Pessarium/cerclage voor de preventie van vroeggeboorte
Uitgangsvraag
Wat is de meest effectieve interventie (Progesteron/pessarium/cerclage) bij een vrouw zwanger van een eenling met een asymptomatische korte cervix met/zonder vroeggeboorte in de voorgeschiedenis?
De uitgangsvraag omvat de volgende deelvragen:
- Voorkomt het gebruik van cerclage (versus geen cerclage, pessarium, progesteron) vroeggeboorte bij vrouwen met een korte cervix en vroeggeboorte in de voorgeschiedenis?
- Voorkomt het gebruik van cerclage (versus geen cerclage, pessarium, progesteron) vroeggeboorte bij vrouwen met een korte cervix zonder vroeggeboorte in de voorgeschiedenis?
- Voorkomt het gebruik van pessarium (versus geen pessarium, cerclage, progesteron) vroeggeboorte bij vrouwen met een korte cervix en vroeggeboorte in de voorgeschiedenis?
- Voorkomt het gebruik van pessarium (versus geen pessarium, cerclage, progesteron) vroeggeboorte bij vrouwen met een korte cervix zonder vroeggeboorte in de voorgeschiedenis?
Aanbeveling
Aanbeveling-1
Adviseer de zwangere vrouw met een vroeggeboorte in de voorgeschiedenis < 34 weken en een asymptomatische korte cervix ≤ 25 mm voor 24 weken zwangerschapsduur, het aanleggen van een cerclage (naast behandeling met progesteron).
Plaats niet standaard cerclage bij vrouwen met een cervix < 25 mm zonder vroeggeboorte in de voorgeschiedenis maar bespreek behandeling met progesteron
Aanbeveling-2
Plaats geen pessarium bij vrouwen met een korte cervix met of zonder vroeggeboorte in de voorgeschiedenis.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Cerclage
Op basis van de literatuuranalyse werden mogelijke voor- en nadelen van cerclage vergeleken met geen cerclage, pessarium of progesteron bij vrouwen met een korte cervix en wel of geen vroeggeboorte in de voorgeschiedenis.
- Cerclage versus geen cerclage bij vrouwen met een vroeggeboorte in de voorgeschiedenis en een midtrimester cervixlengte ≤ 25 mm.
De studie van Conde-Agudelo (2018) laat een afname zien van vroeggeboorte voor 28 weken (Pooled RR 0.64, 95 CI 0.43 – 0.96). voor 32 weken (Pooled RR 0.66, 95% CI 0.48 – 0.91), en en voor 37 weken (Pooled RR 0.70, 95% CI 0.58 – 0.83) bij vrouwen met een vroeggeboorte in de voorgeschiedenis en een mid trimester cervixlengte van ≤ 25 mm wanneer er een cerclage is aangelegd. Tevens laten zij zien dat de composite neonatal morbidity/mortality in de cerclage groep is afgenomen (RR 0.64, CI 0.45 – 0.91). Losse parameters zoals RDS en neonatale sterfte zijn wel lager in de cerclage groep, maar de CI interval is te groot door de relatief lage aantallen. Daarom is gekozen voor de composite outcome neonatal morbidity and mortality waarin wel een significant verschil wordt gezien. In de conclusies van de uitkomstmaten wordt de level of evidence echter afgewaardeerd tot low grade of very low grade als gevolg van imprecision (onnauwkeurigheid) op basis van relatief wijde confidence intervallen of lage aantallen in de studies.
Op basis van de hierboven genoemde argumenten is de werkgroep van mening dat in een hoogrisicopopulatie van vrouwen met een vroeggeboorte in de voorgeschiedenis (naast de behandeling met progesteron) seriele metingen van de cervix moeten worden verricht en bij een midtrimester cervixlengte ≤ 25 mm het aanleggen van een cerclage geadviseerd zou moeten worden, aangezien er bewijsvoering is dat deze behandeling de kans op een (extreme) vroeggeboorte en neonatale morbiditeit en mortaliteit kan verlagen. Hierbij dient u zorgvuldig de risico’s van een operatieve ingreep (zoals het breken van de vliezen, bloedingen of infecties) af te wegen tegen de grotere kans op vroeggeboorte bij een afwachtend beleid. U dient geen cerclage te plaatsen bij een vroeggeboorte in de voorgeschiedenis en normale cervixlengte.
- Cerclage versus geen cerclage bij vrouwen met een korte cervix zonder vroeggeboorte in de voorgeschiedenis.
Op basis van de literatuur lijkt er geen verschil te zijn in de uitkomstmaten tussen de groep vrouwen zonder vroeggeboorte in de voorgeschiedenis die een cerclage krijgt bij een cervix < 25 mm en de groep vrouwen die geen cerclage krijgt bij een cervix < 25 mm. Ook zonder afwaardering van de level of evidence tot “very low grade“ zijn er onvoldoende aanwijzingen dat het plaatsen van een cerclage de uitkomstmaten verbetert. Voor behandeling van deze specifieke groep zwangere vrouwen verwijzen we naar de module progesteron ter preventie van vroeggeboorte die tevens onderdeel is van deze richtlijn. De meta-analyse van Berghella (2017) laat in een subgroep analyse wel een effect van cerclage zien op afname van vroeggeboorte < 35 weken bij een cervixlengte ≤ 10 mm. Aangezien het hier een subgroep analyse betreft met relatief weinig patiënten is de Grade classificatie te laag om dit als routinezorg aan te bieden. . De werkgroep beschouwt behandeling van deze specifieke subgroep nu als een kennislacune.
- Cerclage versus progesteron
Op basis van de literatuuranalyse kan er geen eenduidig besluit worden genomen. Er werd geen verschil gezien in de uitkomstmaten tussen vrouwen die behandeld werden met een cerclage bij een korte cervix versus een behandeling met progesteron. Er kan geen aanbeveling worden gegeven gezien de zeer lage bewijskracht van de conclusies uit de literatuur.
- Cerclage versus pessarium
Er zijn op dit moment geen studies die specifiek een directe vergelijking hebben beschreven van cerclage met pessarium. De werkgroep identificeert het effect van een cerclage versus pessarium bij vrouwen met een korte cervix ≤ 25 mm met een vroeggeboorte in de voorgeschiedenis als een kennislacune. Op dit moment is er een NVOG consortium studie (PC studie) afgerond. De uitkomsten van deze studie zullen in een volgende versie van deze module worden opgenomen.
Pessarium
- Pessarium versus geen pessarium bij korte cervix zonder vroeggeboorte in de voorgeschiedenis.
Voor de vrouwen met een korte cervix zonder een vroeggeboorte in de voorgeschiedenis lijkt er geen verschil te zijn tussen pessarium of geen pessarium (GRADE low). Ten aanzien van de uitkomstmaat neonatale sterfte lijkt er niet tot nauwelijks verschil te zijn bij het gebruik van pessarium bij vrouwen met een verkorte cervix ten opzichte van geen gebruik van pessarium (GRADE low). Voor de samengestelde uitkomstmaat voor neonatale mortaliteit en morbiditeit lijkt er geen tot nauwelijks verschil te zijn bij gebruik van pessarium vergeleken met geen pessarium in de groep vrouwen met een korte cervix (GRADE low). In de studie van Nicolaides werd in 47 vrouwen (11 % van de gevallen) het pessarium verwijderd wegens vaginale afscheiding, discomfort, of bloedverlies.
- Pessarium versus geen pessarium bij korte cervix met vroeggeboorte in de voorgeschiedenis.
Voor de cruciale uitkomstmaat vroeggeboorte <34 weken is het zeer onzeker wat het effect is van pessarium in de groep vrouwen met een korte cervix en met een vroeggeboorte in de voorgeschiedenis (GRADE very low). Andere uitkomstmaten zijn niet afzonderlijk beschreven.
Op basis van de gerapporteerde literatuur lijkt er onvoldoende bewijs te zijn voor het plaatsen van een pessarium bij vrouwen met een korte cervix met of zonder vroeggeboorte in de voorgeschiedenis.
5. Pessarium versus progesteron
Op basis van de literatuuranalyse kan geen eenduidig besluit worden genomen, de literatuurconclusies laten een zeer lage bewijskracht zien.
Welke behandeling (progesteron, cerclage of pessarium) dient u met uw patiënt te bespreken ten aanzien van het beperken van de kans op vroeggeboorte?
Op basis van de huidige literatuur zoals eerder beschreven in de module progesteron ter preventie van vroeggeboorte (aangevuld met de EPPPIC studie, Lancet 2021;397:1183-94) is het advies om bij vrouwen met een korte cervix < 25 mm, met of zonder een vroeggeboorte in de voorgeschiedenis progesteron voor te schrijven. Op basis van de EPPPIC studie leidt behandeling met progesteron tot een afname van vroeggeboorte onder de 34 weken, tot afname van een laag geboortegewicht, en tot afname van NICU opname en RDS. Daarbij is het advies om vaginaal progesteron (Utrogestan 1 dd 200 mg) voor te schrijven.
Indien er sprake is van vroeggeboorte in de voorgeschiedenis < 34 weken en een midtrimester korte cervixlengte ≤ 25 mm, dan is het advies om naast de behandeling met progesteron een cerclage te plaatsen.
Het plaatsen van een cerclage bij een korte cervix zonder vroeggeboorte in de voorgeschiedenis leidt niet tot een significante verbetering van de uitkomstmaten. Deze patiënten hebben wel baat bij behandeling met progesteron. Het plaatsen van een cerclage in een subgroep van vrouwen met een cervixlengte < 10 mm wordt door de werkgroep beschouwd als een kennislacune.
Het plaatsen van een pessarium bij een korte cervix lijkt niet te leiden tot een significante verlenging van de zwangerschapsduur of een significante verlaging van de neonatale composite morbidity/mortality. De uitkomst van de PC studie zal worden meegenomen in een volgende versie van deze module.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Preventie van vroeggeboorte is zinvol, aangezien het leidt tot een vermindering van het aantal vroeggeboortes, hetgeen leidt tot minder neonatale morbiditeit, mortaliteit en een aanzienlijke kostenbesparing voor de maatschappij. Hoewel er aanvankelijk alleen een voordeel van een interventie werd gezien bij een vroeggeboorte in de voorgeschiedenis, zijn er nu ook voldoende aanwijzingen dat er bij een korte cervix (ook zonder vroeggeboorte in de voorgeschiedenis) ook de mogelijkheid is tot behandelen, namelijk met progesteron.
Kosten (middelenbeslag)
Zowel progesteron als cerclages zijn vrij eenvoudige en niet erg kostbare behandelingen, dus indien dit reductie van composite adverse neonatal outcome oplevert, verwacht de werkgroep dat dit kosteneffectief zal zijn. Of screening naar cervixlengtes en de daarbij behorende behandeling kosteneffectief zal zijn, zal in Nederland verder moeten worden onderzocht.
Aanvaardbaarheid, haalbaarheid en implementatie
Implementatie van deze richtlijn is geen probleem ; het meten van een cervixlengte en het behandelen met progesteron in een hoog risicopopulatie is standaard beleid in Nederland, evenals het plaatsen van een cerclage bij een korte cervix in deze hoogrisicogroep. Het meten van de cervixlengte in een laagrisico populatie zal moeten worden geïmplementeerd.
Het plaatsen van een pessarium is minder goed geïmplementeerd en het advies zal zijn om dit alleen nog in studieverband te doen.
Rationale van de aanbeveling-1: weging van argumenten voor en tegen de interventies
De werkgroep is van mening dat in een hoogrisicopopulatie van patiënten met een vroeggeboorte in de voorgeschiedenis ( < 34 weken) seriele metingen van de cervix moeten worden verricht (zie module ‘Herhaalde cervixlengtemetingen bij vroeggeboorte in de voorgeschiedenis’) en bij een midtrimester cervixlengte ≤ 25 mm het aanleggen van een cerclage geadviseerd zou moeten worden, aangezien er bewijsvoering is dat deze behandeling de kans op een (extreme) vroeggeboorte en neonatale morbiditeit en 39mortaliteit kan verlagen. Hierbij dient u zorgvuldig de risico’s van een operatieve ingreep af te wegen tegen de grotere kans op vroeggeboorte bij een afwachtend beleid. Indien er geen vroeggeboorte in de voorgeschiedenis is, dan is er onvoldoende bewijsvoering voor het plaatsen van een cerclage bij een korte cervix.
Rationale van de aanbeveling-2: weging van argumenten voor en tegen de interventie
Het plaatsen van een pessarium bij een korte cervix (met of zonder vroeggeboorte in de voorgeschiedenis) lijkt niet te leiden tot een significante verlenging van de zwangerschapsduur of een significante verlaging van de neonatale composite morbidity/mortality.
Onderbouwing
Achtergrond
Sinds de vorige richtlijn preventie vroeggeboorte uit 2007 zijn een aantal nieuwe studies verschenen die het nut van progesteron (vaginaal, oraal, of intramusculair), cerclage en pessarium hebben onderzocht bij vrouwen met een vroeggeboorte in de voorgeschiedenis en al dan niet een korte cervixlengte. De huidige module is erop gericht om een eenduidig advies te geven aan hulpverleners zodat praktijkvariatie wordt verminderd, en de juiste behandeling voor de juiste patiëntengroep wordt toegepast. De module progesteron is onlangs gepubliceerd (21-09-2019) en zal daarom grotendeels buiten de beschouwing van deze richtlijnmodule blijven. (https://richtlijnendatabase.nl/richtlijn/preventie_vroeggeboorte/progesteron_voor_het_voorkomen_van_vroeggeboorte.html).
Conclusies / Summary of Findings
Conclusions PICO 1- Cerclage versus no cerclage/pessary/progesterone
1.1 Cerclage compared to no cerclage in women with a cervical length < 25 mm
- Preterm birth <28 weeks and previous preterm birth
|
Low GRADE |
Cerclage may reduce spontaneous preterm birth <28 weeks compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
Preterm birth < 28 weeks and no previous preterm birth
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on spontaneous preterm birth <28 weeks compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no previous preterm birth.
Source: Berghella, 2017 |
- Preterm birth <34 weeks (previous history not specified)
|
Very low GRADE |
The evidence is very uncertain about the use of cerclage on spontaneous preterm birth <34 weeks compared to no cerclage in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Jarde, 2019 |
Preterm birth < 32 weeks, and previous preterm birth
|
Low GRADE |
Cerclage may reduce spontaneous preterm birth <32 weeks compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
Preterm birth < 34 weeks and no previous preterm birth
|
low GRADE |
The use of cerclage may result in a small difference in favour of cerclage in spontaneous preterm birth <34 weeks compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no previous preterm birth.
Source: Berghella, 2017 |
- Preterm birth <37 weeks (previous history not specified)
|
Low GRADE |
The use of cerclage may result in a small difference in favour of cerclage in spontaneous preterm birth <37 weeks compared to no cerclage in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Jarde, 2019 |
Preterm birth and previous preterm birth
|
Low GRADE |
Cerclage may reduce spontaneous preterm birth <37 weeks compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
Preterm birth < 37 weeks and no previous preterm birth
|
low GRADE |
The use of cerclage may result in little to no difference in spontaneous preterm birth <37 weeks compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no previous preterm birth.
Source: Berghella, 2017 |
- Neonatal death
|
Low GRADE |
The use of cerclage may reduce the risk of neonatal death compared to no cerclage in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Jarde, 2019 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on neonatal death compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Sources: Conde-Agudelo, 2018 |
|
Low GRADE |
The use of cerclage may result in little to no difference in neonatal death compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no previous preterm birth.
Sources: Berghella, 2017 |
- Composite outcome neonatal mortality/morbidity and previous preterm birth
|
Low GRADE |
Cerclage may reduce composite neonatal mortality/morbidity defined as the occurrence of any of the following neonatal morbidities; respiratory distress syndrome; grade III/IV intraventricular haemorrhage; necrotizing enterocolitis; neonatal sepsis; bronchopulmonary dysplasia, or perinatal death compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Sources: Conde-Agudelo, 2018 |
Composite outcome neonatal mortality/morbidity and no previous preterm birth
|
- |
No data was reported on composite outcome neonatal mortality/morbidity for women with a cervical length ≤25mm and no previous preterm birth.
Sources: - |
- Respiratory distress syndrome
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on respiratory distress syndrome compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on respiratory distress syndrome compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no history of previous preterm birth.
Source: Berghella, 2017 |
- Necrotizing enterocolitis
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on necrotizing enterocolitis compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
|
- GRADE |
The evidence is very uncertain about the effect of cerclage on necrotizing enterocolitis compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no history of previous preterm birth.
Source: Berghella, 2017 |
- Intraventricular haemorrhage
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on intraventricular haemorrhage compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, (preterm birth not considered).
Source: Jarde, 2019 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on intraventricular haemorrhage compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on intraventricular haemorrhage compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no history of previous preterm birth.
Source: Berghella, 2017 |
- Neonatal sepsis
|
Very low GRADE |
The evidence is very uncertain about the effect of use of cerclage on neonatal sepsis compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Conde-Agudelo, 2018 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on neonatal sepsis compared to no cerclage in pregnant women with a singleton gestation, cervical length ≤25mm, and no history of previous preterm birth.
Source: Berghella, 2017 |
1.2 Cerclage compared to Progesterone
|
Very low GRADE |
The use of cerclage may result in little to no difference in spontaneous preterm birth (<34, <37, <28 weeks) compared to progesterone in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Keeler, 2009 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on spontaneous preterm birth (<37 weeks) compared to progesterone in pregnant women with a singleton gestation and cervical length ≤25mm and history of preterm birth
Sources: Keeler, 2009 |
|
Very low GRADE |
The evidence is very uncertain about the effect of cerclage on perinatal mortality/morbidity compared to progesterone in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Keeler, 2009 |
Conclusions PICO-2 Pessary compared to no pessary/cerclage/progesterone
2.1 Pessary compared to no pessary in women with a cervical length < 25 mm
1. Spontaneous birth < 32 weeks and preterm birth not considered
|
Low GRADE |
The use of pessary may result in little to no difference in spontaneous preterm birth (<32 weeks) compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm (preterm birth not considered).
Sources: Conde-Agudelo, 2020 |
2. Spontaneous preterm birth < 34 weeks and preterm birth not considered
|
Very low GRADE |
The evidence is very uncertain about the effect of pessary on spontaneous preterm birth <34 weeks compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
Spontaneous preterm birth < 34 weeks and no previous preterm birth
|
Low GRADE |
The use of pessary may result in little to no difference in spontaneous preterm birth (<34 weeks) compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm, and no previous preterm birth
Sources: Conde-Agudelo, 2020 |
Spontaneous preterm birth < 34 weeks and previous preterm birth
|
Very low GRADE |
The evidence is very uncertain about the effect of pessary on spontaneous preterm birth <34 weeks compared to no pessary in pregnant women with a singleton gestation, cervical length ≤25mm, and previous preterm birth.
Source: Nicolaides, 2016 |
3. Spontaneous birth < 37 weeks and preterm birth not considered
|
Very low GRADE |
The evidence is very uncertain about the effect of pessary on spontaneous preterm birth (<37 weeks) compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm
Sources: Conde-Agudelo, 2020 |
4. Perinatal death
|
Low GRADE |
The use of pessary may result in little to no difference in perinatal death compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
5. Composite morbidity/mortality
|
Very low GRADE |
The evidence is very uncertain about the effect of pessary on composite outcome of neonatal morbidity and mortality compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
6. RDS
|
Low GRADE |
The use of pessary may result in little to no difference in neonatal respiratory distress syndrome compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
7. NEC
|
Low GRADE |
The use of pessary may result in little to no difference in necrotizing enterocolitis compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
8. IVH
|
Low GRADE |
The use of pessary may result in little to no difference in intraventricular hemorrhage compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
9. Sepsis
|
Low GRADE |
The use of pessary may result in little to no difference in neonatal sepsis compared to no pessary in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Conde-Agudelo, 2020 |
2.2 Pessary compared to Progesterone
|
The evidence is very uncertain about the effect of the use of pessary on spontaneous preterm birth (<28, <34, <37 weeks) compared to progesterone in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Cruz-Melguizo, 2018 |
|
Very low GRADE |
The evidence is very uncertain about the effect of the use of pessary on perinatal death compared to progesterone in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Cruz-Melguizo, 2018 |
|
Very low GRADE |
The evidence is very uncertain about the effect of the use of pessary on composite adverse neonatal outcome compared to progesterone in pregnant women with a singleton gestation and cervical length ≤25mm.
Sources: Cruz-Melguizo, 2018 |
Samenvatting literatuur
PICO 1- Cerclage versus no cerclage/pessary/progesterone
Description of studies
The systematic review and network meta-analysis of Jarde (2019) was conducted to compare the relative effects of different types and routes of administration of progesterone, cerclage, and pessary at preventing preterm birth in at-risk women overall and in specific populations.
Medline, EMBASE, CINAHL, Cochrane CENTRAL, and Web of Science were searched up to January 2018. Randomised trials of progesterone, cerclage or pessary for preventing preterm birth in at-risk singleton pregnancies were included (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Otsuki, 2016; Keeler, 2009).
Jarde (2019) reported separate analyses for women with a previous preterm birth and women with a cervical length ≤25 mm.
The systematic review of Conde-Agudelo (2018) was an update of a meta-analysis (Conde-Agudelo, 2013), an adjusted indirect comparison meta-analysis of vaginal progesterone vs cerclage using placebo/no cerclage as the common comparator. The aim of the review was to compare the efficacy of vaginal progesterone and cerclage in preventing preterm birth and adverse perinatal outcomes in women with a singleton gestation, previous spontaneous preterm birth, and a midtrimester sonographic short cervix. The review included data (post hoc analysis; subgroups) from studies that reported on women with cervical length < 25mm and previous preterm birth. MEDLINE, EMBASE, LILACS, and CINAHL were searched from their inception to March 2018 as well as Cochrane databases, bibliographies, and conference proceedings. The review included randomized controlled trials comparing vaginal progesterone to placebo/no treatment or cerclage to no cerclage in women with a singleton gestation, previous spontaneous preterm birth, and a sonographic cervical length <25 mm. Primary outcomes were preterm birth <35 weeks of gestation and perinatal mortality.
In the analysis of the literature data from five studies were included that compared cerclage versus no cerclage (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Owen 2009).
The systematic review of Berghella (2017) was an individual patient data (IPD) meta-analysis of five RCTs (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Otsuki, 2016), reporting on 419 women. The aim of this systematic review and meta-analysis was to quantify the efficacy of cervical cerclage in preventing preterm birth (PTB) in asymptomatic singleton pregnancies with a short mid-trimester cervical length (CL) on transvaginal sonography (TVS) and without prior spontaneous preterm birth.
Electronic databases were searched from inception of each database until February 2017. All randomized controlled trials of asymptomatic singleton pregnancies without prior spontaneous PTB, found to have short cervical length < 25 mm on mid-trimester TVS and then randomized to management with either cerclage or no cerclage, were included.
Trials included in the systematic reviews (Jarde, 2019; Conde-Agudelo, 2018; Berghella, 2017)
Otsuki (2016) is a randomised controlled trial to assess the effects of ultrasound indicated cervical cerclage in the mid-trimester to prevent preterm birth in women who have no signs of infection or inflammation of the lower genital tract. Women with a short cervical length < 25 mm between 16 and 26 weeks of gestation were randomly assigned to receive a Shirodkar cerclage (n=34), McDonald cerclage (n=34), or bedrest (no cerclage) (n=30). History of preterm birth in the cerclage group was 13% (n/N =9/68) and 17% in the control group (n/N= 5/30).
Owen (2009) is a randomised controlled trial to assess cerclage to prevent recurrent preterm birth in women with short cervix. Women with prior spontaneous preterm birth <34 weeks were screened for short cervix, and randomly assigned to cerclage (n=158) or no cerclage (n=153) if cervical length was <25 mm.
Berghella (2004) is a randomised controlled trial comparing the efficacy of cerclage and bed rest versus bed rest only for the prevention of preterm birth in women with a short cervix found on transvaginal ultrasound examination. Women with at least 1 high-risk factor for preterm birth (≥ 1 preterm birth at < 35 weeks of gestation, ≥ 2 curettages, diethylstilbestrol exposure, cone biopsy, Müllerian anomaly, or twin gestation) were screened with transvaginal ultrasonography of the cervix every 2 weeks from 14 weeks of gestation to 23 weeks 6 days of gestation. Enrolment was offered to both asymptomatic women who were at high risk and who were identified to have short cervix (<25 mm) or significant funnelling (>25%) and non-screened women who were at low risk and who were identified incidentally. Women were assigned randomly to receive McDonald cerclage (n=31) or bed rest only (n=30).
To (2004) is a multicentre randomised controlled trial to investigate whether, in women with a short cervix identified by routine transvaginal scanning at 22-24 weeks' gestation, the insertion of a Shirodkar suture reduces early preterm delivery. Cervical length was measured in 47.123 women. The cervix was 15 mm or less in 470, and 253 (54%) of these women participated in the study and were randomised to cervical cerclage (n=127) or to expectant management (n=126). Primary outcome was the frequency of delivery before 33 completed weeks (231 days) of pregnancy.
Althuisius (2001) is a randomised controlled trial that compared preterm delivery rates (before 34 weeks of gestation) and neonatal morbidity and mortality in patients with risk factors or symptoms of cervical incompetence managed with therapeutic McDonald cerclage and bed rest (n=19) versus bed rest alone (n=16). Risk factors for cervical incompetence included previous preterm delivery before 34 weeks of gestation that met clinical criteria for the diagnosis of cervical incompetence, previous preterm premature rupture of membranes before 32 weeks of gestation, history of cold knife conization, diethylstilbestrol exposure, and uterine anomaly. When a cervical length of <25 mm was measured before a gestational age of 27 weeks, a randomization for therapeutic cerclage and bed rest (cerclage group) or bed rest alone (bed rest group) was performed.
Rust (2001) is a randomised controlled trial included patients between 16 and 24 weeks of gestation with dilation of the internal os and either prolapse of membranes >25% or cervix <25 mm (history of PTB not considered). Patients were randomly assigned to McDonald cerclage (n=55) or no cerclage (n=58).
Before randomization, all patients were treated identically with an amniocentesis, multiple urogenital cultures, and therapy with indomethacin and clindamycin for 48 to 72 hours.
Keeler (2009) included patients with a short cervix (≤25 mm) on transvaginal ultrasound between 16 and 24 weeks’ gestation. Patients were randomly assigned to treatment with McDonald cerclage (n=42) or weekly intramuscular injections of 17 ahydroxyprogesterone caproate (17OHP-C, 250mg/week) (n=37). The primary outcome of this study was spontaneous preterm birth (PTB) prior to 35 weeks’ gestation. A post hoc analysis of patients with a prior PTB was performed.
Results
1.1 Comparison Cerclage versus no cerclage
Outcome 1- preterm birth < 28 weeks
- Preterm birth < 28 weeks, cervical length ≤25mm (previous preterm birth not considered)
Jarde (2019) did not report the outcome preterm birth < 28 weeks.
- Preterm birth < 28 weeks, CL < 25mm, history of preterm birth ≥1
Conde-Agudelo (2018) included 5 studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Owen 2009) that reported the outcome preterm birth <28 weeks. The use of cerclage in women with a singleton gestation, previous spontaneous preterm birth, and a cervical length <25 mm in the midtrimester was associated with a lower risk of preterm birth <28 weeks of gestation (pooled RR 0.64, 95% CI 0.43 to 0.96)
c. Preterm birth <28 weeks, cervical length <25mm, no history of preterm birth
Berghella (2017) included 5 studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Otsuki, 2016) that reported the outcome preterm birth < 28 weeks. Preterm birth <28 weeks was reported in 11.6% (n/N= 26/224) in the cerclage group and in 11.3% (n/N=22/195) in the control group (pooled RR 1.55, 95%CI 0.68 to 1.93).
Outcome 2- Preterm birth <34 weeks
- Preterm birth < 34 weeks, cervical length ≤25mm (previous preterm birth not considered)
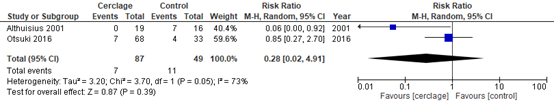
The systematic review of Jarde (2019) included 2 studies (Althuisius, 2001; Otsuki, 2016) (n=136) that reported the outcome preterm birth <34 weeks. Preterm birth < 34 weeks was reported in 7/87 in the group cerclage and 11/49 in the control group (pooled RR 0.28 95%CI 0.02 to 4.19).
Figure 5.1 Outcome spontaneous preterm birth <34 weeks comparison: cerclage versus no cerclage in women with singleton gestations and a cervical length ≤25 mm
Source: Jarde, 2019, Z: p-value of the pooled effect; df: degrees of freedom; I2: statistical heterogeneity; CI: confidence interval.
Conde-Agudelo (2018) did not report the outcome preterm birth < 34 weeks, therefore the outcome < 32 weeks is described. Five trials (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Owen 2009) reported the outcome preterm birth <32 weeks. The use of cerclage in women with a singleton gestation, previous spontaneous preterm birth, and a cervical length <25 mm in the midtrimester was associated with a lower risk of preterm birth <32 weeks (pooled RR 0.66 95% CI 0.48 to 0.91), with 19% (n/N=48/250) in the cerclage group and 30% (n/N=75/254) in the control group.
- Preterm birth <34 weeks, cervical length <25mm, no history of preterm birth
Berghella (2017) included five studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Otsuki, 2016) that reported the outcome preterm birth < 34 weeks. There was a small difference in the risk of preterm birth with 20.1% (n/N= 45/224) in the group cerclage and 25.1% (n/N=49/195) in the group no cerclage (pooled RR 0.89, 95%CI 0.63 to 1.27).
Outcome 3- preterm birth < 37 weeks
- Preterm birth < 37 weeks, cervical length <25mm (preterm birth not considered)
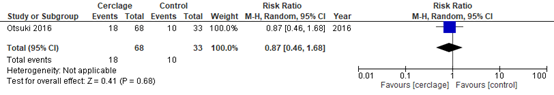
The systematic review of Jarde (2019) included a single trial (n=101) that reported the outcome preterm birth <37 weeks (Otsuki, 2016). Otsuki (2016) reported a small difference in preterm birth <37 weeks between the group cerclage and the control group (RR 0.87 95%CI 0.46 to 1.68).
Figure 5.2 Outcome spontaneous preterm birth <37 weeks comparison: cerclage versus no cerclage in women with singleton gestations and a cervical length ≤25 mm
Source: Jarde, 2019, Z: p-value of the pooled effect; df: degrees of freedom; I2: statistical heterogeneity; CI: confidence interval.
- Preterm birth < 37 weeks, CL < 25mm, history of preterm birth ≥1
Conde-Agudelo (2018) included 5 studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Owen 2009) that reported on the outcome preterm birth <37 weeks. The use of cerclage in women with a singleton gestation, previous spontaneous preterm birth, and a cervical length <25 mm in the midtrimester was associated with a lower risk of preterm birth <37 weeks (pooled RR 0.70 95% CI, 0.58-0.83), with 42% (105/250) in the cerclage group and 61% (154/254) in the control group.
- Preterm birth <37 weeks, cervical length <25mm, no history of preterm birth
Berghella (2017) included 5 studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Otsuki, 2016) that reported the outcome preterm birth < 37 weeks. Preterm birth <37 weeks was reported in 36.2% (n/N= 481/224) in the cerclage group and in 41.0% (n/N=80/195) in the control group (pooled RR 0.93, 95%CI 0.73 to 1.18). This is no clinically relevant difference.
Outcome 4- Neonatal death
- Neonatal death, cervical lenght ≤ 25mm (preterm birth not considered)
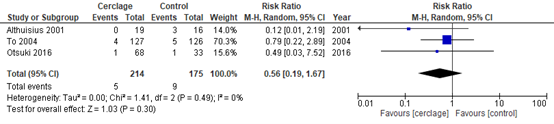
The systematic review of Jarde (2019) included 3 studies (n=389) that reported the outcome neonatal death (Althuisius, 2001; To, 2005; Otsuki, 2016). Neonatal death was reported in 2% (n/N=5/214) in the cerclage group and in 5% (n/N=9/175) in the control group (pooled RR 0.56, 95%CI 0.19 to 1.67).
Figure 5.3 Outcome neonatal death comparison: cerclage versus no cerclage in women with singleton gestations and a cervical length ≤25 mm
Source: Jarde, 2019, Z: p-value of the pooled effect; df: degrees of freedom; I2: statistical heterogeneity; CI: confidence interval.
- Perinatal mortality, cervical length <25mm, history of preterm birth
Conde-Agudelo (2018) included 5 studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Owen 2009) that reported the outcome perinatal mortality. Perinatal mortality was reported in 9% (22/250) in the cerclage group and in 14% (35/254) in the control group (pooled RR 0.65, 95%CI 0.40 to 1.07).
- Neonatal death, cervical length <25mm, no history of preterm birth
Berghella (2017) included 4 studies (Rust, 2001; Berghella, 2004; Althuisius, 2001; Otsuki, 2016) that reported the outcome neonatal death. Neonatal death was reported in 5.9% (n/N= 7/118) in the cerclage group and in 6.5% (n/N=6/92) in the control group (pooled RR 1.08, 95%CI 0.41 to 2.86).
Outcome 5- Composite outcome neonatal mortality/morbidity
- Composite outcome neonatal mortality/morbidity, cervical length <25mm, history of preterm birth not considered
Not reported
- Composite outcome neonatal mortality/morbidity, cervical length <25mm, history of preterm birth
Conde-Agudelo (2018) included 5 studies that reported the outcome perinatal morbidity and mortality (Rust, 2001; Berghella, 2004; Althuisius, 2001; To, 2004; Owen 2009). The composite outcome was defined as the occurrence of any of the following neonatal morbidities; respiratory distress syndrome; grade III/IV intraventricular haemorrhage; necrotizing enterocolitis; neonatal sepsis; bronchopulmonary dysplasia, or perinatal death. The use of cerclage in women with a singleton gestation, previous spontaneous preterm birth, and a cervical length <25 mm in the midtrimester was associated with a significantly lower risk of composite perinatal morbidity and mortality with 16% in the group cerclage (n/N=39/250), and 25% in the group no cerclage (n/N=63/254) (RR 0.64, 95% CI 0.45 to 0.91).
- Composite outcome neonatal mortality/morbidity, cervical length <25mm, no history of preterm birth
Not reported
Outcome 6- Respiratory distress syndrome
- Respiratory distress syndrome, cervical length <25mm, history of preterm birth not considered
Not reported
- Respiratory distress syndrome, cervical length <25mm, history of preterm birth
Conde-Agudelo (2018) included 4 studies […] that reported the outcome RDS. RDS was reported in 6% (13/207) in the cerclage group and in 11% (21/196) in the control group (pooled RR 0.61, 95%CI 0.32 to 1.19).
- Respiratory distress syndrome, cervical length <25mm, no history of preterm birth
Berghella (2017) included 2 studies (Berghella, 2004; Althuisius, 2001) that reported the outcome respiratory distress syndrome. RDS was reported in 14.3% (n/N= 2/14) in the cerclage group and in 12.5% (n/N=2/16) in the group no cerclage (pooled RR 1.33 95%CI 0.23 to 7.74).
Outcome 7- Necrotizing enterocolitis
- NEC, cervical length <25mm, history of preterm birth not considered
Not reported
- NEC, cervical length <25mm, history of preterm birth
Conde-Agudelo (2018) included 4 studies […] that reported the outcome NEC. NEC was reported in 1% (1/207) in the cerclage group and in 1% (2/196) in the control group (pooled RR 0.62 95%CI 0.08 to 4.67).
- NEC, cervical length <25mm, no history of preterm birth
Berghella (2017) included 2 studies (Berghella, 2004; Althuisius, 2001) that reported the outcome NEC. There were no cases of NEC reported in both groups; 0% (n/N= 0/14) in the group cerclage and 0% (n/N=0/16) in the group no cerclage.
Outcome 8- Intraventricular haemorrhage
- Intraventricular haemorrhage, cervical length <25mm, history of preterm birth not considered
Jarde (2019) included 1 study (To, 2004) that reported the outcome intraventricular haemorrhage/periventricular haemorrhage. To (2004) reported 1/123 (1%) IVH/PVH in the cerclage group and 2/121 (2%) IVH/PVH in the expectant group (RR 0.49 95%CI 0.04 to 5.45, p=0.620).
- Intraventricular haemorrhage, cervical length <25mm, history of preterm birth
Conde-Agudelo (2018) included 4 studies […] that reported the outcome Grade III/IV intraventricular haemorrhage. There was no statistically significant difference in IVH between the group cerclage 0% (0/207) and the control group 2% (4/196) (pooled RR 0.28 95%CI 0.05 to 1.64).
- Intraventricular haemorrhage, cervical length <25mm, no history of preterm birth
Berghella (2017) included 2 studies (Berghella, 2004; Althuisius, 2001) that reported the outcome IVH. There was no significant difference in the risk of IVH with 7.1% (n/N= 1/14) in the group cerclage and 0% (n/N=0/16) in the group no cerclage (RR 3.90 95%CI 0.18 to 85.93).
Outcome 9- Neonatal sepsis
- Neonatal sepsis, cervical length <25mm, history of preterm birth not considered
Not reported
- Neonatal sepsis, cervical length <25mm, history of preterm birth
Conde-Agudelo (2018) included 4 studies […] that reported the outcome neonatal sepsis. Neonatal sepsis was reported in 4% (8/207) in the cerclage group and in 9% (17/196) in the control group (Pooled RR 0.47 95%CI 0.21 to 1.05).
- Neonatal sepsis, cervical length <25mm, no history of preterm birth
Berghella (2017) included 2 studies (Berghella, 2004; Althuisius, 2001) that reported the outcome neonatal sepsis. Neonatal sepsis was reported in 14.3% (n/N= 2/14) in the cerclage group and in 12.5% (n/N=2/16) in the group no cerclage (RR 1.33 95%CI 0.23 to 7.74).
Level of evidence of the literature
Studies with a randomized, placebo-controlled design start at a high GRADE, post hoc analysis are considered observational data and start at a low GRADE.
Outcome 1. Spontaneous preterm birth < 28 weeks
The level of evidence regarding the outcome measure spontaneous preterm birth <28 weeks in women with a cervical length ≤25 mm, and history of preterm birth started low and was downgraded by to a very low GRADE because of imprecision (-1) (confidence interval crossing the level of clinical relevance).
The level of evidence regarding the outcome measure spontaneous preterm birth <28 weeks in women with a cervical length ≤25 mm, and no history of preterm birth was downgraded to a low GRADE because of risk of bias and imprecision (-2) (wide confidence interval).
Outcome 2. Spontaneous preterm birth < 34 weeks
The level of evidence regarding the outcome measure spontaneous preterm birth <34 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of heterogeneity (-1) and imprecision (-2) (wide confidence intervals, and low number of events).
The level of evidence regarding the outcome measure spontaneous preterm birth <32 weeks in women with a cervical length ≤25 mm, and history of preterm birth was downgraded by to a low GRADE because of risk of bias and imprecision (-1) (wide confidence intervals).
The level of evidence regarding the outcome measure spontaneous preterm birth <34 weeks in women with a cervical length ≤25 mm, and no history of preterm birth was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 3. Spontaneous preterm birth < 37 weeks
The level of evidence regarding the outcome measure spontaneous preterm birth <37 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by two levels to a low GRADE because of imprecision (-2) (single study, wide confidence intervals, and low number of events).
The level of evidence regarding the outcome measure spontaneous preterm birth <37 weeks in women with a cervical length ≤25 mm, and history of preterm birth was downgraded to a low GRADE because of risk of bias and imprecision (-1) (low number of events).
The level of evidence regarding the outcome measure spontaneous preterm birth <37 weeks in women with a cervical length ≤25 mm, and no history of preterm birth was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 4. Neonatal death
The level of evidence regarding the outcome measure neonatal death in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals, and low number of events).
The level of evidence regarding the outcome measure perinatal mortality in women with a cervical length ≤25 mm, and history of preterm birth was downgraded to a very low GRADE because of risk of bias (-1) and imprecision (-2) (wide confidence intervals and low number of events).
The level of evidence regarding the outcome measure neonatal death in women with a cervical length ≤25 mm, and no history of preterm birth was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals and low number of events).
Outcome 5. Composite outcome neonatal mortality/morbidity
The level of evidence regarding the outcome measure composite outcome neonatal mortality/morbidity in women with a cervical length ≤25 mm, and previous preterm birth started low and was downgraded to a very low GRADE because of imprecision (-1) (confidence interval crossing the borders of clinical relevance).
Outcome 6. Respiratory distress syndrome
The level of evidence regarding the outcome measure respiratory distress syndrome in women with a cervical length ≤25 mm, and previous preterm birth started low and was downgraded to a very low GRADE because of imprecision (-1) (confidence interval crossing the borders of clinical relevance).
The level of evidence regarding the outcome measure respiratory distress syndrome in women with a cervical length ≤25 mm, and no previous preterm birth started low and was downgraded to a very low GRADE because of risk of bias (-1) and imprecision (-2) (low number of events, confidence interval crossing the borders of clinical relevance).
Outcome 7- Necrotizing enterocolitis
The level of evidence regarding the outcome measure necrotizing enterocolitis in women with a cervical length ≤25 mm, and previous preterm birth started low and was downgraded to a very low GRADE because of imprecision (-2) (low number of events).
No level of evidence was determined for the outcome measure necrotizing enterocolitis in women with cervical length ≤25 mm, and no previous preterm (no GRADE); no cases of NEC reported in both groups (cerclage versus no cerclage).
Outcome 8. Intraventricular haemorrhage
The level of evidence regarding the outcome measure intraventricular haemorrhage in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by two levels to a very low GRADE because of imprecision (-3) (one trial. wide confidence intervals, and low number of events).
The level of evidence regarding the outcome measure intraventricular haemorrhage in women with a cervical length ≤25 mm, and history of preterm birth was downgraded to a very low GRADE because of risk of bias (-1) and imprecision (-2) (wide confidence intervals and low number of events).
The level of evidence regarding the outcome measure intraventricular haemorrhage in women with a cervical length ≤25 mm, and no history of preterm birth was downgraded by two levels to a very low GRADE because of imprecision (-3) (wide confidence intervals and low number of events).
Outcome 9. Neonatal sepsis
The level of evidence regarding the outcome measure neonatal sepsis in women with a cervical length ≤25 mm, and history of preterm birth was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals and low number of events).
The level of evidence regarding the outcome measure neonatal sepsis in women with a cervical length ≤25 mm, and no history of preterm birth was downgraded to a very low GRADE because of risk of bias (-1) and imprecision (-2) (wide confidence intervals and low number of events).
1.2 Cerclage versus progesterone
A single study (Keeler, 2009) was included in the systematic review of Jarde (2019) that compared treatment with cerclage to progesterone in women with a short cervix (≤25 mm).
Outcome 1- Spontaneous preterm birth <28 weeks
Keeler (2009) did not report the outcome spontaneous preterm birth <28 weeks
Spontaneous preterm birth prior to 28 weeks' gestation occurred in 23.8% (10/42) in the cerclage group and in 18.9% (7/37) of the 17OHP-C group (RR 0.79 95% CI 0.34 to 1.88).
Outcome 2- Spontaneous preterm birth <34 weeks
Keeler (2009) did not report the outcome spontaneous delivery before 34 weeks of gestation, therefore the outcome preterm birth before 32 weeks is described.
PTB <32 weeks, cervical length <25mm, history of preterm birth not considered
Spontaneous PTB prior to 35 weeks' gestation occurred in 35.7% (15/42) in the cerclage group and in 35.1% (13/37) of the 17OHP-C group (RR 0.98 95% CI 0.54 to 1.79)
Outcome 3- Spontaneous preterm birth <37 weeks
One trial (Keeler, 2009) reported the spontaneous preterm birth prior to 37 weeks' gestation. PTB <37 weeks occurred in 52% (22/42) in the cerclage group and in 63% (22/35) in the 17OHP-C group (RR 0.75 95%CI 0.31 to 1.83).
- PTB <35 weeks, cervical length <25mm, history of preterm birth not considered
Spontaneous PTB prior to 35 weeks' gestation occurred in 38.1% (16/42) in the cerclage group and in 43.2% (16/37) of the 17OHP-C group (RR 1.14 95% CI 0.67 to 1.93).
- PTB < 35 weeks, cervical length <25mm, history of preterm birth
A post hoc analysis of patients with a prior PTB showed no difference in spontaneous PTB <35 weeks between groups (no data reported, Keeler, 2009).
Outcome 4- Perinatal mortality
Keeler (2009) reported the outcome perinatal death, which included any stillbirth or neonatal death during the study period. Perinatal death was reported in 11.9% in the cerclage group (n/N=5/42) and in 10.8% in the group 17OHP-C (n/N=4/37) (RR 1.10 95% CI 0.32 to 3.80).
Outcome 5- Composite outcome neonatal morbidity
Keeler (2009) reported the outcome severe morbidity defined as life threatening morbidity including respiratory distress syndrome requiring mechanical ventilation 24h, intraventricular haemorrhage, neonatal sepsis, or necrotizing enterocolitis.
Severe morbidity was reported in 21.4% in the cerclage group (n/N=9/42) and in 18.9% in the group 17OHP-C (n/N=7/37) (RR 1.17 95%CI 0.39 to 3.53).
Level of evidence of the literature
Studies with a randomized, placebo-controlled design start at a high GRADE.
The level of evidence regarding the outcome measure spontaneous preterm birth <34 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1) (early termination of the trial), indirectness (preterm birth <32 weeks was reported), and imprecision (-2) (single trial, n=77, wide confidence intervals).
The level of evidence regarding the outcome measure spontaneous preterm birth <37 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1), and imprecision (-2) (single trial, n=77, wide confidence intervals).
The level of evidence regarding the outcome measure spontaneous preterm birth <37 weeks in women with a cervical length ≤25 mm, and history of preterm birth started low (posthoc analysis) and was downgraded to a very low GRADE because of risk of bias (-1), indirectness (-1) (outcome <35 weeks was reported) and imprecision (-2) (single trial, wide confidence intervals).
The level of evidence regarding the outcome measure perinatal mortality in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1), and imprecision (-2) (single trial, n=77, wide confidence intervals).
The level of evidence regarding the outcome measure composite outcome neonatal morbidity in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1), and imprecision (-2) (single trial, n=77, wide confidence intervals).
PICO-2 Pessary compared to no pessary/cerclage/progesterone
Description of studies
The systematic review and meta-analysis of Conde-Agudelo (2020) is a Cochrane review that searched MEDLINE, EMBASE, POPLINE, LILACS, CINAHL, the Cochrane Central Register of Controlled Trials, clinical trial registries (all from their inception to October 31,
2019) without language restriction. The review included RCTs comparing cervical pessary with standard care (no pessary) or alternative interventions (such as vaginal progesterone or cervical cerclage) in asymptomatic women at high risk for preterm birth (such as those with a midtrimester sonographic short cervix, history of preterm birth, multiple gestation, and uterine anomalies or excisional cervical procedures) with the aim of preventing preterm birth and/or adverse perinatal outcomes. In the literature analysis six studies from this systematic review are described that included and reported data of women with a cervical length ≤25mm (Goya, 2012; Hui, 2013; Nicolaides, 2016a; Saccone, 2017; Dugoff, 2018; Cruz-Melguizo, 2018).
In three studies (Dugoff, 2018; Nicolaides, 2016a; Saccone 2017) comparing pessary to no pessary, the intervention and control included concomitant use of progesterone in varying percentages of the study population (44-91%).
Pessary compared to no pessary
Goya (2012) is a randomized controlled trial, that included women undergoing cervical length screening at 18-22 weeks of gestation and allocated those with a cervical length ≤25 mm to the Arabin pessary (n=192) or expectant management (n=193). At randomization the mean cervical length was 19 mm and mean gestational age 22.3 weeks. Overall, 11% of women had a prior preterm birth.
Hui (2013) is a randomized controlled trial that enrolled women with a singleton gestation and a cervical length <25 mm (at 20 – 24 weeks) and randomly allocated them to Arabin pessary (n=53) or no pessary (n=55). At randomization the mean cervical length was 20.1 mm and the mean gestational age 21.9 weeks. There was no concomitant use of progesterone in either group.
Nicolaides (2016), a multinational study, enrolled 924 women across 16 hospitals and studied women with a cervical length of ≤25 mm (at 20-25 weeks) of gestation randomly allocated to pessary (n=460) or expectant management (n= 464). The mean cervical length at study entry was 20 mm. Women with a cervical length <15 mm were also treated with 200 mg of vaginal progesterone nightly, regardless of treatment group assignment, with 45% of overall participants receiving progesterone (concomitant use of vaginal progesterone in the pessary group 44%, and 47% in the no pessary group).
Overall, 17% of the participants had a history of preterm birth. While per protocol the pessary was to remain in place until 37 weeks of gestation, in 47 women (11%), the pessary was removed prior to 34 weeks of gestation because of vaginal discharge, discomfort, or bleeding.
Saccone (2017) was a randomized controlled trial that enrolled women with a singleton gestation, no previous spontaneous preterm birth, and a cervical length ≤25 mm (at 18 – 24 weeks), and randomly allocated them to Arabin pessary (n=150) or no pessary (n=150). At randomization the mean cervical length was 12.0 mm and the mean gestational age 22.4 weeks. Concomitant use of progesterone in the pessary group was 89% and 83% in the no pessary group.
Dugoff (2018) was a randomized controlled trial and enrolled women with a singleton gestation, no previous spontaneous preterm birth, and a cervical length ≤25 mm (at 18 – 24 weeks), and randomly allocated them to Bioteque cup pessary (n=60) or no pessary (n=58). At randomization the median cervical length was 17.6 mm in the pessary group and 19.0 in the no pessary group, and mean gestational age 21.1 weeks. Concomitant use of progesteron in the pessary group was 84%, and 91% in the no pessary group.
Pessary compared to progestrone
Cruz-Melguizo (2018) is a randomized non-inferiority trial that compared the efficacy of Arabin pessary (n=125) and vaginal progesterone 200 mg/day (n=118) in women with a singleton gestation and a cervical length ≤25 mm at 19-22 weeks of gestation.
Concomitant use of vaginal progesterone in the pessary group was 5%.
Results
Pessary compared to no pessary
Outcome 1 -Spontaneous preterm birth <28 weeks
Three of the included studies in the review of Conce-Agudelo (2020) reported the outcome spontaneous preterm birth <28 weeks (Nicolaides, 2016; Saccone, 2017, Dugoff, 2018, n=4160). Spontaneous preterm birth <28 weeks with the use of pessary was reported in 5.1% (44/865) compared to no pessary 6.0% (52/865) (pooled RR 0.76 95%CI 0.37 to 1.54, p= 0.44, I2=65%).
Outcome 2- spontaneous preterm birth <34 weeks
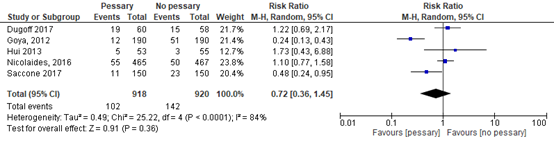
Five of the included studies in the review of Conde-Agudelo (2020) reported the outcome spontaneous preterm birth <34 weeks (Goya, 2012; Hui, 2013; Nicolaides, 2016a; Saccone, 2017; Dugoff, 2018). There was no significant reduction of the risk of spontaneous preterm birth < 34 weeks with the use of pessary compared to no pessary in women with a singleton pregnancy with a cervical length ≤25 mm (pooled data 11% pessary group compared to 15% no pessary group; RR 0.72 95% CI 0.36 to 1.45, P=0.36, I2=84%) (Figure 5.4)
Figure 5.4. Outcome spontaneous preterm birth <34 weeks comparison: cervical pessary versus no pessary in women with singleton gestations and a cervical length ≤25 mm
Source: Conde-Agudelo, 2020, Z: p-value of the pooled effect; df: degrees of freedom; I2: statistical heterogeneity; CI: confidence interval.
1.1 Subgroup obstetric history- no previous preterm birth
Three studies reported the outcome measure spontaneous preterm birth < 34 weeks in a (subgroup of) women with no previous preterm birth (Nicolaides, 2016; Saccone, 2017; Dugoff, 2018). Spontaneous preterm birth < 34 was reported in 12.9% (78/605) in the group pessary, and 12.2% (72/591) in the group no pessary (RR 0.97 95%CI 0.54 to 1.76).
1.2 Subgroup obstetric history – ≥1 previous preterm birth
One study reported the outcome measure spontaneous preterm birth < 34 weeks in a subgroup women with previous preterm birth (Nicolaides, 2016). Spontaneous preterm birth < 34 was reported 10.0% (7/70) in the group pessary, and 19.0% (16/84) in the group no pessary (RR 0.53 95%CI 0.23 to 1.20).
Outcome 3- Spontaneous preterm birth < 37 weeks
Four of the included studies in the review of Conde-Agudelo (2020) reported the outcome spontaneous preterm birth <37 weeks (Goya, 2012; Nicolaides, 2016; Saccone, 2017, Dugoff, 2018).
Spontaneous preterm birth <37 weeks with the use of pessary compared to no pessary in women with a singleton pregnancy and cervical length <25mm, was reported in 22.7% (196/865) in the pessary group and in 32.6% (282/865) in the no pessary group (pooled RR 0.71 95% CI 0.41 to 1.24, favouring pessary, p= 0.23, I2=91%)
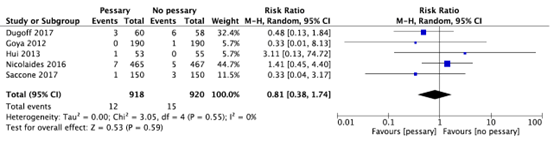
Outcome 4. Perinatal death
Conde-Agudelo (2020) included five trials (Goya, 2012; Hui, 2013; Nicolaides, 2016; Saccone, 2017, Dugoff 2018) that reported on the outcome perinatal death. Perinatal death was reported in 1.3% (12/918) in the pessary group and 1.6% (15/920) in the control group (pooled RR 0.81 95%CI 0.38 to 1.74, p=0.59) (Figure 5.5).
Figure 5.5. Outcome perinatal death: cervical pessary versus no pessary in women with singleton gestations and a cervical length ≤25 mm
Source: Conde-Agudelo, 2020, Z: p-value of the pooled effect; df: degrees of freedom; I2: statistical heterogeneity; CI: confidence interval.
Outcome 5. Composite outcome neonatal mortality/morbidity
Four studies reported a composite outcome (Goya 2012; Nicolaides, 2016; Saccone, 2017; Dugoff, 2018), defined as any composite adverse neonatal outcome (Conde-Agudelo, 2020).
Composite outcome was reported in the group pessary in 8.0% (69/865) and in the group no pessary in 13.2% (114/865) (pooled RR 0.59 95%CI 0.28 to 1.27, p=0.18, I2=83).
Outcome 6. Respiratory distress syndrome
Conde-Agudelo (2020) included 5 trials (Goya, 2012; Hui, 2013; Nicolaides, 2016; Saccone, 2017; Dugoff, 2018) that reported on the outcome respiratory distress syndrome.
Respiratory distress syndrome was reported in 6.8% (62/918) in the pessary group and 9.8% (90/920) in the control group (pooled RR 0.72 95% CI 0.36 to 1.43, p=0.35).
Outcome 7. Necrotizing enterocolitis
Conde-Agudelo (2020) included 4 trials (Goya, 2012; Nicolaides, 2016; Saccone, 2017; Dugoff, 2018) that reported on the outcome necrotizing enterocolitis.
Necrotizing enterocolitis was reported in 1.3% (11/865) in the pessary group and 1.2% (10/856) in the control group (pooled RR 1.15 95% CI 0.47 to 2.79, p=0.76).
Outcome 8. Intraventricular haemorrhage
Conde-Agudelo (2020) included 5 trials (Goya, 2012; Hui, 2013; Nicolaides, 2016; Saccone, 2017; Dugoff, 2018) that reported on the outcome intraventricular haemorrhage.
Intraventricular haemorrhage was reported in 1.9% (17/918) in the pessary group and 1.5% (14/920) in the control group (pooled RR 1.16 95% CI 0.48 to 2.80, p=0.73).
Outcome 9. Neonatal sepsis
Conde-Agudelo (2020) included 5 trials (Goya, 2012; Hui, 2013; Nicolaides, 2016; Saccone, 2017; Dugoff, 2018) that reported on the outcome neonatal sepsis.
Neonatal sepsis was reported in 5.3% (49/918) in the pessary group and 6.1% (56/920) in the control group (pooled RR 0.80 95% CI 0.46 to 1.40, p=0.44).
Level of evidence of the literature
Studies with a randomized, placebo-controlled design start at a high GRADE.
Outcome 1.
The level of evidence regarding the outcome measure spontaneous preterm birth <28 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 2.
The level of evidence regarding the outcome measure spontaneous preterm birth <34 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of inconsistency (-1), and imprecision (-2) (wide confidence intervals).
The level of evidence regarding the outcome measure spontaneous preterm birth <34 weeks in women with a cervical length ≤25 mm, no history of preterm birth was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
The level of evidence regarding the outcome measure spontaneous preterm birth <34 weeks in women with a cervical length ≤25 mm, and a history of >=1 preterm birth was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 3.
The level of evidence regarding the outcome measure spontaneous preterm birth <37 weeks in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a low GRADE because of inconsistency (-1) and imprecision (-2) (wide confidence intervals).
Outcome 4.
The level of evidence regarding the outcome measure perinatal death in women with a cervical length ≤25 mm was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 5.
The level of evidence regarding the composite outcome measure neonatal mortality/morbidity in women with a cervical length ≤25 mm was downgraded by three levels to a very low GRADE because of inconsistency (-1) and imprecision (-2) (wide confidence intervals).
Outcome 6.
The level of evidence regarding the outcome measure respiratory distress syndrome in women with a cervical length ≤25 mm was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 7.
The level of evidence regarding the outcome measure necrotizing enterocolitis in women with a cervical length ≤25 mm was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 8.
The level of evidence regarding the outcome measure intraventricular hemorrhage in women with a cervical length ≤25 mm was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Outcome 9.
The level of evidence regarding the outcome measure neonatal sepsis in women with a cervical length ≤25 mm was downgraded by two levels to a low GRADE because of imprecision (-2) (wide confidence intervals).
Pessary compared to progesterone
A single trial (n=246) was included in the review of Conde-Agudelo (2020) that compared pessary to progesterone (Cruz-Melguizo, 2018).
Outcome -1 spontaneous preterm birth <28 weeks
Cruz-Melguizo (2018) reported no difference between the pessary group (8.0%, n/N=10/125) and the progesterone group (7.6%, N/N=9/118) (RR 1.05, 95% CI 0.44- 2.49).
Outcome-2 spontaneous preterm birth <34 weeks
Cruz-Melguizo (2018) reported no difference between the pessary group and the progesterone group in the rate of spontaneous delivery before 34 weeks of gestation with 14.2% (18/127) in the pessary group and 14.3% (17/119) in the progesterone group (RR 0.99, 95% CI 0.54 to 1.83). The rate of spontaneous delivery before 34 weeks of gestation was 14% (n=18/127) in the pessary group and 14% (n=17/119) in the progesterone group with a risk difference of -0.11% (95% CI -8.85% to 8.62%; P=.99), that is, noninferiority was not shown for the pessary.
Outcome -3 spontaneous preterm birth <37 weeks
Cruz-Melguizo (2018) reported no difference between the pessary group (22%, n/N=27/125) and the progesterone group (21%, N/N=25/118) (RR 1.02, 95% CI 0.63-1.65).
Outcome -4 perinatal death
Cruz-Melguizo (2018) reported fetal and neonatal death in 5% (6/125) in the pessary group and 3% (3/118) the progesterone group (RR 1.89, 95% CI 0.48-7.38).
Outcome -5 Composite adverse neonatal outcome
Cruz-Melguizo (2018) reported no difference between the pessary group (19%, n/N=24/125) and the progesterone group (17%, n/N=20/118) (RR 1.13, 95% CI 0.66-1.94).
Level of evidence of the literature
Studies with a randomized, placebo-controlled design start at a high GRADE.
The level of evidence regarding the outcome measure spontaneous preterm birth (<37, <34, <28 weeks) in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1) (no intention to treat analysis) and imprecision (-2) (1 trial, n=246 participants, wide confidence intervals).
The level of evidence regarding the outcome measure perinatal death in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1) (no intention to treat analysis) and imprecision (-2) (1 trial, n=246 participants, wide confidence intervals).
The level of evidence regarding the outcome measure composite adverse neonatal outcome in women with a cervical length ≤25 mm (preterm birth not considered) was downgraded by three levels to a very low GRADE because of risk of bias (-1) (no intention to treat analysis) and imprecision (-2) (1 trial, n=246 participants, wide confidence intervals).
Zoeken en selecteren
A systematic review of the literature was performed to answer the following questions:
1. What are the (un)favourable effects of cerclage compared to no cerclage, pessary or progesterone in the prevention of spontaneous preterm birth in woman with singleton pregnancies and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks?
|
P: patients |
woman with a singleton pregnancy and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks |
|
I: intervention |
cerclage |
|
C: control |
no cerclage, pessary, progesterone |
|
O: |
preterm birth (<28 weeks, <34 weeks, <37 weeks), composite outcome of neonatal morbidity and mortality (respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, proven neonatal sepsis, neonatal death), perinatal mortality and neonatal death |
2. What are the (un)favourable effects of pessary compared to no pessary, cerclage or progesterone in the prevention of spontaneous preterm birth in woman with singleton pregnancies and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks?
|
P: patients |
woman with a singleton pregnancy and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks |
|
I: intervention |
pessary |
|
C: control |
no pessary, cerclage, progesterone |
|
O: |
preterm birth (<28 weeks, <34 weeks, <37 weeks), composite outcome of neonatal morbidity and mortality (respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, proven neonatal sepsis, neonatal death), perinatal mortality and neonatal death |
Relevant outcome measures
The guideline development group considered preterm birth <34 weeks, composite outcome of neonatal morbidity and mortality, and neonatal death as critical outcome measures for decision making;
A priori, the working group did define the outcome measures preterm birth: i.e., preterm preterm birth <28 weeks, preterm birth <34 weeks, and preterm birth <37 weeks. When a included study did not report the effect of progesterone on preterm birth <34 weeks, but did report preterm birth <32 weeks or preterm birth <33 weeks, if possible those results were included. The same method was used considering outcome measure preterm birth <37 weeks. If possible, the results of preterm birth <35 weeks or <36 weeks were included.
A priori, the working group did define the outcome measures neonatal morbidity and mortality as a composite outcome measure including respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, proven neonatal sepsis, neonatal death. The working group also reported these outcome measures individually.
The outcome measures neonatal death, perinatal mortality, respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, proven neonatal sepsis were not defined a priori, but the definitions applied in the studies were used.
The working group defined a relative risk ≤0.9 or ≥1.1 as a minimal clinically important difference for preterm birth and ≤0.8 or ≥1.25 as a minimal clinically important difference for all other outcome measures.
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms until October, 16th 2019. The working group was aware of the publication of Conde-Agudelo (2020) who searched until October, 31th 2019. Since the included studies did not change the conclusions and therefore recommendations, the original search until October, 16th 2019 was not updated. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 535 hits. Studies were selected based on the following criteria: women cervical length ≤25 mm, treated with pessary, cerclage compared versus no treatment or progesterone and at least one of the relevant outcome measures reported. Only systematic reviews and meta analyses or randomized controlled trials (RCTs), involving the original study data were included. 17 studies were initially selected based on title and abstract screening. After reading the full text, 13 studies were excluded (see the table with reasons for exclusion under the tab Methods), and four studies were included.
Results
Four systematic reviews and meta-analysis were included in the analysis of the literature (Conde-Agudelo, 2020; Jarde, 2019; Conde-Agudelo; 2018; Berghella, 2017). These reviews included six studies directly comparing cerclage to no cerclage, one study comparing cerclage to progesterone, five studies comparing pessary to no pessary, and one study comparing pessary to progesterone. No studies were included that directly compared cerclage versus pessary. Important study characteristics and results are summarized in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
Referenties
- Berghella, V., Ciardulli, A., Rust, O. A., To, M., Otsuki, K., Althuisius, S., ... & Saccone, G. (2017). Cerclage for sonographic short cervix in singleton gestations without prior spontaneous preterm birth: systematic review and meta?analysis of randomized controlled trials using individual patient?level data. Ultrasound in Obstetrics & Gynecology, 50(5), 569-577.
- Conde-Agudelo, A., Romero, R., Da Fonseca, E., OBrien, J. M., Cetingoz, E., Creasy, G. W., ... & Nicolaides, K. H. (2018). Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: updated indirect comparison meta-analysis. American journal of obstetrics and gynecology, 219(1), 10-25.
- Conde-Agudelo, A., Romero, R., & Nicolaides, K. H. (2020). Cervical pessary to prevent preterm birth in asymptomatic high-risk women: a systematic review and meta-analysis. American Journal of Obstetrics and Gynecology.
- Jarde, A., Lutsiv, O., Beyene, J., & McDonald, S. D. (2019). Vaginal progesterone, oral progesterone, 17?OHPC, cerclage, and pessary for preventing preterm birth in at?risk singleton pregnancies: an updated systematic review and network meta?analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 126(5), 556-567.
Evidence tabellen
Evidencetabellen
Evidence table for systematic review of RCTs and observational studies (intervention studies)
Research question (UV5a): What are the (un)favourable effects of cerclage compared to no cerclage, pessary or progesterone in the prevention of spontaneous preterm birth in woman with singleton pregnancies and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks?
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C)
|
Follow-up |
Outcome measures and effect size |
Comments |
|
Jarde, 2019
|
SR and network meta-analysis of RCTs
Literature search up to January 2018
A: Otsuki, 2016 B: Berghella, 2004 C: To, 2004 D: Althuisius, 2001 E: Rust, 2001 F: Keeler, 2009
Study design: RCT
Setting and Country: A: Japan B: USA C: Multinational D: Netherlands E: USA F: USA
Source of funding and conflicts of interest: Not reported for individual studies.
|
Inclusion criteria SR: Randomised controlled trials comparing progesterone, cerclage or pessary with a control group or another intervention for the prevention of preterm birth and/or associated adverse outcomes in at-risk singleton pregnancies
Exclusion criteria SR: - Studies in which a subgroup of women was already receiving an intervention before randomisation, unless this was based on objective risk factors (e.g. cervical length ≤20 mm) and unless results were reported separately for the groups of women with and without a pre-randomisation intervention - Studies assessing interventions in the context of artificial reproductive therapy, assessing combinations of interventions or interventions for the secondary prevention of preterm birth (e.g. tocolytics in women with contractions) - Non-peer-reviewed literature, studies published only as abstracts and other study designs
40 studies included, but six studies used for the literature analysis
Important patient characteristics at baseline: Gestational age A: 16-26 weeks B: 14-24 weeks C: 22-24 weeks D: <37 weeks E: 16-24 weeks F: 16-24 weeks
Unclear if groups were comparable at baseline
|
Describe intervention:
A: McDonald or Shirodkar B: McDonald C: Shirodkar D: McDonald E: McDonald F: McDonald
|
Describe control:
A: no intervention/treatment as usual B: no intervention/treatment as usual C: no intervention/treatment as usual D: no intervention/treatment as usual E: no intervention/treatment as usual F: 17OHP-C (250 mg/week)
|
End-point of follow-up: Not reported.
For how many participants were no complete outcome data available? Not reported.
|
Outcome measure-1 Preterm birth <34 weeks I: 7/87 (8.0%) C: 11/49 (22%) Pooled RR 0.28, 95% CI 0.02 to 4.19 favouring cerclage
Outcome measure-2 Preterm birth <37 weeks I: 18/68 (26%) C: 10/33 (30%) RR 0.87, 95% CI 0.46 to 1.68 favouring cerclage
Comparison progesterone (ref. F) I: 22/42 (52%) C: 22/35 (63%) RR 0.75, 95%CI 0.31 to 1.83 favouring cerclage
Outcome measure-3 Neonatal death I: 5/214 (2%) C: 9/175 (5%) Pooled RR 0.56, 95%CI 0.19 to 1.67 favouring cerclage
Comparison progesterone (ref. F) I: 5/42 (11.9%) C: 4/37 (10.8%) RR 1.10, 95% CI 0.32 to 3.80 favouring progesterone
Outcome measure-4 Intraventricular haemorrhage I: 1/123 (1%) C: 2/121 (2%) RR 0.49, 95% CI 0.04 to 5.45 favouring cerclage
Outcome measure-5 Preterm birth <28 weeks (comparison with progesterone (ref. F)) I: 10/42 (23.8%) C: 7/37 (18.9%) RR 0.79, 95% CI 0.34 to 1.88 favouring progesterone
Outcome measure-6 Preterm birth <32 weeks (comparison with progesterone (ref. F)) I: 15/42 (35.7%) C: 13/37 (35.1%) RR 0.98, 95% CI 0.54 to 1.79 favouring progesterone
Outcome measure-7 Preterm birth <35 weeks (comparison with progesterone (ref. F)) History of preterm birth not considered I: 16/42 (38.1%)
History of preterm birth No difference (no data reported)
Outcome measure-8 Compositie outcome neonatal morbidity (comparison progesterone (ref. F)) I: 9/42 (21.4%) C: 7/37 (18.9%) RR 1.17, 95% CI 0.39 to 3.53 favouring progesterone
|
Brief description of author’s conclusion Vaginal progesterone was the only intervention with consistent effectiveness for preventing preterm birth in singleton at-risk pregnancies overall and in those with a previous preterm birth.
Personal remarks on study quality, conclusions, and other issues (potentially) relevant to the research question Quality of evidence of individual studies was low to very low.
Level of evidence: Low risk of bias for all studies.
Sensitivity analyses Including only studies with low risk of bias and excluding studies with additional post-randomisation interventions. All the analyses and comparisons were repeated assuming that all the twins in the PROGRESS Study had the outcome.
Heterogeneity: Clinical heterogeneity quantified by I2 and subgroup analyses were performed (based on risk factors, intervention type, route). |
|
Conde-Agudelo, 2018 |
Indirect comparison meta-analysis
Literature search up to March 2018
A: Rust, 2001 B: Berghella, 2004 C: Althuisius, 2001 D: To, 2004 E: Owen 2009
Study design: RCT
Setting and Country: A: Single centre in US B: 2 centres in US C: Single centre in The Netherlands D: 12 centres in UK, Brazil, South Africa, Slovenia, Greece, and Chile E: 15 centers in US
Source of funding and conflicts of interest: Not reported for individual studies.
|
Inclusion criteria SR: Studies that primarily aimed to prevent preterm birth in asymptomatic women with a singleton gestation, previous spontaneous preterm birth, and a sonographic short cervix (cervical length <25 mm) in the midtrimester or to prevent preterm birth in women with other characteristics but for whom outcomes were available in those with a singleton gestation, previous spontaneous preterm birth, and a pre-randomization cervical length <25 mm
Exclusion criteria SR: - Quasi randomized trials - Studies that assessed vaginal progesterone in women with threatened or arrested preterm labor, second trimester bleeding, or premature rupture of membranes - Studies that evaluated vaginal progesterone administration in the first trimester to prevent miscarriage - Studies that assessed history-indicated cerclage (placed for the sole indication of poor obstetric history), physical examination indicated cerclage (placed for second trimester cervical dilatation), or compared different cerclage techniques or outpatient cerclage vs inpatient cerclage - Studies that did not provide data for women with a singleton gestation, previous spontaneous preterm birth, and a cervical length <25 mm in the midtrimester.
Ten studies included, but five studies used for the literature analysis
Important patient characteristics at baseline: Not reported.
Unclear if groups were comparable at baseline
|
Describe intervention:
A: McDonald procedure with a single stitch of permanent monofilament B: McDonald procedure with mersilene tape C: McDonald procedure with braided polyester thread D: Shirodkar suture with mersilene tape E: McDonald procedure with nonabsorbable suture (braided tape)
|
Describe control:
A: no cerclage B: no cerclage C: no cerclage D: no cerclage E: no cerclage |
End-point of follow-up: Not reported.
For how many participants were no complete outcome data available? Not reported.
|
Outcome measure-1 Preterm birth < 28 weeks I: 32/250 (13%) C: 51/254 (20%) Pooled RR 0.64, 95% CI 0.43 to 0.96 favouring cerclage
Outcome measure-2 Preterm birth <32 weeks I: 48/250 (19%) C: 75/254 (30%) Pooled RR 0.66, 95% CI 0.48 to 0.91 favouring cerclage
Outcome measure-3 Preterm birth <37 weeks I: 105/250 (42%) Pooled RR 0.70, 95% CI 0.58 to 0.83 favouring cerclage
Outcome measure-4 Perinatal mortality I: 22/250 (9%) C: 35/254 (14%) Pooled RR 0.65, 95%CI 0.40 to 1.07 favouring cerclage
Outcome measure-5 Composite outcome neonatal mortality/morbidity I: 39/250 (16%) C: 63/254 (25%) Pooled RR 0.64, 95% CI 0.45 to 0.91 favouring cerclage
Outcome measure-6 Respiratory distress syndrome I: 13/207 (6%) C: 21/196 (11%) Pooled RR 0.61, 95%CI 0.32 to 1.19 favouring cerclage
Outcome measure-7 Necrotizing enterocolitis I: 1/207 (1%) C: 2/196 (1%) Pooled RR 0.62, 95%CI 0.08 to 4.67 favouring cerclage
Outcome measure-8 Intraventricular haemorrhage I: 0/207 (0%) C: 4/196 (2%) Pooled RR 0.28, 95%CI 0.05 to 1.64 favouring cerclage
Outcome measure-9 Neonatal sepsis I: 8/207 (4%) C: 17/196 (9%) Pooled RR 0.47, 95%CI 0.21 to 1.05 favouring cerclage
|
Brief description of author’s conclusion Vaginal progesterone and cerclage are equally effective for preventing preterm birth and improving perinatal outcomes in women with a singleton gestation, previous spontaneous preterm birth, and a midtrimester sonographic short cervix. The choice of treatment will depend on adverse events and cost-effectiveness of interventions and patient/physician’s preferences.
Personal remarks on study quality, conclusions, and other issues (potentially) relevant to the research question No raw data presented.
Level of evidence: Low risk of bias for all studies.
Sensitivity analyses Impact of cointerventions on the direction and size of effect for preterm birth and perinatal mortality. In this sensitivity analysis, women who received 17a-hydroxyprogesterone caproate (17-OHPC) or vaginal progesterone in trials that compared cerclage vs no cerclage and women who received a cerclage in studies that compared vaginal progesterone to placebo were excluded.
Heterogeneity: Heterogeneity tested with I2 and subgroup analysis for women with a cervical length <16 mm. |
|
Berghella, 2017 |
Systematic review and meta-analysis
Literature search up to February 2017
A: Rust, 2001 B: Althuisius, 2001 C: To, 2004 D: Berghella, 2004 E: Otsuki, 2016
Study design: RCT
Setting and Country: A: USA B: Netherlands C: Multicenter: UK, Brazil, South Africa, Slovenia, Greece, and Chile D: USA E: Japan
Source of funding and conflicts of interest: Not reported. |
Inclusion criteria SR: RCTs of asymptomatic singleton pregnancies without prior spontaneous preterm birth found to have a mid-trimester cervical length <25mm on transvaginal sonography and then randomized to management with either cerclage or no cerclage.
Exclusion criteria SR: - Quasi randomized trials - Studies on multiple pregnancies and studies on symptomatic women - Trials evaluating history-indicated (prior spontaneous preterm birth) or physical examination-indicated (second-trimester cervical dilatation detected on physical examination) cerclage - Trials on ultrasound-indicated (short transvaginal sonography cervical length) cerclage with prior spontaneous preterm birth - Studies on technical aspects of cervical cerclage
Five studies included
Important patient characteristics at baseline: Gestational age A: 16-24 weeks B: 14-27 weeks C: 22-24 weeks D: 14-24 weeks E: 16-26 weeks
Groups were probably comparable at baseline
|
Describe intervention:
A: McDonald cerclage with permanent monofilament B: McDonald cerclage with Braided tape C: Shirodkar cerclage with Braided tape D: McDonald cerclage with Braided tape E: McDonald cerclage or Shirodkar cerclage with Braided tape
|
Describe control:
A: no cerclage B: no cerclage C: no cerclage D: no cerclage E: no cerclage |
End-point of follow-up: 36+0 to 37+6 weeks of gestation (unless spontaneous onset of labour, rupture of membranes or need for early delivery occurred)
For how many participants were no complete outcome data available? C: 0.4% lost to follow-up |
Outcome measure-1 Preterm birth <28 weeks I: 26/224 (11.6%) C: 22/195 (11.3%) Pooled RR 1.55, 95%CI 0.68 to 1.93 favouring no cerclage
Outcome measure-2 Preterm birth <34 weeks I: 45/224 (20.1%) C: 49/195 (25.1%) Pooled RR 0.89, 95%CI 0.63 to 1.27 favouring cerclage
Outcome measure-3 Preterm birth <37 weeks I: 81/224 (36.2%) C: 80/195 (41.0%) Pooled RR 0.93, 95%CI 0.73 to 1.18 favouring cerclage
Outcome measure-4 Neonatal death I: 7/118 (5.9%) C: 6/92 (6.5%) Pooled RR 1.08, 95%CI 0.41 to 2.86 favouring cerclage
Outcome measure-5 Respiratory distress syndrome I: 2/14 (14.3%) C: 2/16 (12.5%) Pooled RR 1.33, 95%CI 0.23 to 7.74 favouring no cerclage
Outcome measure-6 Necrotizing enterocolitis I: 0/14 (0%) C: 0/16 (0%)
Outcome measure-7 Intraventricular haemorrhage I: 1/14 (7.1%) C: 0/16 (0%) RR 3.90, 95%CI 0.18 to 85.93 favouring no cerclage
Outcome measure-8 Neonatal sepsis I: 2/14 (14.3%) C: 2/16 (12.5%) RR 1.33, 95%CI 0.23 to 7.74 favouring no cerclage
|
Brief description of author’s conclusion In singleton gestations without prior spontaneous preterm birth but with transvaginal sonography cervical length <25 mm in the second trimester, cerclage does not seem to prevent preterm delivery or improve neonatal outcome. However, in these pregnancies, cerclage seems to be efficacious at lower cervical lengths, such as <10 mm, and when tocolytics or antibiotics are used as additional therapy, requiring further studies in these subgroups.
Personal remarks on study quality, conclusions, and other issues (potentially) relevant to the research question - Low quality of evidence - No use of progesterone
Level of evidence: Low risk of bias for all studies.
Sensitivity analyses No sensitivity analyses.
Heterogeneity: Between-study heterogeneity was explored using I2 statistic. Statistical heterogeneity between studies was low with no inconsistency in the primary and most of the secondary outcomes. Subgroup analysis of women who had transvaginal sonography cervical length <10 mm or received tocolytics or antibiotics as additional therapy to cerclage. |
Research question (UV5b): What are the (un)favourable effects of pessary compared to no pessary, cerclage or progesterone in the prevention of spontaneous preterm birth in woman with singleton pregnancies and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks?
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C)
|
Follow-up |
Outcome measures and effect size |
Comments |
|
Conde-Agudelo, 2020
|
SR and meta-analysis of RCTs
Literature search up to October 2019
A: Goya, 2012 B: Hui, 2013 C: Nicolaides, 2016 D: Saccone, 2017 E: Dugoff, 2018 F: Cruz-Melguizo, 2018
Study design: RCT
Setting and Country: A: Spain B: China C: Multicountry D: Italy E: US F: Spain
Source of funding and conflicts of interest: Not reported for individual studies. |
Inclusion criteria SR: - randomized controlled trials comparing cervical pessary to standard care (no pessary) or alternative interventions (such as vaginal progesterone or cervical cerclage) in asymptomatic women at high risk for preterm birth (such as those with a midtrimester sonographic short cervix, history of preterm birth, multiple gestation, and uterine anomalies or excisional cervical procedures) with the aim of preventing preterm birth and/or adverse perinatal outcomes. - trials with planned cointerventions if the co-interventions were permitted equally in each trial arm.
Exclusion criteria SR: - quasirandomized trials - assessed cervical pessary in women with arrested preterm labour or placenta previa - did not report clinical outcomes - studies published only as abstracts if additional information on methodological issues and results could not be obtained.
Twelve studies included, but six studies used for the literature analysis
Important patient characteristics at baseline: Gestational age A: 20-23 weeks B: 20-24 weeks C: 20-24 weeks D: 18-23 weeks E: 18-23 weeks F: 19-22 weeks
Cervical length (mm) A: 19.0 ± 4.8 B: 20.1 ± 0.5 C: 20.0 (14.0 – 22.0) D: 12.0 ± 5.8 E: 17.6 (10.9 – 22.0) vs 19.0 (11.2 – 22.9) F: 20.9 ± 4.2
Concomitant use of vaginal progesterone A: 0% B: 0% C: 44% vs 47% D: 89% vs 83% E: 84% vs 91% F: 5% vs 100%
Groups probably comparable at baseline
|
Describe intervention:
A: Arabin pessary B: Arabin pessary C: Arabin pessary D: Arabin pessary E: Bioteque cup pessary F: Arabin pessary
|
Describe control:
A: no pessary B: no pessary C: no pessary D: no pessary E: no pessary F: vaginal progesterone
|
End-point of follow-up: Not reported.
For how many participants were no complete outcome data available? No bias due to missing outcome data.
|
Outcome measure-1 Preterm birth <28 weeks I: 44/865 (5.1%) C: 52/865 (6.0%) Pooled RR 0.76, 95% CI 0.37 to 1.54 favouring pessary
Subgroup for progesterone (ref. F) I: 10/125 (8.0%) C: 9/118 (7.6%) RR 1.05, 95% CI 0.44 to 2.49 favouring progesterone
Outcome measure-2 Preterm birth <34 weeks I: 102/918 (11%) C: 142/920 (15%) Pooled RR 0.72, 95% CI 0.36 to 1.45 favouring pessary
Subgroup no previous preterm birth I: 78/605 (12.9%) C: 72/591 (12.2%) Pooled RR 0.97, 95%CI 0.54 to 1.76 favouring no pessary
Subgroup ³ 1 previous preterm birth I: 7/70 (10%) C: 16/84 (19%) Pooled RR 0.53, 95%CI 0.23 to 1.20 favouring pessary
Subgroup for progesterone (ref. F) I: 18/127 (14.2%) C: 17/119 (14.3%) RR 0.99, 95% CI 0.54 to 1.83 favouring pessary
Outcome measure-3 Preterm birth <37 weeks I: 196/865 (22.7%) C: 282/865 (32.6%) Pooled RR 0.71, 95% CI 0.41 to 1.24 favouring pessary
Subgroup for progesterone (ref. F) I: 27/125 (22%) C: 25/118 (21%) RR 1.02, 95% CI 0.63 to 1.65 favouring progesterone
Outcome measure-4 Perinatal death I: 12/918 (1.3%) C: 15/920 (1.6%) Pooled RR 0.81, 95% CI 0.38 to 1.74 favouring pessary
Subgroup for progesterone (ref. F) I: 6/125 (4.8%) C: 3/118 (2.5%) RR 1.89, 95% CI 0.48 to 7.38 favouring progesterone
Outcome measure-5 Composite outcome neonatal mortality/morbidity I: 69/865 (8.0%) C: 114/865 (13.2%) Pooled RR 0.59, 95%CI 0.28 to 1.27 favouring pessary
Subgroup for progesterone (ref. F) I: 24/125 (19%) C: 20/118 (17%) RR 1.13, 95% CI 0.66 to 1.94 favouring progesterone
Outcome measure-6 Respiratory distress syndrome I: 62/918 (6.8%) C: 90/920 (9.8%) Pooled RR 0.72, 95% CI 0.36 to 1.43 favouring pessary
Outcome measure-7 Necrotizing enterocolitis I: 11/865 (1.3%) C: 10/856 (1.2%) Pooled RR 1.15, 95% CI 0.47 to 2.79 favouring no pessary
Outcome measure-8 Intraventricular haemorrhage I: 17/918 (1.9%) C: 14/920 (1.5%) Pooled RR 1.16, 95% CI 0.48 to 2.80 favouring no pessary
Outcome measure-9 Neonatal sepsis I: 49/918 (5.3%) C: 56/920 (6.1%) Pooled RR 0.80, 95% CI 0.46 to 1.40 favouring pessary |
Brief description of author’s conclusion Current evidence does not support the use of cervical pessary to prevent preterm birth or to improve perinatal outcomes in singleton or twin gestations with a short cervix and in unselected twin gestations. Among patients with a singleton gestation and a short cervix who receive vaginal progesterone, a cervical pessary should not be placed given that the device does not offer any additional benefits over administration of vaginal progesterone alone in reducing preterm birth and adverse perinatal outcomes.
Personal remarks on study quality, conclusions, and other issues (potentially) relevant to the research question - Substantial statistical heterogeneity - Limitations in power for subgroup analyses - Only a few studies about vaginal progesterone
Level of evidence: Low risk of bias for included studies.
Sensitivity analyses Prespecified sensitivity analyses to explore the impact of risk of bias on results were not performed.
Heterogeneity Heterogeneity of treatment effect was assessed with the I2 statistic. Substantial heterogeneity was present. |
Table of quality assessment for systematic reviews of RCTs and observational studies
Based on AMSTAR checklist (Shea et al.; 2007, BMC Methodol 7: 10; doi:10.1186/1471-2288-7-10) and PRISMA checklist (Moher et al 2009, PLoS Med 6: e1000097; doi:10.1371/journal.pmed1000097)
Research question (UV5a): What are the (un)favourable effects of cerclage compared to no cerclage, pessary or progesterone in the prevention of spontaneous preterm birth in woman with singleton pregnancies and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks?
|
Study
First author, year |
Appropriate and clearly focused question?1
Yes/no/unclear |
Comprehensive and systematic literature search?2
Yes/no/unclear |
Description of included and excluded studies?3
Yes/no/unclear |
Description of relevant characteristics of included studies?4
Yes/no/unclear |
Appropriate adjustment for potential confounders in observational studies?5
Yes/no/unclear/notapplicable |
Assessment of scientific quality of included studies?6
Yes/no/unclear |
Enough similarities between studies to make combining them reasonable?7
Yes/no/unclear |
Potential risk of publication bias taken into account?8
Yes/no/unclear |
Potential conflicts of interest reported?9
Yes/no/unclear |
|
Jarde, 2019 |
Yes. Research question and inclusion criteria were mentioned. |
Yes. Search period and search strategy were described. Medline and EMBASE were searched. |
No. Reasons for exclusion were provided but without references. |
Yes. Main characteristics were provided. |
Not applicable (only RCTs). |
Yes. Individual study quality was assessed with Cochrane Risk of Bias tool. |
Yes. Statistical heterogeneity was assessed. |
Yes. Mentioned that publication bias could only assessed if at least 10 studies were available. |
No. Conflict of interest of the systematic review is reported but not for individual studies. |
|
Conde-Agudelo, 2018 |
Yes. Research question and inclusion criteria were mentioned.
|
No. Search period was mentioned, but clear search strategy is missing. |
Yes. Reasons for exclusion were provided with references. |
Yes. Main characteristics were provided. |
Not applicable (only RCTs). |
Yes. Risk of bias assessed with Cochrane Risk of Bias tool and described in the text.
|
Yes. Statistical heterogeneity was assessed (no substantial heterogeneity present). |
Yes. Mentioned that publication bias could not be assessed because of the limited number of trials included in the review.
|
No. Conflict of interest of the systematic review is reported but not for individual studies. |
|
Berghella, 2017 |
Yes. Research question and inclusion criteria were mentioned. |
Yes. Search period and search terms were described. Medline was searched. |
No. Only reasons for exclusion were provided. |
Yes. Main characteristics were provided. |
Not applicable (only RCTs). |
Yes. Risk of bias of individual studies assessed with Cochrane Risk of Bias tool. |
Yes. Statistical heterogeneity was assessed (very low) |
No. Publication bias was assessed using Begg’s and Egger’s tests, but authors only showed p-values and less than ten studies were included. |
No. Conflict of interest not reported. |
- Research question (PICO) and inclusion criteria should be appropriate and predefined
- Search period and strategy should be described; at least Medline searched; for pharmacological questions at least Medline + EMBASE searched
- Potentially relevant studies that are excluded at final selection (after reading the full text) should be referenced with reasons
- Characteristics of individual studies relevant to research question (PICO), including potential confounders, should be reported
- Results should be adequately controlled for potential confounders by multivariate analysis (not applicable for RCTs)
- Quality of individual studies should be assessed using a quality scoring tool or checklist (Jadad score, Newcastle-Ottawa scale, risk of bias table etc.)
- Clinical and statistical heterogeneity should be assessed; clinical: enough similarities in patient characteristics, intervention and definition of outcome measure to allow pooling? For pooled data: assessment of statistical heterogeneity using appropriate statistical tests (e.g. Chi-square, I2)?
- An assessment of publication bias should include a combination of graphical aids (e.g., funnel plot, other available tests) and/or statistical tests (e.g., Egger regression test, Hedges-Olken). Note: If no test values or funnel plot included, score “no”. Score “yes” if mentions that publication bias could not be assessed because there were fewer than 10 included studies.
- Sources of support (including commercial co-authorship) should be reported in both the systematic review and the included studies. Note: To get a “yes,” source of funding or support must be indicated for the systematic review AND for each of the included studies.
Table of quality assessment for systematic reviews of RCTs and observational studies
Based on AMSTAR checklist (Shea et al.; 2007, BMC Methodol 7: 10; doi:10.1186/1471-2288-7-10) and PRISMA checklist (Moher et al 2009, PLoS Med 6: e1000097; doi:10.1371/journal.pmed1000097)
Research question (UV5b): What are the (un)favourable effects of pessary compared to no pessary, cerclage or progesterone in the prevention of spontaneous preterm birth in woman with singleton pregnancies and a cervical length ≤25 mm with or without a history of spontaneous preterm birth <37 weeks?
|
Study
First author, year |
Appropriate and clearly focused question?1
Yes/no/unclear |
Comprehensive and systematic literature search?2
Yes/no/unclear |
Description of included and excluded studies?3
Yes/no/unclear |
Description of relevant characteristics of included studies?4
Yes/no/unclear |
Appropriate adjustment for potential confounders in observational studies?5
Yes/no/unclear/notapplicable |
Assessment of scientific quality of included studies?6
Yes/no/unclear |
Enough similarities between studies to make combining them reasonable?7
Yes/no/unclear |
Potential risk of publication bias taken into account?8
Yes/no/unclear |
Potential conflicts of interest reported?9
Yes/no/unclear |
|
Conde-Agudelo 2020 |
Yes. Research question and inclusion criteria were mentioned. |
No. Search period was described and Medline and EMBASE were searched, but search strategy unclear (only stated that combination of keywords and text words related to cervical pessary and preterm birth were used).
|
No. Reasons for exclusion were provided but without references. |
Yes. Main characteristics were provided. |
Not applicable (only RCTs). |
Yes. Risk of bias was assessed for individual studies based on the Cochrane risk of bias tool. |
No. Statistical heterogeneity was assessed, and substantial heterogeneity was present. |
Yes. Mentioned that publication bias could not be assessed given the limited number of trials in the review. |
No. Conflict of interest of the systematic review is reported but not for individual studies. |
- Research question (PICO) and inclusion criteria should be appropriate and predefined
- Search period and strategy should be described; at least Medline searched; for pharmacological questions at least Medline + EMBASE searched
- Potentially relevant studies that are excluded at final selection (after reading the full text) should be referenced with reasons
- Characteristics of individual studies relevant to research question (PICO), including potential confounders, should be reported
- Results should be adequately controlled for potential confounders by multivariate analysis (not applicable for RCTs)
- Quality of individual studies should be assessed using a quality scoring tool or checklist (Jadad score, Newcastle-Ottawa scale, risk of bias table etc.)
- Clinical and statistical heterogeneity should be assessed; clinical: enough similarities in patient characteristics, intervention and definition of outcome measure to allow pooling? For pooled data: assessment of statistical heterogeneity using appropriate statistical tests (e.g. Chi-square, I2)?
- An assessment of publication bias should include a combination of graphical aids (e.g., funnel plot, other available tests) and/or statistical tests (e.g., Egger regression test, Hedges-Olken). Note: If no test values or funnel plot included, score “no”. Score “yes” if mentions that publication bias could not be assessed because there were fewer than 10 included studies.
- Sources of support (including commercial co-authorship) should be reported in both the systematic review and the included studies. Note: To get a “yes,” source of funding or support must be indicated for the systematic review AND for each of the included studies.
Table of excluded studies
|
Auteur en jaartal |
Redenen van exclusie |
|
Brown, 2019 |
Guideline |
|
Jin, 2019 |
Wrong study design; case-control studies of cervical pessary |
|
Matei, 2019 |
Review published before Conde-Agudelo 2020 |
|
Medley, 2018 |
Review of reviews |
|
Pérez-López, 2019 |
Review published before Conde-Agudelo 2020 |
|
Zheng, 2019 |
Review published before Conde-Agudelo 2020 |
|
Cruz-Melguizo, 2018 |
RCT included in Conde-Agudelo 2020 |
|
Dugoff, 2018 |
RCT included in Conde-Agudelo 2020 |
|
Marat, 2019 |
Wrong study design |
|
Pratcorona, 2018 |
Does not fulfill PICO criteria; wrong study population |
|
Saccone, 2018 |
RCT included in Jarde 2019 |
|
Daskalakis, 2019 |
Commentary |
|
Hermans, 2018 |
Does not fulfill PICO criteria; wrong study population |
|
Correa, 2019 |
5 RCTs included in Conde-Agudelo 2020 |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 10-02-2025
Beoordeeld op geldigheid : 20-11-2024
Algemene gegevens
De ontwikkeling van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2019 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor zwangere vrouwen zonder klinische verschijnselen van een vroeggeboorte, die al dan niet in een eerdere zwangerschap een spontane vroeggeboorte hebben doorgemaakt.
Werkgroep
- Prof. dr. M.A. Oudijk, gynaecoloog, NVOG (voorzitter)
- Dr. N. Horree, gynaecoloog, NVOG
- Dr. J.B. Derks, gynaecoloog, NVOG
- Dr. T.A.J. Nijman, gynaecoloog, NVOG
- Dr. F. Vlemmix, gynaecoloog, NVOG
- Dr. D.A.A. van der Woude, gynaecoloog, NVOG
- L.T. Brammerloo-Read, MSc, verloskundige, KNOV
- Dr. M.A.C. Hemels, kinderarts-neonatoloog, NVK
- F.A.B.A. Schuerman, MSc, kinderarts-neonatoloog, NVK
- J.D.M. Wagemaker, patiëntenvereniging, Care4Neo
Met ondersteuning van:
- Dr. L. Viester, adviseur, Kennisinstituut van Medisch Specialisten (tot augustus 2022)
- T. Geltink, MSc, adviseur, Kennisinstituut van Medisch Specialisten (vanaf augustus 2022)
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Prof. dr. M.A. Oudijk |
Gynaecoloog |
Voorzitter Pijler FMG van de NVOG, onbetaald, alleen vacatiegelden. Voorzitter wetenschapscommissie pijler FMG, onbetaald. Member of the board of the foundation 'Stoptevroegbevallen'; a non-profit foundation with the purpose to raise funds for research projects on preterm labour/birth, onbetaald. Member of the scientific committee of the 'Fonds Gezond Geboren', a non-profit foundation with the purpose to raise funds for reserarch projects on preterm birth and placental insufficiency, onbetaald. Member of the advisory board of the N3, the Dutch Neonatology research network, onbetaald. President of the European Spontaneous Preterm Birth Congress to be held in Haarlem, The Netherlands, www. espbc.eu, onbetaald |
2015 ZonMW836041012 The effect of tocolysis with nifedipine or atosiban on infant development: the APOSTEL III follow-up study. € 43,772. 2015 ZonMW 836041006 Low dose aspirin in the prevention of recurrent spontaneous preterm labour: the APRIL study € 351.898. 2016 Zon|MW 80-84800-98-41027 Atosiban versus placebo in the treatment of late threatened preterm labour: the APOSTEL VIII study € 1.393.639. Hoofdaanvrager/projectleider van deze vroeggeboorte studies. Subsidie wordt alleen aangewend ten behoeve van het onderzoek, promoventi etc. Geen persoonlijke salariëring vanuit deze ZonMw studie |
geen restricties |
|
Dr. N. Horree |
Gynaecoloog |
geen |
Participatie binnen ziekenhuis aan consortium studies vanuit de NVOG. Hieronder vallen ook onderzoek naar vroeggeboorte (o.a. Apnel studies) en preventie vroeggeboorte (April). QP PC - studies |
geen restricties |
|
Dr. J.B. Derks |
Gynaecoloog |
Lid bestuur werkgroep perinatologie en maternale ziektes (onbetaald); Lid otterlo groep (Cie. Ontwikkeling richtlijnen obstetrie) (onbetaald) |
Deelname consortiumstudies waaronder de April studie |
geen restricties |
|
T.A.J. Nijman |
Gynaecoloog |
Lid Commissie Gynaecongres, VAGO-vertegenwoordiger, onbetaald; Lid Koepel Wetenschap. VAGO-vertegenwoordiger, onbetaald |
Project groep April studie, ZonMW gesponsorde Consortium studie naar aspirine vs placebo bij preventie herhaalde vroeggeboorte. |
geen restricties |
|
Dr. F. Vlemmix |
Gynaecoloog |
Lid werkgroep patiëntcommunicatie NVOG |
geen |
geen restricties |
|
Dr. D.A.A. van der Woude |
Gynaecoloog & postdoc |
geen |
geen |
geen restricties |
|
L.T. Brammerloo-Read |
Verloskundige |
geen |
De praktijk + kliniek waarin werkzaam heeft deelname in cervix-meting van patiënten om vroeggeboorte op te kunnen sporen, hierbij geen financieel belang. |
geen restricties |
|
Dr. M.A.C. Hemels |
Kinderarts-neonatoloog |
Faculty cursus antibiotica bij kinderen, betaald |
Deelname APRIL studie, meelezen protocol betreffende de neonatale uitkomst maten |
geen restricties |
|
F.A.B.A. Schuerman |
Kinderarts-neonatoloog |
Bestuurslid stichting kindersedatie Nederland (betaald) |
geen |
geen restricties |
|
J.D.M. Wagemaker |
Patiëntvertegenwoordiger care |
geen |
geen |
geen restricties |
Inbreng patiëntenperspectief
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door uitnodigen van Patiëntenfederatie Nederland, Stichting Kind en Ziekenhuis en Vereniging Ouders Couveusekinderen voor de schriftelijke knelpunteninventarisatie en een afgevaardigde patiëntenvereniging in de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voor commentaar voorgelegd aan Patiëntenfederatie Nederland, Stichting Kind en Ziekenhuis en Vereniging Ouders Couveusekinderen en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijn is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling zijn richtlijnmodules op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Uit de kwalitatieve raming blijkt dat er waarschijnlijk geen substantiële financiële gevolgen zijn.
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor zwangere vrouwen zonder klinische verschijnselen van een vroeggeboorte, die al dan niet in een eerdere zwangerschap een spontane vroeggeboorte hebben doorgemaakt. Tevens zijn er knelpunten aangedragen door Patiëntenfederatie Nederland, Verpleegkundigen & Verzorgenden Nederland, Nederlandse Vereniging voor Kindergeneeskunde, Nederlandse Vereniging voor Medische Microbiologie, LAREB, Nederlandse Vereniging voor Klinische Fysica, Kind en Ziekenhuis via een schriftelijke knelpunteninventarisatie .
Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. Review Manager 5.4 werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
Zoekverantwoording
|
Database |
Zoektermen |
Totaal |
|
Medline (OVID)
|
1 exp Pessaries/ or 'pessaries'.ti,ab,kw. or 'pessarium'.ti,ab,kw. or 'pessary'.ti,ab,kw. (2287) 2 exp Cervix Incompetence/ (1428) 3 limit 2 to yr="1973 - 2001" (815) 4 exp Cerclage, Cervical/ or 'cerclage'.ti,ab,kw. or (cervi* adj3 (stitch* or suture)).ti,ab,kw. or ((shirodkar or mcdonald or macdonald) adj3 (stitch* or procedure* or method* or technique* or operation*)).ti,ab,kw. (3299) 5 3 or 4 (3724) 6 1 or 5 (5895) 7 exp Obstetric Labor, Premature/ or ((labo*r or delivery or parturition or birth) adj3 (premature or preterm or 'pre term' or early or prior)).ti,ab,kw. (57757) 8 6 and 7 (1413) 9 limit 8 to english language (1143) 10 (meta-analysis/ or meta-analysis as topic/ or (meta adj analy$).tw. or ((systematic* or literature) adj2 review$1).tw. or (systematic adj overview$1).tw. or exp "Review Literature as Topic"/ or cochrane.ab. or cochrane.jw. or embase.ab. or medline.ab. or (psychlit or psyclit).ab. or (cinahl or cinhal).ab. or cancerlit.ab. or ((selection criteria or data extraction).ab. and "review"/)) not (Comment/ or Editorial/ or Letter/ or (animals/ not humans/)) (415567) 11 (exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw.) not (animals/ not humans/) (1906456) 12 9 and 10 (110) 13 (9 and 11) not 12 (224) 14 12 or 13 (334) = 334 (96 uniek) |
535 |
|
Embase
|
('vagina pessary'/exp OR 'pessaries':ti,ab OR 'pessarium':ti,ab OR 'pessary':ti,ab OR 'uterine cervix cerclage'/exp OR 'cerclage'/exp OR 'cerclage':ti,ab OR ((cervi* NEAR/3 (stitch* OR suture)):ti,ab) OR (((shirodkar OR mcdonald OR macdonald) NEAR/3 (stitch* OR procedure* OR method* OR technique* OR operation*)):ti,ab) OR) AND 'premature labor'/exp OR (((labo*r OR delivery OR parturition OR birth) NEAR/3 (premature OR preterm OR 'pre term' OR early OR prior)):ti,ab) AND [english]/lim NOT 'conference abstract':it
Sytematische reviews ('meta analysis'/de OR cochrane:ab OR embase:ab OR psycinfo:ab OR cinahl:ab OR medline:ab OR ((systematic NEAR/1 (review OR overview)):ab,ti) OR ((meta NEAR/1 analy*):ab,ti) OR metaanalys*:ab,ti OR 'data extraction':ab OR cochrane:jt OR 'systematic review'/de) NOT (('animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp)
RCT’s ('clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti) NOT 'conference abstract':it
= 454 (439 uniek) |