management (mechanical ventilation). Tanaka (2002) compared surgical stabilization with Internal pneumatic stabilization but did not further specify both procedures. The length of follow-up varied between the three studies. Granetzny (2005) reported outcomes at two months follow-up, Maresco (2005) at six months follow-up, and Tanaka (2002) at twelve months follow-up. The risk of bias was assessed with The Cochrane Collaboration’s ‘Risk of bias’ tool. The reported outcomes were mortality, chest wall deformity, pain, wound infection, pneumonia, tracheostomy, duration of mechanical ventilation, length of stay on the intensive care unit, and length of stay in the hospital.
The randomized controlled trial of Liu (2019) investigated the effect of surgical treatment compared with non-surgical treatment of flail chest in patients with severe polytrauma. Liu (2019) included patients with polytrauma with injury severity score (ISS) of sixteen or more. Exclusion criteria included age younger than 18 years, death within 48 hours, cervical spinal cord injury with paralysis, severe head injury, uncorrected coagulopathy, and pre-existing cardiac or pulmonary conditions. In total, 50 patients were included and allocated to either surgical or non-surgical treatment. Patients undergoing surgical rib fixation received (preferably) a U-plate. Only fractures occurring in ribs four to nine were fixed. Anterior and lateral rib fractures were preferentially fixed over posterior rib fractures. Routine management for all patients in the study included pain control, external fixation by chest splint or bandage, pulmonary physiotherapy, fibrobronchoscopic drainage, and antibiotics administration. Two patients were lost to follow-up (one in each treatment group). The reported outcomes were (in-hospital) mortality, chest wall deformity, pain, pneumonia, tracheostomy, duration of mechanical ventilation, length of stay on the intensive care unit, length of stay in the hospital.
The randomized controlled trial of Marasco (2022) aimed to assess pain and quality of life outcomes in patients with multiple painful displaced fractured ribs with and without operative fixation. Inclusion criteria were previously functionally independent patients with multiple consecutive (≥3), closed fractured ribs between the level of ribs three and ten confirmed on chest x- ray and computed tomography of the chest. Patients also had to have either ongoing pain or displaced fractured ribs. Exclusion criteria were the following: preinjury dependency requiring acts of daily living support, invasive ventilator support at the time of enrollment (patients were not excluded if they deteriorated and required invasive ventilator support after that time), spinal injuries that precluded placement of the patient in a lateral decubitus position, open rib fractures with soiling or infection, severe head injury, uncorrected coagulopathy, adult respiratory distress syndrome, uncorrected sepsis, pregnancy, known opiate dependency, age younger than 18 years or older than 85 years, and inability to provide informed consent. In total, 124 patients were included and randomly allocated to either surgical rib fixation (n=61) or non-operative management (n=63). The maximum length of follow-up was six months. The reported outcomes were hospital length of stay, ICU length of stay, mortality, pain, and quality of life.
The randomized controlled trial of Meyer (2023) compared the effectiveness of surgical stabilization of rib fractures to non-operative management in severe chest wall injury. Patients (aged sixteen years or older) who were admitted to the study institution with a severe chest wall injury sustained secondary to a blunt trauma mechanism were included. Patients younger than sixteen years of age, having a clinical flail chest injury, severe traumatic brain injury, spinal cord injuries, pre-existing congestive heart failure or oxygen-dependent pulmonary disease, lacked equipoise for enrolment, were so severely injured that they were not expected to be able to undergo surgical rib fixation, or having COVID-infection were excluded. In total 84 patients were included and randomly assigned to either surgical stabilization of the rib (n=42) or non-operative management (n=42). The maximum length of follow-up was six months. Six patients in the surgical stabilization group and ten patients in the non-operative management group were lost to follow-up. The reported outcomes were hospital length of stay, mortality, seroma, infections, and pain.
The randomized controlled trial of Pieracci (2020) investigated the efficacy of surgical stabilization of rib fractures, specifically in patients with non-flail, severe rib fracture patterns, compared to non-operative management. Patients with three or more ipsilateral, bicortical, severely displaced, acute fractures of third up to the tenth rib were included. In total, 110 patients were included and assigned to either surgical stabilization or the rib (n=51) or non-operative management (n=59). The reported outcomes were quality of life and pain.
Results
Mortality
Six trials reported mortality; three trials from the systematic review of Cataneo (2015) (Granetzny, 2005; Marasco, 2013; Tanaka, 2002) and three additional trials (Liu, 2019; Marasco, 2022; Meyer, 2023). Liu (2019) reported in-hospital mortality. Granetzny (2005), Marasco (2013), Tanaka (2002) and Liu (2019) reported mortality rates in patients with flail chest trauma, while Marasco (2022) and Meyer (2023) reported mortality rates in patients with non-flail chest trauma.
Flail chest
The pooled mortality rate in the rib fixation group in patients with flail chest trauma was 6/86 (7.0%), compared to 6/87 (6.9%) in the no rib fixation group. This resulted in a pooled risk difference (RD) of -0.01 (95% CI -0.07 to 0.06), in favor of the rib fixation group (figure 1). This was not considered as a clinically relevant difference.
Non-flail chest trauma
The pooled mortality rate in the rib fixation group in patients with non-flail chest trauma was 0/103 (0%), compared to 2/105 (1.9%) in the no rib fixation group. This resulted in a pooled risk difference (RD) of -0.01 (95% CI -0.05 to 0.02), in favor of the rib fixation group (figure 1). This was not considered as a clinically relevant difference.
Figure 1. Forest plot showing the comparison between rib fixation and no rib fixation for mortality in patients with flail chest and non-flail chest trauma
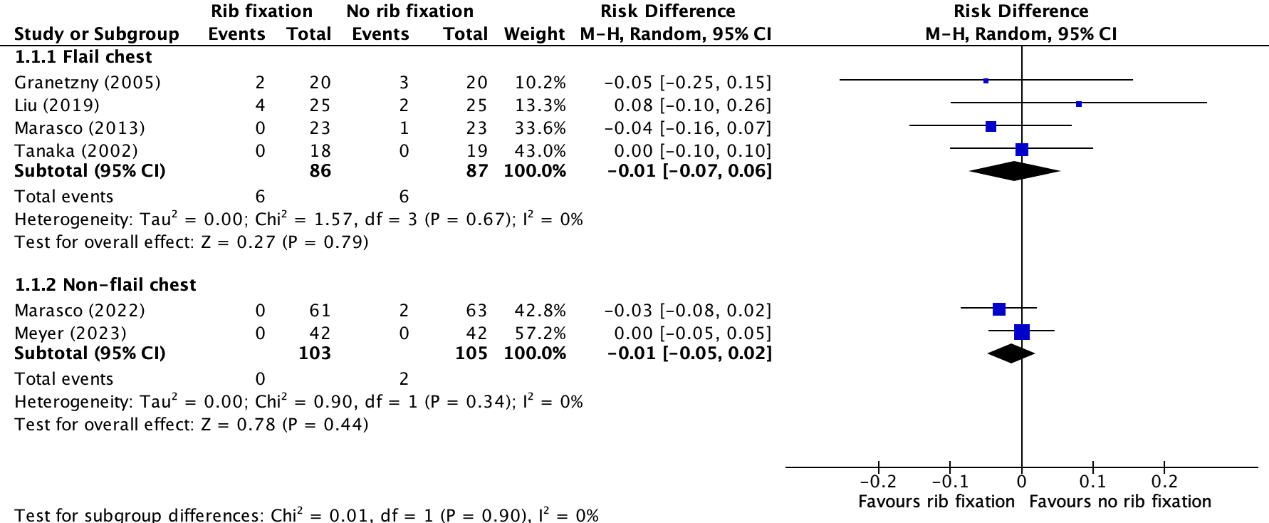
Pooled risk difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Pneumonia
Four trials reported pneumonia; three trials from the systematic review of Cataneo (2015) (Granetzny, 2005; Marasco, 2013; Tanaka, 2002) and one additional trial (Liu, 2019). All four studies reported pneumonia in patients with flail chest trauma. None of the included studies reported pneumonia rates in patients with non-flail chest trauma.
Flail chest
The pooled pneumonia rate in the rib fixation group in patients with flail chest trauma was 29/86 (33.7%), compared to 64/87 (73.6%) in the no rib fixation group. This resulted in a pooled relative risk ratio (RR) of 0.46 (95% CI 0.28 to 0.76), in favor of the rib fixation group (figure 2). This was considered as a clinically relevant difference.
Figure 2. Forest plot showing the comparison between rib fixation and no rib fixation for pneumonia in patients with flail chest trauma
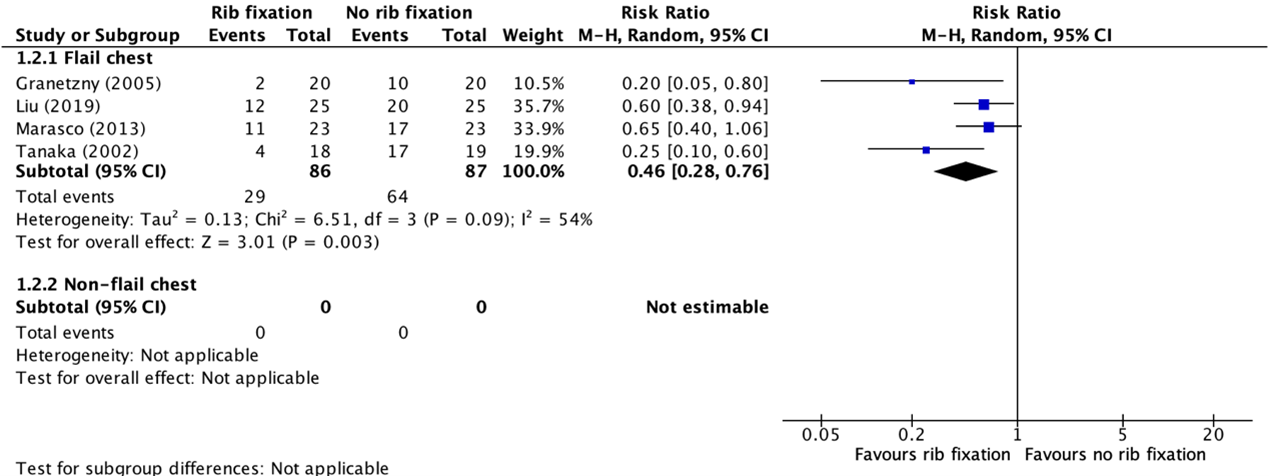
None of the included studies reported pneumonia rates in patients without flail chest traumas. Pooled relative risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Wound infections
Two trials reported wound infections. One trial from the systematic review of Cataneo (2015) (Granetzny, 2005) and one additional trial (Meyer, 2023). Granetzny (2005) reported wound infection rates in patients with flail chest trauma, while Meyer (2023) reported wound infection rates in patients with non-flail chest trauma. We only reported wound infection rates in patients who underwent surgical rib fixation descriptively and did not compare these results with patients who did not underwent rib fixation. The wound infection rate in the conservative treatment group is always zero, since non-operative treatment poses no risk of wound infection and so therefore, comparing both groups has no added value.
Flail chest
The number of wound infection rate in the rib fixation group in the study of Granetzny (2005) in patients with flail chest trauma was 2/20 (10.0%).
Non-flail chest trauma
The wound infection rate in the rib fixation group in the study of Meyer (2023) in patients with non-flail chest trauma was 1/42 (2.4%).
Chest deformity
Two trials reported chest deformities. One trial from the systematic review of Cataneo (2015) (Granetzny, 2005) and one additional trial (Liu, 2019). Both studies reported chest deformity rates in patients with flail chest trauma. None of the included studies reported chest deformity rates in patients with non-flail chest trauma. We only reported chest deformity rates in patients who underwent surgical rib fixation descriptively and did not compare these results with patients who did not underwent rib fixation. The chest deformity rate in the conservative treatment group is always zero, since non-operative treatment poses no risk of chest deformities and so therefore, comparing both groups has no added value.
Flail chest
The pooled chest deformity rate in the studies of Granetzny (2005) and Liu (2019) in patients with flail chest trauma in the rib fixation group was 3/45 (6.6%).
Tracheostomy
Two trials reported the need for tracheostomy. One trial from the systematic review of Cataneo (2015) (Marasco, 2013) and one additional trial (Liu, 2019). Both studies reported the need for tracheostomy in patients with flail chest trauma. None of the included studies reported the need for tracheostomy in patients with (multiple) rib fractures without flail chest trauma.
Flail chest
The pooled need for tracheostomy in patients with flail chest trauma in the rib fixation group was 19/48 (39.6%), compared to 23/48 (47.9%) in the no rib fixation group. This resulted in a pooled relative risk ratio (RR) of 0.86 (95% CI 0.34 to 2.16), in favor of the rib fixation group (figure 3). This was considered as a clinically relevant difference.
Figure 3. Forest plot showing the comparison between rib fixation and no rib fixation for the need for tracheostomy in patients with flail chest trauma
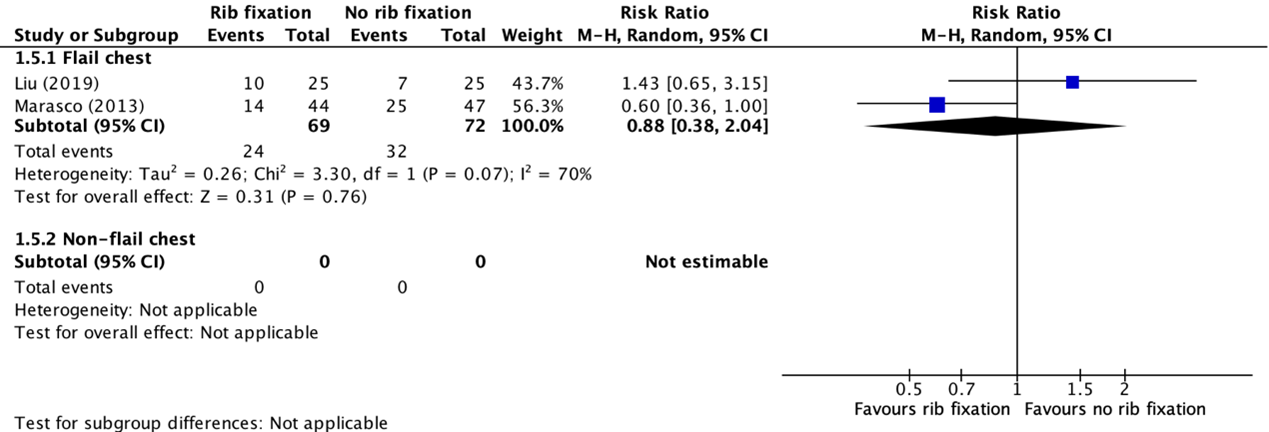
None of the included studies reported the need for tracheostomy in patients without flail chest traumas. Pooled relative risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
Duration of mechanical ventilation
Three trials reported length of mechanical ventilation; two trials from the systematic review of Cataneo (2015) (Granetzny, 2005; Tanaka, 2002) and one additional trial (Liu, 2019). All three studies reported the duration of mechanical ventilation in patients with flail chest trauma. None of the included studies reported duration of mechanical ventilation in patients with non-flail chest trauma. Granetzny (2005) and Tanaka (2002) reported the mean (SD) duration of mechanical ventilation in days. Liu (2019) reported the number of patients who required mechanical ventilation. The results of Granetzny (2005) and Tanaka (2002) were pooled in a meta-analysis. The results of Liu (2019) were presented separately.
Flail chest
The pooled mean difference (MD) in duration of mechanical ventilation in patients with flail chest trauma between the rib fixation group (n=43) and the no rib fixation group (n=43) is -5.71 (95% CI 14.32 to 2.91) days, in favor of the rib fixation group (figure 4). This was considered as a clinically relevant difference.
Figure 4. Forest plot showing the comparison between rib fixation and no rib fixation for duration of mechanical ventilation in patients with flail chest trauma
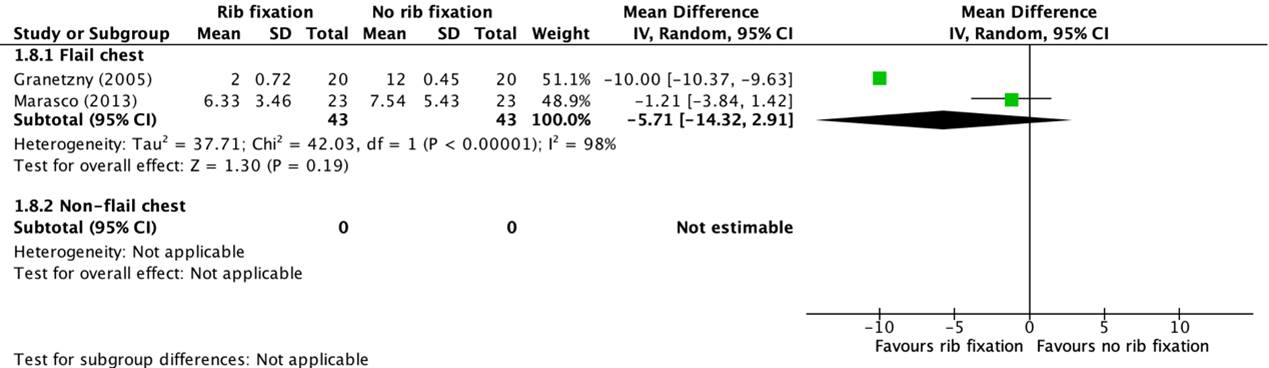
None of the included studies reported duration of mechanical ventilation in patients without flail chest traumas. Pooled mean difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
The requirement rate of mechanical ventilation in the study of Liu (2019) in the rib fixation group was 18/25 (72.0%), compared to 20/25 (80.0%) in the no rib fixation group. This resulted in a relative risk ratio (RR) of 0.90 (95% CI 0.66 to 1.23), in favor of the rib fixation group. This was not considered as a clinically relevant difference.
Length of hospital stay
Three trials reported length of hospital stay (Liu, 2019; Marasco, 2022; Meyer, 2023). Liu (2019) and Marasco (2022) reported the median (IQR) length of hospital stay in days, while Meyer (2023) reported the mean (SD) in days. Therefore, the results could not be pooled in a meta-analysis. Moreover, Liu (2019) reported the length of hospital stay in patients with flail chest trauma, while Marasco (2022) and Meyer (2023) reported length of hospital stay in patients with non-flail chest trauma.
Flail chest
The median (IQR) length of hospital stay in the rib fixation group in patients with flail chest trauma (n=25) in the study of Liu (2019) was 21 (17 to 25) days, compared to 22 (17 to 26) days in the no rib fixation group (n=25). This was considered as a clinically relevant difference.
Non-flail chest trauma
The median (IQR) length of hospital stay in patients with non-flail chest trauma in the study of Marasco (2022) in the rib fixation group was 10 (7 to 13.5) days, compared to 9 (6 to 13) days in the no rib fixation group. This was considered as a clinically relevant difference.
The mean (SD) length of hospital stay in patients with non-flail chest trauma in the rib fixation group (n=42) in the study of Meyer (2023) was 14.5 (10.7) days, compared to 9.9 (9.8) days in the no rib fixation group (n=42). This resulted in a mean difference (MD) of 4.60 (95% CI 0.21 to 8.99), in favor of the no rib fixation group. This was considered as a clinically relevant difference.
Length of ICU stay
Four trials reported length of ICU stay; two trials from the systematic review of Cataneo (2015) (Granetzny, 2005; Tanaka, 2002) and two additional trials (Liu, 2019; Marasco, 2022). Granetzny (2005), Liu (2019), and Tanaka (2002) reported the length of ICU stay in patients with flail chest trauma, while Marasco (2022) reported length of ICU stay in patients with non-flail chest trauma. Granetzny (2005) and Tanaka (2002) reported the mean (SD) length of ICU stay in days. Liu (2019) and Marasco (2022) reported the median (IQR) length of ICU stay in days. The results of Granetzny (2005) and Tanaka (2002) were pooled in a meta-analysis. The results of Liu (2019) and Marasco (2022) were presented separately.
Flail chest
The pooled mean difference (MD) in length of ICU stay in patients with flail chest trauma between the rib fixation group (n=38) and the no rib fixation group (n=39) is -12.55 (95% CI -27.54 to 2.54) days, in favor of the rib fixation group (figure 5). This was considered as a clinically relevant difference.
Figure 5. Forest plot showing the comparison between rib fixation and no rib fixation for length of ICU stay in patients with flail chest trauma
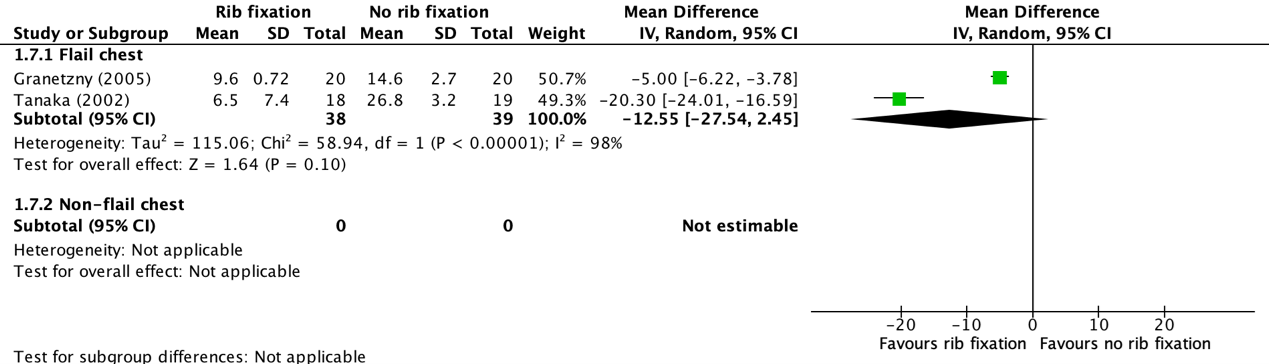
None of the included studies reported length of ICU stay in patients without flail chest traumas. Pooled mean difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; CI: confidence interval
The median (IQR) length of ICU stay in the study of Liu (2019) in the rib fixation group (n=25) was 10 (0 to 2) days, compared to 12 (9 to 15) days in the no rib fixation group (n=25). This was considered as a clinically relevant difference.
Non-flail chest trauma
The median (IQR) length of ICU stay in the study of Marasco (2022) in patients with non-flail chest trauma in the rib fixation group (n=23) was 1 (0 to 2) day, compared to 0 (0 to 2) days in the no rib fixation group (n=23). This was considered as a clinically relevant difference.
Technical failures
None of the included studies reported information with regards to technical failures in patients with flail chest trauma or patients with non-flail chest trauma who underwent rib fixation of no rib fixation.
Pain
Four trials reported pain (Liu, 2019; Marasco, 2022; Meyer, 2023; Pieracci, 2020). Liu (2019) reported pain scores in patients with flail chest trauma, while Marasco (2022), Meyer (2023), and Pieracci (2020) reported pain scores in patients with non-flail chest trauma. Liu (2019) reported the median (IQR) pain score in rest, during coughing and deep breathing on admission and after 1 week. Marasco (2022) reported the number of patients who did not report any pain symptoms at six months follow-up. This study used the VAS score for measuring pain in the first week, during admission and after three and seven days. After three and six months with the McGill Pain Questionnaire. Meyer (2023) used the VAS score and reported the mean (SD) pain score at one month months follow-up, and Pieracci (2020) only reported a numeric pain score (NPS) at two weeks follow-up (without a standard deviation). The results could therefore not be pooled in a meta-analysis and were presented separately.
Flail chest
The median (IQR) pain score in rest in the study of Liu (2019) in patients with flail chest trauma in the rib fixation group (n=25) was 6 (4 to 7) points, compared to 7 (4 to 8) in the no rib fixation group (n=25). This was considered as a clinically relevant difference.
Non-flail chest trauma
The number of patients in the study of Marasco (2022) with non-flail chest trauma who did not report pain symptoms in the rib fixation group was 14/44 (31.8%), compared to 25/47 (53.2%) in the no rib fixation group. This resulted in a relative risk ratio (RR) of 0.60 (95% CI 0.36 to 1.00), in favor of the rib fixation group. This was considered as a clinically relevant difference.
The mean (SD) pain score in the study of Meyer (2023) in patients with non-flail chest trauma in the rib fixation group was 74.0 (23.0) points, compared to 77.0 (20.0) points in the no rib fixation group. This resulted in a mean difference (MD) of -3.00 (95% CI 10.56 to 4.56), in favor of the rib fixation group. This was not considered as a clinically relevant difference.
The mean pain score in the study of Pieracci (2020) in patients with non-flail chest trauma in the rib fixation group (n=26) was 1.5 points, compared to 3.3 points in the no rib fixation group (n=26). Due to the absence of a standard deviation, it was not possible to determine if this difference could be considered clinically relevant.
Quality of life
Quality of life was reported in two trials (Marasco, 2022; Pieracci, 2020). Both studies reported quality of life scores in patients with non-flail chest trauma. Marasco (2022) reported the mean (SD) quality of life, measured with the Short-Form 12 (physical component). Pieracci (2020) reported the mean quality of life on an eleven-point Likert scale. The results could not be pooled in a meta-analysis and were presented separately. None of the included studies reported quality of life in patients with flail chest trauma.
Non-flail chest trauma
The mean (SD) quality of life score on the Short-Form 12 (physical component) in the study of Marasco (2022) in patients with non-flail chest trauma in the rib fixation group was 44.4 (11.5) points, compared to 47.6 (9.5) points in the no rib fixation group. This resulted in a mean difference (MD) of -3.20 (95% CI -7.71 to 1.31), in favor of the no rib fixation group. This was not considered as a clinically relevant difference.
The mean quality of life score in the study of Pieracci (2020) in patients with non-flail chest trauma in the rib fixation group was 10 points, compared to 7 points in the no rib fixation group. Due to the absence of a standard deviation, it was not possible to determine if this difference could be considered clinically relevant.
Costs
None of the included studies reported information with regards to costs in patients with rib fractures who underwent rib fixation of no rib fixation.
Table 1. Summary of results for patients with flail chest trauma
|
Effect size (95% CI) (relative risk (RR), risk difference (RD), or mean difference (MD)) |
|||||
Table 2. Summary of results for patients with non-flail chest trauma
|
Effect size (95% CI) (relative risk (RR), risk difference (RD), or mean difference (MD)) |
|||||
|
|
|||||
|
|
|||||
|
|
|
||||
|
|
|
MD -3.00 (95% CI 10.56 to 4.56)
|
|
||
|
|
|
MD -3.20 (95% CI -7.71 to 1.31)
|
|
||
Level of evidence of the literature
Mortality
The level of evidence regarding the outcome mortality was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of events and the wide confidence interval crossing both boundaries of clinical relevance (imprecision, -3). The level of evidence was considered as very low.
Pneumonia
The level of evidence regarding the outcome pneumonia was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of the small number of events (imprecision, -2). The level of evidence was considered as low.
Wound infections
Due to the fact that the control group doesn’t undergo an operative procedure and the outcome could only be presented descriptively, it was not possible to grade the literature for wound infections between rib fixation and no rib fixation in patients with flail chest trauma and non-flail chest trauma.
Chest deformity
Due to the fact that the control group doesn’t undergo an operative procedure and the outcome could only be presented descriptively, it was not possible to grade the literature for chest deformity between rib fixation and no rib fixation in patients with flail chest trauma and non-flail chest trauma.
Tracheostomy
The level of evidence regarding the outcome tracheostomy was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of events and the wide confidence interval crossing both boundaries of clinical relevance (imprecision, -3). The level of evidence was considered as very low.
Length of hospital stay
The level of evidence regarding the outcome length of hospital stay was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of included patients and the wide confidence interval crossing both thresholds of clinical relevance (imprecision, -3). The level of evidence was considered as very low.
Length of ICU stay
The level of evidence regarding the outcome length of ICU stay was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of included patients and the wide confidence interval crossing both thresholds of clinical relevance (imprecision, -3). The level of evidence was considered as very low.
Technical failures
None of the included studies reported information regarding the outcome ‘technical failures’.
Duration of mechanical ventilation
The level of evidence regarding the outcome duration of mechanical ventilation was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of included patients, the wide confidence interval crossing both thresholds of clinical relevance (both imprecision, -2), and indirectness of the study results (indirectness, -1). The level of evidence was considered as very low.
Pain
The level of evidence regarding the outcome pain was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of included patients, the wide confidence interval crossing both thresholds of clinical relevance (both imprecision, -2), and indirectness of the study results (indirectness, -1). The level of evidence was considered as very low.
Quality of life
The level of evidence regarding the outcome quality of life was derived from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of the small number of included patients, the wide confidence interval crossing both thresholds of clinical relevance (both imprecision, -2), and indirectness of the study results (indirectness, -1). The level of evidence was considered as very low.
Costs
None of the included studies reported information regarding the outcome ‘costs’.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
What are the (un)beneficial effects of rib fixation in comparison with no rib fixation in patients with flail chest trauma or non-flail chest trauma?
| P: |
Patients with flail chest trauma or non-flail chest trauma |
| I: |
Rib fixation |
| C: |
No rib fixation |
| O: |
Mortality, pneumonia, length of hospital stay, length of ICU stay, wound infection, chest deformity, technical failures, duration of mechanical ventilation (length), pain, quality of life, costs |
Relevant outcome measures
The guideline development group considered mortality as a critical outcome for decision making; and pneumonia, length of hospital stay, length of ICU stay, technical failures, length of mechanical ventilation, pain, quality of life, and costs as important outcomes for decision making.
The working group defined a threshold of 10% for continuous outcomes and a relative risk (RR) for dichotomous outcomes of <0.80 and >1.25 as a minimal clinically (patient) important difference.
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms until the 31st of July, 2023. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 361 hits. Studies were selected based on the following criteria: systematic reviews, randomized controlled trials, and observational study designs on fixation after rib fractures. Twenty-one studies (systematic reviews and/or randomized controlled trials) were initially selected based on title and abstract screening. After reading the full text, sixteen studies were excluded (see the table with reasons for exclusion under the tab Methods) and five studies were included.
Results
Five studies were included in the analysis of the literature. Important study characteristics and results are summarized in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
Referenties
- Bauman ZM, Khan H, Cavlovic L, Raposo-Hadley A, Todd SJ, King T, Cahoy K, Kamien A, Cemaj S, Sheppard O, Matos M, Berning B, Evans CH, Cantrell E. Surgical stabilization of rib fractures is associated with better return on investment for a health care institution than nonoperative management. J Trauma Acute Care Surg. 2023 Dec 1;95(6):885-892. doi: 10.1097/TA.0000000000004139. Epub 2023 Sep 15. PMID: 37710365.
- Cataneo AJ, Cataneo DC, de Oliveira FH, Arruda KA, El Dib R, de Oliveira Carvalho PE. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev. 2015 Jul 29;2015(7):CD009919. doi: 10.1002/14651858.CD009919.pub2. PMID: 26222250; PMCID: PMC9189492.
- Choi J, Mulaney B, Laohavinij W, Trimble R, Tennakoon L, Spain DA, Salomon JA, Goldhaber-Fiebert JD, Forrester JD. Nationwide cost-effectiveness analysis of surgical stabilization of rib fractures by flail chest status and age groups. J Trauma Acute Care Surg. 2021 Mar 1;90(3):451-458. doi: 10.1097/TA.0000000000003021. PMID: 33559982.
- Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005 Dec;4(6):583-7. doi: 10.1510/icvts.2005.111807. Epub 2005 Sep 15. PMID: 17670487.
- Liu T, Liu P, Chen J, Xie J, Yang F, Liao Y. A Randomized Controlled Trial of Surgical Rib Fixation in Polytrauma Patients With Flail Chest. J Surg Res. 2019 Oct;242:223-230. doi: 10.1016/j.jss.2019.04.005. Epub 2019 May 14. PMID: 31100568.
- Leinicke JA, Elmore L, Freeman BD, Colditz GA. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013 Dec;258(6):914-21. doi: 10.1097/SLA.0b013e3182895bb0. PMID: 23511840; PMCID: PMC3694995.
- LNAZ, registratiehandleiding LTR versie 2.0.
- Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R, Lee G, Bailey M, Fitzgerald M. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013 May;216(5):924-32. doi: 10.1016/j.jamcollsurg.2012.12.024. Epub 2013 Feb 13. PMID: 23415550.
- Marasco SF, Balogh ZJ, Wullschleger ME, Hsu J, Patel B, Fitzgerald M, Martin K, Summerhayes R, Bailey M. Rib fixation in non-ventilator-dependent chest wall injuries: A prospective randomized trial. J Trauma Acute Care Surg. 2022 Jun 1;92(6):1047-1053. doi: 10.1097/TA.0000000000003549. Epub 2022 Jan 25. PMID: 35081599.
- Meyer DE, Harvin JA, Vincent L, Motley K, Wandling MW, Puzio TJ, Moore LJ, Cotton BA, Wade CE, Kao LS. Randomized Controlled Trial of Surgical Rib Fixation to Nonoperative Management in Severe Chest Wall Injury. Ann Surg. 2023 Sep 1;278(3):357-365. doi: 10.1097/SLA.0000000000005950. Epub 2023 Jun 15. PMID: 37317861; PMCID: PMC10527348.
- Peek J, Beks RB, Hietbrink F, De Jong MB, Heng M, Beeres FJP, IJpma FFA, Leenen LPH Groenwold RHH, Houwert RM. Epidemiology and outcome of rib fractures: a nationwide study in the Netherlands. Eur J Trauma Emerg Surg. 2022 Feb;48(1):265-271. doi: 10.1007/s00068-020-01412-2. Epub 2020 Jun 6. PMID: 32506373; PMCID: PMC8825616.
- Pieracci FM, Leasia K, Bauman Z, Eriksson EA, Lottenberg L, Majercik S, Powell L, Sarani B, Semon G, Thomas B, Zhao F, Dyke C, Doben AR. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). J Trauma Acute Care Surg. 2020 Feb;88(2):249-257. doi: 10.1097/TA.0000000000002559. PMID: 31804414.
- Prins JTH, Wijffels MME, Wooldrik SM, Panneman MJM, Verhofstad MHJ, Van Lieshout EMM. Trends in incidence rate, health care use, and costs due to rib fractures in the Netherlands. Eur J Trauma Emerg Surg. 2022 Oct;48(5):3601-3612. doi: 10.1007/s00068-021-01662-8. Epub 2021 Apr 12. PMID: 33846831; PMCID: PMC9532326.
- Swart E, Laratta J, Slobogean G, Mehta S. Operative Treatment of Rib Fractures in Flail Chest Injuries: A Meta-analysis and Cost-Effectiveness Analysis. J Orthop Trauma. 2017 Feb;31(2):64-70. doi: 10.1097/BOT.0000000000000750. PMID: 27984449.
- Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002 Apr;52(4):727-32; discussion 732. doi: 10.1097/00005373-200204000-00020. PMID: 11956391.
Evidence tabellen
Systematic review(s)
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C)
|
Follow-up |
Outcome measures and effect size |
Comments |
|
Cataneo (2015) |
SR and meta-analysis of RCTs
Literature search up to the 12th of May 2014.
A: Granetzny (2005) B: Marasco (2013) C: Tanaka (2002)
Study design: A: RCT (parallel) B: RCT (parallel) C: RCT (parallel)
Setting and Country: A: B: C:
Source of funding and conflicts of interest: Frederico HS de Oliveira: none known. Daniele C Cataneo: none known. Karine A Arruda: none known. Antonio José Maria Cataneo: none known. Regina El Dib: none known. Paulo Eduardo de Olivira Carvalho: none known.
|
Inclusion criteria SR:
Three studies included
Important patient characteristics at baseline:
N A: N = 40 B: N = 46 C: N = 37
Sex: A: 31 males B: 40 males C: 26 males
Groups comparable at baseline? |
Describe intervention:
A: surgical fixation of fractured ribs with stainless steel wire or Kirschner wires, or both after 24-36 hours of ICU admission. Until the participants were operated upon, they were treated conservatively as if they were in Group I
B: only rib fractures between the levels of ribs 3 and 10 were fixed. Ribs fractured more than once were usually addressed by fixing 1 fracture per rib, converting a flail segment to simple fractured ribs. Ribs with a single fracture were not fixed unless there was gross deformity mandating intervention. Anterior and lateral rib fractures were preferentially fixed over posterior rib fractures
C: surgical stabilization
|
Describe control:
A: conservative treatment using strapping and packing in the form of dressing and fixing with an adhesive bandage, which was put adhesively to the flail segment within 5 cm anterior and posterior to the flail segment and 1 rib above and below it. This adhesive plaster was put in place for at least 7-10 days, during this period of follow-up ABGs and chest X-rays were obtained
B: Nonsurgical management: mechanical ventilation
C: Internal pneumatic stabilization.
|
End-point of follow-up:
A: 2 months. B: 6 months. C: 12 months.
|
Mortality A (Granetzny, 2005) I: 2/20 C: 3/20
B (Marasco, 2013) I: 0/23 C: 1/23
C (Tanaka, 2002) I: 0/18 C: 0/19
Chest deformity A (Granetzny, 2005) I: 1/20 C: 9/20
B (Marasco, 2013) I: 0/23 C: 2/23
Wound infection A (Granetzny, 2005) I: 2/20 C: 0/20
Pneumonia A (Granetzny, 2005) I: 2/20 C: 10/20
B (Marasco, 2013) I: 11/23 C: 17/23
C (Tanaka, 2002) I: 4/18 C: 17/19
Tracheostomy B (Marasco, 2013) I: 9/23 C: 16/23
C (Tanaka, 2002) I: 3/18 C: 15/19
Duration of mechanical ventilation A (Granetzny, 2005) I: 2.0 (0.72) days (N=20) C: 12.0 (0.45) days (N=20)
B (Marasco, 2013) I: 6.33 (3.46) days (N=23) C: 7.54 (5.43) days (N=23)
C (Tanaka, 2002) I: 10.8 (3.4) days (N=18) C: 18.3 (7.4) days (N=19)
Length of intensive care unit stay A (Granetzny, 2005) I: 9.6 (0.72) days (N=20) C: 14.6 (2.7) days (N=20)
C (Tanaka, 2002) I: 6.5 (7.4) days (N=18) C: 26.8 (3.2) days (N=19) |
Author’s conclusion There was some evidence from three small studies that showed surgical treatment was preferable to nonsurgical management in reducing pneumonia, chest deformity, tracheostomy, duration of mechanical ventilation, and length of ICU stay. Further well-designed studies with a sufficient sample size are required to confirm these results and to detect possible surgical effects on mortality. |
Randomized controlled trial(s)
|
Study reference |
Study characteristics |
Patient characteristics 2 |
Intervention (I) |
Comparison / control (C) 3
|
Follow-up |
Outcome measures and effect size 4 |
Comments |
|
Liu (2019)
|
Type of study: RCT
Setting and country: Trauma center.
Funding and conflicts of interest: None of the authors have any conflict of interest to declare about this article.
|
Inclusion criteria:
Exclusion criteria:
N total at baseline: Intervention: N = 25 Control: N = 25
Important prognostic factors2: age ± IQR: I: 42 (25-58) C: 39 (24-56)
Sex: I: 21/25 M C: 20/25 M
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
Operative rib fixation.
|
Describe control (treatment/procedure/test):
Non-surgical management. |
Length of follow-up: No information.
Loss-to-follow-up: One in each group.
|
Mechanical ventilation days (IQR) I: 7 (6 to 10) days C: 9 (7 to 12) days
ICU length of stay I: 10 (7 to 12) days C: 12 (9 to 15) days
Hospital length of stay I: 21 (17 to 25) days C: 22 (17 to 26) days
In-hospital mortality I: 4/25 (16%) C: 2/25 (8%)
Pneumonia I: 12/25 (48%) C: 20/25 (80%)
Tracheostomy I: 10/25 (40%) C: 7/25 (28%)
Mechanical ventilation required I: 18/25 (72%) C: 20/25 (80%)
Pain (rest) I: 6 (4 to 7) points C: 7 (4 to 8) points
Thoracic deformity I: 2/25 (8%) C: 9/25 (36%)
|
Author’s conclusion: This study reveals that surgical rib fixation may provide some critical care benefits for severe polytrauma patients with FC, including less medical resource use and lower risk of complications. Further studies should be designed to optimally identify patients who are most likely to benefit from this surgery. |
|
Marasco (2022)
|
Type of study: RCT
Setting and country: 12 USA trauma centers.
Funding and conflicts of interest: S.F.M. reports personal fees (consulting/lectures from Johnson & Johnson; consulting/lectures from Zimmer Biomet) outside the submitted work. M.B. reports fees for statistical consulting. J.H. reports personal fees (advi- sory board, Acumed; educational support and producing educational material, DePuy Synthes). For the remaining authors, no conflicts were declared. |
Inclusion criteria:
Exclusion criteria:
N total at baseline: Intervention: N = 61 Control: N = 63
Important prognostic factors2: age ± SD: I: 59.1 (15.1) C: 55.0 (15.1)
Sex: I: 48/61 (77.4%) M C: 51/63 (83.6%) M
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
Rib fixation.
|
Describe control (treatment/procedure/test):
Non-operative management |
Length of follow-up: Maximum of 6 months.
Loss-to-follow-up: I: 15 patients at 3 months and 17 patients at 6 months follow-up.
C: 11 patients at 3 months and 16 at 6 months follow-up.
|
Hospital length of stay I: 10 (7 to 13.5) days C: 9 (6 to 13)
ICU length of stay I: 1 (0 to 2) days C: 0 (0 to 2) days
Mortality I: 0/61 (0%) C: 2/63 (3.3%)
Pain (number of patients with no pain reported) I: 14/44 (32.0%) C: 25/47 (53.0%)
Quality of life (SF 12 at 6 months) Physical component I: 44.4 (11.5) points C: 47.6 (9.5) points
Mental component I: 51.6 (10.1) points C: 50.5 (11.9) points |
Author’s conclusion: In this study, no improvements in pain or QoL at 3 and 6 months in patients undergoing rib fixation for non-flail, non–ventilator-dependent rib fractures have been demonstrated. |
|
Meyer (2023) |
Type of study: RCT
Setting and country:
Funding and conflicts of interest: The authors report no conflicts of interest.
|
Inclusion criteria:
Exclusion criteria:
N total at baseline: Intervention: N = 42 Control: N = 42
Important prognostic factors2: age ± SD: I: 50 (15) C: 49 (15)
Sex: I: 28/42 (67%) M C: 31/42/ (74%) M
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
Surgical stabilization of rib fractures.
|
Describe control (treatment/procedure/test):
Usual care. |
Length of follow-up: 6 months.
Loss-to-follow-up: I: N = 6 C: N = 10 |
Hospital length of stay I: 14.5 (10.7) days C: 9.9 (9.8) days
Mortality I: 0/42 ()%) C: 0/42 (0%)
Seroma I: 1/42 (2.4%) C: 0/42 (0%)
Infections I: 1/42 (2.4%) C: 0/42 (0%)
Pain (6 months) (VAS) I: 74 (23) points C: 77 (20) points |
Author’s conclusion: In this clinical trial, SSRF performed within 72 hours improved the primary outcome of NPS at two week follow up among patients with ≥ 3 displaced fractures in the absence of flail chest. These data support a role for SSRF in patients without flail chest. |
|
Pieracci (2020) |
Type of study: RCT
Setting and country:
Funding and conflicts of interest: This work was funded in part by an investigator-initiated research grant from DePuy Synthes, Inc. (Raynham, MA), awarded to Denver Health Medical Center, Denver, CO.
- Fredric M. Pieracci MD: paid educator (past) and research funding (current) for DePuy Synthes, Inc. - Kiara Leasia MD: nothing to disclose. - Zach Bauman DO: nothing to disclose. - Evert Eriksson MD: paid educator (current) for DePuy Synthes, Inc. - Lawrence Lottenberg MD: paid consultant (current) for Acute Innovations, Inc, KLS Martin, Inc., and DePuy Synthes, Inc. - Sarah Majercik MD: nothing to disclose. - Ledford Powell MD: paid educator (current) for DePuy Synthes, Inc. - Babak Sarani MD: paid educator (current) for Acute Innovations, Inc. - Gregory Semon MD: nothing to disclose. - Bradley Thomas MD: paid educator (current) for Zimmer Biomet, Inc. - Frank Zhao MD: nothing to disclose. - Cornelius Dyke MD: nothing to disclose.
|
Inclusion criteria:
Exclusion criteria:
N total at baseline: Intervention: N = 51 Control: N = 59
Important prognostic factors2: age ± SD: I: 54.6 C: 55.3
Sex: I: 39/51 (76.5%) M C: 43/59 (74.1%) M
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
Operative fixation.
|
Describe control (treatment/procedure/test):
Non-operative treatment. |
Length of follow-up: 8 weeks.
Loss-to-follow-up: None. |
Quality of life (1-11) I: 10 points C: 7 points
Pain I: 1.5 points (N=26) C: 3.3 points (N=19) |
Author’s conclusion: In this clinical trial, SSRF performed within 72 hours improved the primary outcome of NPS at two week follow up among patients with ≥ 3 displaced fractures in the absence of flail chest. These data support a role for SSRF in patients without flail chest. |
Risk of bias tabel
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients/healthcare providers/data collectors/assessors/data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measure
LOW Some concerns HIGH
|
|
Liu (2019)
|
Definitely yes.
Reason: The enrolled patients were randomly assigned to the surgical or nonsurgical group. |
Probably yes.
Reason: Patients were randomized either to surgical or conservative treatment for FC by using random numbers balanced with block size of 10. |
Definitely no.
Reason: Blinding not possible. |
Probably yes.
Reason: One patient lost to follow-up in each group. |
Probably yes.
Reason: All pre-defined outcomes were reported. |
Probably yes.
Reason: No other biases reported. |
Some concerns. |
|
Marasco (2022)
|
Definitely yes.
Reason: Patients were randomized |
Probably yes.
Reason: Randomization was by computer allocation in a four-block design over all enrollments, irrespective of site. |
Definitely no.
Reason: Blinding not possible. |
Probably yes
Reason: Lost to follow-up almost equal in both groups. |
Probably yes.
Reason: All pre-defined outcomes were reported. |
Probably yes.
Reason: No other biases reported. |
Some concerns. |
|
Meyer (2023)
|
Definitely yes.
Reason: Patients were randomized with a 1:1 ratio. |
Definitely yes.
Reason: Allocation ratio using permuted blocks of 4 or 6 to ensure an equal number of patients in each group. |
Definitely no.
Reason: Given the nature of the intervention, the patients and treating physicians were not blinded to the allocation group.
|
Probably no.
Reason: Few cross-overs. |
Probably yes.
Reason: All pre-defined outcomes were reported. |
Probably yes.
Reason: No other biases reported. |
Some concerns. |
|
Pieracci (2020) |
Definitely yes.
Reason: The trial consisted of both randomized and observational arms. |
Probably yes.
Reason: Each study center followed an independent, block randomization schema. |
Definitely no.
Reason: Blinding not possible. |
Definitely yes.
Reason: No lost to follow-up reported. |
Probably yes.
Reason: All pre-defined outcomes were reported. |
Definitely no.
Reason: Unequal enrollment across centers may have resulted in unmeasured institutional bias |
Some concerns.
|
Exclusie tabel
|
Author and year |
Reason for exclusion |
|
Beks (2019) |
Includes the same studies as Cataneo (2015). |
|
Coughlin (2016) |
Includes the same studies as Cataneo (2015). |
|
Craxford (2022) |
Includes the same studies as Cataneo (2015). |
|
Granetzny (2005) |
Already included in SR of Cataneo (2015). |
|
Hoepelman (2023) |
Only includes observational studies, no RCTs. |
|
Ingoe (2019) |
Wrong study design. |
|
Leinicke (2013) |
Includes the same studies as Cataneo (2015). |
|
Liang (2019) |
Includes the same studies as Cataneo (2015). |
|
Liu (2019) |
Includes the same studies as Cataneo (2015). |
|
Long (2020) |
Includes the same studies as Cataneo (2015). |
|
Marasco (2022) |
Already included in SR of Cataneo (2015). |
|
Schuurmans (2017) |
Includes the same studies as Cataneo (2015). |
|
Sawyer (2022) |
Includes the same studies as Cataneo (2015). |
|
Schuurmans (2017) |
Includes the same studies as Cataneo (2015). |
|
Slobogean (2013) |
Includes the same studies as Cataneo (2015). |
|
Swart (2017) |
Includes the same studies as Cataneo (2015). |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 28-05-2025
Beoordeeld op geldigheid : 28-05-2025
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Stichting Kwaliteitsgelden Medisch Specialisten (SKMS) en/of andere bron. De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2022 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met thoracale letsels na trauma.
Werkgroep
- Dr. M.M.E. (Mathieu) Wijffels, traumachirurg, NVvH (voorzitter)
- Drs. P.J. (Pieter Jan) van Huijstee, longchirurg, NVvH (voorzitter)
- Dr. D. (Doeke) Boersma, chirurg, NVvH
- Dr. W.P. (Wietse) Zuidema, chirurg, NVvH
- Drs. W.W.L. (Wilson) Li, cardiothoracaal chirurg, NVT
- Drs. A.W.M. (Antoinette) Stolwijk, chirurg-intensivist, NVIC
- Drs. V.P.M. (Vincent) Rietveld, SEG, NVSHA
- Dr. M. (Monique) Brink, radioloog, NVvR
- Drs. S.A.S. (Sandra) van den Heuvel, anesthesioloog, NVA
- L. (Lydia) Köster MSc, fysiotherapeut, KNGF
Klankbordgroep
- T. (Thomas) Jonkergouw, adviseur patiëntbelang, Patiëntenfederatie Nederland
- Dr. H. (Hendrik-Jan) Dieker, cardioloog, NVVC
Met ondersteuning van
- Dr. R. (Romy) Zwarts – van de Putte, adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- M. (Mitchel) Griekspoor MSc., adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Drs. E.R.L. (Evie) Verweg, junior adviseur, Kennisinstituut van Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Wijffels |
Traumachirurg, Erasmus MC |
Geen |
Onderzoeksbeurzen van ZonMw (prospectieve ribfixatie studie), Johnson en Johnson DePuy Synthes, OTC/Stryker, Stichting Coolsingel, KLS Martin (onderzoek naar ribplaten) |
Gedeeltelijke restrictie. Het werkgroeplid zal niet meebeslissen over ribfixatie en/of ribplaten. Wanneer deze onderwerpen worden besproken zal Monique Brink de vergadering voorzitten. |
|
Van Huijstee |
Algemeen Thoracaal en Trauma-Chirurg, Medische Specialistische Co-operatie HAGA Ziekenhuis, Den Haag
|
Voorzitter Ned. Ver. Voor Longchirurgie (Onbetaald), Bestuurslid Ned. Ver. Voor Heelkunde (Onbetaald), ATLS-instructeur bij stichting ALSG.
Executive Board Member of Chest Wall International Group (onbezoldigd) |
Ad Hoc, Betaald adviseurschap bij Distrimed voor ontwikkeling van nieuwe implantaten voor congenitale borstkasafwijkingen en onkostenvergoeding bij proctoring van collega-chirurgen in het gebruik van deze implantaten. |
Gedeeltelijk restrictie. Het werkgroeplid zal niet meebeslissen over ribfixatie en/of ribplaten. Wanneer deze onderwerpen worden besproken zal Monique Brink de vergadering voorzitten. |
|
Stolwijk |
Traumachirurg, intensivist, MUMC+ |
Lid klankbordgroep richtlijn abdominale letsels na trauma medisch Manager Acute Zorg Limburg (NAZL) |
Geen.
|
Geen restrictie |
|
Boersma |
Chirurg |
Geen |
Geen |
Geen restrictie |
|
Köster |
Fysiotherapeut projectleider/ adviseur Traumazorg bij het traumacentrum Zuid West Nederland. |
Geen. Penningmeester geworden van Stichting Netwerk Traumarevalidatie Nederland (onbetaald). |
Geen |
Geen restrictie |
|
Brink |
Radioloog, Radboud UMC |
Sprekersbureau Canon Medical Systems |
Research Grant Canon Medical Systems 2016-2020 |
Geen restrictie |
|
Rietveld |
SEH-arts, Rijnstate |
Partner en course director DEUS |
Ontwikkeling point-of-care echografie |
Geen restrictie |
|
Zuidema |
Traumachirurg, Amsterdam UMC |
Secretaris NVT, Lid Geschillencommisie Ziekenhuizen |
Unrestricted grant (Mendela) voor studie over digitale pneumothorax zuigsystemen |
Geen restrictie |
|
Van den Heuvel |
Anesthesioloog 50%, pijnspecialist 50%, Radboud UMC |
Geen |
Regiehouder pijn Radboudumc, Editor pijn.nl Co-secretaris World Institute of Pain Benelux, onbetaald Educational committee web-based learning World Institute of Pain, onbetaald |
Geen restrictie |
|
Li |
Cardiothoracaal chirurg, Radboudumc |
Secretaris NVT |
Geen |
Geen restrictie |
|
Jonkergouw |
Adviseur Patiëntbelang Patiëntenfederatie Nederland |
Vrijwilliger Diabetes Vereniging Nederland |
Geen |
Geen restrictie |
|
Dieker |
Cardioloog, Radboudumc |
Geen |
Geen |
Geen restrictie |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door deelname aan de schriftelijke knelpunteninventarisatie en een afgevaardigde patiëntenvereniging in de klankbordgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voor commentaar voorgelegd aan de Patiëntenfederatie Nederland en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijnmodule is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd om te beoordelen of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling is de richtlijnmodule op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
|
Module |
Uitkomst raming |
Toelichting |
|
Module Fixatie na een ribfractuur |
Geen financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (5.000-40.000 patiënten), volgt ook uit de toetsing dat het geen nieuwe manier van zorgverlening of andere organisatie van zorgverlening betreft. Er worden daarom geen financiële gevolgen verwacht. |
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor patiënten met thoracale letsels. Tevens zijn er knelpunten aangedragen door wetenschappelijke verenigingen via een schriftelijke knelpunteninventarisatie. Een verslag hiervan is opgenomen onder aanverwante producten.
Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. Review Manager 5.4 werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nul effect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), duurzaamheid, aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
Algemene informatie
|
Richtlijn: NVvH Thoracale letsels na trauma |
|
|
Uitgangsvraag: Wat is de plaats van fixatie van de ribben na een ribfractuur? |
|
|
Database(s): Medline (OVID), Embase |
Datum: 31-07-2023 |
|
Periode: >2000 |
Talen: Geen beperking |
|
Literatuurspecialist: Linda Niesink |
|
|
BMI zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting en opmerkingen:
→ Voor deze vraag is gezocht op de elementen ribfractuur (in het blauw) en fixatie (van de ribben) (in het groen).
→ De genoemde sleutelartikelen van Beks (2019), Long (2020), Apampa (2022), Majeed (2018), Liu (2019) en Cataneo (2015) zitten in de zoekopbrengst.
→ Resultaten staan in Rayyan. |
|
|
Te gebruiken voor richtlijnen tekst: In de databases Embase (via embase.com) en Medline (via OVID) is op 31-07-2023 met relevante zoektermen gezocht vanaf 2000 naar systematische reviews, RCT’s en observationele studiedesigns over fixatie na een ribfractuur. De literatuurzoekactie leverde 361 unieke treffers op. |
|
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SRs |
40 |
35 |
44 |
|
RCTs |
73 |
64 |
89 |
|
Observationele studies |
203 |
165 |
228 |
|
Totaal |
316 |
264 |
361 |
Zoekstrategie
|
Database |
Zoektermen |
|||||||||||||||||||||||||||||||||
|
Embase
|
|
|||||||||||||||||||||||||||||||||
|
Medline (OVID)
|
1 exp Rib Fractures/ or exp Flail Chest/ or 'broken rib*'.ti,ab,kf. or ((rib or ribs or ribcage or 'rib cage' or costa or costal) adj3 fracture*).ti,ab,kf. or 'flail chest'.ti,ab,kf. (6595) 2 exp Fracture Fixation/ or ((rib* OR operative OR surgical OR internal) adj3 fixation*).ti,ab,kf. OR (fix* adj3 fracture*).ti,ab,kf. OR (rib adj3 (plate OR stent OR osteosynthesis)).ti,ab,kf. (87679) 3 1 and 2 (790) 4 limit 3 to yr="2000 -Current" (618) 5 4 not (comment/ or editorial/ or letter/ or ((exp animals/ or exp models, animal/) not humans/)) (589) 6 meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. (683534) 7 exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. (2615479) 8 Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) (5476978) 9 5 and 6 (35) – SRs 10 (5 and 7) not 9 (64) - RCTs 11 (5 and 8) not (9 or 10) (165) – observationele studies 12 9 or 10 or 11 (264) |
