Optimale eerstelijns systeemtherapie niet-heldercellig niercelcarcinoom
Uitgangsvraag
Welke eerstelijns systeemtherapie heeft de voorkeur bij patiënten met gemetastaseerd niet-heldercellig niercelcarcinoom?
Aanbeveling
Bespreek palliatieve behandeling met sunitinib bij een patiënt met een gemetastaseerd niet-heldercellig niercelcarcinoom als patient in afdoende conditie is voor palliatieve systeemtherapie.
Maak bij patiënten met een gemetastaseerd papilliar niercelcarcinoom de afweging of er een meerwaarde is van cabozantinib boven sunitinib als er palliatieve systemische therapie gestart gaat worden.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Er werden één systematische review en 3 RCT's gevonden die rapporteerden over de uitkomstmaten van progressievrije overleving, overall survival, kwaliteit van leven en complicaties.
In de studies werden vier verschillende vergelijkingen (everolimus versus sunitinib; Temsirolimus vs sunitinib; Savolitinib vs sunitinib; Cabozantinib, crizotinib and savolitinib vs sunitinib) gerapporteerd met betrekking tot de uitkomstmaten. Het bewijsniveau met betrekking tot everolimus versus sunitinib was matig en voor de rest van de vergelijkingen laag.
Zelfs zonder verdere onderverdeling in verschillende histologische subtypes is de mate van bewijsvoering matig tot zelfs laag. Op basis van survival overwegingen (OS en/of PFS) lijkt sunitinib de voorkeur te hebben boven een mTOR remmer zoals naar voren komt in de systematic review van Osterman.
De studies van Pal en Choueri hebben beide gekeken naar patiënten met een tumor van het papillaire subtype, waarbij de laatste studie zich beperkt heeft tot de MET gedreven papillaire niercelcarcinomen.
Als er gekeken wordt naar de studie waarbij alleen papillaire histologie werd toegestaan dan lijkt cabozantinib superieur aan sunitib als het gaat om progressie vrije overleving. Een positief effect op OS heeft deze fase II studie niet kunnen aan tonen bij de analyse van 152 patienten.
Van de savolitinib studie van Choueiri is het wachten op een update van de gegevens. Op basis van de huidige gegevens is er geen plek voor savolitinib.
Onlangs zijn er twee fase 2-onderzoeken uitgevoerd naar Pembrolizumab in combinatie met Lenvatinib en Nivolumab in combinatie met Cabozantinib als eerstelijnsbehandeling voor gevorderd niet-heldercellig niercelcarcinoom (Albiges, 2023). Omdat dit onderzoek beschikbaar is gekomen na het verrichten van de literatuuur analyse laat het proces van opstellen van de richtlijn geen ruimte voor volledig opnemen van deze gegevens. Hoe de optie pembrolizumab + lenvatinib zich verhoudt tot monotherapie TKI zal onderwerp van discussie kunnen zijn in de Medische Inhoudelijke Standpuntgroep (MIS-groep) van de landelijke tumorwerkgroep (DRCG). De studie met Pembrolizumab en Lenvatinib (Keynote B61: Albiges, 2023) heeft aanvullend bewijs geleverd over de werkzaamheid en veiligheid van deze behandeling bij deze specifieke groep patiënten. Een aanzienlijk percentage van de patiënten (49%) vertoonde een bevestigde objectieve respons, waaronder complete en gedeeltelijke responsen. De combinatie van pembrolizumab en lenvatinib toonde antitumoractiviteit bij gevorderd niet-heldercellig niercelcarcinoom. Hoewel enkele bijwerkingen werden waargenomen, waren er geen nieuwe veiligheidssignalen. Ongeveer de helft van de patiënten (51%) ervoer graad 3-4 behandelingsgerelateerde bijwerkingen, zoals hypertensie, proteïnurie en stomatitis. Hoewel de activiteit en veiligheid van deze behandeling zijn aangetoond, zijn verdere langetermijnresultaten en onderzoek noodzakelijk om een volledig begrip te krijgen van de effectiviteit en veiligheid van deze combinatie. Daarnaast includeerde de cabozantinib- en nivolumabstudie 40 patiënten met papillaire en niet-geclassificeerde RCC met een responspercentage van 47% en een PFS van 13 (7-16) maanden (Lee, 2022). In deze studie werd chromofoob RCC uitgesloten en was het percentage papRCC 68%. Indirecte vergelijkingen suggereren dat deze gegevens vergelijkbaar zijn met een verhoogde werkzaamheid met die van VEGFR-TKI monotherapie (Lee, 2022).
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Gezien de beperkte opties, overwegen patiënten vooral of de aangetoonde meerwaarde ten opzichte van de bekende bijwerkingen van sunitinib voldoende is om deze therapie te ondergaan. In het geval van een gemetastaseerd papillair niercelcarcinoom zijn zowel sunitinib als cabozantinib mogelijkheden. Deze keuze moet samen met de patiënt worden afgewogen tegen de bijwerkingen van beide TKI's. Het bijwerkingenpatroon van beide TKI's komt overeen met de uitgebreidere gegevens die we kennen bij gemetastaseerd heldercellig niercelcarcinoom. Hoewel de effectiviteit van cabozantinib lijkt toe te nemen, zoals blijkt uit een betere PFS, lijkt ook de toxiciteit groter te zijn.
Kosten (middelenbeslag)
Voor de meeste histologische subtypes van het niet-heldercellige niereclcarcinoom is er dus één eerstelijns optie en dat is sunitinib.
Voor patienten met een gemetastaseerd papillair niercelcarcinoom moet (als er gekozen wordt voor therapie) de afweging gemaakt worden tussen sunitinib en cabozantinib. Sunitinib is inmiddels van patent af en heeft daarom een evidente andere impact op kosten dan cabozantinib. Daarbij lijkt het bijwerkingenpatroon van sunitinib gunstiger dan dat van cabozantinib. Dit zal mee genomen moeten worden in de afweging tegen signalen van hogere effectiviteit die zich (nog) niet vertaald hebben in een langere overleving.
Aanvaardbaarheid, haalbaarheid en implementatie
Sunitinib wordt momenteel als de standaard behandeling gezien. De waarde van cabozantinib bij het niet-heldercellig niercelcarcinoom is nog niet eerder opgenomen in de Nederlandse Richtlijn, maar is wel toepasbaar.
Zeer binnenkort worden data van meerdere studies verwacht mbt rol van immunotherapie. Een hoopvol signaal is gezien in de fase 2 studie met permbrolizumab in combinatie met lenvatinib.
Onderbouwing
Achtergrond
In de behandeling van patienten met een gemetastaseerd heldercellig niercelcarcinoom zijn het afgelopen decennium veel middelen ter beschikking gekomen (zie module Keuze eerstelijns systemische therapie heldercellig niercelcarcinoom). In het verleden werden therapie opties bij het niet-heldercellig niercelcarcinoom toegepast naar aanleiding van extrapolatie van gegevens bij het heldercellig niercelcarcinoom of zeer beperkte observaties.
Complex blijft dat niet-heldercellig niercelcarcinoom nog steeds een heterogene groep is, waarbij de patientenaantallen relatief laag zijn. Er is momenteel geen uniform
behandeladvies in de landelijke richtlijn.
Conclusies / Summary of Findings
mTOR inhibitor vs sunitinib
Everolimus versus sunitinib
|
Moderate GRADE |
Sunitinib probably results in an increase in progression-free survival rate when compared with everolimus in patient population with non clear cell RCC.
Source: Osterman, 2020 |
|
Moderate GRADE |
Sunitinib probably results in little to no difference in overall survival when compared with everolimus in patients with non clear cell RCC.
Source: Osterman, 2020 |
|
Moderate GRADE |
Everolimus probably results in little to no difference in quality of life when compared with sunitinib in patient population with non clear cell RCC.
Source: Osterman, 2020 |
|
Moderate GRADE |
Everolimus probably reduces complications slightly when compared with sunitinib in patient population with non clear cell RCC.
Source: Osterman, 2020 |
Temsirolimus vs sunitinib
|
Low GRADE |
The evidence suggests that temsirolimus results in little to no difference in progression-free survival rate when compared with sunitinib in patient population with non clear cell RCC.
Source: Bergmann, 2020 |
|
Low GRADE |
The evidence suggests that temsirolimus results in little to no difference in overall survival when compared with sunitinib in patient population with non clear cell RCC.
Source: Bergmann, 2020 |
|
No GRADE |
No evidence was found regarding the effect of temsirolimus on quality of life when compared with sunitinib in patient with non clear cell RCC. |
|
Low GRADE |
The evidence suggests that temsirolimus results in little to no difference in complications when compared with sunitinib in patient population with non clear cell RCC.
Source: Bergmann, 2020 |
MET inhibitor vs sunitinib
Savolitinib vs sunitinib
|
Low GRADE |
The evidence suggests that savolitinib results in little to no difference in progression-free survival rate when compared with sunitinib in patient population with non clear cell RCC.
Source: Choueiri, 2020 |
|
Low GRADE |
The evidence suggests that savolitinib results in little to no difference in overall survival when compared with sunitinib in patient population with non clear cell RCC.
Source: Choueiri, 2020 |
|
Low GRADE |
The evidence suggests that savolitinib results in little to no difference in quality of life when compared with sunitinib in patient population with non clear cell RCC.
Source: Choueiri, 2020 |
|
Low GRADE |
Savolitinib may reduce complications when compared with sunitinib in patient population with non clear cell RCC.
Source: Choueiri, 2020 |
Cabozantinib, crizotinib and savolitinib vs sunitinib
|
Low GRADE |
The evidence suggests Cabozantinib increases progression-free survival rate when compared with sunitinib in patient population with metastatic papillary renal cell carcinoma.
Source: Pal, 2021 |
|
Low GRADE |
The evidence suggests that Cabozantinib results in little to no difference in overall survival when compared with sunitinib in patient population with metastatic papillary renal cell carcinoma.
Source: Pal, 2021 |
|
No GRADE |
No evidence was found regarding the effect of cabozantinib, crizotinib and savolitinib on quality of life when compared with sunitinib in patient with non clear cell RCC. |
|
Low GRADE |
The evidence suggests that Cabozantinib, crizotinib and savolitinib results in little to no difference in complications when compared with sunitinib in patient population with metastatic papillary renal cell carcinoma.
Source: Pal, 2021 |
Samenvatting literatuur
Description of studies
Systematic Review by Osterman (2020) evaluated systemic treatment options in locally advanced or metastatic nccRCC between 2000-2019. Randomized controlled trials, single-arm phase II–IV trials, and prospective analyses of medication access programs were included. The primary outcome measures were progression free survival (PFS), overall survival (OS), and objective response rate (ORR).
Armstrong (2016) enrolled patients with metastatic papillary, chromophobe, or unclassified non-clear-cell renal cell carcinoma with no history of previous systemic treatment to compare the mTOR inhibitor everolimus and the VEGF receptor inhibitor sunitinib in patients with non-clear-cell renal cell carcinoma (ASPEN). Patients were randomly assigned (1:1) to receive everolimus (10 mg/day) or sunitinib (50 mg/day; 6-week cycles of 4 weeks with treatment followed by 2 weeks without treatment) administered orally until disease progression or unacceptable toxicity. Randomisation was stratified by Memorial Sloan Kettering Cancer Center risk group and papillary histology.
Tannir (2016) conducted a randomized phase 2 trial (ESPN) comparing sunitinib and everolimus in non–clear cell RCC (non-ccRCC). Patients with metastatic, non-ccRCC, or ccRCC with >20% sarcomatoid features (ccSRCC) were randomized to receive sunitinib or everolimus with crossover at disease progression. Primary end point was progression-free survival (PFS) in first-line therapy; 108 patients were needed to show improvement in median PFS (mPFS) from 12 wk with sunitinib to 20 wk with everolimus. Patients were stratified by Memorial Sloan Kettering Cancer Center risk group [19] and histologic RCC subtype (papillary vs other), and they were randomized 1:1 to receive either everolimus or sunitinib.
Motzer (2014) conducted a multicenter, randomized phase II trial (RECORD-3) to compare first-line everolimus followed by sunitinib at progression with the standard sequence of first-line sunitinib followed by everolimus in patients with metastatic renal cell carcinoma. RECORD-3 used a crossover treatment design. The primary objective was to assess progression-free survival (PFS) noninferiority of first-line everolimus compared with first-line sunitinib. Secondary end points included combined PFS for each sequence, overall survival (OS), and safety. The population comprised patients age 18 years or older who had measurable version clear cell or non–clear cell mRCC, with or without nephrectomy. Key eligibility criteria included no prior systemic therapy; a Karnofsky performance status of 70% or greater; adequate hematologic, liver, and kidney function; and normal left ventricular ejection fraction.
Bergmann (2020) performed a prospectively randomized phase IIa multicenter trial, investigating temsirolimus (TEM) versus sunitinib (SUN) as first-line therapy in patients with metastatic nccRCC. The patients were randomized 1:1 to either TEM in a dose of 25 mg i.v. once a week or SUN with 50 mg p.o. daily for 4 weeks on and 2 weeks off. Primary endpoint was progression-free survival (PFS). In total, 22 patients were included with predominantly papillary RCC (16/22) followed by chromophobe RCC and others. This trial had to be terminated due to low recruitment.
Choueiri (2020) conducted a phase 3, open-label, randomized clinical trial (SAVOIR) to investigate efficacy of savolitinib vs sunitinib in patients with MET-Driven papillary renal cell carcinoma. Overall, 360 to 450 patients were to be screened to randomize approximately 180 patients. Patients were adults with MET-driven (centrally confirmed), metastatic PRCC, with 1 or more measurable lesions. Overall, 254 patients were screened. Patients received 600mg of savolitinib orally once daily (qd), or 50mg of sunitinib orally qd for 4 weeks, followed by 2 weeks without treatment. The primary end point was progression-free survival (PFS). Secondary end points included overall survival (OS), objective response rate (ORR), duration of response, and safety/tolerability. Premature termination of the study and the limited number of patients randomized were key limitations of this study.
Pal (2021) conducted a randomized, open-label, phase II trial involving 147 patients with metastatic papillary renal cell carcinoma (PRCC) who had received up to one prior therapy (excluding vascular endothelial growth factor-directed agents). They aimed to compare the effectiveness and safety of an existing standard (sunitinib) to MET kinase inhibitors (cabozantinib, crizotinib, and savolitinib). The patients were randomly assigned to receive sunitinib (46 patients), cabozantinib (n=44), savolitinib (n=29) and crizotinib (n=28), with stratification by receipt of prior therapy and PRCC subtype, until their disease progressed or they had unacceptable side effects. Progression-free survival (PFS) was the primary endpoint. The trial was then temporarily stopped for savolitinib and crizotinib arms because of hazard ratio for PFS greater than 1 relative to sunitinib.
Results
nccRCC subtypes
Papillary
1) Progression-free survival (PFS) rate
In the Pal trial, the MET inhibitor cabozantinib demonstrated a median PFS of 9.0 months (95% CI: 5.6–12.4) compared to 5.6 months (95% CI: 2.9–6.7) for sunitinib. The hazard ratio (HR) for PFS favored cabozantinib over sunitinib significantly (HR: 0.60, 95% CI: 0.37–0.97). This is considered a clinically relevant difference. In addition to comparing cabozantinib and sunitinib, an additional 57 patients were inrolled to crizotinib and savolitinib arms. Both arms were closed due to hazard ratio for PFS greater than 1 at prespecified interim analysis. Savolitinib and crizotinib did not improve PFS relative to sunitinib.
Additionally, in the SAVOIR trial, the MET inhibitor savolitinib showed a median PFS of 7.0 months (95% CI: 2.8–not calculated) compared to 5.6 months (95% CI: 4.1–6.9) for sunitinib. This was not a statistically significance but a clinically relevant difference between the arms (HR 0.71, 95% CI 0.37–1.36, p = 0.31).
In the ESPN trial, the mTOR inhibitor everolimus exhibited a median PFS of 4.1 months (95% CI: 1.5–7.4) compared to 5.7 months (95% CI: 1.4–19.8) for sunitinib.
In the ASPEN trial, the MET inhibitor sunitinib showed a median PFS of 8.1 months (95% CI: 5.8–11.1), while the mTOR inhibitor everolimus exhibited a median PFS of 5.5 months (95% CI: 4.4–5.6).
2) Overall survival (OS) rate
In the Pal trial, the overall survival did not significantly differ among the treatment groups. The hazard ratio for the survival comparison between cabozantinib and sunitinib was 0.84 (95%CI, 0.47–1.51). The reported median overall survival was 16.4 months (95% CI, 12.8–21.6) for the sunitinib arm, 20.0 months (95% CI, 11.3-Not calculated) for the cabozantinib arm, 19.9 months (95% CI, 11.2-NR) for the crizotinib arm, and 11.7 months (95% CI, 6.7-28.9)for the savolitinib arm.
Similarly, in the SAVOIR trial, no significant difference was observed in overall survival between treatment arms. The hazard ratio for overall survival comparison between savolitinib and sunitinib was 0.51 (95% CI, 0.21–1.17), indicating no significant difference but a clinically relevant difference. The median overall survival was not reached for the savolitinib group and was 13.2 months (95% CI, 7.6-NC) for the sunitinib group.
In the ASPEN trial, no differences in overall survival were noted within subsets of patients according to treatment group assignment.
In the ESPN trial, the median overall survival was 14.9 months (95% CI,7.1-22.1) for the everolimus arm and 16.6 months (95% CI ,5.9-NA) for the sunitinib arm.
3) Quality of life
In the SAVOIR trial, the effect of treatment on health-related quality of life and disease-related symptoms, as assessed by FACIT-F and FKSI-19 scores, revealed no significant variances between treatment arms. Notably, compliance rates were higher in the savolitinib arm compared to the sunitinib arm for both FACIT-F (91% vs. 78%, respectively) and FKSI-19 (88% vs. 67%, respectively) questionnaires.
EQ-5D-5L scores indicated fewer patients in the savolitinib group reported severe issues with pain/discomfort and anxiety/depression compared to the sunitinib group. Specifically, there was a change of 1 in score from baseline for savolitinib (n = 6) versus -12 for sunitinib (n = 6). Additionally, compliance rates were higher in the savolitinib group compared to the sunitinib group (88% vs. 67%, respectively).
4) Complications
In both the Pal and SAVOIR trials, which investigated MET inhibitors, adverse events were notable among patients receiving these inhibitors compared to those receiving sunitinib.
In the Pal trial, grade 3 or 4 adverse events occurred in 69%, 74%, 37%, and 39% of patients receiving sunitinib, cabozantinib, crizotinib, and savolitinib, respectively. Additionally, one grade 5 thromboembolic event was observed with cabozantinib. Treatment discontinuation due to adverse events attributed to study medication was highest with sunitinib (24%), followed by cabozantinib (23%), crizotinib (16%), and savolitinib (10%).
Similarly, in the SAVOIR trial, adverse events were reported in a significant proportion of patients receiving MET inhibitors. Specifically, grade 3 or higher adverse events were observed in 42% and 81% of patients receiving savolitinib and sunitinib, respectively. Moreover, adverse events led to dose modifications in 30% and 74% of patients receiving savolitinib and sunitinib, respectively. Notably, adverse events of any cause occurred in 91% of patients in the savolitinib group and 100% of patients in the sunitinib group. Additionally, all deaths attributed to adverse events occurred in the sunitinib group.
Non-clear cell other than papillary
1) Progression-free survival rate
The ASPEN and ESPN trials provided insights into the progression-free survival (PFS) outcomes specifically for the subgroup of chromophobe patients. In contrast to the overall trial results, both trials demonstrated a longer median PFS duration in the everolimus group compared to the sunitinib group. In the ASPEN trial, the median PFS was 11.4 months for everolimus and 5.5 months for sunitinib among chromophobe patients. Similarly, in the ESPN trial, the median PFS was not reached for everolimus and 8.9 months for sunitinib, although these differences were non-significant.
Specifically, in the ASPEN trial, among chromophobe patients, patients in the sunitinib group had a median PFS of 5.5 months (80% CI, 3.3–19.7), while the median PFS for everolimus was 11.4 months (80% CI, 5.7–19.4). Moreover, among patients WITH unclassified histology in the ASPEN trial, 15 out of 22 patients in the sunitinib group had a median PFS of 11.5 months (95% CI, 5.3–not reached), while the median PFS for everolimus was 5.7 months (95% CI, 2.8–7.2).
In the ESPN trial, the overall median PFS for everolimus was 3.0 months (95% CI, 1.3–NA), and for sunitinib, it was 7.5 months (95% CI, 3.1–16.7).
2) Overall survival rate
In the ESPNtrial, the overall median overall survival for everolimus was 15.7 months (95% CI: 4.7–NA) and for sunitinib was 17.6 (95% CI: 9.6–NA).
3) Quality of life
The included literature did not report on this outcome measure.
4) Complications
The included literature did not report on this outcome measure.
Treatments of nccRCC
mTOR inhibitor vs sunitinib
Everolimus versus sunitinib
There were 3 RCTs comparing the mammalian target of rapamycin (mTOR) inhibitor everolimus to the vascular endothelial growth factor (VEGF) TKI sunitinib in first line treatment of metastatic nccRCC. The ASPEN and ESPN trials enrolled only nccRCC, and the RECORD-3 trial enrolled patients with any RCC histology but reported PFS results for nccRCC alone.
1) Progression-free survival rate
The median PFS was numerically longer with first line sunitinib compared to everolimus in all 3 trials, but was only statistically significant and clinically relavnt in the ASPEN (8.3 months vs. 5.6 months; HR 1.41 (80% CI 1.03–1.92)) and RECORD-3 (7.2 months vs. 5.1 months; HR 1.5 (95% CI 0.9–2.8)) trials.
2) Overall survival rate
Median overall survival was numerically greater in the sunitinib group compared to the everolimus group in both ASPEN (31.5 months vs. 13.2 months; HR 1.12 (95% CI 0.7–2.1)) and ESPN (16.2 months vs. 14.9 months; stratified log-rank p = 0.18), however this failed to reach statistical significance and clinical relevance in either trial. Response rates were reported in ASPEN and ESPN with higher ORR seen for the sunitinib group in both trials (18% vs. 9% and 9% vs. 3%, respectively).
3) Quality of life
In the longitudinal sensitivity analysis of RECORD-3, EORTC QLQ-C30 global health status/quality of life and fatigue scores, which were previously equivocal, demonstrated a significant benefit to everolimus. Also, results demonstrated that everolimus as firstline treatment in mRCC does not impair patient quality of life.
In ASPEN at baseline, the median FACT-KSI score was 47⋅5 (IQR 23–59) for patients in the everolimus group and 45 (27–56) in the sunitinib group. By the third cycle, the median KSI was 44 (IQR 37–50) for everolimus (change from baseline of −4⋅5, n=31) and 43 (36–49) for sunitinib (change from baseline −1⋅0, n=33). At progression or end of treatment, median FACT-KSI score was 44 (32–50) for everolimus (change from baseline −7⋅5) and 42 (31–48) for sunitinib (change from baseline −5⋅0). Between-group differences in quality-of-life measures, including disease-related subscales, were not significant nor clinically relevant.
4) Complications
Common treatment-emergent adverse events in RECORD-3 during first-line everolimus or sunitinib were stomatitis (53% and 57%, respectively), fatigue (45% and 51%, respectively), and diarrhea (38% and 57%, respectively).
In ASPEN overall, 40 (78%) patients receiving sunitinib had grade 3 or worse treatment-related adverse event compared with 34 (60%) patients receiving everolimus. Serious adverse events (grade 3–5) that were felt to be at least possibly related to study treatment per protocol were reported in 34 (60%) of everolimus-treated patients and 40 (78%) of sunitinib-treated patients.
In ESPN, any grade 3 or 4 AE occurred in 29 of 33 patients (88%) who received first-line sunitinib and in 19 of 35 patients (54%) who received first-line everolimus. Common grade 3 or 4 sunitinib-associated treatment-emergent AEs included fatigue (36%), hypertension (18%), diarrhea (21%), neutropenia (27%), and hyponatremia (15%). Grade 3 anemia occurred in 11% of patients who received everolimus.
Temsirolimus vs sunitinib
1) Progression-free survival rate
In the study by Bergmaan, temsirolimus was compared to sunitinib in 22 patients with advanced RCC. This trial did not achieve its prespecified endpoint, as the difference in median PFS between sunitinib and temsirolimus, 13.2 vs 9.3 months (HR 1.64; 95% CI 0.65–4.18 in favor of sunitinib), was not statistically significant but clinically relevant.
2) Overall survival rate
There was also no significant difference in median OS, 19.8 vs. 19.4 months.
3) Quality of life
The included literature did not report on this outcome measure.
4) Complications
Eleven of 12 patients had drug-related severe adverse events (SAE) in the Temsirolimus arm and all patients in the sunitinib arm.
MET inhibitor vs sunitinib
Savolitinib vs sunitinib
1) Progression-free survival rate
Choueiri (2020) In terms of PFS, there was not a statistically significance but a clinically relevant difference between the arms (HR 0.71, 95% CI 0.4–1.4, p = 0.31). Median PFS was 7.0 months (95% CI 2.8- not calculated) in the savolitinib arm and 5.6 months (95% CI 4.1–6.9) in the sunitinib arm.
2) Overall survival rate
There was also not a significant difference in terms of OS (HR 0.51, 95% CI 11.9-not calculated, p = 0.11). This is considered a clinically relevant difference.
3) Quality of life
The impact of treatment on health-related quality of life and disease-related symptoms based on the FACIT-F scores and FKSI-19 scores showed no notable differences between treatment groups. Compliance was higher in the savolitinib group compared with the sunitinib group for both the FACIT-F questionnaire (91% vs 78%, respectively) and the FKSI-19 questionnaire (88% vs 67%, respectively).
The EQ-5D-5L scores showed fewer patients reporting severe problems in pain/discomfort and anxiety/depression in the savolitinib group than in the sunitinib group: there was a change from baseline of 1 in score for savolitinib (n = 6) compared with -12 for sunitinib (n = 6). Furthermore, compliance was higher in the savolitinib group compared with sunitinib group (88% vs 67%, respectively).
4) Complications
For savolitinib and sunitinib respectively, grade 3 or higher adverse events (AEs) were reported in 14 (42%) and 22 (81%) of patients and AE-related dose modifications in 10 (30%) and 20 (74%). Adverse events (AEs) of any cause occurred in 30 of 33 (91%) of the savolitinib group and 100% of the sunitinib group. Twenty-two patients died during the study;with 3 deaths attributed to AEs, all in the sunitinib group.
Cabozantinib, crizotinib and savolitinib vs sunitinib
1) Progression-free survival rate
Median PFS was 9.0 months (95% CI 5.6–12.4) for cabozantinib and 5.6 months (95% CI 2.9–6.7) for sunitinib, with significantly improved HR for PFS of 0.60 (95% CI 0.37–0.97). This is considered a clinically relevant difference.
In addition to comparing cabozantinib and sunitinib, an additional 57 patients were inrolled to crizotinib and savolitinib arms. Both arms were closed due to hazard ratio for PFS greater than 1 at prespecified interim analysis. Savolitinib and crizotinib did not improve PFS relative to sunitinib.
2. Overall survival rate
There was no significant difference in overall survival between the four treatment groups, with reported median OS of 20.0 months (95% CI 11.3-Not calculated) in the cabozantinib arm and 16.4 months (95% CI 12.8–21.6) in the sunitinib arm.
3. Quality of life
The included literature did not report on this outcome measure.
4. Complications
Grade 3 or 4 adverse events occurred in 69%, 74%, 37% and 39% of patients receiving sunitinib, cabozantinib, crizotinib and savolitinib, respectively; one grade 5 thromboembolic event was seen with cabozantinib.
Level of evidence of the literature
Systematic reviews of RCTs for therapeutic research questions start at high GRADE.
mTOR inhibitor vs sunitinib
Everolimus versus sunitinib
The level of evidence regarding the outcome measure progression-free survival rate was downgraded by one level because of the relatively small number of included patients (imprecision) to Moderate GRADE.
The level of evidence regarding the outcome measure overall survival rate was downgraded by one level because of the relatively small number of included patients (imprecision) to moderate GRADE.
The level of evidence regarding the outcome measure quality of life was downgraded by one level because of the relatively small number of included patients (imprecision) to moderate GRADE.
The level of evidence regarding the outcome measure complications was downgraded by one level because of the relatively small number of included patients (imprecision) to moderate GRADE.
Temsirolimus vs sunitinib
The level of evidence regarding the outcome measure progression-free survival rate was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
The level of evidence regarding the outcome measure overall survival rate was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
The level of evidence regarding the outcome measure complications was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
Due to lack of evidence, no grading was possible for the outcome measures quality of life.
MET inhibitor vs sunitinib
Savolitinib vs sunitinib
The level of evidence regarding the outcome measure progression-free survival rate was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
The level of evidence regarding the outcome measure overall survival rate was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
The level of evidence regarding the outcome measure quality of life was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
The level of evidence regarding the outcome measure complications was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
Cabozantinib, crizotinib and savolitinib vs sunitinib
The level of evidence regarding the outcome measure measures progression-free survival rate was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to very low GRADE.
The level of evidence regarding the outcome measure overall survival rate was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
The level of evidence regarding the outcome measure complications was downgraded by two levels, one level because of study limitations (risk of bias) and one level because of the relatively small number of included patients (imprecision) to low GRADE.
Due to lack of evidence, no grading was possible for the outcome quality of life.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question: Is immunotherapy and/or targeted therapy as a first-line systemic therapy preferred to sunitinib in patients with metastatic non-clear cell renal cell carcinoma?
| P (Patients): |
Patients with metastatic non-clear cell renal cell carcinoma (nccRCC) |
| I (Intervention): |
Immunotherapy and/or targeted therapy |
| C (Control): | Sunitinib |
| O (Outcome measure): | 1) Progression-free survival rate, 2) overall survival rate, 3) quality of life and 4) complications |
Relevant outcome measures
The guideline development group considered progression-free survival rate and overall survival rate as a critical outcome measures for decision making; and quality of life and complications as important outcome measures for decision making.
A priori, the working group did not define the outcome measures listed above but used the definitions used in the studies.
The working group defined a relative risk (RR) or hazard ratio (HR) < 0.80 or >1.25 as a minimal clinically (patient) important difference for dichotomous or survival variables, and >0.5 SD for continuous variables.
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms from 2011 until December 31st 2022. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 431 hits. Studies that met the following criteria were eligible for selection: studies reporting original data, systematic reviews, randomized controlled trials (RCTs) and observational comparative studies reporting on various combinations of immunotherapy and targeted therapy with each other or with sunitinib in patients with metastatic non-clear cell renal carcinoma. Twenty-eight studies were initially selected based on title and abstract screening. After reading the full text, 26 studies were excluded (see the table with reasons for exclusion under the tab Methods), and 2 studies were included. Two other RCTs (Bergmann, 2020; Choueiri, 2020) were also included by reviewing reference list of included studies.
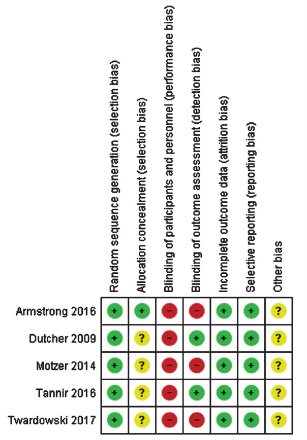
Results
One systematic review (Osterman, 2020) and one randomized, open-label, phase II trial (Pal, 2021) were included in the analysis of the literature. Systematic review of Osterman included 31 studies, of which 3 RCTs (Armstrong, 2016; Tannir, 2016 and Motzer, 2014) matched our PICO criteria. Two other RCTs (Bergmann, 2020; Choueiri, 2020) were also included by reviewing reference list of included studies. Important study characteristics and results are summarized in the evidence table. The assessment of the risk of bias is summarized in the risk of bias table.
Referenties
- 1 - Albiges, Laurence, et al. "Pembrolizumab plus lenvatinib as first-line therapy for advanced non-clear-cell renal cell carcinoma (KEYNOTE-B61): a single-arm, multicentre, phase 2 trial." The Lancet Oncology 24.8 (2023): 881-891.
- 2 - Bergmann, L., Grünwald, V., Maute, L., Grimm, M. O., Weikert, S., Schleicher, J., ... & Gauler, T. (2020). A randomized phase IIa trial with temsirolimus versus sunitinib in advanced non-clear cell renal cell carcinoma: An intergroup study of the CESAR Central European Society for Anticancer Drug Research-EWIV and the Interdisciplinary Working Group on Renal Cell Cancer (IAGN) of the German Cancer Society. Oncology research and treatment, 43(7-8), 333-339.
- 3 - Choueiri, T. K., Heng, D. Y., Lee, J. L., Cancel, M., Verheijen, R. B., Mellemgaard, A., ... & Albiges, L. (2020). Efficacy of savolitinib vs sunitinib in patients with MET-driven papillary renal cell carcinoma: the SAVOIR phase 3 randomized clinical trial. JAMA oncology, 6(8), 1247-1255.
- 4 - Lee, C.H., et al. Phase II Trial of Cabozantinib Plus Nivolumab in Patients With Non-Clear-Cell Renal Cell Carcinoma and Genomic Correlates. J Clin Oncol, 2022. 40: 2333.
- 5 - Osterman, C. K., & Rose, T. L. (2020). A systematic review of systemic treatment options for advanced non-clear cell renal cell carcinoma. Kidney Cancer, 4(1), 15-27.
- 6 - Pal, S. K., Tangen, C., Thompson, I. M., Balzer-Haas, N., George, D. J., Heng, D. Y., ... & Lara, P. N. (2021). A comparison of sunitinib with cabozantinib, crizotinib, and savolitinib for treatment of advanced papillary renal cell carcinoma: a randomised, open-label, phase 2 trial. The Lancet, 397(10275), 695-703.
- 7 - Singla, N., Hutchinson, R. C., Ghandour, R. A., Freifeld, Y., Fang, D., Sagalowsky, A. I., ... & Woldu, S. L. (2020, June). Improved survival after cytoreductive nephrectomy for metastatic renal cell carcinoma in the contemporary immunotherapy era: an analysis of the National Cancer Database. In Urologic Oncology: Seminars and Original Investigations (Vol. 38, No. 6, pp. 604-e9). Elsevier.
Evidence tabellen
Risk of Bias
|
Study
|
Appropriate and clearly focused question?1 |
Comprehensive and systematic literature search?2 |
Description of included and excluded studies?3 |
Description of relevant characteristics of included studies?4 |
Appropriate adjustment for potential confounders in observational studies?5 |
Assessment of scientific quality of included studies?6 |
Enough similarities between studies to make combining them reasonable?7 |
Potential risk of publication bias taken into account?8 |
Potential conflicts of interest reported?9
|
|
Osterman, 2020 |
Yes. Research question and inclusion criteria were clearly described. |
Yes. Medline and EMBASE were searched, and search period and strategy were reported.
|
Yes. Reasons for the excluded studies were reported. |
Yes. Characteristics were presented. |
Not applicable. |
Yes. Risk of bias was assessed. |
Yes. Clinical and statistical heterogeneity were considered. No meta-analyses were performed because of the heterogeneity. |
Yes. Authors stated that Based on the inclusion of multiple negative studies within this review, we do not suspect that publication bias had a significant impact on our results or conclusions. |
No. Source of funding not indicated for the included studies. |
Evidence table for systematic review of RCTs and observational studies (intervention studies)
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C)
|
Follow-up |
Outcome measures and effect size |
Comments |
|
Osterman, 2020
study characteristics and results are extracted from the SR (unless stated otherwise) |
SR and meta-analysis of RCTs
Literature search up to [month/year]
June 2019
A: Armstrong, 2016 B: Motzer, 2014 C: Tannir, 2016
Study design:
A: multicentre, open-label, randomised phase 2 trial B: open-label, randomized, multicenter, phase II C: Randomized Multicenter Phase 2 Trial
Setting and Country: A: 17 centres in the USA, Canada, and the UK B: 83 sites in 19 countries C: to 10 countries worldwide in approximately 50 to 75 sites
Source of funding and conflicts of interest: [commercial / non-commercial / industrial co-authorship]
|
Inclusion criteria SR:
Exclusion criteria SR:
3 studies included
Important patient characteristics at baseline:
N, mean age A: 108 patients, 61.5 yrs B: 471 patients, 62 years C: 68 patients, 59 years
Sex: A: 75% Male B: 73% Male C: 63% Male
Groups comparable at baseline? yes |
Describe intervention:
A: Everolimus 10 mg once daily B: Everolimus 10 mg daily continually C: Everolimus 10 mg/d orally
|
Describe control:
A: Sunitinib 50 mg once daily, for treatment cycles of 4 weeks on treatment and 2 weeks off treatment B: Sunitinib 50 mg daily in a schedule of 4 weeks on followed by 2 weeks off C: Sunitinib 50 mg/d orally for 4 wk on and 2 wk off.
|
End-point of follow-up:
A: 24 months after study closure, B: Not reported C: median follow-up of 23.6 mo (95% confidence interval [CI], 15.7–30.2).
For how many participants were no complete outcome data available? (intervention/control) A: I 13 participants (22%) C 10 participants (20%) B: I 0 participants (0%) C 1 participants (1%) C: I 2 participants (5.3%) C 1 participant (2.9%)
|
Outcome measure-1 Progression free survival
Effect measure: RR, RD, mean difference [95% CI]: A: I 5.6 (80% CI 5.5–6.0) C 8.3 (80% CI 5.8–11.4) HR 1.41 (80% CI 1.03–1.92) B: I 5.1 (2.6–7.9) C 7.2 (5.4–13.8) HR 1.5 (95% CI 0.9–2.8) C: I 4.1 (2.7–10.5) C 6.1 (4.2–9.4)
Outcome measure-2 Overall survival
A: I 13.2 (9.7 – 37.9) C 31.5 (14.8 – NR) HR 1.12 (0.7 – 2.1) B: C: I 14.9 (8.0 – 23.4) C 16.2 (14.2 – NR)
Outcome measure-3 Quality of life A: I the median FACT-KSI score was 47⋅5 (IQR 23–59); C 45 (27–56) B: EORTC QLQ-C30 global health status scores, fatigue scores, and physical functioning scores showed no significant difference between the two arms in both TDD and the longitudinal analysis. C:Not reported
Outcome measure-4 Complications (Any grade 3 or 4 AE) A: Everolimus 34 (60%) patients sunitinib 40 (78%) patients B: Everolimus (14; 14%) sunitinib (10; 9%) C: Everolimus 19 of 35 patients (54%) and in sunitinib 29 of 33 patients (88%)
|
Risk of bias (high, some concerns or low):
Facultative:
Brief description of author’s conclusion This systematic review supports current consensus guidelines recommending sunitinib or enrollment in a clinical trial as first-line treatment options for nccRCC, but also suggests a more nuanced approach to management and new options for therapy such as immune checkpoint inhibition. All patients with locally advanced or metastatic nccRCC should have genetic and molecular sequencing to identify those that may benefit from targeted therapies.
|
Evidence table for intervention studies (randomized controlled trials and non-randomized observational studies [cohort studies, case-control studies, case series])1
Research question:
|
Study reference |
Study characteristics |
Patient characteristics 2 |
Intervention (I) |
Comparison / control (C) 3
|
Follow-up |
Outcome measures and effect size 4 |
Comments |
|
Choueiri et al., 2020 |
Type of study: Randomized controlled trial (Phase 3)
Setting and country: Multicenter study, 32 centers across 7 countries
Funding and conflicts of interest: Funded by AstraZeneca, no significant conflicts of interest |
Inclusion criteria: MET-driven PRCC, measurable lesions, no prior treatment with MET or sunitinib inhibitors
Exclusion criteria: Prior sunitinib or MET inhibitor therapy
N total at baseline: 60 patients Intervention: 33 Control:27
Important prognostic factors2: Median age: 62 (23-78) I: 60 (23-78) years C: 65 (31-77) years
Sex: I: 29 (88) M C: 17 (63) M
Groups comparable at baseline? yes
|
Describe intervention (treatment/procedure/test): Savolitinib 600 mg once daily
|
Describe control (treatment/procedure/test): Sunitinib 50 mg once daily for 4 weeks on, 2 weeks off
|
Length of follow-up: Study terminated early; median follow-up not fully specified
Loss-to-follow-up: Intervention: N (%) 1 (2.7%) Reasons (describe) One patient withdrew consent after randomization.
Control: N (%) 3 (6.5%) Reasons (describe) Three patients discontinued due to adverse events.
Incomplete outcome data: Intervention: N (%) 2 (5.4%) Reasons (describe) Two patients were lost to follow-up before the first assessment.
Control: N (%)4 (8.7%) Reasons (describe) Four patients had incomplete data due to withdrawal from the study or adverse events. |
Outcome measures and effect size (include 95%CI and p-value if available):
PFS: savolitinib 7.0 (2.8-NC) Sunitinib 5.6 (4.1-6.9); HR (95% CI): 0.71 (0.37-1.36)
OS: Not reached for savolitinib vs. 13.2 (7.6-NC) months for sunitinib; HR (95% CI): 0.51 (0.21-1.17)
AEs: Grade 3 or higher AEs in 42% for savolitinib, 81% for sunitinib |
Limitations Premature termination of the study and the limited number of patients randomized are key limitations of this study and make definitive conclusions on safety and efficacy difficult to draw. |
|
Pal et al., 2021 |
Type of study: Randomized controlled trial (Phase 2)
Setting and country: Conducted at 65 centers in the US and Canada
Funding and conflicts of interest: Supported by NIH/National Cancer Institute, conflicts reported by some authors |
Inclusion criteria: Advanced PRCC, up to one prior therapy
Exclusion criteria: Untreated brain metastases
N total at baseline:147 46 sunitinib, 44 cabozantinib, 29 savolitinib, 28 crizotinib)
Important prognostic factors2: Median age: 66 (58-75) I: Cabozantinib 65 (58,75) years Crizotinib 68 (61,75) Savolitinib 67 (58,72) C: 65 (58-73)
Sex: 112 (76%) I: Cabozantinib 36 (82%) Crizotinib 22 (79%) Savolitinib 19 (66%) C: 35 (76%)
Groups comparable at baseline? yes |
Describe intervention (treatment/procedure/test):
Cabozantinib 60 mg oral daily with dose reductions to 40 mg and 20 mg permitted Crizotinib 250 mg twice daily with dose reductions to 200 mg twice daily and 250 mg once daily permitted Savolitinib 600 mg daily with dose reductions to 400 mg and 200 mg oral daily permitted
|
Describe control (treatment/procedure/test):
Sunitinib 50 mg once daily for 4 weeks on, 2 weeks off with dose reductions to 37.5 mg and 25 mg permitted |
Length of follow-up: Savolitinib arm halted early due to futility
Loss-to-follow-up: Intervention: N (%)2 (4.5%) Reasons (describe) Two patients discontinued due to adverse events.
Control: N (%) 3 (6.5%) Reasons (describe) Three patients withdrew consent.
Incomplete outcome data: Intervention: N (%)1 (2.3%) Reasons (describe) One patient had missing data due to a delay in follow-up.
Control: N (%) 2 (4.3%) Reasons (describe) Two patients had incomplete data due to treatment discontinuation.
|
Outcome measures and effect size (include 95%CI and p-value if available):
PFS: cabozantinib 9.0 months (95% CI: 5.6–12.4) Crizotinib 2.8 (2.6-3.6) savolitinib 3.0 (2.8-7.2) months sunitinib 5.6 (2.9-6.7) months
OS: cabozantinib 20 months (95% CI: 11.3–NR) Crizotinib 19.9 (11.2-NR) savolitinib 11.7 (6.7-28.9) months sunitinib 16.4 (12.8-21.6) months
AEs: Grade 3 or 4 AEs in 32 (74%) for Cabozantinib; 10 (37%) for Crizotinib; 11(39%) for savolitinib, 31 (68%) for sunitinib |
|
|
Bergmann 2020 |
Type of study: A Randomized Phase IIa Trial
Setting and country: Multicenter study conducted in Germany and Austria (CESAR and IAGN societies)
Funding and conflicts of interest: Supported by a grant from Pfizer Germany; no major conflicts reported. |
Inclusion criteria: Patients with histologically confirmed advanced non-clear cell renal cell carcinoma (nccRCC), including those with sarcomatoid features (>50% sarcomatoid component).
Exclusion criteria: Patients with previous treatment with VEGF or mTOR inhibitors, untreated brain metastases, and severe comorbidities.
N total at baseline:22 Intervention: 12 Control: 10
Important prognostic factors2: age ± SD: 60.8 (29–85) I: 59.5 years (29–85) C: 65.5 (46–80)
Sex: I: 67% male (8/12) C: 80% male (8/10)
Groups comparable at baseline? yes |
Describe intervention (treatment/procedure/test):
Temsirolimus: 25 mg intravenously once weekly
|
Describe control (treatment/procedure/test):
Sunitinib: 50 mg orally, daily for 4 weeks on, 2 weeks off |
Length of follow-up:
Median follow-up duration of 9.3 months
Loss-to-follow-up: Intervention: N (%) 0 Reasons (describe) No patients were lost to follow-up.
Control: N (%) 1 (10%) Reasons (describe) One patient discontinued due to treatment-related adverse events.
Incomplete outcome data: Intervention: N (%) 1 (8.3%) Reasons (describe) One patient was unable to complete the treatment due to disease progression.
Control: N (%) 1 (10%) Reasons (describe) One patient discontinued treatment due to intolerable side effects.
|
Outcome measures and effect size (include 95%CI and p-value if available):
Progression-free survival (PFS): Median PFS was 9.3 months for temsirolimus vs. 13.2 months for sunitinib (HR: 1.64, 95% CI: 0.65–4.18, p = 0.20).
Overall survival (OS): Median OS was 19.4 months for temsirolimus vs. 19.8 months for sunitinib (HR 0.98, 95% CI: 0.31–3.09).
Adverse events (AEs): Serious AEs occurred in 91.7% of temsirolimus patients and 100% of sunitinib patients. The most common AEs included cytopenia, gastrointestinal events, and infections. |
The recruitment rate was low and the trial had to be ended prematurely. |
Table of quality assessment for systematic reviews of RCTs and observational studies
Based on AMSTAR checklist (Shea et al.; 2007, BMC Methodol 7: 10; doi:10.1186/1471-2288-7-10) and PRISMA checklist (Moher et al 2009, PLoS Med 6: e1000097; doi:10.1371/journal.pmed1000097)
Risk of bias table for intervention studies (randomized controlled trials; based on Cochrane risk of bias tool and suggestions by the CLARITY Group at McMaster University)
Research question: Is immunotherapy and/or targeted therapy as a first-line systemic therapy preferred to sunitinib in patients with metastatic non-clear cell renal cell carcinoma?
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
|
Was the allocation adequately concealed?
|
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded? |
Was loss to follow-up (missing outcome data) infrequent?
|
Are reports of the study free of selective outcome reporting?
|
Was the study apparently free of other problems that could put it at a risk of bias?
|
Overall risk of bias If applicable/necessary, per outcome measure
|
|
Pal, 2020 |
Probably yes;
Reason: Randomization was dynamically balanced on two stratification factors. |
Probably no;
Reason: not reported |
Definitely no;
Reason: open-label |
Probably yes;
Reason: No loss to follow-up reported. |
Probably yes;
Reason: All relevant outcomes were reported. |
Probably yes;
Reason: No other problems noted. |
Some concerns |
|
Bergman, 2020 |
Probably no;
Patients who met the eligibility criteria were randomly assigned 1: 1 |
Probably no;
Not reported |
Definitely no;
Reason: open-label |
Probably yes;
Reason: No loss to follow-up reported. |
Probably yes;
Reason: All relevant outcomes were reported. |
Probably no;
Trial had to be terminated due to low recruitment and the small numbers. |
High |
|
Choueiri, 2020 |
Probably no;
Patients were randomized in a 1:1 ratio |
Probably no;
Not reported |
Probably no;
Open label sponsor-blinded study; blinded independent central review; |
Definitely yes
1 Lost to follow-up in savolitinib |
Probably yes;
Reason: All relevant outcomes were reported. |
Probably no;
Premature termination of the study and the limited number of patients randomized |
High
|
Table of excluded studies
|
Authors |
Reason |
|
Brown, 2022 |
Better systematic review available |
|
Bellmunt, 2013 |
Narrative review |
|
Bellmunt, 2013 |
Narrative review |
|
Bitting, 2011 |
Narative review |
|
Buti, 2021 |
Does not comply with PICO (clear cell) |
|
Chahoud, 2020 |
Does not comply with PICO (No comparison with sunitinib) |
|
Choueiri, 2021 |
Post hoc from JAVELIN Renal 101 trial |
|
de Vries-Brilland, 2021 |
Narrative review |
|
Fernandez-Pello, 2017 |
Better systematic review available |
|
Graham, 2022 |
Retrospective study -VEGF targeted therapy, mTOR targeted therapy, ICI-based therapy- |
|
Gulati, 2020 |
Narrative review |
|
Hutson, 2021 |
Does not comply with PICO (non comparative study, single arm phase II Lenvatinib+everolimus ) |
|
Jung, 2018 |
Does not comply with PICO ( No RCT, single arm, no comparison with sunitinib) |
|
Martin, 2019 |
Retrospective study |
|
McDermott, 2021 |
Does not comply with PICO ( No RCT, single arm, no comparison with sunitinib) |
|
Palma Dos Reis, 2022 |
Does not comply with PICO (no comparison with sunitinib) |
|
Papanikolaou, 2020 |
Does not comply with PICO (wrong population, retrospective studies included) |
|
Park, 2018 |
Does not comply with PICO (no comparison with sunitinib, Phase II Axitinib) |
|
Puente, 2016 |
Summary of an expert review panel meeting |
|
Sepe, 2021 |
Narrative review |
|
Tachibana, 2021 |
Does not comply with PICO (no comparison with sunitinib, retrospective of 30 patients) |
|
Tannir, 2012 |
Does not comply with PICO (no comparison, single arm Phase II with sunitinib) |
|
Tannir, 2021 |
Post hoc of CheckMate 214 |
|
Tazi, 2011 |
Narrative review |
|
Twardowski, 2017 |
Does not comply with PICO (no comparison, single arm Phase II with sunitinib) |
|
Vogelzang, 2020 |
Does not comply with PICO ( No RCT, single arm, no comparison with sunitinib) |
|
Voss, 2016 |
Does not comply with PICO (no comparison with sunitinib, Phase II, Everolimus Plus Bevacizumab) |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 30-09-2025
Beoordeeld op geldigheid : 13-05-2025
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Stichting Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2021 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met nierkanker en een vertegenwoordiger namens de patiëntenvereniging.
Werkgroep
- Dr. A. (Axel) Bex, uroloog, Antoni van Leeuwenhoek, Amsterdam, NVU (voorzitter)
- Dr. R.F.M. (Rob) Bevers, uroloog, Leids Universitair Medisch Centrum, Leiden, NVU
- Dr. J.F. (Hans) Langenhuijsen, uroloog, Radoudumc, Nijmegen, NVU
- Dr. A.P. (Paul) Hamberg, internist-oncoloog, Franciscus Gasthuis en Vlietland Ziekenhuis, Rotterdam, NIV/NVMO
- Dr. J.V. (Hans) van Thienen, internist-oncoloog, Antoni van Leeuwenhoek, Amsterdam, NIV/NVMO
- J. (Jolanda) Bloos-van der Hulst, verpleegkundig specialist, Antoni van Leeuwenhoek, Amsterdam, V&VN
- Dr. A.M.E. (Anna) Bruynzeel, radiotherapeut-oncoloog, Amsterdam Medisch Centrum, NVRO
- Dr. L. (Linda) Kerkmeijer, radiotherapeut-oncoloog, Radboudumc, Nijmegen, NVRO
- Drs. E. (Else) Wolak, belangenbehartiger Kwaliteit van zorg, Patiëntenvereniging Blaas- of Nierkanker
- Dr. M.A.J. (Mark) Meier, interventieradioloog, Isala Ziekenhuis, Zwolle, NVvR / NVIR
Met ondersteuning van
- Drs. D.A.M. (Danique) Middelhuis, junior adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Dr. M.H.D. (Majke) van Bommel, adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Dr. M. (Mohammadreza) Abdollahi, adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Dr. J.H. (Hanneke) van der Lee, senior-adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Dr. I.M. (Irina) Mostovaya, senior-adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Linda Niesink, medisch informatie specialist, Kennisinstituut van de Federatie Medisch Specialisten
- Esther van der Bijl, medisch informatie specialist, Kennisinstituut van de Federatie Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Bex (voorzitter) |
Uroloog AVL Amsterdam. Afdelingshoofd in het Specialist Centre of Kidney Cancer, Royal Free London NHS Foundation Trust, Professor of Urology, UCL Division of Surgery and Investigational Science. |
Alle nevenfuncties zijn onbetaald: |
- Restricted educational grant van Pfizer tbv een neoadjuvante studie (sponsor is het NKI-AvL). - Steering committee op twee internationale adjuvante fase 3 studies van BMS en Roche. - Lid van medical steering committee van twee patientenorganisaties (Kidney Cancer Association en IKCC). - Financier BMS: randomised phase 3 trial of adjuvant nivolumab plus ipilimumab versus placebo in high risk RCC. - Financier Roche: randomised phase 3 trial of adjuvant atezolizumab versus placebo in high risk RCC. - Financier Pfizer: single-arm phase 2 trial of neoadjuvant avelumab plus axitinib in high risk RCC (funded by restricted educational grant) |
Geen restricties |
|
Bevers |
Uroloog LUMC Leiden |
Geen |
Geen |
Geen restricties |
|
Langenhuijsen |
Uroloog Radboudumc Nijmegen |
Invited speaker Update Urology (Astra Zeneca), vergoeding+reiskosten |
Financier: ZonMW Voorbereidende studie Doelmatigheidsonderzoek, Pentixafor PET vs veneuze sampling bij primair hyperaldosteronisme - Financier: PentixaPharm GmbH, CASTUS trial. |
Geen restricties |
|
Hamberg |
Oncoloog Franciscus Gasthuis en Vlietland Rotterdam |
voorzitter WIN-O nier (onbetaald) bestuurslid Pro RCC (onbetaald) |
- Adviesraden meerdere farmaceutische bedrijven actief binnen RCC zorg - lokale hoofonderzoeker van aantal adjuvante nierkanker studies (Farma sponsored). Tevens ook van studies (farma sponsored) naar medicamenteuze interventies bij gemetastaseerde ziekte (oa RCC) |
Geen restricties |
|
Van Thienen |
Internist-oncoloog NKI-AvL Amsterdam |
Alle nevenfuncties zjn onbetaald: - Inhoudelijk/vice voorzitter Medisch Inhoudelijke Standpunten (MIS) groep van DRCG - Lid wetenschappelijke adviesraad Stichting PRO-RCC |
Pfizer Neoadjuvant axitinib en avelumab bij niercelcarcinoom (projectleider); BMS Checkmate 914 Adjuvant immunotherapy in high-risk renal cancer (onderzoeker); Eisai CLEAR study: levantinib and everolimus or pembrolizumab vs sunitinib in mRCC (onderzoeker); Goethe University Frankfurt am Main Sunniforecast (nivolumab+ipilimumab vs sunitinib in non-clear cell mRCC)(onderzoeker); Roche Adjuvant atezolizumab in high risk renal cancer (onderzoeker) |
Geen restricties |
|
Bloos-van der Hulst |
Verpleegkundig specialist uro-oncologie AVL Amsterdam |
Geen |
Geen |
Geen restricties |
|
Kerkmeijer |
Radiotherapeut-oncoloog, Radboudumc Nijmegen. Plaatsvervangend keteneigenaar Urologische Oncologie Radboudumc Nijmegen |
Alle nevenfuncties zjn onbetaald: - DUOS bestuurslid - Raad van Advies Tie Ribbon - Associate Editor Frontiers in oncology - Radiotherapeut-oncoloog UMC Utrecht (gastaanstelling) |
KWF subsidie FLAME studie prostaatcarcinoom |
Geen restricties |
|
Wolak |
Belangenbehartiger kwaliteit van zorg Patiëntenvereniging blaas- of nierkanker (PBNK) |
Patiëntenvereniging blaas- of nierkanker |
Werkzaam bij patiëntenorganisatie Leven met blaas- of nierkanker, geen boegbeeldfunctie |
Geen restricties |
|
Meier |
Interventieradioloog Isala Zwolle Voorzitter RVE Medische Beeldvorming, Isala Zwolle |
|
Geen |
Geen restricties |
|
Bruynzeel |
Radiotherapeut-oncoloog, Amsterdam UMC |
Geen |
ViewRay Inc: Een onderzoek naar hoge en precieze bestraling (stereotactische ablatieve radiotherapie) bij patiënt |
Geen restricties |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door uitnodigen van de Patiëntenvereniging blaas- of nierkanker (PBNK) voor de schriftelijke knelpunteninventarisatie en afvaardiging namens PBNK in de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen (zie per module ook “Waarden en voorkeuren van patiënten”). De conceptrichtlijn is tevens voor commentaar voorgelegd aan Patiëntenvereniging blaas- of nierkanker (PBNK) en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijnmodule is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd om te beoordelen of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling is de richtlijnmodule op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Module |
Uitkomst raming |
Toelichting |
|
Module Optimale eerstelijns systeemtherapie niet-heldercellig niercelcarcinoom |
geen financiële gevolgen |
Uitkomst 1 |
De kwalitatieve raming volgt na de commentaarfase.
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 3.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor patiënten met nierkanker. Tevens zijn er knelpunten aangedragen door de NVU (Nederlandse Vereniging voor Urologie) en NVRO, NVVR en Patiëntenvereniging blaas- of nierkanker (PBNK) via een schriftelijke knelpuntenanalyse.
Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. Review Manager 5.4 werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
Algemene informatie
|
Richtlijn: Herziening Niercelcarcinoom |
|
|
Uitgangsvraag: Wat is de optimale eerstelijns systeemtherapie bij patiënten met gemetastaseerd niet-heldercellig niercelcarcinoom? |
|
|
Database(s): Medline (OVID), Embase |
Datum: 31-12-2022 |
|
Periode: >2011 |
Talen: Engels, Nederlands |
|
Literatuurspecialist: Linda Niesink |
|
|
BMI zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting:
→ Voor deze vraag is gezocht op de elementen gemetastaseerd, niet-heldercellig (in het groen) niercelcarcinoom (in het blauw), en immuuntherapie óf targeted therapy (in het oranje).
→ Resultaten staan in Rayyan. |
|
|
Te gebruiken voor richtlijnen tekst: In de databases Embase (via embase.com) en Medline (via OVID) is op 04-01-2022 met relevante zoektermen gezocht naar systematische reviews en RCT’s over immuuntherapie en/of targeted therapy bij patiënten met gemetastaseerd niet-heldercellig niercelcarcinoom. De literatuurzoekactie leverde 51 unieke treffers op. |
|
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SRs |
15 |
13 |
17 |
|
RCTs |
32 |
15 |
34 |
|
Totaal |
47 |
28 |
51 |
Zoekstrategie
|
Database |
Zoektermen |
||||||||||||||||||||||||||||||
|
Embase
|
|
||||||||||||||||||||||||||||||
|
Medline (OVID)
|
1 exp Carcinoma, Renal Cell/ or (('kidney cell*' or 'renal cell*' or nephroid or hypernephroid or 'collecting duct') adj3 (cancer* or carcinoma* or adenocarcinoma* or neoplasm* or tumor* or tumour* or mass*)).ti,ab,kf. or (grawitz* adj3 (tumor* or tumour*)).ti,ab,kf. or hypernephroma*.ti,ab,kf. or (RCC or MRCC or nccrcc or ncrcc).ti,ab,kf. (54683) 2 (exp Neoplasm Metastasis/ or (advanced or metastat*).ti,ab,kf.) AND ('non clear' or nccrcc or ncrcc).ti,ab,kf. (326) 3 exp Molecular Targeted Therapy/ or (targeted adj3 therap*).ti,ab,kf. or exp Nivolumab/ or exp Axitinib/ or exp Ipilimumab/ or nivolumab.ti,ab,kf. or lenvatinib.ti,ab,kf. or tivozanib.ti,ab,kw. or axitinib.ti,ab,kw. or exp IMMUNOTHERAPY/ or (immune therap* or immunotherap* or 'immune checkpoint' or cabozantinib or ipilimumab or pembrolizumab or tivozanib or avelumab).ti,ab,kf. (474659) 4 1 and 2 and 3 (161) 5 limit 4 to ((english or dutch) and yr="2011 -Current") (138) 6 5 not (comment/ or editorial/ or letter/ or ((exp animals/ or exp models, animal/) not humans/)) (134) 7 (meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf.) (565255) 8 (exp randomized controlled trial/ or randomized controlled trials as topic/ or random*.ti,ab. or rct?.ti,ab. or ((pragmatic or practical) adj "clinical trial*").ti,ab,kf. or ((non-inferiority or noninferiority or superiority or equivalence) adj3 trial*).ti,ab,kf.) not (animals/ not humans/) (1341657) 9 6 and 7 (13) – SRs 10 (6 and 8) not 9 (15) - RCTs 11 9 or 10 (28) |