Longfysiotherapie
Uitgangsvraag
Wat is de toegevoegde waarde van perioperatieve (long)fysiotherapie om de kans op postoperatieve pulmonale complicaties bij pulmonaal belaste patiënten te verkleinen?
Aanbeveling
Overweeg 2-3 weken voorafgaand aan een grote abdominale ingreep ademverdiepingsoefeningen te geven aan alle pulmonaal belaste patiënten. De werkgroep adviseert om zoveel mogelijk aan te sluiten bij bestaande prehabilitatieprogramma’s.
Overweeg hoogrisicopatiënten naar de (long)fysiotherapeut te verwijzen om de preoperatieve pulmonale conditie te optimaliseren met behulp van ademspiertraining en/of sputum-evacuerende technieken.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Er is een literatuuronderzoek verricht naar de impact van (een combinatie van) pre- en postoperatieve (long)fysiotherapie bij pulmonaal belaste patiënten die een niet-pulmonale operatie ondergaan. Er is 1 systematische review en er zijn 7 additionele studies geïncludeerd over de effecten van pre- en postoperatieve fysiotherapie op het ontstaan van PPC’s. Uit de systematische review zijn 20 gerandomiseerde studies opgenomen in de literatuursamenvatting. De interventies uit de geïncludeerde studies waren in te delen in de volgende categorieën: ademspiertraining, ademverdiepingsoefeningen, lichamelijke oefeningen (mobiliseren) of een combinatie hiervan.
De cruciale uitkomstmaat was het optreden van PPC’s. Het niveau van bewijs voor alle uitkomsten was gebaseerd op gerandomiseerde gecontroleerde onderzoeken en begon daarom op hoog. Echter, onder andere omdat de studies ook patiënten zonder pulmonale voorgeschiedenis includeerden, werd het niveau van bewijs afgeschaald naar laag tot zeer laag.
Voor preoperatieve fysiotherapie was de bewijskracht zeer laag, waardoor geen richting kan worden gegeven aan de besluitvorming. Er is afgewaardeerd voor indirectheid vanwege een bredere patiëntengroep, vanwege risico op bias en voor imprecisie vanwege de betrouwbaarheidsintervallen die de grenzen van klinische relevantie overschrijden. Door de lage bewijskracht van de uitkomstmaat PPC’s, zowel voor pre-operatieve fysiotherapie als postoperatieve fysiotherapie kan de literatuur voor die interventies beperkt richting geven aan de besluitvorming.
Bij patiënten die postoperatieve fysiotherapie kregen, en de patiënten die een combinatie van pre- en postoperatieve fysiotherapie kregen, kwamen minder postoperatieve pulmonale complicaties voor, vergeleken met patiënten die reguliere zorg kregen (lage bewijskracht). Er is afgewaardeerd voor indirectheid vanwege een bredere patiëntengroep, vanwege risico op bias en voor imprecisie vanwege de betrouwbaarheidsintervallen die de grenzen van klinische relevantie overschrijden.
Andere belangrijke uitkomstmaten waren kwaliteit van leven en verblijfsduur in het ziekenhuis. Kwaliteit van leven werd door één studie gerapporteerd die pre-/postoperatieve fysiotherapie onderzocht. Er werd geen klinisch relevant verschil gevonden in kwaliteit van leven. De bewijskracht van deze uitkomstmaat was zeer laag. Er is hierbij afgewaardeerd voor indirectheid vanwege een bredere patiëntengroep en imprecisie vanwege de hele kleine studiepopulatie.
Er werd geen verschil gevonden in verblijfsduur in het ziekenhuis in de studie die preoperatieve fysiotherapie vergeleek met reguliere zorg (i.e. zonder fysiotherapie). Er werd wel een klinisch relevant verschil gevonden in de verblijfsduur in het ziekenhuis in het voordeel van de groep patiënten die perioperatieve fysiotherapie kreeg en in het voordeel van de groep patiënten die postoperatieve fysiotherapie kreeg. De bewijskracht van deze uitkomstmaat was laag tot zeer laag. Er is hierbij afgewaardeerd voor indirectheid vanwege een bredere patiëntengroep en voor imprecisie vanwege het brede betrouwbaarheidsinterval en de kleine studiepopulatie. Door de lage tot zeer lage bewijskracht van de belangrijke uitkomstmaten kan de literatuur beperkt richting geven aan de besluitvorming. Er bestaat dus een kennisvraag omtrent het effect van pre-/postoperatieve fysiotherapie op pulmonaal belaste patiënten die een niet-pulmonale ingreep ondergaan.
In veel ziekenhuizen worden diverse patiëntengroepen voorbereid op een operatieve ingreep. Deze prehabilitatie omvat het multimodaal optimaliseren van patiëntgebonden modificeerbare risicofactoren voorafgaand aan een operatie of behandeling om de individuele weerbaarheid van de patiënt te verhogen. Pre-/postoperatieve fysiotherapie is hier onderdeel van. Het klinisch relevante voordeel (dus minder postoperatieve pulmonale complicaties) werd gevonden bij abdominale én thoracale ingrepen. De bewijskracht was echter laag, na afwaardering voor indirectheid vanwege een bredere patiëntengroep en voor imprecisie vanwege het brede betrouwbaarheidsinterval.
Omdat het relatief makkelijk is om in de klinische praktijk bij pulmonaal belaste patiënten preoperatief adem(verdiepings)oefeningen te starten en dit postoperatief te continueren, raadt de werkgroep aan om de prehabilitatieprogramma’s uit te breiden met deze oefeningen die de patiënt zelf preoperatief thuis kan doen (eventueel met een incentive spirometer). Bij het ontbreken van een prehabilitatieprogramma kan overwogen worden om gebruik van (pre- en/of postoperatieve ademverdiepingsoefeningen alléén toe te passen, aangezien deze eenvoudig kunnen worden toegepast. Voor het onderscheid tussen adem(verdiepings)oefeningen en ademspiertraining, zie ook de module Ademoefeningen en ademspiertraining binnen de MSR/GRZ - COVID 19.
Ademspiertraining en het aanleren van sputum-evacuerende technieken zijn een specialistische voorbereiding waarvoor een (long)fysiotherapeut nodig is. Deze vorm van training lijkt daarom met name geschikt voor (pulmonale) hoogrisicopatiënten. Hoge leeftijd, pulmonale voorgeschiedenis, hoge frailty-score, comorbiditeit (diabetes, roken) én een ingreep in de bovenbuik of thorax zijn dan risicofactoren die in overweging genomen moeten worden.
De gebruikte studies laten geen van allen zien dat preoperatieve (long)fysiotherapie een verbetering van de kwaliteit van leven geeft in pulmonaal belaste patiënten, omdat hier niet expliciet naar is gekeken. Omdat er een mogelijke verlaging van het risico op pulmonale complicaties is aangetoond en een mogelijke verkorting van de opnameduur in het gehele cohort, lijkt het aannemelijk te veronderstellen dat er ook een gunstig effect zal bestaan met betrekking tot de kwaliteit van leven. Om dit vast te stellen zal aanvullend onderzoek noodzakelijk zijn.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Het is belangrijk om patiënten in de preoperatieve fase te informeren over de risico’s van de ingreep en deze met hen te bespreken, zodat zij zelf een afweging kunnen maken of de risico’s opwegen tegen de voordelen van de ingreep. Daarbij is een goede uitleg over het ontstaan van postoperatieve pulmonale complicaties door onvoldoende analgesie, immobiliteit en onvoldoende doorzuchten een onderdeel. Hoewel de bewijskracht van de literatuur laag is, doordat de studies weinig onderscheid maken tussen patiënten in het algemeen en pulmonaal belaste patiënten, lijkt het toepassen van ademverdiepingsoefeningen en ademspiertraining wel een risicoverlagend effect te hebben wat patiënten makkelijk zelf kunnen beïnvloeden door dagelijks deze eenvoudige oefening (thuis) uit te voeren. Patiënten moeten ook geïnformeerd worden over de mogelijke effecten van ademverdiepingsoefeningen en ademspiertraining.
Kosten (middelenbeslag)
Op basis van de geïncludeerde studies wordt geconcludeerd dat (long)fysiotherapie mogelijk leidt tot een verkorting van de opnameduur in patiënten in het algemeen, zonder onderscheid te maken tussen wel en niet-pulmonaal belaste patiënten. De invoering van (long)fysiotherapie door middel van ademverdiepingsoefeningen en ademspiertraining bij patiënten die een operatieve ingreep moeten ondergaan, lijkt een kosteneffectieve manier om de verblijfsduur te verkorten. Bovendien kan de patiënt na goede instructies van een (long)fysiotherapeut de oefeningen zelf (thuis) uitvoeren en is verdere begeleiding door een professionele zorgverlener niet beslist noodzakelijk, maar kan eventueel ook via beeldbellen plaats vinden. Voor het gebruik van een incentive spirometer en ademspiertrainer worden de benodigde materialen vooralsnog niet vergoed in het basispakket.
Aanvaardbaarheid, haalbaarheid en implementatie
De werkgroep heeft geen informatie over de implementatie van ademverdiepingsoefeningen en ademspiertraining in pulmonaal belaste patiënten. Ademverdiepingsoefeningen zijn relatief eenvoudig te implementeren. De training is gemakkelijk door de patiënt zelf (thuis) uit te voeren na een korte instructievideo bekeken te hebben. De implementatie kan worden vergemakkelijkt door de interventie bij alle operatiepatiënten, zonder uitzondering toe te passen.
Ademspiertraining moet onder begeleiding van een (long)fysiotherapeut worden opgestart. Het is niet duidelijk of hiervoor een meerwaarde is omdat deze vorm van training in de gebruikte literatuur onvoldoende is gespecificeerd. Deze vorm van training behoeft begeleiding door een (gespecialiseerd) fysiotherapeut.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
De studies die zijn gevonden maken geen onderscheid tussen algemene patiënten of pulmonaal belaste patiënten. Daarmee was het voor de werkgroep lastig om een specifieke uitspraak te doen voor pulmonaal belaste patiënten. Daarnaast kon over de kwaliteit van leven geen uitspraak worden gedaan omdat deze uitkomstmaat niet werd gerapporteerd.
Omdat de beschreven studies wel een beschermend effect lieten zien in de algemene populatie, lijkt het zinvol om ademverdiepingsoefeningen bij alle patiënten toe te passen.
Op basis van expert opinion zou een hoogrisicopatiënt (hoge leeftijd, diabetes, roken en pulmonale voorgeschiedenis, bestaande sputumproblemen, langdurige beademing) die een ingreep in de bovenbuik of intrathoracaal moet ondergaan, mogelijk baat hebben bij ademspiertraining en/of het aanleren van sputum-evacuerende technieken onder begeleiding van een (long)fysiotherapeut.
Onderbouwing
Achtergrond
Introduction
It is unclear whether pre- and postoperative pulmonary optimization by physiotherapy reduces the risk of developing postoperative pulmonary complications in patients with a pulmonary precondition. Preoperative involvement of an anesthesiologist is often difficult to organize, therefore any preoperative optimalisation will also depend on other healthcare providers e.g. physiotherapists. As it is uncertain whether pre-operative pulmonary optimization by physiotherapy provides a benefit that justifies the effort required, we performed this systematic review.
Conclusies / Summary of Findings
Postoperative pulmonary complications
Preoperative physiotherapy
|
Very low GRADE |
The evidence is very uncertain about the effect of preoperative physiotherapy on postoperative pulmonary complications when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Sources: Ball, 2020; Kulkarni, 2010; Onerup, 2022 |
Perioperative physiotherapy
|
Low GRADE |
Perioperative physiotherapy may reduce postoperative pulmonary complications when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Sources: Ball, 2020; Chen, 2022; Huang, 2022; Qin, 2020 |
Postoperative physiotherapy
|
Low GRADE |
Postoperative physiotherapy may reduce postoperative pulmonary complications when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Sources: Ball, 2020; Svensson-Raskh, 2021; Yamana, 2015 |
Quality of life
Preoperative physiotherapy
|
No GRADE |
No evidence was found regarding the effect of preoperative physiotherapy on quality of life when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Source: - |
Perioperative physiotherapy
|
Very low GRADE |
The evidence is very uncertain about the effect of perioperative physiotherapy on quality of life when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Source: Huang, 2022 |
Postoperative physiotherapy
|
No GRADE |
No evidence was found regarding the effect of postoperative physiotherapy on quality of life when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Source: - |
Length of hospital stay
Preoperative physiotherapy
|
Very low GRADE |
The evidence is very uncertain about the effect of preoperative physiotherapy on length of hospital stay when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Source: Onerup, 2022 |
Perioperative physiotherapy
|
Low GRADE |
Perioperative physiotherapy may reduce length of hospital stay when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Source: Chen, 2022; Huang, 2022; Qin, 2020 |
Postoperative physiotherapy
|
Very low GRADE |
The evidence is very uncertain about the effect of postoperative physiotherapy on length of hospital stay when compared with regular care in patients with a pulmonary precondition undergoing major non-pulmonary surgery.
Source: Svensson-Raskh, 2021 |
Samenvatting literatuur
Description of studies
Ball (2020) performed a systematic review and meta-analysis of randomized controlled trials in non-cardiothoracic surgery focusing on preoperative physiotherapy, preoxygenation, intraoperative mechanical ventilation, postoperative prophylactic CPAP or HFNC, and postoperative physiotherapy. RCTs comparing strategies of preoxygenation, preoperative physiotherapy, intraoperative ventilation or postoperative prophylactic CPAP, HFNC, and physiotherapy in surgical patients; adult patients >18 years old; patients undergoing general anesthesia; English language; and specific postoperative lung injury outcomes reported were the inclusion criteria used for the systematic review. Trials of patients undergoing cardiothoracic surgery, trials that did not report the outcomes of interest, case reports, reviews, neonatal studies, and pediatric and neonatal studies were excluded. A systematic search was conducted until August 2020, in the Cochrane Central Register of Controlled Trials, MEDLINE, and EMBASE. In total, 39 randomized controlled trials were included in the systematic review, but only 20 RCTs were taken into account here. Relevant study characteristics are presented in table 1. The following relevant outcome measure was reported in the systematic review: postoperative pulmonary complications.
Chen (2022) performed a prospective randomized controlled trial to investigate the impact of breathing exercises on recovery in elderly patients receiving laparoscopic colorectal surgery. Patients aged from 65 to 80 years, diagnosed with primary colorectal tumor receiving elective laparoscopic colorectal surgery, undergoing general anesthesia, with a BMI between 18 mg/m2 and 30 kg/m2, and ASA grading scale from I to III were eligible for trial participation. In total, 264 patients were randomized to either the intervention or control group. The intervention group (n=132) received breathing exercises and standardized ERAS care. The control group (n=132) received standardized ERAS strategies. The duration of the follow-up was 90 days postoperatively. The study reported the following relevant outcome measures: postoperative pulmonary complications, length of hospital stay.
Huang (2022) performed a randomized controlled trial to determine the effect of a fully engaged inspiratory muscle training (IMT) on PPCs and respiratory function in patients undergoing upper abdominal surgery. Patients 20 years or older with abdominal surgery, ASA I to IV, BMI of at least 18 and able to follow the exercise protocol were eligible for trial participation. In total, 30 patients were randomized to either the intervention or control group. The intervention group (n=14) received a fully engaged IMT program. The control group (n=16) received regular health care. The duration of the follow-up was 1 week after discharge (4 weeks postoperatively). The study reported the following relevant outcome measures: postoperative pulmonary complications, length of hospital stay, quality of life.
Kulkarni (2010) performed a randomized pilot study to assess the effect of pre-operative IMT on respiratory variables in patients undergoing major abdominal surgery. Patients who were over eighteen years of age, undergoing major abdominal general surgery, or major urological surgery, with ASA grades I-IV requiring any length of hospital stay were eligible for trial participation. In total, 80 patients were randomized to either intervention or control. Three intervention groups were compared with one control group. Intervention group B (n=20) received deep breathing exercises, intervention group C (n=20) received incentive spirometry, and intervention group D (n=20) received a Powerbreathe® (a hand-held inspiratory muscle trainer). The control group A (n=20) received no intervention. For this analysis, intervention group D was compared with control group A. The duration of the follow-up was between one and seven days postoperatively. The study reported the following relevant outcome measure: postoperative pulmonary complications.
Qin (2020) performed a single-blind randomized controlled trial to determine whether perioperative breathing training reduces the incidence of postoperative pulmonary complications in patients undergoing laparoscopic colorectal surgery. Patients over 18 years old who had received elective laparoscopic colorectal surgery were eligible for trial participation. In total, 245 patients were randomized to either the intervention or control group. The intervention group (n=122) received breathing training for at least five days and standard care. The control group (n=123) received standard care. The duration of the follow-up was until hospital discharge. The study reported the following relevant outcome measures: postoperative pulmonary complications, length of hospital stay.
Svensson-Raskh (2021) performed a randomized controlled trial to investigate if mobilization out of bed, within 2 hours after abdominal surgery, improved participants’ respiratory function and whether breathing exercises had an additional positive effect. Patients speaking Swedish or English, planned for elective gynecological, urological or endocrinological open or robot-assisted laparoscopic surgery because of cancer, with an expected anesthetic duration of at least two hours were considered eligible for trial participation. In total, 214 patients were randomized to either the intervention or one of the two control groups. The intervention group (n=73) received early mobilization and breathing exercises (PEP). The first control group (n=76) received early mobilization and the second control group (n=65) received no interventions. The duration of the follow-up was at least four hours postoperatively. The study reported the following relevant outcome measures: postoperative pulmonary complications (pneumonia, respiratory insufficiency), length of hospital stay.
Onerup (2022) performed a randomized, parallel, open-label controlled trial to determine the effect of a short-term, unsupervised exercise intervention before and after colorectal cancer surgery on self-assessed physical recovery. Patients 20 years or older, planned for elective colorectal cancer surgery at any of the recruiting hospitals were eligible for trial participation. In total, 761 patients were randomized to either the intervention or control group. The intervention group (n=379) received daily aerobic activity, IMT and general information and instructions about local routines. The control group (n=382) received general information and instructions about local routines. The duration of the follow-up was twelve months. The study reported the following relevant outcome measures: postoperative pulmonary complications (pneumonia, respiratory insufficiency), length of hospital stay.
Yamana (2015) performed a prospective randomized controlled study to examine the efficacy of preventing postoperative pulmonary complications by an intensive preoperative respiratory rehabilitation program for esophageal cancer patients. Patients with esophageal cancer who underwent esophagectomy with gastric tube reconstruction were eligible for trial participation. In total, 63 patients were randomized to either intervention or control. The intervention group (n=30) received a preoperative respiratory rehabilitation program. The control group (n=30) received no preoperative respiratory rehabilitation program. The duration of the follow-up was not reported. The study reported the following relevant outcome measure: postoperative pulmonary complications.
Table 1. Study characteristics of the included studies
|
|
||||||||
|
25-30 min, twice a day, five days per week for at least 2 weeks |
||||||||
|
I1: 73, 72 (IQR 63.5-77) years, 62% |
||||||||
NR: not reported, NA: not applicable, RMT: Respiratory muscle training, ET: Endurance training, Combined: combination of RMT and ET, MIA: minimally invasive approach. *Moderate intensity: achieve <75%of maximal heart rate for ET; achieve ≥30% of maximal inspiratory pressure or ≥30% of maximal voluntary ventilation or use volumetric/incentive spirometry for RMT; or no physiological marker used as a target for ET/RMT. High intensity: achieve ≥75%of maximal heart rate, 100% of peak work rate, or >5% of rate perceived exercise for ET; achieve ≥60% of maximal inspiratory pressure or guided to achieve rate of perceived exercise >5% for RMT
Results
Postoperative pulmonary complications (PPC)
Preoperative physiotherapy
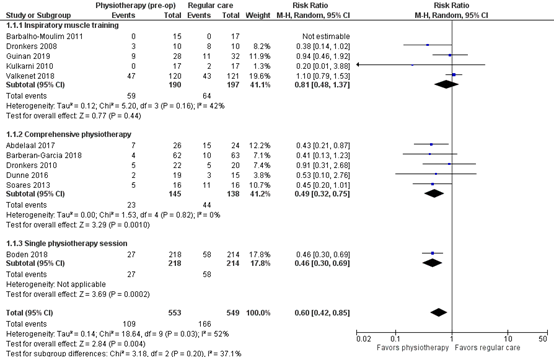
One systematic review and two additional studies reported the incidence of PPCs after preoperative physiotherapy (Ball, 2020; Kulkarni, 2010; Onerup, 2022). The results are presented in Figure 1. With 109 events of postoperative pulmonary complications in 553 patients in the preoperative physiotherapy group and 166 events of postoperative pulmonary complications in 549 patients in the regular care group, the pooled risk ratio (RR) was 0.60 (95% CI 0.42 to 0.85), in favor of the patients who received preoperative physiotherapy. This difference is considered clinically relevant in favor of preoperative physiotherapy.
Figure 1. Postoperative pulmonary complications after preoperative physiotherapy
Z: p-value of the pooled effect; df: degrees of freedom; I2: statistic heterogeneity; CI: Confidence Interval
Postoperative pneumonia
One study reported the outcome measure postoperative pneumonia (Onerup, 2022). In total, 10 of the 317 patients (3.2%) who received pre-operative physiotherapy, and 13 of the 351 patients (3.7%) who received regular care had postoperative pneumonia. The RR was 0.85 (95% CI 0.38 to 1.92), in favor of the patients who received pre-operative physiotherapy. This difference is not considered clinically relevant.
Perioperative physiotherapy
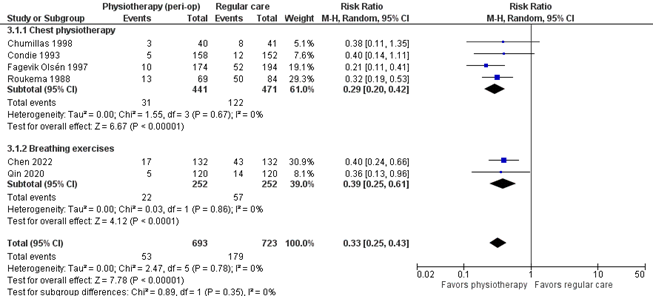
One systematic review and three additional studies reported the incidence of PPCs after perioperative physiotherapy (Ball, 2020; Chen, 2022; Huang, 2022; Qin, 2020). Huang (2022) reported the total number of PPCs, but did not report the number of patients that experienced one or more PPCs. Therefore these results cannot be taken into account to calculate the overall effect. The results are presented in Figure 2. With 53 events of postoperative pulmonary complications in 693 patients in the perioperative physiotherapy group and 179 events of postoperative pulmonary complications in 723 patients in the regular care group, the pooled risk ratio was 0.33 (95% CI 0.25 to 0.43), in favor of the patients who received perioperative physiotherapy. This difference is considered clinically relevant.
Figure 2. Postoperative pulmonary complications after perioperative physiotherapy
Z: p-value of the pooled effect; df: degrees of freedom; I2: statistic heterogeneity; CI: Confidence Interval
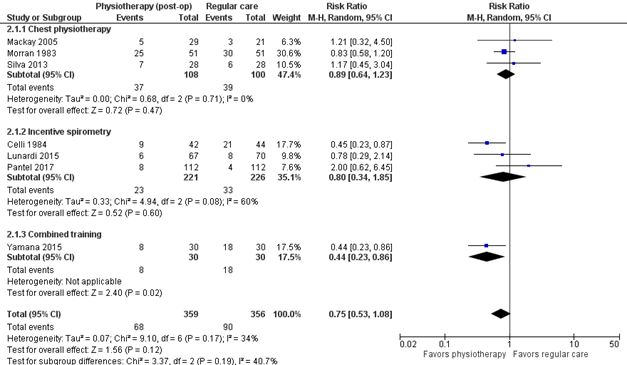
Postoperative physiotherapy
One systematic review and one additional study reported the incidence of PPCs after postoperative physiotherapy (Ball, 2020; Yamana, 2015). The results are presented in Figure 3. With 68 events of postoperative pulmonary complications in 359 patients in the postoperative physiotherapy group and 90 events of postoperative pulmonary complications in 356 patients in the regular care group, the pooled RR was 0.75 (95% CI 0.53 to 1.08), in favor of the patients who received postoperative physiotherapy. This difference is considered clinically relevant in favor of postoperative physiotherapy.
Figure 3. Postoperative pulmonary complications after postoperative physiotherapy
Z: p-value of the pooled effect; df: degrees of freedom; I2: statistic heterogeneity; CI: Confidence Interval
Respiratory insufficiency
One study reported the outcome measure respiratory insufficiency (Svensson-Raskh, 2021). Svensson-Raskh (2021) reported an Odds Ratio (OR) of 0.73 (95% CI 0.33 to 1.61) in favor of the group of patients that received mobilization and breathing exercises when compared with the control group. This difference is considered clinically relevant.
Pneumonia
One study reported the outcome measure pneumonia (Svensson-Raskh, 2021). Svensson-Raskh (2021) reported an OR of 0.17 (95% CI 0.02 to 1.47) in favor of the group of patients that received mobilization and breathing exercises when compared with the control group. This difference is considered clinically relevant.
Quality of life
Preoperative physiotherapy
None of the studies reported the outcome measure quality of life for a postoperative physiotherapy intervention.
Perioperative physiotherapy
One study reported the outcome measure quality of life (Huang, 2022).
Huang (2022) reported the outcome measure quality of life at one week after discharge, measured by the World Health Organization Quality of Life Briefing. Different domains were included in the test: physical health, psychological state, social relationships, and environment.
- Physical health domain: The patients who received IMT (n=13) had a mean WHOQOL-BREF score of 24.1 ± 3.5 at one week after discharge, compared with 22.8 ± 4 for the patients in the control group (n=15). The mean difference between the groups was 1.30 (95% CI -1.48 to 4.08), in favor of the patients who received IMT. This difference is not considered clinically relevant.
- Psychological domain: The patients who received IMT (n=13) had a mean WHOQOL-BREF score of 21.1 ± 2.6 at one week after discharge, compared with 20.6 ± 4 for the patients in the control group (n=15). The mean difference between the groups was 0.50 (95% CI -1.97 to 2.97), in favor of the patients who received IMT. This difference is not considered clinically relevant.
- Social relationships domain: The patients who received IMT (n=13) had a mean WHOQOL-BREF score of 14.2 ± 1.6 at one week after discharge, compared with 13.9 ± 1.8 for the patients in the control group (n=15). The mean difference between the groups was 0.30 (95% CI -0.96 to 1.56), in favor of the patients who received IMT. This difference is not considered clinically relevant.
- Environment domain: The patients who received IMT (n=13) had a mean WHOQOL-BREF score of 33.7 ± 3.4 at one week after discharge, compared with 31.6 ± 3.1 for the patients in the control group (n=15). The mean difference between the groups was 2.10 (95% CI -0.32 to 4.52), in favor of the patients who received IMT. This difference is not considered clinically relevant.
Postoperative physiotherapy
None of the studies reported the outcome measure quality of life for a postoperative physiotherapy intervention.
Length of hospital stay
Preoperative physiotherapy
One study reported the outcome measure length of hospital stay (Onerup, 2022).
Onerup (2022) reported length of index hospital stay. The patients who received pre-operative physiotherapy (n=317) had a mean length of hospital stay of 9 days (SD ± 9 days), and the patients who received control (n=351) had a mean length of hospital stay of 9 days (SD ± 8 days). The mean difference between the groups was 0.00 (95% CI -1.30 to 1.30), which indicates there was no difference between the groups.
Perioperative physiotherapy
Three studies reported the outcome measure length of hospital stay (Chen, 2022; Huang, 2022; Qin, 2020).
Chen (2022) reported length of stay. The patients who received pre-operative physiotherapy (n=132) had a median length of stay of 5 days (IQR 3-8), and the patients who received control (n=132) had a median length of stay of 7 days (IQR 4-10). The difference in medians was -2 days, in favor of the patients who received pre-operative physiotherapy. This difference is considered clinically relevant.
Huang (2022) reported length of hospitalization. The patients who received pre-operative physiotherapy (n= 13) had a mean length of hospitalization of 21.5 days, and the patients who received control (n=15) had a mean length of hospitalization of 18.5 days. The mean difference was 3 days, in favor of the patients who received control. This difference is considered clinically relevant.
Qin (2020) reported length of stay. The patients who received pre-operative physiotherapy (n=120) had a median length of stay of 6 days (IQR 5-7), and the patients who received control (n=120) had a median length of stay of 8 days (IQR 7-9). The difference in medians was -2 days, in favor of the patients that received pre-operative physiotherapy. This difference is considered clinically relevant.
Postoperative physiotherapy
One study reported the outcome measure length of hospital stay (Svensson-Raskh, 2021). The patients who received mobilization and breathing exercises (n=73) had a mean length of hospital stay of 5 days (SD ± 3 days), the patients who received mobilization only (n=76) had a mean length of hospital stay of 4 days (SD ± 3 days), and the patients who received control (n=65) had a mean length of hospital stay of 4 days (SD ± 3 days). The mean difference between the patients who received mobilization and breathing exercises and the patients who received control was 1 day (95% CI -0.00 to 2.00), in favor of the patients who received control. This difference is considered clinically relevant.
Level of evidence of the literature
The level of evidence for all outcomes was based on randomized controlled trials and therefore started at high.
Postoperative pulmonary complications
Preoperative physiotherapy
The level of evidence regarding the outcome measure postoperative pulmonary complications after preoperative physiotherapy was downgraded by three levels to VERY LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), because of study limitations (risk of bias, -1), and because the confidence interval exceeds the lower limit for clinical relevance (imprecision, -1).
Perioperative physiotherapy
The level of evidence regarding the outcome measure postoperative pulmonary complications after perioperative physiotherapy was downgraded by two levels to LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), and because of study limitations (risk of bias, -1).
Postoperative physiotherapy
The level of evidence regarding the outcome measure postoperative pulmonary complications after postoperative physiotherapy was downgraded by two levels to LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), and because the confidence interval exceeds the lower limit for clinical relevance (imprecision, -1).
Quality of life
Preoperative physiotherapy
The level of evidence regarding the outcome measure quality of life after preoperative physiotherapy interventions was not determined, since this was not reported in the included systematic review and additional studies.
Perioperative physiotherapy
The level of evidence regarding the outcome measure quality of life after perioperative physiotherapy was downgraded by three levels to VERY LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), and because of the very small sample size (imprecision, -2).
Postoperative physiotherapy
The level of evidence regarding the outcome measure quality of life after postoperative physiotherapy interventions was not determined, since this was not reported in the included systematic review and additional studies.
Length of hospital stay
Preoperative physiotherapy
The level of evidence regarding the outcome measure length of hospital stay after preoperative physiotherapy was downgraded by three levels to VERY LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), and because the confidence interval exceeds the lower and upper limits for clinical relevance (imprecision, -2).
Perioperative physiotherapy
The level of evidence regarding the outcome measure length of hospital stay after perioperative physiotherapy was downgraded by two levels to LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), and because of the small sample size (imprecision, -1).
Postoperative physiotherapy
The level of evidence regarding the outcome measure length of hospital stay after postoperative physiotherapy was downgraded by three levels to VERY LOW because the study population also included patients without a pulmonary precondition (indirectness, -1), and because of the very small sample size (imprecision, -2).
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
What are the benefits and harms of preoperative (pulmonary) physiotherapy in patients with pulmonary precondition undergoing non-pulmonary surgery?
| P (Patients): | Patients with a pulmonary precondition undergoing major non-pulmonary surgery |
| I (Intervention): | Pre-, peri- or postoperative (lung)physiotherapy |
| C (Comparison): | Regular care (no (lung)physiotherapy before or after surgery) |
| O (Outcomes): |
Postoperative pulmonary complications, quality of life, length of hospital stay |
Relevant outcome measures
The guideline development group considered postoperative pulmonary complications as a critical outcome measure for decision making; and quality of life and length of hospital stay as an important outcome measure for decision making.
A priori, the working group did not define the outcome measures listed above but used the definitions used in the studies.
The working group defined the following minimal clinically (patient) important differences:
- postoperative pulmonary complications: 25%: RR <0.8 or >1.25;
- quality of life: 10% difference of the maximum score;
- length of hospital stay: At least 1 day.
Search and select (Methods)
The search was based on a recent systematic review about the effect of pre-admission interventions on postoperative outcomes in patients undergoing major elective surgery (Perry, 2021). The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms from June 2020 (the search date of the systematic review by Perry, 2021) until 11 July 2023. This resulted in 310 hits. The search was updated and expanded to also include perioperative and postoperative interventions on 13 May 2024. This resulted in 264 additional hits. The detailed search strategy is depicted under the tab Methods.
Studies were selected based on the following criteria:
- Systematic review or randomized controlled trial
- Type of surgery: major non-pulmonary surgery (including intrathoracic procedures)
- Preoperative, perioperative or postoperative (lung)physiotherapy intervention vs standard care
- Intervention: only preoperative (lung)physiotherapy intervention, no combination with other modalities
- Reporting at least one of the outcomes specified in the PICO.
24 studies were initially selected based on title and abstract screening for systematic reviews. After reading the full texts, 1 systematic review was included and 23 studies were excluded. Additionally, 2 randomized controlled trials from another systematic review were included. Subsequently, RCTs published after the search date of the included systematic review (August 2020) were identified. 33 studies were initially selected based on title and abstract screening. After reading the full texts, 28 studies were excluded and 5 studies were included. See the table with reasons for exclusion under the tab Methods).
Results
One systematic review and seven additional randomized controlled trials were included in the analysis of the literature. Important study characteristics, results and the assessment of the risk of bias are summarized in the evidence table.
Referenties
- Ball L, Almondo C, Pelosi P. Perioperative Lung Protection: General Mechanisms and Protective Approaches. Anesth Analg. 2020 Dec;131(6):1789-1798. doi: 10.1213/ANE.0000000000005246. PMID: 33186165.
- Chen J, Peng LH, Min S. Implementation of perioperative breathing exercises and its effect on postoperative pulmonary complications and long-term prognosis in elderly patients undergoing laparoscopic colorectal surgery: A randomized controlled trial. Clin Rehabil. 2022 Sep;36(9):1229-1243. doi: 10.1177/02692155221097762. Epub 2022 May 29. PMID: 35635180.
- Huang YT, Lin YJ, Hung CH, Cheng HC, Yang HL, Kuo YL, Chu PM, Tsai YF, Tsai KL. The fully engaged inspiratory muscle training reduces postoperative pulmonary complications rate and increased respiratory muscle function in patients with upper abdominal surgery: a randomized controlled trial. Ann Med. 2022 Dec;54(1):2222-2232. doi: 10.1080/07853890.2022.2106511. PMID: 35942800; PMCID: PMC9455324.
- Kulkarni SR, Fletcher E, McConnell AK, Poskitt KR, Whyman MR. Pre-operative inspiratory muscle training preserves postoperative inspiratory muscle strength following major abdominal surgery - a randomised pilot study. Ann R Coll Surg Engl. 2010 Nov;92(8):700-7. doi: 10.1308/003588410X12771863936648. Epub 2010 Jul 26. PMID: 20663275; PMCID: PMC3229384.
- Onerup A, Andersson J, Angenete E, Bock D, Börjesson M, Ehrencrona C, Fagevik Olsén M, Larsson PA, de la Croix H, Wedin A, Haglind E. Effect of Short-term Homebased Pre- and Postoperative Exercise on Recovery After Colorectal Cancer Surgery (PHYSSURG- C): A Randomized Clinical Trial. Ann Surg. 2022 Mar 1;275(3):448-455. doi: 10.1097/SLA.0000000000004901. PMID: 33843798; PMCID: PMC8820776.
- Perry R, Herbert G, Atkinson C, England C, Northstone K, Baos S, Brush T, Chong A, Ness A, Harris J, Haase A, Shah S, Pufulete M. Pre-admission interventions (prehabilitation) to improve outcome after major elective surgery: a systematic review and meta- analysis. BMJ Open. 2021 Sep 30;11(9):e050806. doi: 10.1136/bmjopen-2021- 050806. PMID: 34593498; PMCID: PMC8487197.
- Qin PP, Jin JY, Wang WJ, Min S. Perioperative breathing training to prevent postoperative pulmonary complications in patients undergoing laparoscopic colorectal surgery: A randomized controlled trial. Clin Rehabil. 2021 May;35(5):692-702. doi: 10.1177/0269215520972648. Epub 2020 Dec 7. PMID: 33283533.
- Svensson-Raskh A, Schandl AR, Ståhle A, Nygren-Bonnier M, Fagevik Olsén M. Mobilization Started Within 2 Hours After Abdominal Surgery Improves Peripheral and Arterial Oxygenation: A Single-Center Randomized Controlled Trial. Phys Ther. 2021 May 4;101(5):pzab094. doi: 10.1093/ptj/pzab094. PMID: 33742678; PMCID: PMC8136304.
- Yamana I, Takeno S, Hashimoto T, Maki K, Shibata R, Shiwaku H, Shimaoka H, Shiota E, Yamashita Y. Randomized Controlled Study to Evaluate the Efficacy of a Preoperative Respiratory Rehabilitation Program to Prevent Postoperative Pulmonary Complications after Esophagectomy. Dig Surg. 2015;32(5):331-7. doi: 10.1159/000434758. Epub 2015 Jul 14. PMID: 26183420.
Evidence tabellen
Definitie van PPC’s in de verschillende studies
|
Author, year |
Definition criteria PPCs |
|
Barbalho-Moulim, 2011 |
Pneumonia: temperature >38°C, productive cough with purulent sputum, presence of pulmonary infiltration on chest X- ray, increased leukocyte count) Atelectasis: based on chest X- rays and associated with respiratory discomfort Acute respiratory failure: poor gas exchange and requirement for mechanical ventilation |
|
Roukema, 1988 |
Grade I: Minor atelectasis in 1 lung, no hypoxemia or hypoxemia <3d duration, no fever Grade II: Minor atelectasis in both lungs or major atelectasis in one lung, hypoxemia <3d duration, no fever Grade III: Major atelectasis in 1 lung or in both lungs, hypoxemia >3d duration, fever >3d duration |
|
Condie, 1993 |
- |
|
Fagevik Olsén, 1997 |
- |
|
Chumillas, 1998 |
Bronchitis: Chest X-ray negative, temperature of <37.5 degrees Celsius, auscultation rales, sputum abundant and clear Atelectasis: Chest X-ray collapse, diaphragmatic elevation, temperature of < 38 degrees Celsius, auscultation diminished or abolished vesicular murmur Pneumonia: Chest X-ray consolidation, pleurisy, temperature of <38 degrees Celsius at least 4 days, auscultation rales, sputum abundant and purulent |
|
Dronkers, 2008 |
- |
|
Barbalho-Moulim, 2011 |
Pneumonia: temperature >38°C, productive cough with purulent sputum, presence of pulmonary infiltration on chest X- ray, increased leukocyte count) Atelectasis: based on chest X- rays and associated with respiratory discomfort Acute respiratory failure: poor gas exchange and requirement for mechanical ventilation |
|
Valkenet, 2018 |
Pneumonia: a score of 2 points or more with at least 1 point assigned based on Temperature (≥ 36⋅1 and ≤ 38.4°C: 0; ≤ 36⋅0 and ≥ 38⋅5°C: 1), Leucocyte count (≥ 4⋅0 and ≤ 11⋅0 × 109 /l: 0; < 4⋅0 or > 11⋅0 × 109 /l: 1), chest X-rays (No infiltrate: 0; Diffused (or patchy) infiltrate: 1; Well circumscribed infiltrate: 2) |
|
Guinan, 2019 |
- |
|
Onerup, 2022 |
- |
|
Huang, 2022 |
Respiratory infection: Patient has received antibiotics for a suspected respiratory infection and met one or more of the following criteria: new or changed sputum, new or changed lung opacities, fever, white blood cell count > 12 x 10^9 /L Respiratory failure: Postoperative PaO2 < 8 kPa (60 mmHg) on room air, a PaO2:FI02 ratio < 90% and requiring oxygen therapy Pleural effusion: Chest radiograph demonstrating blunting of the costophrenic angle, loss of sharp silhouette of the ipsilateral hemidiaphragm in upright position, evidence of displacement of adjacent anatomical structures or (in supine position) a hazy opacity in one hemithorax with preserved vascular shadows Atelectasis: Lung opacification with a shift of the mediastinum, hilum or hemidiaphragm toward the affected area, and compensatory over-inflation in the adjacent non-atelectatic lung Pneumothorax: Air in the pleural space with no vascular bed surrounding the visceral pleura Bronchospasm: Newly detected expiratory wheezing treated with bronchodilators Aspiration pneumonitis: Acute lung injury after the inhalation of regurgitated gastric contents |
|
Kulkarni, 2010 |
Pneumonia: based on positive sputum culture and antibiotic treatment |
|
Dronkers, 2010 |
Atelectasis, diagnosed on chest-XRays by a “blinded” radiologist Pneumonia, fever, cough, and development of purulent sputum, in conjunction with radiologic evidence of a new or progressive pulmonary infiltrate, a suggestive Gram stain, and positive cultures of sputum, tracheal aspirate, pleural fluid, or blood Acute respiratory failure, need for mechanical ventilation |
|
Soares, 2013 |
Pneumonia: based on clinical, laboratory and chest X-rays as well as the need for antibiotic therapy Atelectasis, based on chest X-rays and need for bronchoscopy |
|
Dunne, 2016 |
- |
|
Abdelaal, 2017 |
- |
|
Barberan-Garcia, 2018 |
Clavien-Dindo classification or Thoracic Morbidity and Mortality classification for all complications (grades I to V) (Dindo D, Demartines N, Clavien PA. Ann Surg 2004; 240 :205-13) Grade I: complication without need for pharmacologic treatment or other intervention. Grade II: complication requiring pharmacologic treatment or minor intervention. Grade III: complication requiring surgical, radiologic, endoscopic intervention, or multitherapy. Grade IIIa: invasive treatment with no need for general anesthesia Grade IIIb: invasive treatment under general anesthesia Grade IV: complication requiring intensive care unit management and life support. Grade IVa: single organ major dysfunction. Grade IVb: multiorgan major dysfunction. Grade V: complication leading to the death of the patient. |
|
Boden, 2018 |
Diagnosis confirmed when four or more criteria are present in a postoperative day: ∙ New abnormal breath sounds on auscultation different from in the preoperative assessment ∙ Production of yellow or green sputum different from in the preoperative assessment ∙ Pulse oximetry oxygen saturation (SpO2 ) 38°C on more than one consecutive postoperative day ∙ Chest radiography report of collapse or consolidation ∙ An unexplained white cell count greater than 11×109 /L ∙ Presence of infection on sputum culture report ∙ Physician’s diagnosis of pneumonia, lower or upper respiratory tract infection, an undefined chest infection, or prescription of an antibiotic for a respiratory infection |
|
Qin, 2020 |
Pneumonia: chest radiograph with at least one of the following: infiltrates, consolidation, cavitation; and at least one of the following: fever (>38°C) with no other recognized cause, white cell count >12×109 /l or 70years old with altered mental status with no other recognized cause; and at least two of the following: purulent sputum or increased respiratory secretions, cough or dyspnea or tachypnoea, rales or bronchial breath sounds, worsening gas exchange. Atelectasis: Lung opacification with a shift of the mediastinum, hilum or hemidiaphragm toward the affected area, and compensatory overexpansion in the adjacent non-atelectatic area. Respiratory failure: Postoperative PaO2 <60 mmHg on room air, Ol < 300 mmHg or arterial oxyhemoglobin saturation measured with pulse oximetry <90% and requiring oxygen therapy Unplanned intubations: Placement of a breathing tube and ventilator support which was not intended or planned |
|
Chen, 2022 |
Respiratory failure: PaO2 < 60 mmHg when breathing in room air, FiO2 < 300mmHg or arterial oxygen saturation measured with pulse oximetry < 90% and requiring oxygen therapy Pleural effusion: Chest X-ray demonstrates blunting of the costophrenic angle, loss of clear contour of ipsilateral hemidiaphragm in upright position, displacement of adjacent anatomical structures to the unimpaired side, or a hazy opacity in one hemithorax with preserved vascular shadows in supine position Atelectasis: Chest X-ray or computed tomography reveals that mediastinum, hilum, or diaphragm move toward the affected area and compensatory hyper-aeration occurs in the adjacent non-atelectasis area Pneumonia Chest X-ray or computed tomography shows new or progressive and persistent infiltrates in the lungs with at least one of the following: body temperature ≥38.5°C or 12 × 109 /l or <4 x 10^9 and with at least two of the following purulent sputum, new cough or dyspnea, worsening of previous cough or dyspnea Pneumothorax: Chest X-ray or computed tomography shows air in the pleural space with no vascular bed around the visceral pleura |
|
Yamana, 2015 |
Clavien-Dindo classification or Thoracic Morbidity and Mortality classification for all complications (grades I to V) Grade I: complication without need for pharmacologic treatment or other intervention. Grade II: complication requiring pharmacologic treatment or minor intervention. Grade III: complication requiring surgical, radiologic, endoscopic intervention, or multitherapy. Grade IIIa: invasive treatment with no need for general anesthesia Grade IIIb: invasive treatment under general anesthesia Grade IV: complication requiring intensive care unit management and life support. Grade IVa: single organ major dysfunction. Grade IVb: multiorgan major dysfunction. Grade V: complication leading to the death of the patient. |
|
Morran, 1983 |
- |
|
Mackay, 2005 |
A postoperative pulmonary complication is deemed to have occurred if three or more of the following respiratory signs occur within the same day, in the first 14 days after surgery: • Auscultation changes (decreased breath sounds, crackles, wheezes, bronchial breathing) that were additional to those found prior to surgery. • Temperature over 38 degrees Celsius. • Chest X-ray changes consistent with collapse, consolidation, or atelectasis. • Increase in amount and/or changed colour of sputum produced, compared to what the patient reports is usual for them. |
|
Silva, 2013 |
A postoperative pulmonary complication is deemed to have occurred if three or more of the following signs occur within the same day: • Auscultation changes (decreased breath sounds, crackles, wheezes, bronchial breath sounds) in addition to those prior to surgery • Otherwise unexplained temperature >38 ◦C • Chest radiography changes (atelectasis, collapse, consolidation) • Changes to sputum (increase in amount and/or change in colour) compared with what the patient reports is usual for them |
|
Celli, 1984 |
- |
|
Lunardi, 2015 |
- |
|
Pantel, 2017 |
- |
|
Svensson-Raskh, 2021 |
- |
Risk of bias table
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measure
LOW Some concerns HIGH
|
|
From Ball, 2020 |
|||||||
|
Roukema, 1988 |
Probably yes
Reason: Randomization was done by odd or even year of birth. |
No information
Reason: Not reported. |
Definitely no
Reason: It was not possible to blind patients and health care providers. |
Probably yes
Reason: No loss-to-follow-up or missing outcome data reported. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Probably yes
Reason: No other problems noted. |
Some concerns
|
|
Condie, 1993 |
Definitely yes
Reason: Patients were allocated to groups using a table of random numbers. |
No information
Reason: Not reported. |
Definitely no
Reason: The independent observer did not know to which group each patient had been allocated. |
Definitely yes
Reason: 20 of the 330 patients were lost-to-follow-up, which is less than 10%. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Definitely no
Reason: Personnel involved in treatment and outcome measurement, possible interrater unreliability, treatment time, number of breathing exercises varied. |
Some concerns |
|
Fagevik Olsén, 1997 |
Probably yes
Reason: To avoid patient interference a cluster randomization was performed to alternate months. |
No information
Reason: Not reported. |
Definitely no
Reason: It was not possible to blind patients and health care providers. |
Definitely yes
Reason: 4 of 368 did not complete the study, which is less than 10%. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Probably no
Reason: More determinants for pulmonary complications such as length of anaesthesia and type of operation should be taken into account. |
Some concerns |
|
Chumillas, 1998 |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
Probably yes
Reason: No loss-to-follow-up or missing outcome data reported. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Definitely no
Reason: Limitations due to sample size |
HIGH |
|
Dronkers, 2008 |
Definitely yes
Reason: An independent research assistant randomly assigned patients to the intervention or control group. |
Definitely yes
Reason: An independent research assistant randomly assigned patients to the intervention or control group by opening a sealed and numbered envelope. |
Definitely no
Reason: The main postoperative outcome was diagnosed by a blinded radiologist. Single-blind study. Patients and physiotherapists could not be blinded. |
Definitely yes
Reason: All patients completed primary outcome assessment, secondary outcomes assessment was not completed by 6 of 20 patients. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Probably no
Reason: Relatively small groups, underpowered. |
Some concerns |
|
Barbalho-Moulim, 2011 |
Definitely yes
Reason: Patients were randomly assigned to the intervention or control group by opening a sealed envelope. |
Definitely yes
Reason: Patients were randomly assigned to the intervention or control group by opening a sealed envelope. |
Definitely no
Reason: The images were analysed by a radiologist who was blinded to the information regarding to which group each patient belonged. |
Definitely yes
Reason: All patients completed postoperative assessment. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Probably yes
Reason: No other problems noted. |
LOW |
|
Valkenet, 2018 |
Definitely yes
Reason: Participants were assigned randomly in a 1:1 ratio to intervention and control. Randomization was concealed and performed with a web-based system. |
No information
Reason: Not reported. |
Definitely no
Reason: Assessors of the baseline and follow-up measurements, and assessors of the postoperative outcomes were blinded for allocation. Patients and physiotherapists could not be blinded. |
Definitely no
Reason: 29 of 270 patients were lost to follow-up, which is more than 10%. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Probably yes
Reason: No other problems noted. |
Some concerns |
|
Guinan, 2019 |
Definitely yes
Reason: Randomization was performed on a 1:1 ratio using a flexible web-based randomized system. |
No information
Reason: Not reported. |
Definitely no
Reason: Baseline assessments were completed by a physiotherapist that was blinded to the participants’ intervention assignment. Patients and physiotherapists could not be blinded. |
Definitely no
Reason: 12 of 72 patients were lost to follow-up, which is more than 10%. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Definitely no
Reason: Results are a subset of a larger trial, statistical power not high enough, randomization stratified by recruiting site, full data not available at all time points, use of ANCOVA, unsupervised intervention |
HIGH |
|
Dronkers, 2010 |
Definitely yes
Reason: Participants were randomly assigned (block randomization) |
Definitely yes
Reason: Use of prepared envelopes. |
Definitely no
Reason: It was not possible to blind patients and physical therapists. |
Definitely yes
Reason: Loss to follow-up was less than 10%. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Definitely no
Reason: The effect of an intensive therapeutic exercise program was not investigated, patients were less active, study is not powered to detect significant effects on all outcome measures. |
Some concerns |
|
Soares, 2013 |
Definitely yes
Reason: Patients were randomly allocated, by means of sealed envelope randomization. |
Definitely yes
Reason: Patients were randomly allocated, by means of sealed envelope randomization. |
Definitely no
Reason: Neither patients nor physical therapists were blinded to group assignment, and the investigators responsible for data collection were aware of allocation. |
Definitely no
Reason: 9 out of 37 patients were lost to follow-up, which is more than 10%. |
Definitely yes
Reason: All relevant outcome measures were reported. |
Definitely no
Reason: Low-intensity exercises, small sample size and number of participants who completed all variables and all assessments, duration of post-operative physical therapy, heterogeneity of the surgical procedures, lack of strict protocol for assessment of postoperative pulmonary complications. |
Some concerns |
|
Dunne, 2016 |
Definitely yes
Reason: Participants were randomized by means of a random number block randomization list. |
Definitely yes
Reason: An individual, independent of the study group, held this list and provided e-mail results of randomization following recruitment. |
Probably no
Reason: Clinicians providing care were blinded to the intervention and to the results of all but the baseline CPET values. |
Definitely yes
Reason: Loss to follow-up was less than 10%. |
Definitely yes
|
Probably no
Reason: Confirmation for the benefits associated with improved fitness is required in a larger trial. |
LOW |
|
Abdelaal, 2017 |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
Definitely yes
Reason: Loss to follow-up was less than 10%. |
Definitely yes
|
Probably no
Reason: Low-intensity exercises used in the preoperative physical therapy program. |
HIGH |
|
Barberan-Garcia, 2018 |
Definitely yes
Reason: Assignment to group allocation was carried out by means of a computer-generated random number through a web-based centralized procedure. |
No information
Reason: Not reported. |
Definitely no
Reason: The collaborating anaesthesiologists and surgeons who attended and followed the patients to register perioperative incidents were blinded to the patients’ group allocation. |
Definitely no
Reason: 34 of 144 patients were lost to follow-up, which is more than 10%. |
Definitely yes
|
Probably no
Reason: Design limitation. |
HIGH |
|
Boden, 2018 |
Definitely yes
Reason: The allocation sequence was determined by a web based computer generated blocked random number table. |
Definitely yes
Reason: Preoperative physiotherapists randomly assigned consecutive patients using sequentially numbered sealed opaque envelopes containing allocation cards wrapped in aluminium foil. |
Definitely yes
Reason: Site investigators and preoperative physiotherapists aware of group allocation had no contact with patients postoperatively. Patients, postoperative physiotherapists, hospital staff, and statisticians were unaware of group allocation. |
Definitely yes
Reason: 9 of 441 patients were withdrawn, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: Larger sample size needed for some outcome measures, |
LOW |
|
Morran, 1983 |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
Probably yes
Reason: No loss to follow-up reported. |
Definitely yes
|
Probably yes
Reason: No other limitations reported. |
Some concerns |
|
Mackay, 2005 |
Definitely yes
Reason: Patients were randomized using a random numbers table. |
Probably yes
Reason: Concealed allocation prior to the initial contact. |
Probably yes
Reason: All outcomes were assessed by a physiotherapist who was blinded to group allocation. Chest X-ray findings were reported by a radiographer who was blinded. |
Definitely no
Reason: 6 of 56 patients were lost to follow-up, which is more than 10%. |
Definitely yes
|
Probably yes
Reason: No other limitations noted. |
Some concerns |
|
Silva, 2013 |
Probably yes
Reason: An independent investigator selected one of 105 sealed opaque envelopes with the group allocation for that week. All patients operated on during that week were allocated to that group. |
Definitely yes
Reason: An independent investigator selected one of 105 sealed opaque envelopes with the group allocation for that week. All patients operated on during that week were allocated to that group. |
Probably yes
Reason: Patients were blinded, the assessor was blinded, the radiologist was blinded, but the ward physiotherapist was not blinded. |
Definitely yes
Reason: There were no dropouts. |
Definitely yes
|
Definitely no
Reason: Patient numbers were small, with cluster randomization it is unclear whether there was contamination, despite being blinded the staff may have encouraged deep breathing exercises, patient adherence was not measured, the assessor was not involved in group allocation or treatment. |
Some concerns |
|
Lunardi, 2015 |
No information
Reason: Not reported. |
No information
Reason: Not reported. |
Definitely no
Reason: PPC occurrence was monitored by a blinded assessor. Patients and health care providers could not be blinded. |
Definitely yes
Reason: 7 of 164 patients were lost to follow-up, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: The control group performed deep breaths, which could have been considered an intervention, ambulation during hospitalization was not quantified. |
HIGH |
|
Pantel, 2017 |
Probably yes
Reason: Use of a simple randomization scheme for group allocation. Computer randomized list was generated. |
Probably yes
Reason: Patients were randomized by sequentially accessing this list. Concealment of the next allocation was used. |
Definitely no
Reason: Power analysis and statistical analysis were performed by a blinded data assessor. Patients and health care providers could not be blinded. |
Definitely yes
Reason: Missing data of 10 out of 224 patients, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: The study was not powered to detect differences in pulmonary complications, patients with COPD were not stratified, observed compliance in the control group was lower than policy. |
Some concerns |
|
Individual studies |
|||||||
|
Chen, 2022 |
Definitely yes
Reason: Patients were randomly allocated by Statistics Analysis System, which was used to computer-generated random numbers. |
Definitely yes
Reason: Participants were assigned in numerical order with sealed opaque envelopes containing the grouping information by an independent researcher. |
Definitely no
Reason: single blind study, assessment of the 6 min walk test by blinded doctor. Patient could not be blinded. |
Definitely yes
Reason: 5 out of 264 patients were lost to follow-up, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: Relatively small number of patients, patients’ physical activity after discharge was not accurately supervised, single-centre study. |
Some concerns |
|
Huang, 2022 |
Definitely yes
Reason: The online random generator was used for randomization. |
No information
Reason: Not reported. |
Definitely no
Reason: Blinding was not achievable both in subjects and researchers due to an individualized respiratory muscle training program. |
Definitely yes
Reason: 2 out of 30 patients were lost to follow-up, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: Small sample size, single surgical procedure, lack of long-term follow-up. |
Some concerns |
|
Qin, 2020 |
Definitely yes
Reason: Patients were randomly assigned to either an intervention or control group using a computer-generated randomized block design. |
Definitely yes
Reason: The numbers were sealed in sequentially numbered opaque envelopes organized in randomization sequence by an independent researcher. |
Definitely no
Reason: Single-blind study. |
Definitely yes
Reason: 5 out of 245 patients were lost to follow-up, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: The study is unable to evaluate the effect of breathing training on long-term outcomes, the mobilization of patients during hospitalization was not accurately quantified, single large academic hospital. |
Some concerns |
|
Svensson-Raskh, 2021 |
Definitely yes
Reason: A computer-generated randomization in blocks of 9 was used to allocate patients to the different trial groups. |
Definitely yes
Reason: A nurse at the recovery unit, independent of the trial, randomly assigned the patients to the different groups, using opaque sealed envelopes. |
Definitely no
Reason: Patients and health care professionals at the recovery unit were not blinded, but surgeons, anaesthesiologists, research nurses, and physical therapists were blinded. |
Definitely yes
Reason: 13 out of 214 patients were lost to follow-up, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: Baseline imbalances in patient characteristics, study inclusion limited to daytime only, missing PaO2 data, some patients discharged before third hour assessment. |
Some concerns |
|
Onerup, 2022 |
Definitely yes
Reason: Participants were randomly assigned to 1 of the 2 study groups through a computer system creating the allocation sequence with a block size of 4, unknown to personnel. |
Probably yes
Reason: Study numbers were assigned sequentially as patients were recruited and study group could not be changed. |
Definitely no
Reason: Due to the nature of the intervention neither participants nor personnel were blinded. Medical staff was not actively informed, and outcome assessors for postoperative complications and length of hospital stay were masked regarding allocation. |
Definitely no
Reason: 93 out of 761 patients were lost to follow-up, which is more than 10%. |
Definitely no
Reason: The outcome measure quality of life is not reported. |
Definitely no
Reason: Pragmatic design, the primary outcome measure had not been evaluated regarding measurement properties or minimally important difference, Sample size was not calculated for postoperative complications, rate of missing data regarding adherence. |
Some concerns |
|
Kulkarni, 2010 |
Definitely yes
Reason: Patients were allocated to four groups by computer-generated, random numbers placed in sequentially numbered sealed envelopes. |
Definitely yes
Reason: Patients were allocated to four groups by computer-generated, random numbers placed in sequentially numbered sealed envelopes. |
Definitely no
Reason: Group allocation was non-blinded. |
Definitely no
Reason: 14 of the 80 patients were lost-to-follow-up, which is more than 10%. |
Definitely no
Reason: Multiple secondary outcome measures were not reported. |
Probably no
Reason: Some patients may be fitter and at lower risk than others, there may be a case for selecting only high-risk patients, a large number of patients awaiting intra-abdominal cancer surgery were not included. |
HIGH |
|
Yamana, 2015 |
No information
Reason: Not reported. |
Definitely yes
Reason: The patients were randomly assigned by opening a sealed envelope. |
No information
Reason: Not reported. |
Definitely yes
Reason: 3 of the 63 patients were lost-to-follow-up, which is less than 10%. |
Definitely yes
|
Definitely no
Reason: Only the value of the PEF was evaluated as an indicator of the respiratory muscle strength, the impact of PR appears to influence only minor lung infiltrates, because there was no mortality and a few major complications. |
Some concerns |
Table of excluded studies
|
Reference |
Reason for exclusion |
|
An KR, Seijas V, Xu MS, Grüßer L, Humar S, Moreno AA, Turk M, Kasanagottu K, Alzghari T, Dimagli A, Ko MA, Villena-Vargas J, Papatheodorou S, Gaudino MFL. Does prehabilitation before esophagectomy improve postoperative outcomes? A systematic review and meta-analysis. Dis Esophagus. 2024 Feb 29;37(3):doad066. doi: 10.1093/dote/doad066. PMID: 38018252. |
More relevant systematic review available |
|
Assouline B, Cools E, Schorer R, Kayser B, Elia N, Licker M. Preoperative Exercise Training to Prevent Postoperative Pulmonary Complications in Adults Undergoing Major Surgery. A Systematic Review and Meta-analysis with Trial Sequential Analysis. Ann Am Thorac Soc. 2021 Apr;18(4):678-688. doi: 10.1513/AnnalsATS.202002-183OC. PMID: 33030962. |
More relevant systematic review available |
|
Auclair A, Harvey J, Leclerc J, Piché ME, O'Connor K, Nadreau É, Pettigrew M, Haykowsky MJ, Marceau S, Biertho L, Hould FS, Lebel S, Biron S, Julien F, Bouvet L, Lescelleur O, Poirier P. Determinants of Cardiorespiratory Fitness After Bariatric Surgery: Insights From a Randomised Controlled Trial of a Supervised Training Program. Can J Cardiol. 2021 Feb;37(2):251-259. doi: 10.1016/j.cjca.2020.03.032. Epub 2020 Mar 30. PMID: 32738206. |
Wrong outcome (No PPCs) |
|
Bilyy A, El-Nakhal T, Kadlec J, Bartosik W, Tornout FV, Kouritas V. Preoperative training education with incentive spirometry may reduce postoperative pulmonary complications. Asian Cardiovasc Thorac Ann. 2020 Nov;28(9):592-597. doi: 10.1177/0218492320957158. Epub 2020 Sep 11. PMID: 32915659. |
Wrong study design (cohort) |
|
Boden I, Denehy L. Respiratory prehabilitation for the prevention of postoperative pulmonary complications after major surgery. Curr Anesthesiol Rep. 2022;1-15. |
More relevant systematic review available |
|
Boden I, Reeve J, Jernås A, Denehy L, Fagevik Olsén M. Preoperative physiotherapy prevents postoperative pulmonary complications after major abdominal surgery: a meta-analysis of individual patient data. J Physiother. 2024 Jul;70(3):216-223. doi: 10.1016/j.jphys.2024.02.012. Epub 2024 Mar 11. PMID: 38472053. |
Wrong study design/more relevant systematic review available |
|
Boden I, Reeve J, Robertson IK, Browning L, Skinner EH, Anderson L, Hill C, Story D, Denehy L. Effects of preoperative physiotherapy on signs and symptoms of pulmonary collapse and infection after major abdominal surgery: secondary analysis of the LIPPSMAck-POP multicentre randomised controlled trial. Perioper Med (Lond). 2021 Oct 25;10(1):36. doi: 10.1186/s13741-021-00206-3. PMID: 34689825; PMCID: PMC8543902. |
Secondary analysis of other article, no relevant outcomes |
|
Boden I, Robertson IK, Neil A, Reeve J, Palmer AJ, Skinner EH, Browning L, Anderson L, Hill C, Story D, Denehy L. Preoperative physiotherapy is cost-effective for preventing pulmonary complications after major abdominal surgery: a health economic analysis of a multicentre randomised trial. J Physiother. 2020 Jul;66(3):180-187. doi: 10.1016/j.jphys.2020.06.005. Epub 2020 Jul 14. PMID: 32680742. |
Wrong outcome (cost-effectiveness instead of PPCs) |
|
Boden I, Sullivan K, Hackett C, Winzer B, Hwang R, Story D, Denehy L. Intensive physical therapy after emergency laparotomy: Pilot phase of the Incidence of Complications following Emergency Abdominal surgery Get Exercising randomized controlled trial. J Trauma Acute Care Surg. 2022 Jun 1;92(6):1020-1030. doi: 10.1097/TA.0000000000003542. Epub 2022 Jan 18. PMID: 35609291. |
Wrong population/type of surgery (only emergency surgery) |
|
Chang PC, Chen PH, Chang TH, Chen KH, Jhou HJ, Chou SH, Chang TW. Incentive spirometry is an effective strategy to improve the quality of postoperative care in patients. Asian J Surg. 2023 Sep;46(9):3397-3404. doi: 10.1016/j.asjsur.2022.11.030. Epub 2022 Nov 24. PMID: 36437210. |
Wrong type of surgery (thoracic) |
|
DeSai AR, Hathila VP. Effectiveness of respiratory and abdominal strength exercises in postoperative patients with abdominal surgeries: a narrative review. J Clin Diagn Res. 2022;16(4). |
Wrong study design (narrative review, no systematic search and analysis) |
|
Dhillon G, Buddhavarapu VS, Grewal H, Munjal R, Verma RK, Surani S, Kashyap R. Evidence-based Practice Interventions for Reducing Postoperative Pulmonary Complications: A Narrative Review. Open Respir Med J. 2023 Dec 4;17:e18743064271499. doi: 10.2174/012210299X247199231128100613. PMID: 38655075; PMCID: PMC11037507. |
Wrong study design (narrative review, no systematic search and analysis) |
|
do Nascimento Junior P, Módolo NS, Andrade S, Guimarães MM, Braz LG, El Dib R. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev. 2014 Feb 8;2014(2):CD006058. doi: 10.1002/14651858.CD006058.pub3. PMID: 24510642; PMCID: PMC6769174. |
More recent systematic review available |
|
Freitas ER, Soares BG, Cardoso JR, Atallah ÁN. Incentive spirometry for preventing pulmonary complications after coronary artery bypass graft. Cochrane Database Syst Rev. 2012 Sep 12;2012(9):CD004466. doi: 10.1002/14651858.CD004466.pub3. PMID: 22972072; PMCID: PMC8094624. |
Wrong type of surery (CABG) |
|
Fuchita M, Ridgeway KJ, Kimzey C, Melanson EL, Fernandez-Bustamante A. Accelerometer-Measured Inpatient Physical Activity and Associated Outcomes After Major Abdominal Surgery: Systematic Review. Interact J Med Res. 2023 May 15;12:e46629. doi: 10.2196/46629. PMID: 37184924; PMCID: PMC10227699. |
Wrong type of intervention |
|
Janssen THJB, Fransen LFC, Heesakkers FFBM, Dolmans-Zwartjes ACP, Moorthy K, Nieuwenhuijzen GAP, Luyer MDP. Effect of a multimodal prehabilitation program on postoperative recovery and morbidity in patients undergoing a totally minimally invasive esophagectomy. Dis Esophagus. 2022 Jul 12;35(7):doab082. doi: 10.1093/dote/doab082. PMID: 34875680. |
Wrong study design (retrospective cohort) |
|
Kızmaz E, Gürsoy S, Atalay OT, Sungurtekin U. Expiratory muscle training versus incentive spirometry after colorectal surgery. Ann Clin Anal Med. 2023. |
Wrong comparison (2 interventions no control group/usual care) |
|
Kotta PA, Ali JM. Incentive Spirometry for Prevention of Postoperative Pulmonary Complications After Thoracic Surgery. Respir Care. 2021 Feb;66(2):327-333. doi: 10.4187/respcare.07972. Epub 2020 Aug 25. PMID: 32843511. |
Wrong study design (narrative review, no systematic search and analysis) |
|
Kumar S, Gupta S, Upreti L, Parik RM. A prospective study to evaluate the effect of deep breathing exercises and incentive spirometry on pulmonary functions in patients before and after laparoscopic cholecystectomy. Int J Pharm Clin Res. 2022;14(7):409-413. |
Wrong outcome (no PPCs) |
|
Kumar S, Parshad S, Bijyal S, Mittal G, Sikka G. A Comparison of Two Methods of Pre-operative Inspiratory Muscle Training on Post-operative Outcome Following Esophagectomy. Indian J Surg Oncol. 2023 Dec;14(4):956-962. doi: 10.1007/s13193-023-01812-x. Epub 2023 Sep 25. PMID: 38187852; PMCID: PMC10766938. |
Wrong comparison (2 intervention groups, no control/usual care) |
|
Kunadharaju R, Saradna A, Ray A, Yu H, Ji W, Zafron M, Mador MJ. Post-Operative Outcomes of Pre-Thoracic Surgery Respiratory Muscle Training vs Aerobic Exercise Training: A Systematic Review and Network Meta-analysis. Arch Phys Med Rehabil. 2023 May;104(5):790-798. doi: 10.1016/j.apmr.2022.10.015. Epub 2022 Dec 17. PMID: 36539175. |
More relevant systematic review available |
|
Labuschagne R, Roos R. Pre-operative physiotherapy for elderly patients undergoing abdominal surgery. S Afr J Physiother. 2022 Sep 27;78(1):1782. doi: 10.4102/sajp.v78i1.1782. Erratum in: S Afr J Physiother. 2023 Jun 23;79(1):1870. doi: 10.4102/sajp.v79i1.1870. PMID: 36262215; PMCID: PMC9575366. |
Less than 10 patients per arm |
|
López-Rodríguez-Arias F, Sánchez-Guillén L, Aranaz-Ostáriz V, Triguero-Cánovas D, Lario-Pérez S, Barber-Valles X, Lacueva FJ, Ramirez JM, Arroyo A. Effect of home-based prehabilitation in an enhanced recovery after surgery program for patients undergoing colorectal cancer surgery during the COVID-19 pandemic. Support Care Cancer. 2021 Dec;29(12):7785-7791. doi: 10.1007/s00520-021-06343-1. Epub 2021 Jun 24. PMID: 34169328; PMCID: PMC8225311. |
Wrong intervention (multimodal programme) |
|
Maity B, Choudhury A, Banerjee C. The efficacy of incentive spirometry in restoring baseline lung capacity after upper abdominal and midline laparotomy: a randomised case control study. Int J Acad Med Pharm. 2023;5(3):1961-1966. |
Wrong comparison (2 intervention groups, no comparison with control group/usual care) |
|
Mikami Y, Kouda K, Kawasaki S, Okada KI, Kawai M, Kitahata Y, Miyazawa M, Hirono S, Unno M, Tajima F, Yamaue H. Preoperative In-Hospital Rehabilitation Improves Physical Function in Patients with Pancreatic Cancer Scheduled for Surgery. Tohoku J Exp Med. 2020 Aug;251(4):279-285. doi: 10.1620/tjem.251.279. PMID: 32759553. |
Wrong study design (single arm) |
|
Mohamed B, Wang MC, Bisson EF, Dimar J, Harrop JS, Hoh DJ, Mummaneni PV, Dhall S. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines for Perioperative Spine: Preoperative Pulmonary Evaluation and Optimization. Neurosurgery. 2021 Oct 13;89(Suppl 1):S33-S41. doi: 10.1093/neuros/nyab319. PMID: 34490879. |
Wrong study aim/outcome (identification of risk facors) |
|
Molenaar CJL, Minnella EM, Coca-Martinez M, Ten Cate DWG, Regis M, Awasthi R, Martínez-Palli G, López-Baamonde M, Sebio-Garcia R, Feo CV, van Rooijen SJ, Schreinemakers JMJ, Bojesen RD, Gögenur I, van den Heuvel ER, Carli F, Slooter GD; PREHAB Study Group. Effect of Multimodal Prehabilitation on Reducing Postoperative Complications and Enhancing Functional Capacity Following Colorectal Cancer Surgery: The PREHAB Randomized Clinical Trial. JAMA Surg. 2023 Jun 1;158(6):572-581. doi: 10.1001/jamasurg.2023.0198. Erratum in: JAMA Surg. 2023 Jun 1;158(6):675. doi: 10.1001/jamasurg.2023.1553. PMID: 36988937; PMCID: PMC10061316. |
Wrong intervention (multimodal programme) |
|
Nirali M, Srivastava S. Added effect of deep breathing and diaphragmatic breathing exercise in upper abdominal surgery patients: a randomised clinical trial. Indian J Public Health Res Dev. 2020;11(2). |
Wrong comparison (2 intervention groups, no comparison with control group/usual care), wrong outcome (no PPCs) |
|
Overbeek MC, Reijneveld EA, Valkenet K, van Adrichem EJ, Dronkers JJ, Ruurda JP, Veenhof C. The Association Between Preoperative Inspiratory Muscle Training Variables and Postoperative Pulmonary Complications in Subjects With Esophageal Cancer. Respir Care. 2024 Feb 28;69(3):290-297. doi: 10.4187/respcare.11199. PMID: 37935528; PMCID: PMC10984600. |
Wrong study design (cohort) |
|
Pazzianotto-Forti EM, da Costa Munno CM, Merino DFB, Simões da Rocha MR, de Mori TA, Júnior IR. Effects of Inspiratory Exercise With Linear and Nonlinear Load on Respiratory Variables Post-Bariatric Surgery. Respir Care. 2019 Dec;64(12):1516-1522. doi: 10.4187/respcare.05841. Epub 2019 Aug 6. PMID: 31387894. |
Wrong study design (cohort) |
|
Perry R, Herbert G, Atkinson C, England C, Northstone K, Baos S, Brush T, Chong A, Ness A, Harris J, Haase A, Shah S, Pufulete M. Pre-admission interventions (prehabilitation) to improve outcome after major elective surgery: a systematic review and meta-analysis. BMJ Open. 2021 Sep 30;11(9):e050806. doi: 10.1136/bmjopen-2021-050806. PMID: 34593498; PMCID: PMC8487197. |
More relevant systematic review available |
|
Piraux E, Reychler G, de Noordhout LM, Forget P, Deswysen Y, Caty G. What are the impact and the optimal design of a physical prehabilitation program in patients with esophagogastric cancer awaiting surgery? A systematic review. BMC Sports Sci Med Rehabil. 2021 Mar 25;13(1):33. doi: 10.1186/s13102-021-00260-w. PMID: 33766107; PMCID: PMC7993458. |
More relevant systematic review available |
|
Ramkumar PP, Kalaiyarasan K, Sridhar R, Sendhil R. Postoperative pulmonary complications in chronic obstructive pulmonary disease patients undergoing abdominal surgery in a tertiary care institute. Int J Acad Med Pharm. 2023;5(4):633-639. |
Wrong study design (cohort) |
|
Sadiq H, Rampam S, Patel J, Crawford S, Walz M, Kapoor A. Preoperative walking intervention did not appear to improve patient-reported postoperative recovery in older adults with frailty traits: Randomized trial. Medicine (Baltimore). 2022 Sep 23;101(38):e30689. doi: 10.1097/MD.0000000000030689. PMID: 36197179; PMCID: PMC9509049. |
Wrong outcome (no PPCs) |
|
Singh V, Agumbe Pai S, Hosmath V. Clinical outcome of patients undergoing preoperative chest physiotherapy in elective upper abdominal surgeries. J Perioper Pract. 2023 Jun;33(6):182-189. doi: 10.1177/17504589211045225. Epub 2022 May 5. PMID: 35510720. |
Wrong population (patients with respiratory system disorder excluded) |
|
Smith NA, Martin G, Marginson B. Preoperative assessment and prehabilitation in patients with obesity undergoing non-bariatric surgery: A systematic review. J Clin Anesth. 2022 Jun;78:110676. doi: 10.1016/j.jclinane.2022.110676. Epub 2022 Feb 10. PMID: 35152081. |
More relevant systematic review available |
|
Swaminathan N, Kundra P, Ravi R, Kate V. ERAS protocol with respiratory prehabilitation versus conventional perioperative protocol in elective gastrectomy- a randomized controlled trial. Int J Surg. 2020 Sep;81:149-157. doi: 10.1016/j.ijsu.2020.07.027. Epub 2020 Jul 30. PMID: 32739548. |
Wrong intervention (ERAS protocol) |
|
Sweity EM, Alkaissi AA, Othman W, Salahat A. Preoperative incentive spirometry for preventing postoperative pulmonary complications in patients undergoing coronary artery bypass graft surgery: a prospective, randomized controlled trial. J Cardiothorac Surg. 2021 Aug 24;16(1):241. doi: 10.1186/s13019-021-01628-2. PMID: 34429138; PMCID: PMC8383237. |
Wrong type of surgery (CABG) |
|
Taha MM, Draz RS, Gamal MM, Ibrahim ZM. Adding autogenic drainage to chest physiotherapy after upper abdominal surgery: effect on blood gases and pulmonary complications prevention. Randomized controlled trial. Sao Paulo Med J. 2021 Nov 15;139(6):556-563. doi: 10.1590/1516-3180.2021.0048.0904221. PMID: 34787294; PMCID: PMC9634842. |
Wrong intervention/comparison: autogenic drainage |
|
Tegegne BA, Lema GF, Fentie DY, Bizuneh YB. Perioperative risk stratification and strategies for reducing postoperative pulmonary complications following major surgery in resource-limited areas: a systematic review. Int J Surg Open. 2021;30:100322. |
More relevant systematic review available |
|
Triguero-Cánovas D, López-Rodríguez-Arias F, Gómez-Martínez M, Sánchez-Guillén L, Peris-Castelló F, Alcaide-Quirós MJ, Morillas-Blasco P, Arroyo A, Ramírez JM. Home-based prehabilitation improves physical conditions measured by ergospirometry and 6MWT in colorectal cancer patients: a randomized controlled pilot study. Support Care Cancer. 2023 Nov 6;31(12):673. doi: 10.1007/s00520-023-08140-4. PMID: 37930478. |
Wrong outcome (no PPCs) |
|
Tukanova KH, Chidambaram S, Guidozzi N, Hanna GB, McGregor AH, Markar SR. Physiotherapy Regimens in Esophagectomy and Gastrectomy: a Systematic Review and Meta-Analysis. Ann Surg Oncol. 2022 May;29(5):3148-3167. doi: 10.1245/s10434-021-11122-7. Epub 2021 Dec 27. PMID: 34961901; PMCID: PMC8990957. |
More relevant systematic review available |
|
van Gestel T, Groen LCB, Puik JR, van Rooijen SJ, van der Zaag-Loonen HJ, Schoonmade LJ, Danjoux G, Daams F, Schreurs WH, Bruns ERJ. Fit4Surgery for cancer patients during covid-19 lockdown - A systematic review and meta-analysis. Eur J Surg Oncol. 2022 Jun;48(6):1189-1197. doi: 10.1016/j.ejso.2022.02.010. Epub 2022 Feb 9. PMID: 35183411; PMCID: PMC8828288. |
More relevant systematic review available |
|
Vetrugno L, Deana C, Colaianni-Alfonso N, Tritapepe F, Fierro C, Maggiore SM. Noninvasive respiratory support in the perioperative setting: a narrative review. Front Med (Lausanne). 2024 Apr 17;11:1364475. doi: 10.3389/fmed.2024.1364475. PMID: 38695030; PMCID: PMC11061466. |
Wrong study design (narrative review, no systematic search and analysis) |
|
Waterland JL, McCourt O, Edbrooke L, Granger CL, Ismail H, Riedel B, Denehy L. Efficacy of Prehabilitation Including Exercise on Postoperative Outcomes Following Abdominal Cancer Surgery: A Systematic Review and Meta-Analysis. Front Surg. 2021 Mar 19;8:628848. doi: 10.3389/fsurg.2021.628848. PMID: 33816546; PMCID: PMC8017317. |
More relevant systematic review available |
|
Willner A, Teske C, Hackert T, Welsch T. Effects of early postoperative mobilization following gastrointestinal surgery: systematic review and meta-analysis. BJS Open. 2023 Sep 5;7(5):zrad102. doi: 10.1093/bjsopen/zrad102. PMID: 37846641; PMCID: PMC10580147. |
Wrong intervention (mobilization) |
|
Worraphan S, Thammata A, Chittawatanarat K, Saokaew S, Kengkla K, Prasannarong M. Effects of Inspiratory Muscle Training and Early Mobilization on Weaning of Mechanical Ventilation: A Systematic Review and Network Meta-analysis. Arch Phys Med Rehabil. 2020 Nov;101(11):2002-2014. doi: 10.1016/j.apmr.2020.07.004. Epub 2020 Aug 1. PMID: 32750371. |
Wrong population (ICU patients who are weaning of mechanical ventilation instead of surgical patients) |
|
Zhao CH, Sun YH, Mao XM. Volume Incentive Spirometry Reduces Pulmonary Complications in Patients After Open Abdominal Surgery: A Randomized Clinical Trial. Int J Gen Med. 2023 Mar 1;16:793-801. doi: 10.2147/IJGM.S400030. PMID: 36883125; PMCID: PMC9985979. |
Wrong outcome (no PPCs) |
|
Zhao B, Zhang T, Chen Y, Zhang C. Effects of unimodal or multimodal prehabilitation on patients undergoing surgery for esophagogastric cancer: a systematic review and meta-analysis. Support Care Cancer. 2023 Dec 7;32(1):15. doi: 10.1007/s00520-023-08229-w. PMID: 38060053. |
More relevant systematic review available |
|
Zhong J, Zhang S, Li C, Hu Y, Wei W, Liu L, Wang M, Hong Z, Long H, Rong T, Yang H, Su X. Active cycle of breathing technique may reduce pulmonary complications after esophagectomy: A randomized clinical trial. Thorac Cancer. 2022 Jan;13(1):76-83. doi: 10.1111/1759-7714.14227. Epub 2021 Nov 12. PMID: 34773384; PMCID: PMC8720618. |
Wrong comparison (control group also receives an intervention) |
|
Zhou W, Woo S, Larson JL. Effects of perioperative exercise interventions on lung cancer patients: An overview of systematic reviews. J Clin Nurs. 2020 Dec;29(23-24):4482-4504. doi: 10.1111/jocn.15511. Epub 2020 Oct 19. PMID: 32979874. |
Wrong population (lung cancer patients) |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 29-09-2025
Beoordeeld op geldigheid : 09-07-2025
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Stichting Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2022 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met een hoog risico op pulmonale complicaties die een niet-pulmonale ingreep ondergaan.
Werkgroep
Drs. R.P. (Peter) Meijer (voorzitter), anesthesioloog, NVA
Dr. J.P. (Jop) van den Berg, anesthesioloog, NVA
Dr. S.N.T. (Sabrine) Hemmes, anesthesioloog, NVA
Dr. M. (Marije) Marsman, anesthesioloog, NVA
Drs. M.W. (Mart) Groot, anesthesioloog-intensivist, NVIC
Drs. M. (Marjolein) van Laren, longarts, NVALT
Klankbordgroep
Dr. M. (Martijn) Boon, anesthesioloog, NVA
Drs. J.L.A (Jurriën) Embrechts, KNO-arts, NVKNO
Dr. H.J. (Erik) Hulzebos, klinisch inspanningsfysioloog en (sport)fysiotherapeut, KNGF
Drs. Y.J. (Yvonne) Kappe, senior beleidsadviseur/ patiëntvertegenwoordiger, Longfonds
Met ondersteuning van
Drs. F. (Femke) Janssen, junior adviseur, Kennisinstituut van de Federatie Medisch Specialisten, t/m mei 2023
Drs. A.E. (Amber) van der Meij, adviseur, Kennisinstituut van de Federatie Medisch Specialisten, vanaf maart 2023
Dr. M.S. (Matthijs) Ruiter, senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Romke Peter Meijer (voorzitter) |
Anesthesioloog, Amsterdam UMC adjunct medisch directeur, Amsterdam UMC tot 1-5-2019
|
Geen |
Geen |
Geen |
|
Johannes Pieter (Jop) van den Berg |
Anesthesioloog in het UMC Groningen, 0,9FTE, betaald. |
Medisch Manager Evenementenzorg, Rode Kruis, vrijwillig (inmiddels afgerond) Lid Medische Raad, Nederlandse Reanimatieraad, vrijwillig |
Uitsluitend de afdeling anesthesiologie ontving (soms) funding voor lopend onderzoek. Er zijn geen individuele financiële conflicten van belangen te vermelden. |
Geen |
|
Marjolein van Laren |
Longarts Dijklander Ziekenhuis Hoorn en Purmerend |
Geen |
Geen |
Geen |
|
Marije Marsman |
Anesthesioloog UMC Utrecht |
Geen |
Artikel gepubliceerd bij NTVG dat gaat over mate van implementatie van deze richtlijn in het UMC Utrecht. |
Geen |
|
Mart Wouter Groot |
Anesthesioloog-intensivist, Erasmus MC |
Geen |
Geen |
Geen |
|
Sabrine Nienke Tallechina Hemmes |
Anesthesioloog, Het Nederlands Kanker Instituut – Antoni van Leeuwenhoek Ziekenhuis, Afdeling Anesthesiologie. |
Geen |
Publicaties over postoperative pulmonale complicaties. Enkele gepubliceerde onderzoeken werden deels gefinancieerd door onderzoek-specifieke beurzen van de ESAIC. |
Geen |
|
Amber van der Meij |
Adviseur, Kennisinstituut van de Federatie Medisch Specialisten |
Geen |
Geen |
Geen |
|
Matthijs Ruiter |
Senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten |
Geen |
Geen |
Geen |
|
Klankbord-groeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Erik Hulzebos
|
Medisch Fysioloog en (sport)fysiotherapeut, UMC Utrecht |
Secretaris VHVL |
Extern gefinancierd onderzoek: Prinses Beatrix Spierfonds |
Geen |
|
Jurriën Embrechts |
Rhinologist / anterior skull base surgeon, Christchurch city hospital, (New Zealand).
|
Data scientist, Expertisecentrum Zorgalgoritmen |
Geen |
Geen |
|
Martijn Boon |
Anesthesioloog Leids Universitair Medisch Centrum |
Geen |
Extern gefinancierd onderzoek: 2. MSD: Invloed van diepe neuromusculaire blokkade op de incidentie van intraoperatieve adverse events, projectleider Ja |
Geen |
|
Yvonne Kappe (Longfonds) |
Senior Beleidsadviseur Longfonds |
Beleidsadviseur astmaVereniging Nederland en Davos |
Geen |
Geen |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door het uitnodigen van de Patiëntenfederatie Nederland en Longfonds voor de knelpunteninventarisatie en deelname van Longfonds aan de klankbordgroep. De binnengekomen reacties tijdens op de knelpunteninventarisatie zijn besproken in de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voorgelegd aan Longfonds en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijnmodule is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd om te beoordelen of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling is de richtlijnmodule op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
|
Module |
Uitkomst kwalitatieve raming |
Toelichting |
|
Longfysiotherapie |
Geen substantiële financiële gevolgen |
De aanbevelingen zijn breed toepasbaar, maar de verwachting is dat de beperkte kosten voor toepassing opwegen tegen de kostenbesparing door reductie van de ziektelast. Er worden daarom geen substantiële financiële gevolgen verwacht. |
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase beoordeelde de werkgroep de aanbevelingen uit de eerdere richtlijn Perioperatieve pulmonale complicaties (NVA, 2012) op noodzaak tot revisie. Daarnaast inventariseerde de werkgroep de knelpunten in de zorg voor patiënten met een hoog risico op pulmonale complicaties die een niet-pulmonale ingreep ondergaan. Tevens zijn er knelpunten aangedragen door de NVA, NVKNO en NVKG via een schriftelijke knelpunteninventarisatie. Een overzicht hiervan is opgenomen onder aanverwante producten.
Op basis van de uitkomsten van de knelpunteninventarisatie zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. Review Manager 5.4 werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwaliteit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
Algemene informatie
|
Database(s): Embase.com, Ovid/Medline |
Datum: 11 juli 2023 |
|
Periode: vanaf juni 2020 (search PMID:34593498) |
Talen: geen restrictie |
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SR |
92 |
49 |
102 |
|
RCT |
190 |
58 |
208 |
|
Totaal |
282 |
107 |
310* |
*in Rayyan
Zoekstrategie
Embase.com
|
No. |
Query |
Results |
|
#12 |
#10 OR #11 |
282 |
|
#11 |
#7 AND #9 NOT #10 = RCT |
190 |
|
#10 |
#7 AND #8 = SR |
92 |
|
#9 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
3827532 |
|
#8 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
942968 |
|
#7 |
#6 AND [01-06-2020]/sd |
715 |
|
#6 |
#5 NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) |
2609 |
|
#5 |
(#1 OR (#2 AND #3)) AND #4 |
3499 |
|
#4 |
('postoperative period'/exp OR 'postoperative care'/exp OR 'postoperative pain'/exp OR 'postoperative complication'/exp OR postoperative:ti,ab,kw OR 'post operative':ti,ab,kw OR postsurg*:ti,ab,kw OR 'post surg*':ti,ab,kw OR 'surgery induced':ti,ab,kw OR 'surgery related':ti,ab,kw OR 'surgery derived':ti,ab,kw OR 'surgery associated':ti,ab,kw) AND ('pulmonary complication'/exp OR (((pulmon* OR lung* OR respirat*) NEAR/2 complication*):ti,ab,kw) OR 'pneumonia'/exp OR pneumonia:ti,ab,kw OR (((lung OR pulmon*) NEAR/3 inflamm*):ti,ab,kw) OR 'hypoxemia'/exp OR hypoxia:ti,ab,kw OR 'hypoxaem*':ti,ab,kw OR 'hypoxem*':ti,ab,kw OR 'oxygen deficienc*':ti,ab,kw OR 'respiratory failure'/exp OR 'adult respiratory distress syndrome'/exp OR (((respirat* OR pulmon* OR lung*) NEAR/3 (failur* OR deficien* OR disturb* OR insufficien* OR dysfunction* OR distress OR shock)):ti,ab,kw) OR ards:ti,ab,kw OR 'reintubation'/exp OR reintubat*:ti,ab,kw OR 're intubat*':ti,ab,kw OR ((extubat* NEAR/3 failure):ti,ab,kw) OR 'artificial ventilation'/exp OR 'assisted ventilation'/exp OR (((artificial OR control* OR mechanical* OR assist* OR auxiliar* OR support*) NEAR/3 (respirat* OR ventilat*)):ti,ab,kw) OR ventilation:ti,ab,kw OR 'atelectasis'/exp OR 'atelectasis':ti,ab,kw OR (((lung OR pulmonar*) NEAR/3 (collaps* OR deflat*)):ti,ab,kw) OR 'pneumothorax'/exp OR 'pneumothorax':ti,ab,kw OR 'bronchospasm'/exp OR 'bronchiospasm*':ti,ab,kw OR 'bronchismus':ti,ab,kw OR 'bronchospasm*':ti,ab,kw OR 'bronchostriction*':ti,ab,kw OR ((bronch* NEAR/3 (constrict* OR spasm* OR syndrome* OR spastica)):ti,ab,kw)) |
143195 |
|
#3 |
'physiotherapy'/exp/mj OR 'physical therap*':ti,ab,kw OR 'physio therap*':ti,ab,kw OR 'physiotherap*':ti,ab,kw OR 'kinesiotherapy'/exp/mj OR 'kinesiotherap*':ti,ab,kw OR 'kinesitherap*':ti,ab,kw OR 'physical activity'/exp/mj OR 'exercise'/exp/mj OR 'physical activit*':ti,ab,kw OR (((exercis* OR 'physical fitness') NEAR/3 (therap* OR treatment* OR program*)):ti,ab,kw) OR (((muscle OR endurance OR aerobic* OR respirat* OR resistance OR weight OR strength) NEAR/2 training):ti,ab,kw) OR 'spirometry'/exp OR 'incentive spirometry'/exp OR 'incentive spirometr*':ti,ab,kw OR triflow:ti,ab,kw OR triflo:ti,ab,kw |
666137 |
|
#2 |
'perioperative period'/de OR 'perioperative care'/de OR 'preoperative care'/de OR 'preoperative period'/de OR 'preoperative education'/exp OR 'preoperative evaluation'/exp OR preoperati*:ti,ab,kw OR 'pre operati*':ti,ab,kw OR presurg*:ti,ab,kw OR 'pre surg*':ti,ab,kw OR perioperati*:ti,ab,kw OR 'peri operati*':ti,ab,kw OR preconditioning:ti,ab,kw OR 'pre conditioning':ti,ab,kw |
839051 |
|
#1 |
'preoperative exercise'/exp OR (((preoperati* OR 'pre operati*' OR presurg* OR 'pre surg*' OR perisurg* OR 'peri surg*' OR perioperati* OR 'peri operati*') NEAR/3 (training OR 'muscle training' OR exercis* OR rehabilit* OR condition* OR therap* OR intervention OR optimis* OR optimiz*)):ti,ab,kw) OR prehabilitat*:ti,ab,kw OR prerehabilitat*:ti,ab,kw OR 'pre habilitat*':ti,ab,kw OR (((preadmission OR 'pre admission') NEAR/3 (intervention* OR training OR exercis* OR rehabilit*)):ti,ab,kw) |
29768 |
Ovid/Medline
|
# |
Searches |
Results |
|
12 |
10 or 11 |
107 |
|
11 |
(7 and 9) not 10 = RCT |
58 |
|
10 |
7 and 8 = SR |
49 |
|
9 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2609251 |
|
8 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
679922 |
|
7 |
6 and 20200601:20230711.(dt). |
315 |
|
6 |
5 not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
1794 |
|
5 |
(1 or (2 and 3)) and 4 |
1844 |
|
4 |
(exp Postoperative Period/ or exp Postoperative Care/ or exp Pain, Postoperative/ or exp Postoperative Complications/ or postoperative.ti,ab,kf. or 'post operative'.ti,ab,kf. or postsurg*.ti,ab,kf. or 'post surg*'.ti,ab,kf. or 'surgery induced'.ti,ab,kf. or 'surgery related'.ti,ab,kf. or 'surgery derived'.ti,ab,kf. or 'surgery associated'.ti,ab,kf.) and (((pulmon* or lung* or respirat*) adj2 complication*).ti,ab,kf. or exp Pneumonia/ or pneumonia.ti,ab,kf. or ((lung or pulmon*) adj3 inflamm*).ti,ab,kf. or exp Hypoxia/ or hypoxia.ti,ab,kf. or 'hypoxaem*'.ti,ab,kf. or 'hypoxem*'.ti,ab,kf. or 'oxygen deficienc*'.ti,ab,kf. or exp Respiratory Insufficiency/ or Respiratory Distress Syndrome/ or ((respirat* or pulmon* or lung*) adj3 (failur* or deficien* or disturb* or insufficien* or dysfunction* or distress or shock)).ti,ab,kf. or ards.ti,ab,kf. or reintubat*.ti,ab,kf. or 're intubat*'.ti,ab,kf. or (extubat* adj3 failure).ti,ab,kf. or exp Respiration, Artificial/ or ((artificial or control* or mechanical* or assist* or auxiliar* or support*) adj3 (respirat* or ventilat*)).ti,ab,kf. or ventilation.ti,ab,kf. or exp Pulmonary Atelectasis/ or 'atelectasis'.ti,ab,kf. or ((lung or pulmonar*) adj3 (collaps* or deflat*)).ti,ab,kf. or exp Pneumothorax/ or 'pneumothorax'.ti,ab,kf. or exp Bronchial Spasm/ or 'bronchiospasm*'.ti,ab,kf. or 'bronchismus'.ti,ab,kf. or 'bronchospasm*'.ti,ab,kf. or 'bronchostriction*'.ti,ab,kf. or (bronch* adj3 (constrict* or spasm* or syndrome* or spastica)).ti,ab,kf.) |
62679 |
|
3 |
exp Physical Therapy Modalities/ or 'physical therap*'.ti,ab,kf. or 'physio therap*'.ti,ab,kf. or 'physiotherap*'.ti,ab,kf. or 'kinesiotherap*'.ti,ab,kf. or 'kinesitherap*'.ti,ab,kf. or exp Exercise/ or 'physical activit*'.ti,ab,kf. or ((exercis* or 'physical fitness') adj3 (therap* or treatment* or program*)).ti,ab,kf. or ((muscle or endurance or aerobic* or respirat* or resistance or weight or strength) adj2 training).ti,ab,kf. or exp Spirometry/ or 'incentive spirometr*'.ti,ab,kf. or triflow.ti,ab,kf. or triflo.ti,ab,kf. |
559264 |
|
2 |
exp Perioperative Care/ or exp Perioperative Medicine/ or exp Perioperative Period/ or exp Preoperative Care/ or exp Preoperative Period/ or preoperati*.ti,ab,kf. or 'pre operati*'.ti,ab,kf. or presurg*.ti,ab,kf. or 'pre surg*'.ti,ab,kf. or perioperati*.ti,ab,kf. or 'peri operati*'.ti,ab,kf. or preconditioning.ti,ab,kf. or 'pre conditioning'.ti,ab,kf. |
688072 |
|
1 |
exp Preoperative Exercise/ or ((preoperati* or 'pre operati*' or presurg* or 'pre surg*' or perisurg* or 'peri surg*' or perioperati* or 'peri operati*') adj3 (training or 'muscle training' or exercis* or rehabilit* or condition* or therap* or optimis* or optimiz*)).ti,ab,kf. or prehabilitat*.ti,ab,kf. or prerehabilitat*.ti,ab,kf. or 'pre habilitat*'.ti,ab,kf. or ((preadmission or 'pre admission') adj3 (intervention* or training or exercis* or rehabilit*)).ti,ab,kf. |
18087 |