Beeldvorming MRI of CT
Uitgangsvraag
Welk (aanvullend) beeldvormend onderzoek wordt aanbevolen bij chronische posttraumatische anterieure schouderinstabiliteit?
Aanbeveling
Verricht bij patiënten met chronische posttraumatische anterieure schouderinstabiliteit indien een operatieve ingreep wordt overwogen slechts één vorm van aanvullend beeldvormend onderzoek: een MRI-scan of een CT-scan.
- Kies voor MRI (bij voorkeur artrografie) bij patiënten bij wie informatie over wekedelen status gewenst is en bepaal hiermee ook de aanwezigheid van eventuele ossale schade.
- Kies voor CT bij patiënten bij wie op basis van conventionele röntgenopnamen (de mate van) ossale schade onvoldoende te beoordelen is voor de keuze van aanvullende behandeling, óf als MRI niet mogelijk/ beschikbaar is.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Naast het labrum speelt ossale integriteit een belangrijke rol in glenohumerale stabiliteit. Ossale schade na een anterieure schouderluxatie is het gevolg van impactie van de posterosuperieure humeruskop tegen de anteroinferieure glenoïdrand, wat kan leiden tot respectievelijk een Hill Sachs deformiteit van de humeruskop, een losliggend ossaal Bankart fragment van het glenoïd en/of glenoïdaal botverlies na recidiverende luxaties.
Ten tijde van het trauma wordt gebruik gemaakt van beeldvorming in de vorm van röntgenonderzoek als eerste screening; bij patiënten met schouderinstabiliteit na recidiverende luxaties wordt in de preoperatieve planning aanvullend onderzoek zoals CT en MRI aangewend, veelal in combinatie. De huidige standaard om glenohumeraal botverlies te detecteren en kwantificeren is een 3D-CT (Bishop, 2013; Rerko, 2013). CT-onderzoek is in de meeste ziekenhuizen breed beschikbaar en gemakkelijk te interpreteren.
In het afgelopen decennium zijn MRI-technieken sterk verbeterd, waardoor de werkgroep wilde onderzoeken of MRI de CT kan vervangen. De belangstelling om door middel van MRI ossale schade vast te stellen en te kwantificeren komt voort uit het ontbreken van potentieel schadelijke röntgenstraling in een veelal jonge patiëntengroep én het feit dat MRI vaak al routinematig wordt vervaardigd bij patiënten met schouderinstabiliteit om schade aan weke delen te beoordelen. Hieronder verstaan we labrum-, capsuloligamentaire en rotatorcuffpees-letsels, die ook veelvoorkomend zijn na een traumatische (sub)luxatie.
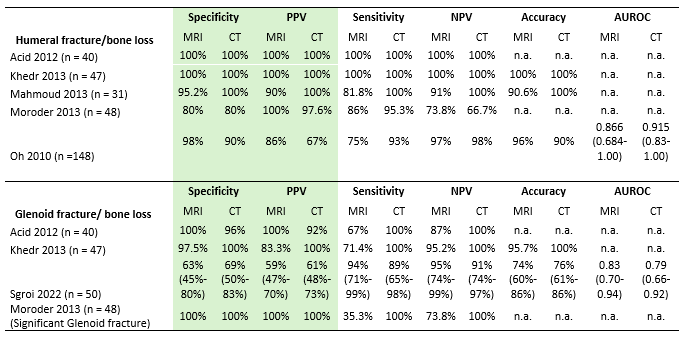
In de systematische literatuuranalyse werden diverse studies geïncludeerd die de sensitiviteit en specificiteit van MRI en CT vergeleken met referentiestandaard arthroscopie (Oh, 2010; Acid, 2012; Khedr, 2013; Moroder, 2013; Mahmoud, 2013; Sgroi, 2022). De werkgroep concludeert dat voor de cruciale uitkomstmaten (specificiteit en positief voorspellende waarde) MRI een vergelijkbare accuratesse heeft als CT voor het vaststellen van humeruskop fracturen en glenoïdaal botverlies. Beide modaliteiten kunnen als zodanig aangewend worden als primaire modaliteit voor preoperatieve evaluatie van de ossale situatie.
De kwaliteit van het bewijs werd als laag beoordeeld, doordat in accuratessestudies MRI versus CT de gekozen referentiestandaard arthroscopie vrijwel altijd wordt geïnterpreteerd met kennis van de resultaten van de beeldvorming, wat mogelijk bias veroorzaakt. Bovendien waren patiëntaantallen laag. Mede door deze lage zekerheid kiest de werkgroep ervoor om niet MRI als voorkeursmodaliteit aan te dragen boven CT, ondanks dat dit bij vergelijkbare accuratesse wellicht voor de hand ligt vanwege het ontbreken van potentieel schadelijke röntgenstraling en de extra informatie over weke delen status die een MRI oplevert. Bovendien heeft de werkgroep rekening gehouden met het landelijke capaciteitsprobleem met betrekking tot de beschikbaarheid van MRI. In Nederlandse ziekenhuizen is op dit moment CT doorgaans beter en sneller beschikbaar en ook goedkoper. Voor de behandelend trauma-/ orthopedisch chirurg is soms informatie over weke delen status niet meer bijdragend voor de keuze van de operatieve techniek, omdat bij een bewezen luxatie op de initiële röntgenopnamen er doorgaans vanuit kan worden gegaan dat het labrum ook beschadigd is.
De belangrijkste aanbeveling is om niet (meer) allebei de onderzoeken te verrichten in de preoperatieve setting. In het geval dat MRI voor beoordeling weke delen status en CT voor beoordeling ossale status nog worden gecombineerd, kan het CT-onderzoek achterwege worden gelaten, omdat de toch al vervaardigde MRI vergelijkbare informatie geeft over de aanwezigheid van ossale schade.
Wat opvalt is dat de literatuuranalyse studies includeerde die - met inachtneming van de snelheid van ontwikkeling van MRI-scanners en technieken - alweer redelijk gedateerd zijn. Van de zes studies dateert er één uit 2022; de overige stammen uit de periode 2010-2013. In recentere literatuur wordt wél gepleit voor MRI als eerste keuze onderzoek om glenoïdaal en humeraal botverlies te kwantificeren, echter in de opzet van deze studies worden veelal ofwel CT of MRI versus arthroscopie bestudeerd, of ontbreekt een referentiestandaard waardoor het onmogelijk is een uitspraak te doen over diagnostische accuratesse (Walter, 2019; Sgroi, 2021). Deze twee recente reviews concluderen dat 2D of 3D MRI en CT vergelijkbare methoden zijn voor het bepalen van glenoïdaal botverlies (Walter, 2019), en dat MRI en CT gelijkwaardig zijn in het bepalen van humeraal botverlies, met uitzondering van het bepalen van het Hill Sachs interval waar MRI een hogere accuratesse toont (Sgroi, 2021).
Buiten de scope van de huidige vraagstelling valt het gebruik van intra-articulair contrast (artrografie). Van de geselecteerde onderzoeken onderzochten vier studies CT-artrografie versus MRI (Acid, 2012; Kehdr, 2013; Mahmoud, 2013; Oh, 2010), terwijl de in Nederland gangbare praktijk is om een CT zonder intra-articulair contrast te verrichten. In de overige twee studies werd CT vergeleken met MRI zonder artrografie (Moroder, 2013; Sgroi, 2022), terwijl in Nederland vaak MRI met artrografie wordt gebruikt. Distensie van het gewrichtskapsel middels intra-articulair contrast maakt intra-articulaire structuren beter zichtbaar en afgrensbaar en verhoogt de detectie van labro-ligamentair letsel (Smith; 2012). Aangezien de focus van deze module op ossale structuren ligt, heeft de werkgroep besloten in het literatuuronderzoek geen onderscheid te maken tussen CT en MRI met of zonder intra-articulair contrast.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
CT kent een lagere belasting voor de patiënt; het onderzoek is sneller uitvoerbaar en heeft minder contra-indicaties, zoals aanwezigheid van metaal/ implantaten in het lichaam. Door de snelheid van het onderzoek is claustrofobie ook minder een probleem. CT is in de meeste Nederlandse ziekenhuizen toegankelijker, waardoor de patiënt minder lang op de wachtlijst staat. Waarschijnlijk hebben patiënten hierdoor een voorkeur voor CT. Daarentegen zal door het nadeel van stralenbelasting de patiënt mogelijk de voorkeur geven aan MRI. Het verrichten van slechts één preoperatief onderzoek, in plaats van de combinatie CT én MRI, draagt vanzelfsprekend ook bij aan verhoging van patiënten comfort.
Kosten (middelenbeslag)
Een MRI-onderzoek is duurder dan een CT-onderzoek. Buiten de bovengenoemde voor- en nadelen van beide modaliteiten, kan dit ook nog worden meegenomen in de overwegingen.
Naar verwachting kan deze richtlijn voor een vermindering in kosten zorgen, omdat nu vaak zowel CT als MRI worden gemaakt. Het doen van één onderzoek brengt minder kosten met zich mee.
Aanvaardbaarheid, haalbaarheid en implementatie
De werkgroep voorziet geen problemen met het implementeren van de aanbevelingen. In de huidige situatie wordt er gebruik gemaakt van ofwel CT, ofwel MRI (artrografie) of een combinatie van beide onderzoeken, gebaseerd op lokale voorkeur van orthopedisch/ traumachirurgen en radiologen. Metingen om ossale schade aan glenoïd en humeruskop te bepalen kunnen op beide modaliteiten op dezelfde manier worden verricht, mits 2D CT en MRI onderzoeken optimaal worden geanguleerd parallel aan het glenoïd, of er gebruik wordt gemaakt van een 3D-techniek zodat de beoordelaar zelf reconstructies kan maken. De werkgroep adviseert hierbij om een MRI-scanner met tenminste een veldsterkte van 1.5 Tesla te gebruiken, omdat hierbij een resolutie wordt gehaald die de corticale contouren van het glenoïd betrouwbaar weergeeft. Bij voorkeur worden ossale structuren beoordeeld op een T1-gewogen sequentie zonder vetonderdrukking.
Rationale van de aanbeveling: weging van argumenten voor en tegen de diagnostische procedure
Systematisch literatuuronderzoek toonde aan dat MRI mogelijk een vergelijkbare diagnostische accuratesse heeft als CT voor de detectie van ossale schade bij patiënten met posttraumatische schouderinstabiliteit. Dit geldt voor zowel schade aan het glenoïd als aan de humeruskop. Het ligt derhalve voor de hand om MRI aan te bevelen als voorkeursmodaliteit voor preoperatieve beeldvorming, gezien het ontbreken van potentieel schadelijke röntgenstraling én de extra informatie die een MRI oplevert over weke delen. Echter, de werkgroep houdt ook rekening met de in Nederlandse ziekenhuizen doorgaans betere beschikbaarheid en lagere kosten van CT en situaties waarin informatie over weke delen status niet meer bijdragend is voor de keuze van de operatieve techniek. Hierdoor is het ook te verantwoorden om CT als eerste keuze diagnostische modaliteit te verrichten. De belangrijkste aanbeveling is om niet allebei de onderzoeken te verrichten in de preoperatieve setting.
Onderbouwing
Achtergrond
Bone loss in patients with post-traumatic shoulder instability can occur on both the glenoid and humeral sides, respectively anteroinferior glenoid bone loss or a loose (bony Bankart) fragment, and a humeral (Hill Sachs) impaction fracture. The gold standard for determining the presence of bone loss is arthroscopy. Additional imaging is often performed preoperatively with a CT-scan.
The issue with this CT-scan is that potentially harmful X-rays are used, and that CT-scans only provide information about osseous damage, while MRI also shows damage to soft tissues. For example, labral, capsuloligamentous and rotator cuff tendon injuries can occur after a (sub)luxation. In the past decade, new MRI techniques have been developed and existing techniques have been greatly improved, which means that they can possibly replace CT. This can also be cost-efficient, because CT and MRI are now often performed both. The presence or absence and degree of glenoid and/or humeral bone loss contributes to the choice of a particular orthopedic strategy: soft tissue repair alone or in combination with bony reconstruction.
Conclusies / Summary of Findings
|
Low GRADE |
The use of MRI may result in comparable specificity and positive predictive value compared with CT for diagnosing humeral fracture / bone loss in patients with suspicion of osseous component post-traumatic shoulder instability.
Sources: Acid, 2012; Khedr, 2013; Mahmoud, 2013; Moroder, 2013; Oh, 2010 |
|
Low GRADE |
The use of MRI may result in comparable specificity and positive predictive value compared with CT for diagnosing glenoid fracture/ bone loss in patients with suspicion of osseous component post-traumatic shoulder instability.
Sources: Acid, 2012; Khedr, 2013; Sgroi, 2022 |
|
Very low GRADE |
The evidence is very uncertain about the specificity and positive predictive value of using MRI compared with CT for diagnosing significant glenoid defect in patients with suspicion of osseous component post-traumatic shoulder instability.
Source: Mahmoud, 2013 |
Samenvatting literatuur
Description of studies
Acid (2012) performed a cross-sectional study in the setting of radiology department in France. The inclusion criteria were: patients proposed with arthroscopic treatment, underwent both Multidetector Computed Tomography (MDCT) and Magnetic Resonance Angiography (MRA) on the same day in the author’s institution according to a standardized protocol as part of the preoperative workup, and arthroscopy of the shoulder was performed by the same orthopedic surgeon, with a prospective description of the intraarticular lesions related to anterior shoulder instability. The exclusion criteria were a history of arthroscopic or open shoulder surgery, and a time delay between imaging and arthroscopy longer than 1 month. Forty patients were included in the study, whereas the number of eligible patients was unreported. The mean age was 26 years (range 17-48), with 75% males. The index test was MDCT and MRA, whereas the reference test was arthroscopy. The prevalence of humeral head fracture was 98% and of glenoid rim fracture was 30% in this study population.
Khedr (2013) conducted a cross-sectional study in the setting of radiology department in Egypt. The inclusion criteria were: Patients with anterior shoulder instability with proposed arthroscopic treatment; MDCT arthrography and MR arthrography of the shoulder performed (with the time interval between the two examinations is 1 hour) in the author’s institution according to a standardized protocol as part of the preoperative workup; and arthroscopy of the shoulder performed by the same orthopedic surgeon, with a prospective description of the intraarticular lesions related to anterior shoulder instability. The exclusion criteria were a time delay between imaging and arthroscopy longer than 1 month. Forty-seven patients included in the study, whereas the number of eligible patients was unreported. The mean age was 26 years (range 21-48), with 74% males. The index test was MDCT and MRA, whereas the reference test was arthroscopy. The prevalence of humeral head fracture was 57% and of glenoid fracture was 15% in this study population.
Mahmoud (2013) demonstrated a cross-sectional study in the setting of diagnostic radiology department in Egypt. The inclusion criteria were consecutive patients referred from the orthopedic clinic with planned arthroscopy for a clinical diagnosis of shoulder lesion. The exclusion criteria were fractures, septic shoulder, and a gap of more than 100 days between the imaging and the operation. Also, all metallic (non-titanium) body implants and early pregnancy were considered an absolute contraindication to the performance of MRA and MDCTA procedures. Thirty-one patients were included in the study, whereas the number of eligible patients was unreported. The mean age was not reported, and the range was 21-70 years, with 77% males. The index test was MDCTA and MRI, whereas the reference test was arthroscopy. The prevalence of Hill-Sachs (and bone lesions) was 35% in this study population.
Moroder (2013) performed a retrospective study in the setting of surgical department in Germany. The inclusion criteria were history of recurrent anterior shoulder instability, including failed prior arthroscopic or open stabilization surgery, and complete pre-operative MRI and CT-scans with 3D-reconstruction of the glenoid. There were no specific exclusion criteria. Forty-eight patients out of 83 (57.8%) eligible patients included. The mean age was 31 years (range 20-78), with 83% males. The index test was CT and MRI, whereas the reference test was open surgery. The prevalence of significant glenoid defect (defect >= 20% of the glenoid width) was 35% and Hill-Sachs was 90% in this study population.
Oh (2010) reported a cross-sectional study in the setting of Orthopaedic Surgical department in Korea. The inclusion criteria were consecutive patients who underwent CTA or MRA of the shoulder and a subsequent arthroscopic surgical procedure performed by a single surgeon. The exclusion criteria were fracture, septic shoulder, and a gap of more than 100 days between the imaging test and the operation. There were 148 out of the 168 (88%) eligible patients included. Patients were randomly referred for CTA (n = 78) and MRA (n = 70). The mean age all included patients was 46.6 years (range 17-78), with 53% males. The index tests were CTA and MRA, whereas the reference test was arthroscopy. The prevalence of Hill-Sachs (and bone lesions) was not reported in this study population.
Sgroi (2022) demonstrated a cross-sectional study in the setting of Orthopaedic Surgical department in Germany. The inclusion criteria were patients with available preoperative AP radiographs, WP radiographs, CT, and MR images of the affected shoulder. The exclusion criteria were not all planes or layers (such as sagittal, axial, or frontal) of each diagnostic imaging modalities were available and insufficient quality of diagnostic images (for example, setting of the layers did not allow adequate face view of the glenoid). Fifty out of 80 eligible patients (68.5%) were included. The mean age was 26 years (SD 12), with 74% males. The index test was CT and MRI, whereas the reference test was arthroscopy. The prevalence of glenoid bone loss was not reported in this study population.
Results
Humeral fracture/bone loss
Specificity
Five studies reported on specificity. Acid (2012) demonstrated a specificity of 100% for both MRI and CT, based on data from 40 patients. Khedr (2013) reported a specificity of 100% for both MRI and CT, based on data from 47 patients. Mahmoud (2013) demonstrated a specificity of 95.2% for MRI and 100% for CT based on data from 31 patients. Moroder (2013) reported a specificity of 80% for both MRI and CT based on data from 48 patients. Oh (2010) presented a specificity of 98% for MRI and 90% for CT based on data from 148 patients.
Positive predictive value (PPV)
Five studies reported on PPV. Acid (2012) demonstrated a PPV of 100% for both MRI and CT, based on data from 40 patients. Khedr (2013) reported a PPV of 100% for both MRI and CT, based on data from 47 patients. Mahmoud (2013) demonstrated a PPV of 90% for MRI and 100% for CT based on data from 31 patients. Moroder (2013) reported a PPV of 100% for MRI and 97.6% for CT based on data from 48 patients. Oh (2010) presented a PPV of 86% for MRI and 67% for CT based on data from 148 patients.
Sensitivity
Five studies reported on PPV. Acid (2012) demonstrated a sensitivity of 100% for both MRI and CT, based on data from 40 patients. Khedr (2013) reported a sensitivity of 100% for both MRI and CT, based on data from 47 patients. Mahmoud (2013) demonstrated a sensitivity of 81.8% for MRI and 100% for CT based on data from 31 patients. Moroder (2013) reported a sensitivity of 86% for MRI and 95.3% for CT based on data from 48 patients. Oh (2010) presented a sensitivity of 75% for MRI and 93% for CT based on data from 148 patients.
Negative predictive value (NPV)
Five studies reported on PPV. Acid (2012) demonstrated a NPV of 100% for both MRI and CT, based on data from 40 patients. Khedr (2013) reported a NPV of 100% for both MRI and CT, based on data from 47 patients. Mahmoud (2013) demonstrated a NPV of 91% for MRI and 100% for CT based on data from 31 patients. Moroder (2013) reported a NPV of 73.8% for MRI and 66.7% for CT based on data from 48 patients. Oh (2010) presented a NPV of 97% for MRI and 98% for CT based on data from 148 patients.
Accuracy
Three studies reported on accuracy. Khedr (2013) reported an accuracy of 100% for both MRI and CT, based on data from 47 patients. Mahmoud (2013) demonstrated an accuracy of 90.6% for MRI and 100% for CT based on data from 31 patients. Oh (2010) presented an accuracy of 96% for MRI and 90% for CT based on data from 148 patients.
Area under the curve
One study has reported on area under the curve for MRI and CT scansOh (2010) presented an area under the curve of 0.866 (95%CI: 0.684-1.0) for MRI and 0.915 (95%CI: 0.83-1.0) for CT based on data from 148 patients.
(Significant) Glenoid fracture/bone loss
Three studies reported glenoid fracture/bone loss, and one study by Moroder (2013) reported significant glenoid defect which was defined as defect >=20% of the glenoid width.
Specificity
Four studies have reported on specificity for MRI and CT scans. Acid (2012) demonstrated a specificity of 100% for MRI and 96% for CT based on data from 40 patients. Khedr (2013) reported a specificity of 97.5% for MRI and 100% for CT based on data from 47 patients. Sgroi (2022) presented a specificity of 63% (95%CI: 45-80%) for MRI and 69% (95%CI: 50-83%) for CT. Moroder (2013) demonstrated a specificity of 100% for both MRI and CT, based on data from 48 patients.
PPV
Four studies have reported on PPV for MRI and CT scans. Acid (2012) demonstrated a PPV of 100% for MRI and 92% for CT based on data from 40 patients. Khedr (2013) reported a PPV of 83.3% for MRI and 100% for CT based on data from 47 patients. Sgroi (2022) presented a PPV of 59% (95%CI: 47-70%) for MRI and 61% (95%CI: 48-73%) for CT. Moroder (2013) demonstrated a PPV of 100% for both MRI and CT, based on data from 48 patients.
Sensitivity
Four studies have reported on sensitivity for MRI and CT scans. Acid (2012) demonstrated a sensitivity of 67% for MRI and 100% for CT based on data from 40 patients. Khedr (2013) reported a sensitivity of 71.4% for MRI and 100% for CT based on data from 47 patients. Sgroi (2022) presented a sensitivity of 94% (95%CI: 71-99%) for MRI and 89% (95%CI: 65-98%) for CT. Moroder (2013) reported a sensitivity of 35.3% for MRI and 100% for CT, based on data from 48 patients.
NPV
Four studies have reported on NPV for MRI and CT scans. Acid (2012) demonstrated a NPV of 87% for MRI and 100% for CT based on data from 40 patients. Khedr (2013) reported a NPV of 95.2% for MRI and 100% for CT based on data from 47 patients. Sgroi (2022) presented a NPV of 95% (95%CI: 74-99%) for MRI and 91% (95%CI: 74-97%) for CT. Moroder (2013) reported a NPV of 73.8% for MRI and 100% for CT, based on data from 48 patients.
Accuracy
Two studies have reported on accuracy for MRI and CT scans. Khedr (2013) reported an accuracy of 95.7% for MRI and 100% for CT based on data from 47 patients. Sgroi (2022) presented an accuracy of 74% (95%CI: 60-86%) for MRI and 76% (95%CI: 61-86%) for CT.
Area under the curve
One study has reported on area under the curve for MRI and CT scans. Sgroi (2022) presented an area under the curve of 0.83 (95%CI: 0.70-0.94) for MRI and 0.79 (95%CI: 0.66-0.92) for CT.
Table 2. Overview of the diagnostic accuracy per outcome
Abbreviations: n.a.: not available. PPV: positive predictive value. NPV: negative predictive value. AUROC: Area Under the Receiving Operator Characteristic Curve
Level of evidence of the literature
Humeral fracture/bone loss
Specificity
The level of evidence regarding specificity was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ or ‘unclear’ in more than half of the domains) and the number of included patients (1 level for imprecision: the number of included patients is low and no confidence interval is provided); Publication bias was not assessed.
PPV
The level of evidence regarding PPV was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ or ‘unclear’ in more than half of the domains) and the number of included patients (1 level for imprecision: the number of included patients is low and no confidence interval is provided); Publication bias was not assessed.
Sensitivity
The level of evidence regarding sensitivity was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ or ‘unclear’ in more than half of the domains) and the number of included patients (1 level for imprecision: the number of included patients is low and no confidence interval is provided); Publication bias was not assessed.
NPV
The level of evidence regarding NPV was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ or ‘unclear’ in more than half of the domains) and the number of included patients (1 level for imprecision: the number of included patients is low and no confidence interval is provided); Publication bias was not assessed.
Accuracy
The level of evidence regarding accuracy was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ or ‘unclear’ in more than half of the domains) and the number of included patients (1 level for imprecision: the number of included patients is very low, and no confidence interval is provided); Publication bias was not assessed.
Area under the curve
The level of evidence regarding accuracy was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ or ‘unclear’ in more than half of the domains) and the number of included patients (1 level for imprecision: the number of included patients is very low, and no confidence interval is provided); Publication bias was not assessed.
Glenoid fracture/bone loss
Specificity
The level of evidence regarding specificity was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ in the domain of reference standard in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is low, and no confidence is interval provided); Publication bias was not assessed.
PPV
The level of evidence regarding PPV was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ in the domain of reference standard in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is low, and no confidence interval is provided); Publication bias was not assessed.
Sensitivity
The level of evidence regarding sensitivity was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ in the domain of reference standard in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is low, and no confidence interval is provided); Publication bias was not assessed.
NPV
The level of evidence regarding NPV was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ in the domain of reference standard in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is low, and no confidence interval is provided); Publication bias was not assessed.
Accuracy
The level of evidence regarding accuracy was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ in the domain of reference standard in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is low, and no confidence interval is provided); Publication bias was not assessed.
Area under the curve
The level of evidence regarding area under the curve was downgraded by 2 levels because of the study limitations (1 level for risk of bias: judgements were ‘high’ in the domain of reference standard in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is very low); Publication bias was not assessed.
Significant glenoid defect (defect >=20% of the glenoid width)
Specificity
The level of evidence regarding specificity was downgraded by 3 levels because of the study limitations (2 levels for risk of bias: judgements were ‘high’ in two domains in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is very low, and no confidence interval is provided); Publication bias was not assessed.
PPV
The level of evidence regarding PPV was downgraded by 3 levels because of the study limitations (2 levels for risk of bias: judgements were ‘high’ in two domains in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is very low, and no confidence interval is provided); Publication bias was not assessed.
Sensitivity
The level of evidence regarding sensitivity was downgraded by 3 levels because of the study limitations (2 levels for risk of bias: judgements were ‘high’ in two domains in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is very low, and no confidence interval is provided); Publication bias was not assessed.
NPV
The level of evidence regarding NPV was downgraded by 3 levels because of the study limitations (2 levels for risk of bias: judgements were ‘high’ in two domains in the risk of bias assessment) and the number of included patients (1 level for imprecision: the number of included patients is very low, and no confidence interval is provided); Publication bias was not assessed.
Accuracy
The accuracy was not reported and therefore a GRADE assessment could not be performed.
Area under the curve
The area under the curve was not reported and therefore a GRADE assessment could not be performed.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
‘’What is the diagnostic accuracy of MRI compared to CT in patients with suspected post-traumatic shoulder instability (osseous component) to determine the presence of glenoid and humeral bone loss?’’
Table 1. PICRO
| Patients | Patients with suspicion of osseous component post-traumatic shoulder instability based on history, physical examination and X-ray |
| Indextest | MRI (a, 2D, 3D) |
| Comparator | CT |
| Reference | Arthroscopy/open surgery |
| Outcomes | Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy (correct results/all results), diagnostic odds ratio, positive likelihood ratio, negative likelihood ratio, and area under the curve (AUC) |
Relevant outcome measures
The guideline development group considered specificity and PPV as critical outcome measures for decision making; and sensitivity, NPV, AUC, accuracy, diagnostic odds ratio, positive likelihood ratio, negative likelihood ratio, and AUC as important outcome measures for decision making.
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms since 2000 until February 6, 2024. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 960 hits. Studies were selected based on the following criteria: the population were patients with suspicion of osseous component post-traumatic shoulder instability, the patients underwent both MRI and CT tests, the reference standard was assessed, the diagnostic accuracy was reported.
Thirty-eight studies were initially selected based on title and abstract screening. After reading the full text, 32 studies were excluded (see the table with reasons for exclusion under the tab Methods), and six studies were included.
Results
Six studies were included in the analysis of the literature. Important study characteristics and results are summarized in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
Referenties
- Acid S, Le Corroller T, Aswad R, Pauly V, Champsaur P. Preoperative imaging of anterior shoulder instability: diagnostic effectiveness of MDCT arthrography and comparison with MR arthrography and arthroscopy. American Journal of Roentgenology. 2012 Mar;198(3):661-7.
- Bishop JY, Jones GL, Rerko MA, Donaldson C; MOON Shoulder Group. 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss. Clin Orthop Relat Res. 2013 Apr;471(4):1251-6. doi: 10.1007/s11999-012-2607-x. Epub 2012 Sep 21. PMID: 22996361; PMCID: PMC3585993.
- Khedr SA, Kassem HM, Azab MA. Comparative study of direct MR arthrography and CT arthrography with arthroscopic correlation in preoperative evaluation of anterior shoulder instability. The Egyptian Journal of Radiology and Nuclear Medicine. 2013 Dec 1;44(4):817-27.
- Mahmoud MK, Badran YM, Zaki HG, Ali AH. One-shot MR and MDCT arthrography of shoulder lesions with arthroscopic correlation. The Egyptian Journal of Radiology and Nuclear Medicine. 2013 Jun 1;44(2):273-81.
- Moroder P, Resch H, Schnaitmann S, Hoffelner T, Tauber M. The importance of CT for the pre-operative surgical planning in recurrent anterior shoulder instability. Archives of orthopaedic and trauma surgery. 2013 Feb;133:219-26.
- Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. Journal of shoulder and elbow surgery. 2010 Jan 1;19(1):14-20.
- Rerko MA, Pan X, Donaldson C, Jones GL, Bishop JY. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elbow Surg. 2013 Apr;22(4):528-34. doi: 10.1016/j.jse.2012.05.034. Epub 2012 Jun 27. PMID: 22748926.
- Sgroi M, Huzurudin H, Ludwig M, Zippelius T, Reichel H, Kappe T. MRI allows accurate measurement of glenoid bone loss. Clinical Orthopaedics and Related Research®. 2022 Sep 1;480(9):1731-42.
- Smith TO, Drew BT, Toms AP. A meta-analysis of the diagnostic test accuracy of MRA and MRI for the detection of glenoid labral injury. Arch Orthop Trauma Surg. 2012 Jul;132(7):905-19. doi: 10.1007/s00402-012-1493-8. Epub 2012 Mar 7. PMID: 22395821.
- Walter WR, Samim M, LaPolla FWZ, Gyftopoulos S. Imaging Quantification of Glenoid Bone Loss in Patients With Glenohumeral Instability: A Systematic Review. AJR Am J Roentgenol. 2019 May;212(5):1096-1105. doi: 10.2214/AJR.18.20504. Epub 2019 Mar 5. PMID: 30835517.
Evidence tabellen
Abbreviations: Sens, sensitivity; Spec, specificity; PPV, positive predictive value; NPV, negative predictive value; Accu, accuracy; AUROC, area under receiver operating characteristic curve.
[1] In geval van een case-control design moeten de patiëntkarakteristieken per groep (cases en controls) worden uitgewerkt. NB; case control studies zullen de accuratesse overschatten (Lijmer et al., 1999)
[2] Comparator test is vergelijkbaar met de C uit de PICO van een interventievraag. Er kunnen ook meerdere tests worden vergeleken. Voeg die toe als comparator test 2 etc. Let op: de comparator test kan nooit de referentiestandaard zijn.
[3] De referentiestandaard is de test waarmee definitief wordt aangetoond of iemand al dan niet ziek is. Idealiter is de referentiestandaard de Gouden standaard (100% sensitief en 100% specifiek). Let op! dit is niet de “comparison test/index 2”.
Risk of bias assessment diagnostic accuracy studies (QUADAS II, 2011)
|
Study reference |
Patient selection
|
Index test |
Reference standard |
Flow and timing |
Comments with respect to applicability |
|
Acid, 2012 |
Was a consecutive or random sample of patients enrolled? Unclear (patients were prospectively enrolled, further no explanation)
Was a case-control design avoided? Yes
Did the study avoid inappropriate exclusions? Yes
|
Were the index test results interpreted without knowledge of the results of the reference standard? Yes
If a threshold was used, was it pre-specified? Thresholds were not defined. The criteria for the diagnoses were pre-described.
|
Is the reference standard likely to correctly classify the target condition? Yes
Were the reference standard results interpreted without knowledge of the results of the index test? No (During arthroscopy, MDCT arthrography and MR arthrography images on film hard copy were available to the surgeon.)
|
Was there an appropriate interval between index test(s) and reference standard? Yes (<1 month)
Did all patients receive a reference standard? Yes (one of the inclusion criteria)
Did patients receive the same reference standard? Yes
Were all patients included in the analysis? Probably yes |
Are there concerns that the included patients do not match the review question? No
Are there concerns that the index test, its conduct, or interpretation differ from the review question? No
Are there concerns that the target condition as defined by the reference standard does not match the review question? No |
|
CONCLUSION: Could the selection of patients have introduced bias?
RISK: UNCLEAR |
CONCLUSION: Could the conduct or interpretation of the index test have introduced bias?
RISK: LOW |
CONCLUSION: Could the reference standard, its conduct, or its interpretation have introduced bias?
RISK: HIGH |
CONCLUSION Could the patient flow have introduced bias?
RISK: LOW |
|
|
|
Khedr, 2013 |
Was a consecutive or random sample of patients enrolled? Unclear (patients were prospectively enrolled, further no explanation)
Was a case-control design avoided? Yes Did the study avoid inappropriate exclusions? Yes
|
Were the index test results interpreted without knowledge of the results of the reference standard? Yes
If a threshold was used, was it pre-specified? Thresholds were not defined. The criteria for the diagnoses were pre-described.
|
Is the reference standard likely to correctly classify the target condition? Yes
Were the reference standard results interpreted without knowledge of the results of the index test? No (During arthroscopy, MDCT arthrography and MR arthrography images on film hard copy were available to the surgeon.)
|
Was there an appropriate interval between index test(s) and reference standard? Yes (<1 month)
Did all patients receive a reference standard? Yes (one of the inclusion criteria)
Did patients receive the same reference standard? Yes
Were all patients included in the analysis? Probably yes |
Are there concerns that the included patients do not match the review question? No
Are there concerns that the index test, its conduct, or interpretation differ from the review question? No
Are there concerns that the target condition as defined by the reference standard does not match the review question? No |
|
|
CONCLUSION: Could the selection of patients have introduced bias?
RISK: UNCLEAR |
CONCLUSION: Could the conduct or interpretation of the index test have introduced bias?
RISK: LOW |
CONCLUSION: Could the reference standard, its conduct, or its interpretation have introduced bias?
RISK: HIGH |
CONCLUSION Could the patient flow have introduced bias?
RISK: LOW |
|
|
Mahmoud, 2013 |
Was a consecutive or random sample of patients enrolled? Yes (consecutive)
Was a case-control design avoided? Yes
Did the study avoid inappropriate exclusions? Yes
|
Were the index test results interpreted without knowledge of the results of the reference standard? Yes
If a threshold was used, was it pre-specified? Thresholds were not defined. The criteria for the diagnoses were pre-described.
|
Is the reference standard likely to correctly classify the target condition? Yes
Were the reference standard results interpreted without knowledge of the results of the index test? Unclear (Unknown whether the MRI/CT results were blinded to the surgeon who the arthroscopy performed)
|
Was there an appropriate interval between index test(s) and reference standard? Yes (<100 days, longer than other studies, unclear whether this might influence the diagnosis since it is a maximal time range)
Did all patients receive a reference standard? Yes
Did patients receive the same reference standard? Unclear (No description about under which standard the arthroscopy was performed) Were all patients included in the analysis? Yes |
Are there concerns that the included patients do not match the review question? No
Are there concerns that the index test, its conduct, or interpretation differ from the review question? No
Are there concerns that the target condition as defined by the reference standard does not match the review question? No |
|
|
CONCLUSION: Could the selection of patients have introduced bias?
RISK: LOW |
CONCLUSION: Could the conduct or interpretation of the index test have introduced bias?
RISK: LOW |
CONCLUSION: Could the reference standard, its conduct, or its interpretation have introduced bias?
RISK: UNCLEAR |
CONCLUSION Could the patient flow have introduced bias?
RISK: UNCLEAR |
|
|
Moroder, 2013 |
Was a consecutive or random sample of patients enrolled? No (only patients with complete pre-operative MRI from other physicians and CT-scans were included, 48/83 due to incompleteness of MRI or CT) Was a case-control design avoided? Yes
Did the study avoid inappropriate exclusions? Yes
|
Were the index test results interpreted without knowledge of the results of the reference standard? No (The index tests were retrospectively evaluated. All available MRIs and CT-scans were re-evaluated for study purposes in a blinded fashion by the same musculoskeletal radiologist. Pathological findings were listed and compared with the intra-operatively described pathomorphological findings documented on the surgical report.)
If a threshold was used, was it pre-specified? Thresholds were not defined.
|
Is the reference standard likely to correctly classify the target condition? Yes
Were the reference standard results interpreted without knowledge of the results of the index test? Unclear (Not specifically described. However, the information from MRI and CI were used for the planning of the open surgery)
|
Was there an appropriate interval between index test(s) and reference standard? Unclear (Not described, MRI reports were from other physicians apart from the research institution; MRI and CT were retrospectively evaluated)
Did all patients receive a reference standard? Yes
Did patients receive the same reference standard? Yes
Were all patients included in the analysis? Probably yes |
Are there concerns that the included patients do not match the review question? Yes (All patients included in the analysis underwent surgical stabilization, among who the incidence of the outcomes might be higher than other diagnostic studies)
Are there concerns that the index test, its conduct, or interpretation differ from the review question? Yes (MRI and CT were retrospectively evaluated after the surgery, and it was unclear whether the information from the index text were interpreted without the knowledge of the reference test, also the other way around) Are there concerns that the target condition as defined by the reference standard does not match the review question? Yes (open surgery was chosen over arthroscopy as the reference standard) |
|
CONCLUSION: Could the selection of patients have introduced bias?
RISK: UNCLEAR |
CONCLUSION: Could the conduct or interpretation of the index test have introduced bias?
RISK: HIGH |
CONCLUSION: Could the reference standard, its conduct, or its interpretation have introduced bias?
RISK: UNCLEAR |
CONCLUSION Could the patient flow have introduced bias?
RISK: UNCLEAR |
|
|
|
Oh, 2010 |
Was a consecutive or random sample of patients enrolled? Yes (consecutive. The present study ultimately enrolled 148 patients, of whom 78 were randomly referred for CTA and 70 patients for MRA. Patients were randomly selected to perform CT or MRI, but in Table 1 differences in patient characteristics are clearly shown)
Was a case-control design avoided? No (The present study ultimately enrolled 148 patients, of whom 78 were randomly referred for CTA and 70 patients for MRA.)
Did the study avoid inappropriate exclusions? Yes |
Were the index test results interpreted without knowledge of the results of the reference standard? Yes
If a threshold was used, was it pre-specified? Thresholds were not defined. The criteria for the diagnoses were not pre-described in detail. Whether this would have an influence on the results is not clear.
|
Is the reference standard likely to correctly classify the target condition? Yes
Were the reference standard results interpreted without knowledge of the results of the index test? Unclear (Unknown whether the MRI/CT results were blinded to the surgeon who the arthroscopy performed)
|
Was there an appropriate interval between index test(s) and reference standard? Yes (<100 days, longer than other studies, unclear whether this might influence the diagnosis since it is a maximal time range)
Did all patients receive a reference standard? Yes
Did patients receive the same reference standard? Unclear (No description about under which standard the arthroscopy was performed)
Were all patients included in the analysis? Probably yes |
Are there concerns that the included patients do not match the review question? Yes (Patients were randomly selected to perform CT or MRI, but in Table 1 differences in patient characteristics are clearly shown)
Are there concerns that the index test, its conduct, or interpretation differ from the review question? No
Are there concerns that the target condition as defined by the reference standard does not match the review question? No |
|
CONCLUSION: Could the selection of patients have introduced bias?
RISK: HIGH |
CONCLUSION: Could the conduct or interpretation of the index test have introduced bias?
RISK: UNCLEAR |
CONCLUSION: Could the reference standard, its conduct, or its interpretation have introduced bias?
RISK: UNCLEAR |
CONCLUSION Could the patient flow have introduced bias?
RISK: UNCLEAR |
|
|
|
Sgroi, 2022 |
Was a consecutive or random sample of patients enrolled? No (only patients with available preoperative AP radiographs, WP radiographs, CT, and MR images of the affected shoulder as potentially eligible.)
Was a case-control design avoided? Yes
Did the study avoid inappropriate exclusions? Yes
|
Were the index test results interpreted without knowledge of the results of the reference standard? Unclear (The assessment was perioperatively performed and postoperatively analysed. During the analyzation, all imaging modalities were anonymized, but it is unclear whether it was blinded to the results from the arthroscopies.)
If a threshold was used, was it pre-specified? Thresholds were not defined. The diagnosis focused on glenoid bone loss.
|
Is the reference standard likely to correctly classify the target condition? Yes
Were the reference standard results interpreted without knowledge of the results of the index test? No (The surgical indication was based on patient history, clinical examination, and it was MRI-confirmed. All analysed patients had clinically relevant anterior shoulder instability after at least one shoulder dislocation, and all patients were diagnosed with at least anterior labral Bankart lesion by MRI.)
|
Was there an appropriate interval between index test(s) and reference standard? Unclear (No description about the interval between the preoperative assessment and the arthroscopies.) Did all patients receive a reference standard? Yes
Did patients receive the same reference standard? Yes
Were all patients included in the analysis? No (Not all planes or layers (such as sagittal, axial, or frontal) of each diagnostic imaging modalities were available and 6% (5 of 80) because of the insufficient quality of diagnostic images (for example, setting of the layers did not allow adequate en face view of the glenoid. The effect on the results is unclear). |
Are there concerns that the included patients do not match the review question? Yes (All analyzed patients had clinically relevant anterior shoulder instability after at least one shoulder dislocation, and all patients were diagnosed with at least anterior labral Bankart lesion by MRI.)
Are there concerns that the index test, its conduct, or interpretation differ from the review question? Unclear (The index tests were shortly described)
Are there concerns that the target condition as defined by the reference standard does not match the review question? No
|
|
CONCLUSION: Could the selection of patients have introduced bias?
RISK: UNCLEAR |
CONCLUSION: Could the conduct or interpretation of the index test have introduced bias?
RISK: UNCLEAR |
CONCLUSION: Could the reference standard, its conduct, or its interpretation have introduced bias?
RISK: HIGH |
CONCLUSION Could the patient flow have introduced bias?
RISK: UNCLEAR |
|
Judgments on risk of bias are dependent on the research question: some items are more likely to introduce bias than others, and may be given more weight in the final conclusion on the overall risk of bias per domain:
1. Patient selection:
- Consecutive or random sample has a low risk to introduce bias.
- A case control design is very likely to overestimate accuracy and thus introduce bias.
- Inappropriate exclusion is likely to introduce bias.
2. Index test:
- This item is similar to “blinding” in intervention studies. The potential for bias is related to the subjectivity of index test interpretation and the order of testing.
- Selecting the test threshold to optimise sensitivity and/or specificity may lead to overoptimistic estimates of test performance and introduce bias.
3. Reference standard:
- When the reference standard is not 100% sensitive and 100% specific, disagreements between the index test and reference standard may be incorrect, which increases the risk of bias.
- This item is similar to “blinding” in intervention studies. The potential for bias is related to the subjectivity of index test interpretation and the order of testing.
4. Flow and timing:
- If there is a delay or if treatment is started between index test and reference standard, misclassification may occur due to recovery or deterioration of the condition, which increases the risk of bias.
- If the results of the index test influence the decision on whether to perform the reference standard or which reference standard is used, estimated diagnostic accuracy may be biased.
- All patients who were recruited into the study should be included in the analysis, if not, the risk of bias is increased.
Judgement on applicability:
1. Patient selection: there may be concerns regarding applicability if patients included in the study differ from those targeted by the review question, in terms of severity of the target condition, demographic features, presence of differential diagnosis or co-morbidity, setting of the study and previous testing protocols.
2. Index test: if index tests methods differ from those specified in the review question there may be concerns regarding applicability.
3. Reference standard: the reference standard may be free of bias but the target condition that it defines may differ from the target condition specified in the review question.
List of excluded studies
|
Reference |
Reason for exclusion |
|
3-D CT is the most reliable imaging modality when quantifying glenoid bone loss shoulder |
Wrong outcome |
|
Zero echo time imaging of the shoulder: Enhanced osseous detail by using MR imaging |
Wrong outcome |
|
Does Bone Loss Imaging Modality, Measurement Methodology, and Interobserver Reliability Alter Treatment in Glenohumeral Instability? |
Wrong outcome |
|
3D-MRI FRACTURE Sequence is equivalent to 3D-CT in quantifying bone loss and measuring shoulder morphology in patients with shoulder dislocation |
Wrong outcome |
|
Three-Dimensional Zero Echo Time Magnetic Resonance Imaging Versus 3-Dimensional Computed Tomography for Glenoid Bone Assessment |
Wrong outcome |
|
Shoulder joint instability evaluation by CT arthrography and MR arthro graphy |
Wrong outcome |
|
Assessment of glenoid bone loss and other osseous shoulder pathologies comparing MR-based CT-like images with conventional CT |
Wrong outcome |
|
Glenoid bone loss measurement in recurrent shoulder dislocation: Assessment of measurement agreement between CT and MRI |
Wrong outcome |
|
Diagnostic accuracy of MRI in the measurement of glenoid bone loss |
Wrong outcome |
|
3DMR osseous reconstructions of the shoulder using a gradient-echo based two-point Dixon reconstruction: A feasibility study |
Wrong outcome |
|
Use of 3D MR reconstructions in the evaluation of glenoid bone loss: A clinical study |
Wrong outcome |
|
Quantification of a glenoid defect with three-dimensional computed tomography and magnetic resonance imaging: a cadaveric study |
Wrong outcome |
|
Variability in quantifying the Hill-Sachs lesion: A scoping review |
Wrong study design; unclear study population |
|
A PROSPECTIVE STUDY TO ASSESS THE ROLE OF MAGNETIC RESONANCE IMAGING IN ASSESSING GLENOID BONE LOSS IN SHOULDER DISLOCATION |
Wrong outcome |
|
Comparison of computed tomography and 3D magnetic resonance imaging in evaluating glenohumeral instability bone loss |
Wrong outcome |
|
Automated 3-Dimensional Magnetic Resonance Imaging Allows for Accurate Evaluation of Glenoid Bone Loss Compared With 3-Dimensional Computed Tomography |
Wrong outcome |
|
Glenoid bone loss: Assessment with MR imaging |
Wrong outcome |
|
Feasibility of using an inversion-recovery ultrashort echo time (UTE) sequence for quantification of glenoid bone loss |
Wrong outcome |
|
How to measure a Hill-Sachs lesion: A systematic review |
Unclear study population |
|
The quantification of glenoid bone loss in anterior shoulder instability; MR-arthro compared to 3D-CT |
Wrong outcome |
|
Area Measurement Percentile of 3-Dimensional Computed Tomography Has the Highest Interobserver Reliability When Measuring Anterior Glenoid Bone Loss |
Wrong outcome |
|
Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability |
Wrong outcome |
|
With the exception of the Hill-Sachs interval, CT and MRI show no significant differences in the diagnostic value of the HSL measurement regardless of the measurement technique |
Wrong outcome |
|
MRI can assess glenoid bone loss after shoulder luxation: inter- and intra-individual comparison with CT |
Wrong outcome |
|
3D-MR vs. 3D-CT of the shoulder in patients with glenohumeral instability |
Wrong outcome |
|
Glenoid bone lesions: Comparison between 3D VIBE images in MR arthrography and nonarthrographic MSCT |
Wrong outcome |
|
Measurement of Glenoid Bone Loss With 3-Dimensional Magnetic Resonance Imaging: A Matched Computed Tomography Analysis |
Wrong outcome |
|
Glenoid bone loss in shoulder instability: Superiority of three-dimensional computed tomography over two-dimensional magnetic resonance imaging using established methodology |
Wrong outcome |
|
A Comparative Study on the Diagnostic Value of CTA and MRA in Anterior Dislocation of Shoulder |
Wrong outcome |
|
Three-Dimensional Magnetic Resonance Imaging Quantification of Glenoid Bone Loss Is Equivalent to 3-Dimensional Computed Tomography Quantification: Cadaveric Study |
Wrong outcome |
|
Glenoid bone loss in anterior shoulder dislocation: a multicentric study to assess the most reliable imaging method |
Wrong outcome |
|
Comparison of magnetic resonance imaging and computed tomography scans of the glenoid version in anterior dislocation of the shoulder |
Wrong outcome |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 17-02-2026
Beoordeeld op geldigheid : 17-02-2026
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd door de Stichting Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodules is in 2022 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met schouderinstabiliteit.
Werkgroep richtlijn schouderinstabiliteit
- Prof. Dr. M.P.J (Michel) Bekerom, orthopedisch chirurg OLVG en MC Jan van Gooijen, NOV – voorzitter richtlijnwerkgroep
- Dr. J.J.A.M. (Jos) van Raaij, orthopedisch chirurg, niet praktiserend, NOV
- Dr. O.A.J. (Olivier) van der Meijden, orthopedisch chirurg Albert Schweitzer Ziekenhuis, NOV
- Dr. A.R. (Alex) Poublon, orthopedisch chirurg Ziekenhuis Gelderse Vallei, NOV
- Dr. T.D.W. (Tjarco) Alta, orthopedisch chirurg Spaarne Gasthuis, NOV
- Dr. R.J. (Robert Jan) Derksen, traumachirurg, Zaans Medisch Centrum, NVvH
- MSc. F. (Femke) Boon, fysio-, manueel therapeut, extended scope specialist Schoudercentrum IBC, KNGF
- MSc. K.M.C. (Karin) Hekman, fysio-, manueel therapeut, extended scope specialist, Schoudercentrum IBC, KNGF
- Dr. I.D. (Iris) Kilsdonk, radioloog Deventer Ziekenhuis, NVvR
- Dr. H.J. (Henk-Jan) van der Woude, radioloog OLVG, NVvR
- Drs. H.K. (Rik) van der Kolk, sportarts OLVG, VSG
- Mevr. drs. G. (Gerardine) Willemsen-de Mey, patiëntvertegenwoordiger Nationale Vereniging ReumaZorg Nederland
Met ondersteuning van
- Dr. J. (Jacqueline) Jennen, adviseur Kennisinstituut van de Federatie Medisch Specialisten (tot december 2023)
- Dr. F. (Floor) Willeboordse, senior adviseur Kennisinstituut van de Federatie Medisch Speciaisten (tot januari 2025)
- Dr. M.S. (Matthijs) Ruiter, senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten (vanaf januari 2025)
- MSc. D.G. (Dian) Ossendrijver, adviseur kennisinstituut van de Federatie Medisch Specialisten (vanaf december 2023)
- Dr. M. (Michiel) Oerbekke, adviseur Kennisinstituut van de Federatie Medisch Specialisten
- Dr. J. (Jing) de Haan-Du, adviseur Kennisinstituut van de Federatie Medisch Specialisten
- E. (Esther) van Bijl, medisch informatiespecialist, kennisinstituut van de Federatie Medisch Specialisten
Belangenverklaringen
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten via secretariaat@kennisinstituut.nl.
Gemelde (neven)functies en belangen werkgroep
|
Naam |
Hoofdfunctie |
Neven werkzaamheden |
Persoonlijke financiële belangen |
Persoonlijke relaties |
Extern gefinancierd onderzoek |
Intellectuele belangen en reputatie |
Overige belangen |
Datum |
Restrictie |
|
Michel van den Bekerom (voorzitter) |
Orthopedisch chirurg, OLVG, Amsterdam |
Betaald onderwijs geven bij/voor: |
Geen |
Geen |
Onderzoek gesteund door: SECEC (European Society for surgery of the shoulder an the elbow), ZonMW, SNN (Smith and Nephew). Het OLVG ontvangt financiële support voor een shoulder and elbow clinical and research fellowship van van Smith en Nephew. Dit fellowship wordt mede (financieel) ondersteund door een firma die materiaal maakt dat gebruikt wordt voor schouderstabilisaties. Het betreft een overeenkomst tussen het OLVG en de firma vanwege educatieve doeleinden. |
Geen |
Het OLVG is voornemens om een consultancy contract met zimmer/biomet op te stellen zodat ik op vraag elders kan opereren. |
19-10-2022 |
Geen restricties
|
|
Jos van Raaij |
Orthopedisch chirurg, Martini ziekenhuis Groningen |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
11-07-2022 |
Geen restricties |
|
Olivier van der Meijden |
Orthopedisch chirurg |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
28-09-2023 |
Geen restricties |
|
Alexander Poublon |
Orthopedisch chirurg met aandachtsgebied schouder |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
06-10-2023 |
Geen restricties |
|
Tjarco Alta |
Orthopedisch Chirurg |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
28-09-2023 |
Geen restricties |
|
Karin Hekman |
Fysiotherapeut bij Schoudercentrum IBC |
Voorzitter Schoudernetwerk Nederland; onkostenvergoeding |
Ik behandel patiënten die schouderinstabiliteit hebben binnen het schoudercentrum en binnen MC Jan van Goyen, dit is de reden voor het plaatsnemen in deze expertise groep. |
Geen |
Geen |
Het enige voordeel dat deelname aan deze richtlijn oplevert is nog meer persoonlijke expertise wat mogelijk leidt tot een verdieping van de fysiotherapeutische toepassingen bij schouderinstabiliteit. Dit is voor het SchouderNetwerk Nederland van primair belang en kan leiden tot uitdragen van kennis naar de regionale netwerken. Als voorzitter van deze stichting voel ik mij hier verantwoordelijk voor. |
Geen |
09-10-2023 |
Geen restricties |
|
Femke Boon |
Fysio- manueel therapeut en Extended Scope specialist bij Schoudercentrum IBC locatie Amstelland |
- 2x/ maand elleboog-schouder orthopedie poli bij Medisch Centrum Jan van Goyen (betaald, gedetacheerd vanuit IBC) |
Werkzaam bij Schoudercentrum IBC Amstelland |
Geen |
Richtlijn ontwikkeling FMS primaire anterieure schouderluxaties |
Geen |
Geen |
4-10-2023 |
Geen restricties |
|
Iris Kilsdonk |
Deventer Ziekenhuis |
Bestuurslid NVvR, sectie muskuloskeletale radiologie |
Geen |
Geen |
Geen |
Geen |
Geen |
2-10-2023 |
Geen restricties |
|
Robert Jan Derksen |
Traumachirurg Zaans Medisch Centrum |
Bestuurslid NVT |
Geen |
Geen |
Geen |
Geen |
Geen |
28-08-2022 |
Geen restricties |
|
Rik van der Kolk |
Sportarts, OLVG |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
10-08-2022 |
Geen restricties |
|
Henk-Jan van der Woude |
Radioloog Onze Lieve Vrouwe Gasthuis Amsterdam |
Consulent Commissie voor Beentumoren, onbezoldigd |
Geen |
Geen |
Geen |
Geen |
Geen |
07-02-2023 |
Geen restricties |
Inbreng patiëntenperspectief
De werkgroep besteedde aandacht aan het patiëntenperspectief door het uitnodigen van de Patiëntenfederatie Nederland en de Nationale Vereniging ReumaZorg Nederland voor de knelpunteninventarisatie. Daarnaast nam een patiëntvertegenwoordiger van ReumaZorg Nederland deel aan de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voor commentaar voorgelegd aan Patiëntenfederatie Nederland en ReumaZorg Nederland en de eventueel aangeleverde commentaren zijn bekeken en verwerkt
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijnmodule voerde de werkgroep conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uit om te beoordelen of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling is de richtlijnmodule op verschillende domeinen getoetst (zie het stroomschema bij Werkwijze).
|
Module |
Uitkomst raming |
Toelichting |
|
Beeldvorming MRI of CT |
Geen financiële gevolgen |
Uit de toetsing volgt dat de aanbeveling(en) niet breed toepasbaar zijn (<5.000 patiënten) en zal daarom naar verwachting geen substantiële financiële gevolgen hebben voor de collectieve uitgaven.
|
Werkwijze
Voor meer details over de gebruikte richtlijnmethodologie verwijzen wij u naar de Werkwijze. Relevante informatie voor de ontwikkeling van deze richtlijn is hieronder weergegeven.
Zoekverantwoording
Algemene informatie
|
Cluster/richtlijn: Schouderinstabiliteit - Module 2 Posttraumatische schouderinstabiliteit |
|
|
Uitgangsvraag/modules: Welk (aanvullend?) beeldvormend onderzoek moet worden verricht bij post traumatische schouderinstabiliteit? |
|
|
Database(s): Embase.com, Ovid/Medline |
Datum: 6-2-2024 |
|
Periode: vanaf 2000 |
Talen: geen restrictie |
|
Literatuurspecialist: Esther van der Bijl |
Rayyan review: https://rayyan.ai/reviews/922035 |
|
BMI-zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting: Voor deze vraag is gezocht op de elementen Schouderinstabiliteit en MRI.
à De sleutelartikelen PMID 22996361, PMID 18061117 en PMID 35452020 worden gevonden met deze search.
Zoals besproken is er gezocht met de P, I en het diagnostisch filter. In overleg zijn bij de P ook de zoektermen ‘glenoid bone loss’ en ‘glenoid defect’ meegenomen, omdat anders relevante artikelen gemist worden. |
|
|
Te gebruiken voor richtlijntekst: In de databases Embase.com en Ovid/Medline is op 6 februari 2024 systematisch gezocht naar systematische reviews, RCTs en observationele studies over de diagnostische accuratesse van MRI bij patiënten met verdenking op posttraumatische schouderinstabiliteit (ossale component). De literatuurzoekactie leverde 960 unieke treffers op. |
|
Zoekopbrengst - 6 februari 2024
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SR |
80 |
11 |
83 |
|
RCT |
199 |
30 |
210 |
|
Observationeel |
633 |
206 |
667 |
|
Totaal |
912 |
247 |
960* |
*in Rayyan
Zoekstrategie - 6 februari 2024
Embase.com
|
No. |
Query |
Results |
|
#1 |
'shoulder dislocation'/exp OR 'recurrent shoulder dislocation'/exp OR 'bankart lesion'/exp OR ((('shoulder*' OR 'gleno-humer*' OR 'glenoid*' OR 'humer*' OR 'scapulohumer*' OR 'glenohumer*') NEAR/3 ('dislocat*' OR 'diastasis' OR 'instabil*' OR 'luxat*' OR 'subluxat*' OR 'defect*')):ti,ab,kw) OR (('shoulder*':ti,ab,kw OR glenoid*:ti,ab,kw OR 'gleno-humer*':ti,ab,kw OR 'humer*':ti,ab,kw OR 'scapulohumer*':ti,ab,kw OR 'glenohumer*':ti,ab,kw) AND (('bon*' NEAR/3 ('loss*' OR 'erosion*')):ti,ab,kw)) OR ((('bankart' OR 'hill-sachs') NEAR/3 ('fracture*' OR 'lesion*' OR 'tear*')):ti,ab,kw) OR ((('on track' OR 'off track') NEAR/3 ('hill sachs' OR 'bone loss*' OR 'shoulder*' OR 'lesion*')):ti,ab,kw) |
17298 |
|
#2 |
'nuclear magnetic resonance imaging'/exp OR 'mri scanner'/exp OR ('magnetic resonance':ab,ti AND (image:ab,ti OR images:ab,ti OR imaging:ab,ti)) OR mri:ab,ti OR mris:ab,ti OR nmr:ab,ti OR mra:ab,ti OR mras:ab,ti OR zeugmatograph*:ab,ti OR 'mr tomography':ab,ti OR 'mr tomographies':ab,ti OR 'mr tomographic':ab,ti OR 'mr imag*':ti,ab,kw OR 'proton spin':ab,ti OR ((magneti*:ab,ti OR 'chemical shift':ab,ti) AND imaging:ab,ti) OR fmri:ab,ti OR fmris:ab,ti OR rsfmri:ti,ab,kw |
1604297 |
|
#3 |
'diagnostic procedure'/exp OR 'sensitivity and specificity'/de OR sensitivity:ab,ti OR specificity:ab,ti OR predict*:ab,ti OR 'roc curve':ab,ti OR 'receiver operator':ab,ti OR 'receiver operators':ab,ti OR likelihood:ab,ti OR 'diagnostic error'/exp OR 'diagnostic accuracy'/exp OR 'diagnostic test accuracy study'/exp OR 'inter observer':ab,ti OR 'intra observer':ab,ti OR interobserver:ab,ti OR intraobserver:ab,ti OR validity:ab,ti OR kappa:ab,ti OR reliability:ab,ti OR reproducibility:ab,ti OR ((test NEAR/2 're-test'):ab,ti) OR ((test NEAR/2 'retest'):ab,ti) OR 'reproducibility'/exp OR accuracy:ab,ti OR 'differential diagnosis'/exp OR 'validation study'/de OR 'measurement precision'/exp OR 'diagnostic value'/exp OR 'reliability'/exp OR 'predictive value'/exp OR ppv:ti,ab,kw OR npv:ti,ab,kw OR (((false OR true) NEAR/3 (negative OR positive)):ti,ab) OR diagnos*:ti,ab |
24669709 |
|
#4 |
#1 AND #2 AND #3 |
2429 |
|
#5 |
#4 AND [2000-2024]/py NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) |
1863 |
|
#6 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
999431 |
|
#7 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
3963976 |
|
#8 |
'major clinical study'/de OR 'clinical study'/de OR 'case control study'/de OR 'family study'/de OR 'longitudinal study'/de OR 'retrospective study'/de OR 'prospective study'/de OR 'comparative study'/de OR 'cohort analysis'/de OR ((cohort NEAR/1 (study OR studies)):ab,ti) OR (('case control' NEAR/1 (study OR studies)):ab,ti) OR (('follow up' NEAR/1 (study OR studies)):ab,ti) OR (observational NEAR/1 (study OR studies)) OR ((epidemiologic NEAR/1 (study OR studies)):ab,ti) OR (('cross sectional' NEAR/1 (study OR studies)):ab,ti) |
8055848 |
|
#9 |
'case control study'/de OR 'comparative study'/exp OR 'control group'/de OR 'controlled study'/de OR 'controlled clinical trial'/de OR 'crossover procedure'/de OR 'double blind procedure'/de OR 'phase 2 clinical trial'/de OR 'phase 3 clinical trial'/de OR 'phase 4 clinical trial'/de OR 'pretest posttest design'/de OR 'pretest posttest control group design'/de OR 'quasi experimental study'/de OR 'single blind procedure'/de OR 'triple blind procedure'/de OR (((control OR controlled) NEAR/6 trial):ti,ab,kw) OR (((control OR controlled) NEAR/6 (study OR studies)):ti,ab,kw) OR (((control OR controlled) NEAR/1 active):ti,ab,kw) OR 'open label*':ti,ab,kw OR (((double OR two OR three OR multi OR trial) NEAR/1 (arm OR arms)):ti,ab,kw) OR ((allocat* NEAR/10 (arm OR arms)):ti,ab,kw) OR placebo*:ti,ab,kw OR 'sham-control*':ti,ab,kw OR (((single OR double OR triple OR assessor) NEAR/1 (blind* OR masked)):ti,ab,kw) OR nonrandom*:ti,ab,kw OR 'non-random*':ti,ab,kw OR 'quasi-experiment*':ti,ab,kw OR crossover:ti,ab,kw OR 'cross over':ti,ab,kw OR 'parallel group*':ti,ab,kw OR 'factorial trial':ti,ab,kw OR ((phase NEAR/5 (study OR trial)):ti,ab,kw) OR ((case* NEAR/6 (matched OR control*)):ti,ab,kw) OR ((match* NEAR/6 (pair OR pairs OR cohort* OR control* OR group* OR healthy OR age OR sex OR gender OR patient* OR subject* OR participant*)):ti,ab,kw) OR ((propensity NEAR/6 (scor* OR match*)):ti,ab,kw) OR versus:ti OR vs:ti OR compar*:ti OR ((compar* NEAR/1 study):ti,ab,kw) OR (('major clinical study'/de OR 'clinical study'/de OR 'cohort analysis'/de OR 'observational study'/de OR 'cross-sectional study'/de OR 'multicenter study'/de OR 'correlational study'/de OR 'follow up'/de OR cohort*:ti,ab,kw OR 'follow up':ti,ab,kw OR followup:ti,ab,kw OR longitudinal*:ti,ab,kw OR prospective*:ti,ab,kw OR retrospective*:ti,ab,kw OR observational*:ti,ab,kw OR 'cross sectional*':ti,ab,kw OR cross?ectional*:ti,ab,kw OR multicent*:ti,ab,kw OR 'multi-cent*':ti,ab,kw OR consecutive*:ti,ab,kw) AND (group:ti,ab,kw OR groups:ti,ab,kw OR subgroup*:ti,ab,kw OR versus:ti,ab,kw OR vs:ti,ab,kw OR compar*:ti,ab,kw OR 'odds ratio*':ab OR 'relative odds':ab OR 'risk ratio*':ab OR 'relative risk*':ab OR 'rate ratio':ab OR aor:ab OR arr:ab OR rrr:ab OR ((('or' OR 'rr') NEAR/6 ci):ab))) |
14796927 |
|
#10 |
#5 AND #6 – SR’s |
80 |
|
#11 |
#5 AND #7 NOT #10 – RCT’s |
199 |
|
#12 |
#5 AND (#8 OR #9) NOT (#10 OR #11) – Observationele studies |
633 |
|
#13 |
#10 OR #11 OR #12 |
912 |
Ovid/Medline
|
# |
Searches |
Results |
|
1 |
exp Shoulder Dislocation/ or exp Bankart Lesions/ or ((shoulder* or gleno-humer* or glenoid* or humer* or scapulohumer* or glenohumer*) adj3 (dislocat* or diastasis or instabil* or luxat* or subluxat* or defect*)).ti,ab,kf. or ((shoulder* or glenoid* or gleno-humer* or humer* or scapulohumer* or glenohumer*) and (bon* adj3 (loss* or erosion*))).ti,ab,kf. or ((bankart or hill-sachs) adj3 (fracture* or lesion* or tear*)).ti,ab,kf. or ((on track or off track) adj3 (hill sachs or bone loss* or shoulder* or lesion*)).ti,ab,kf. |
13706 |
|
2 |
exp magnetic resonance imaging/ or ("magnetic resonance" and (image or images or imaging)).ti,ab,kf. or mri.ti,ab,kf. or mris.ti,ab,kf. or nmr.ti,ab,kf. or mra.ti,ab,kf. or mras.ti,ab,kf. or zeugmatograph*.ti,ab,kf. or "mr tomography".ti,ab,kf. or "mr tomographies".ti,ab,kf. or "mr tomographic".ti,ab,kf. or 'mr imag*'.ti,ab,kf. or "proton spin".ti,ab,kf. or ((magneti* or "chemical shift") and imaging).ti,ab,kf. or fmri.ti,ab,kf. or fmris.ti,ab,kf. or rsfmri.ti,ab,kf. |
981588 |
|
3 |
exp "Sensitivity and Specificity"/ or (sensitivity or specificity).ti,ab. or (predict* or ROC-curve or receiver-operator*).ti,ab. or (likelihood or LR*).ti,ab. or exp Diagnostic Errors/ or (inter-observer or intra-observer or interobserver or intraobserver or validity or kappa or reliability).ti,ab. or reproducibility.ti,ab. or (test adj2 (re-test or retest)).ti,ab. or "Reproducibility of Results"/ or accuracy.ti,ab. or Diagnosis, Differential/ or Validation Study/ or ((false or true) adj3 (negative or positive)).ti,ab. |
5006646 |
|
4 |
1 and 2 and 3 |
408 |
|
5 |
limit 4 to yr="2000 -Current" |
349 |
|
6 |
5 not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
343 |
|
7 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
724616 |
|
8 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2687808 |
|
9 |
Epidemiologic studies/ or case control studies/ or exp cohort studies/ or Controlled Before-After Studies/ or Case control.tw. or cohort.tw. or Cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or Longitudinal.tw. or Retrospective*.tw. or prospective*.tw. or consecutive*.tw. or Cross sectional.tw. or Cross-sectional studies/ or historically controlled study/ or interrupted time series analysis/ [Onder exp cohort studies vallen ook longitudinale, prospectieve en retrospectieve studies] |
4645843 |
|
10 |
Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) |
5616453 |
|
11 |
6 and 7 – SR’s |
11 |
|
12 |
(6 and 8) not 11 – RCT’s |
30 |
|
13 |
(6 and (9 or 10)) not (11 or 12) – Observationele studies |
206 |
|
14 |
11 or 12 or 13 |
247 |