Profylactische nierfunctievervangende therapie tegen PC-AKI
Uitgangsvraag
Dient profylactische nierfuncievervangende therapie te worden aanbevolen bij patiënten met chronisch nierfalen stadium 4-5, die intravasculaire jodiumhoudend contrastmiddel (CM) toegediend krijgen bij coronaire angiografie met of zonder percutane interventie, om het risico op PC-AKI te verminderen?
Aanbeveling
Gebruik geen profylactische hemodialyse bij niet dialyse-afhankelijke patiënten met chronische nierschade stadium 4-5, die intravasculair jodiumhoudend CM toegediend krijgen bij coronaire angiografie met of zonder percutane interventie, om het risico van PC-AKI te verminderen.
Gebruik profylactische hemofiltratie niet routinematig bij patiënten met chronische nierschade stadium 4-5, die intravasculair jodiumhoudend CM toegediend krijgen bij coronaire angiografie met of zonder percutane interventie.
Pas het hemodialyseschema van patiënten met chronische nierfunctievervangende therapie niet aan, wanneer deze patiënten intravasculair jodiumhoudend CM toegediend krijgen. (In andere woorden: bij het inplannen van een onderzoek met jodiumhoudend CM hoeft er geen rekening gehouden worden met het dialyseschema van de patiënt.)
Overwegingen
Renal replacement therapy for the prevention of PC-AKI
The present systematic review and meta-analysis shows that prophylactic HD increases the risk of PC-AKI in patient with CKD stage 4 to 5 (eGFR <30 ml/min/1.73m2), (albeit not significantly) but also that prophylactic HF may reduce the risk of PC-AKI, the need of acute RRT and possible long term outcome, especially if applied before and after iodine-containing contrast medium administration.
A limitation of using PC-AKI as an endpoint is that creatinine, which forms the base of the PC-AKI definition, is removed by RRT. However, creatinine is removed both by HD and HF. Nevertheless, haemodialysis increases the risk of PC-AKI while HF does not. HF might even be beneficial.
A possible explanation for the harmful effect of prophylactic HD is that the risk of RRT-induced hypotension is greater when using HD compared to HF/HDF. The risk of hypotension may especially be increased in the patients with diminished myocardial function. Continuous hemofiltration further allows for guided fluid removal and thereby prevents hydration-associated pulmonary oedema, for which patients with combined cardiac and renal dysfunction are at risk.
However, the beneficial effects of pre-and post-hemofiltration with regard to lowering the risk of PC-AKI, are only reported by one centre, if the analysis is restricted to RCTs. This limits the generalizability of the results. For this reason, we do not recommend using prophylactic hemofiltration as standard intervention in patients undergoing percutaneous coronary interventions. Pre- and post-contrast hemofiltration could however be considered in a dedicated population with combined severe renal and cardiac dysfunction having a high risk of pulmonary oedema during hydration and after intracoronary contrast administration.
Schedule of chronic dialysis
There is no literature available that answers the question whether the timing of the dialysis in regard to the timing of the contrast administration has any effect on the PC-AKI risk. It is the opinion of the working group that the scheduling of an iodine-containing contrast-enhanced imaging study does not need to be adapted to the dialysis schedule of the patient. Or vice versa: the schedule of chronic dialysis does not need to be adapted for the purpose of an iodine-containing contrast-enhanced imaging study.
Onderbouwing
Achtergrond
PC-AKI may increase cardiovascular morbidity and mortality. However, it should be noted, that the incidence of PC-AKI is low and PC-AKI only occurs in the presence of patient-, disease- or contrast-related risk factors and not in a young and healthy patient.
An impaired glomerular filtration rate, especially below 30 ml/min/1.73m2, seems the most important risk factor of PC-AKI. Adequate hydration during contrast administration seems the best preventive measure and bicarbonate hydration is recommended in this population (see Chapter 6).
Hemofiltration
The commonly used contrast media (CM) have a molecular weight below 1000 Da and are easily removed by hemofiltration. The sieving coefficient of iohexol is approximately 1 at ultrafiltrate rates between 1 and 6 L/h (Yardman, 2015) in vitro. However, during haemodialysis, sieving coefficient was about 1 at 1 L/h but decreased to 0.57 at 6 L/h. Thus hemofiltration reduced CM more effectively that haemodialysis.
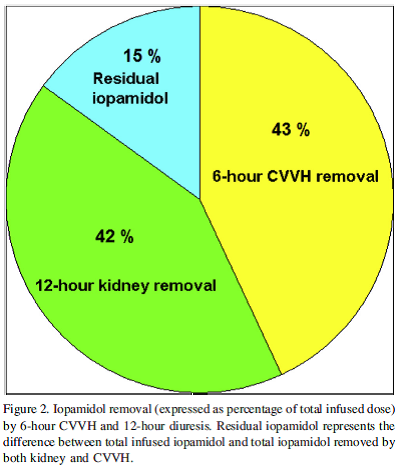
In patients with an eGFR <30 ml/min/1.73m2 (CKD stage 4 to 5), undergoing coronary angiography, the sieving coefficient of iopamidol during continuous hemofiltration was about 0.85 (Guastoni, 2014). A 6-hour session of continuous hemofiltration removed a similar amount of CM as did the kidneys in 12-hours (see figure 1). Thus in patients with CKD stage 4-5, hemofiltration significantly adds to the removal of the CM.
Figure 1 from Gastoni (1)
The main aim of the present chapter is to evaluate whether prophylactic renal replacement therapy (RRT) reduces the incidence of PC-AKI and associated complications in patients with CKD stage 4-5 (eGFR <30 ml/min/1.73m2) receiving intravascular iodine-containing CM.
Conclusies / Summary of Findings
|
Very Low GRADE |
There is a very low level of evidence that prophylactic haemodialysis does not reduce the risk of PC-AKI compared to standard medical treatment in patients with chronic kidney disease stage 4-5 (eGFR <30 ml/min/1.73m2) receiving intravascular iodine-containing contrast administration for coronary angiography with or without percutaneous intervention.
(Cruz, 2012) |
|
Very Low GRADE |
There is a very low level of evidence that prophylactic hemo(dia)filtration does not reduce the risk of PC-AKI compared to standard medical treatment in patients with Chronic Kidney Disease stage 4-5 receiving intravascular iodine-containing contrast administration for coronary angiography with or without percutaneous intervention.
(Cruz, 2012) |
|
Very Low GRADE |
There is a very low level of evidence that prophylactic hemo(dia)filtration reduces the risk of acute renal replacement therapy compared to standard medical treatment in patients with Chronic Kidney disease stage 4 or 5 receiving intravascular iodine-containing contrast administration for coronary angiography with or without percutaneous intervention.
(Cruz, 2012) |
|
Very Low GRADE |
There is a very low level of evidence that a combination of hemodiafiltration before and after contrast administration is more effective for the prevention of PC-AKI when compared to hemodiafiltration after iodine-containing contrast administration alone, in patients undergoing percutaneous intervention.
(Spini, 2013; Marenzi 2006) |
Samenvatting literatuur
Description of studies
One systematic review (Cruz, 2012) and a non-randomized controlled trial (Spini, 2013) were included in this literature analysis.
Cruz (2012) studied whether periprocedural renal replacement therapy (RRT) decreased the risk of PC-AKI in patients receiving intravascular radiocontrast when compared to standard medical therapy (SMT). The search was preformed up to March 2011. A total of 9 randomized controlled trials (RCTs) with 751 patients and 2 observational studies with 259 patients (Hsieh, 2005; Gabutti, 2003) were included in this review. Furthermore, 7 of the included RCTs contained patients with chronic kidney disease (CKD) stage 4 and 5 (n=455) (Berger, Gabutti, Hsieh, Marenzi 2003, Marenzi 2006, Sterner, Vogt); these were pooled separately in a sub analysis. This subgroup is of specific interest regarding our question.
Spini (2013) studied 46 patients with CKD, defined as serum Creatinine >177 µmol/L or eGFR less than 30 ml/min, submitted to Percutaneous coronary intervention (PCI), who received either continuous renal replacement therapy only after PCI (CRRTpost, n=21) or CRRT before and after PCI (CRRTpre-post, n=25) in addition to saline hydration in both groups.
CRRT consisted of continuous venovenous hemofiltration (CVVH) for patients with serum creatinine <265 µmol/L or continuous venovenous hemodiafiltration (CVVHDF) for patients with serum creatinine >265 µmol/L, initiated 6 to 8 hours before PCI and restarted immediately after PCI for 18-24 hours (CRRTpre-post) or CRRT applied only after PCI (CRRTpost).
Of note, the study was not randomized. Whether patients received either CRRTpost or CRRTpre-post depended on logistics and preference of the attendant physician. Furthermore, the study did not include a control group receiving hydration only. Finally, the type of replacement fluid was not specified.
The main characteristics of the individual studies included in the meta-analysis and the Spini study are presented in Table 1.
Table 1 Description of the studies regarding renal replacement therapy, type of hydration and incidence of PC-AKI
|
Author year |
Design |
Inclusion |
Intervention |
Hydration |
PC AKI RR |
Risk of acute RRT |
Mortality Hospital/long-term |
|
|
Hemofiltration (HF) or Hemodiafiltration (HDF) |
|
|||||||
|
Gabutti 2003 |
Obs 49 |
CKD st 4 |
HDF during-post vs. SMT |
16/26 of the RRT SMT: all |
1.56 (0.66-3.72) |
2.89 (0.12-67.75) |
NR |
NR |
|
Marenzi 2006 |
RCT 92 |
CKD st 4-5 |
HF pre-post vs. HF-HDF post vs. SMT |
Pre-post group: No Post group: yes SMT: yes |
0.48 (0.27-0.88) |
0.16 (0.05-0.55) |
0%
10%
20% |
NR
NR |
|
Marenzi 2003 |
RCT 114 |
CKD st 4 |
HF pre-post vs. SMT |
HF group: No |
0.12 (0.05-0.32) |
0.14 (0.03-0.58) |
3%
10% |
14%
30% |
|
Spini 2013 |
Non-RCT 46 |
CKD st 4-5 |
HF-HDF pre-post vs. HF-HDF post |
Both groups |
0.0499 (0.003-0.801) |
8% vs.
19% |
NR
NR |
16%
57% |
|
Haemodialysis |
|
|||||||
|
Berger 2001 |
RCT 15 |
CKD st 4 |
HD post vs. SMT |
Both groups |
3.43 (0.45-25.93) |
|
|
|
|
Frank 2003 |
RCT 17 |
CKD st 4 |
HD during-post vs. SMT |
Both groups |
Creat clearance not different |
|
|
|
|
Hsieh 2004 |
Obs 40 |
CKD st 4-5 |
HD post vs. SMT |
70% of the RRT SMT: all |
0.33 (0.01-7.72) |
|
|
|
|
Lee 2007 |
RCT 82 |
CKD st 5 |
HD vs. SMT |
Both groups |
|
0.07 (0.01-0.49) |
|
|
|
Lehnert 1998 |
RCT 30 |
CKD st 3-4 |
HD post vs. SMT |
Both groups |
1.33 (0.61-2.91) |
|
|
|
|
Sterner 2000 |
RCT 32
|
CKD st 4-5 |
HD post vs. SMT |
Both groups |
1.70 (0.59-4.90) |
|
|
|
|
Reinecke 2007 |
RCT 424 |
CKD st 3 |
HD post vs. SMT |
Both groups |
2.81 (1.43-5.52) |
2.05 (0.29-14.41) |
|
|
|
Vogt 2001 |
RCT 113 |
CKD st 4 |
HD post vs. SMT |
Both groups |
1.27 (0.80-2.01) |
2.81 (0.79-10.06) |
|
|
PC-AKI: post contrast acute kidney injury; RRT: renal replacement therapy; SMT: standard medical therapy; RCT: randomized controlled trial; CKD: chronic kidney disease, stage (st) 3 eGFR 30 to 60 ml/min/1.73m2, stage 4 15-30 ml/min/1.73m2, stage 5 <15 ml/min/1.73m2; HF: hemofiltration; pre-post: before and after contrast administration; post: after contrast administration; HDF: hemodiafiltration, HD: haemodialysis.
Results
Post contrast-AKI
Cruz (2012) reported that in 9 RCTs and 2 observational studies; a total of 1010 patients (n=751 for the RCTs) were included (see table 2). All studies included patients who underwent coronary angiography (CAG), with or without Percutaneous coronary intervention (PCI).
Studies were highly heterogeneous in type of RRT, timing of RRT, type of contrast given and type of hydration given as SMT (see Table 2).
Eight of the studies used haemodialysis (HD) as mode of RRT (Berger, 2001; Frank, 2003; Hsieh, 2006; Lee, 2007; Lehnert, 1998; Reinecke, 2007; Sterner, 2000; Vogt, 2001). One of these had an observational design (Hsieh, 2006) and two included patients with CKD stage stage 3 (Lehnert, 1998; Reinecke, 2007). These three studies were therefore not included in the analysis. Out of the five RCTs comparing HD to standard medical treatment (SMT), two only reported creatinine change after contrast medium administration (Frank, 2003; Lee, 2007) and not PC-AKI risk, and thus these studies also were excluded from the analysis. When the three RCTs comparing HD to SMT were pooled (Berger, 2001; Sterner, 2000; Vogt, 2001), the incidence of PC-AKI was 43% in the HD group and 30% in the SMT group. There was no significant difference in risk op PC-AKI in the patients receiving HD versus those who received SMT: risk ratio (RR): 1.38 (95% CI: 0.91 to 2.10; p=0.13) as shown in Figure 2.
Four of the included studies applied hemofiltration (HF) or hemodiafiltration (HDF). One of these compared HF before and after iodine-containing contrast (HFpre-post) to SMT (Marenzi, 2003), one study compared three groups: HFpre-post and HF after iodine-containing contrast only (HFpost) to SMT (Marenzi, 2006), one study compared HDF started just before iodine-containing contrast administration to SMT (Gabutti, 2003), and one study compared HF-HDF pre-post to HF-HDF post. The latter two studies had an observational design and were, therefore, not included in the main analysis. When the two RCTs comparing HDF to SMT were pooled (Marenzi, 2003; Marenzi, 2006) the incidence of PC-AKI was 15% in the HDF group and 53% in the SMT group. There was no significant difference in risk op PC-AKI in the patients receiving HDF versus those who received SMT: risk ratio (RR): 0.25 (95% CI: 0.06 – 1.11; p=0.07) as shown in Figure 3.
Figure 2 Pooled analysis of PC-AKI risk in CKD 4-5 patient undergoing CAG and/or PCI and receiving either HD or SMT
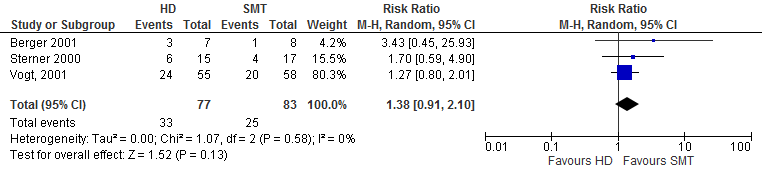
Figure 3 Pooled analysis of PC-AKI risk in CKD 4-5 patient undergoing CAG and/or PCI and receiving either HF or SMT
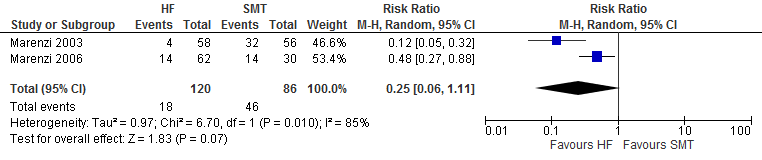
Most importantly, haemodialysis was associated with an increased risk of PC-AKI 1.38 (95% CI: 0.91 to 2.10; p=0.13), albeit this result was not statistically significant. Meanwhile HF/HDF did not reduce the occurrence of PC-AKI, but appeared to reduce the risk of acute temporary RRT (RR 0.22, 0.06-0.74). Of note, 80% of the patients receiving HF came from one centre (Cruz, 2012).
Pre- contrast medium HDF versus pre- and post-contrast medium HDF
Spini (2013) reported that none of the patients in the HF-HDFpre-post group 0/25 developed PC-AKI, while 13/21 (62%) patient in the HF-HDFpost group developed PC-AKI (RR 0.0499 (95% CI 0.003 to 0.801, p <0.001)). Furthermore, during a follow-up of 15 months (median) a worsening of kidney function was observed in 3/25 patients in the HF-HDFpre-post group compared to 9/21 in the HF-HDFpost group (p=0.042). However, this study was not randomized and might be confounded.
Three of the studies investigating pre- and post-contrast hemofiltration found a reduction of in-hospital complications (Marenzi, 2003; Marenzi, 2006; Spini, 2015).
In addition, three of the studies investigating pre- and post-contrast hemofiltration found a reduction in mortality. Marenzi (2003) and Marenzi (2006) reported a reduction in hospital mortality, while Marenzi (2003) and Spini reported a reduction in late mortality.
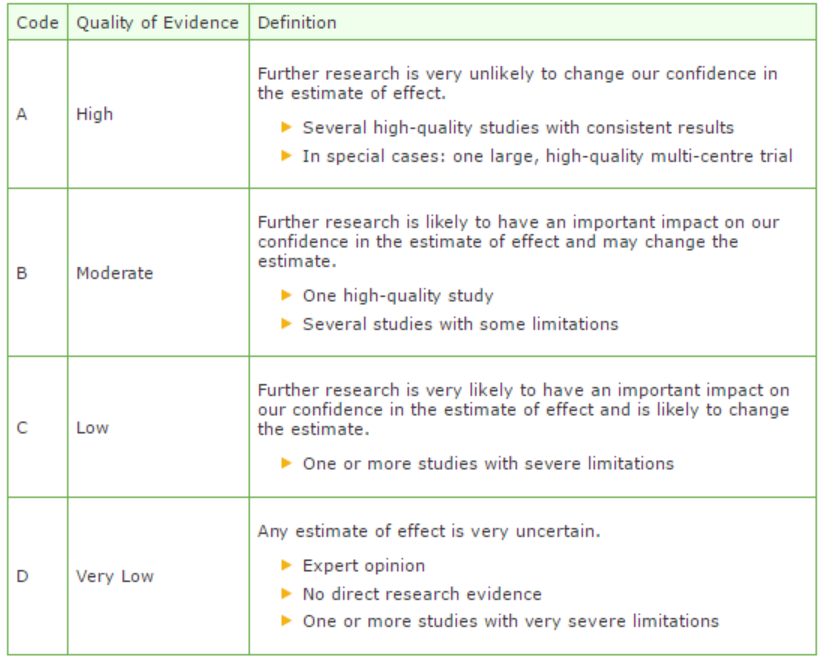
Quality of evidence
The quality of evidence for the outcome PC-AKI in the comparison HD or HDF versus SMT in patients with CKD 4-5 was downgraded by three points, from high to very low; one point due to heterogeneity of the included studies and two points due to wide confidence intervals of effect size (imprecision).
The quality of evidence for the outcome PC-AKI in the comparison post-CRRT versus pre- and post-CRRT was downgraded by three points, from high to very low, due to wide confidence intervals of effect size (imprecision).
Zoeken en selecteren
To answer our clinical question a systematic literature analysis was performed for the following research question:
Can prophylactic hemofiltration reduce the risk of PC-AKI in patients with pre-existent reduced kidney function (pre-existent eGFR less than 30 ml/min/1.73m2) receiving intravascular contrast?
P (patient category) Patients with impaired kidney function (eGFR less than 30 ml/min/1.73m2) undergoing radiological examinations or interventions with reduced kidney function receiving intravascular contrast.
I (intervention) hemofiltration with or without hydration.
C (comparison) hydration alone.
O (outcome) Contrast-induced nephropathy (CIN) / contrast-associated acute kidney injury (CA-AKI), Post Contrast AKI (PC-AKI), start dialysis, chronic decrease in residual kidney function.
Relevant outcome measures
The working group considered PC-AKI, mortality, start dialysis, decrease in residual kidney function, critical outcome measures for the decision making process.,
A difference of at least 10% in relative risk was defined as a clinically relevant difference; by expert opinion of the working group (no literature was available to substantiate the decision). To illustrate, if PC-AKI occurs with an incidence of 10% in the patient population, a difference of 10% of relative risk would mean a difference of 1% in absolute risk. Thus the number needed to treat would be 100, ergo: a doctor would need to treat 100 patients to prevent one case of PC-AKI. When the incidence of PC-AKI is 5%, a difference of 10% in relative risk would mean a difference of 0.5% in absolute risk, and a number needed to treat of 200.
Search and select (method)
The data bases Medline (OVID), Embase and the Cochrane Library were searched from January 1995 to 15th of October 2015 using relevant search terms for systematic reviews (SRs) and randomized controlled trials (RCTs). A search update was performed on the 3rd of May 2017. The literature search procured 126 hits. A total of 113 papers were found in the initial search, and 14 in the search update.
The following search criteria were applied:
- Randomized controlled trial or meta-analysis.
- Adult patients who underwent radiological examination or intervention using intravascular contrast media.
- Patients with impaired kidney function (eGFR <30 ml/min/1.73m2).
- Hydration types: hydration with intravenous (i.v.) NaCl 0.9% or bicarbonate 1.4%, oral hydration.
- Treatment arm consisted out of patients receiving renal replacement therapy (haemodialysis, hemodiafiltration, hemofiltration).
- The control arm consisted of patients that received hydration only.
- At least one of the outcome measures was described: Contrast-induced nephropathy (CIN) / contrast-induced acute kidney injury (CI-AKI)/PC-AKI, start dialysis, chronic decrease in kidney function, adverse effects of hydration (fluid overload, intensive care unit admission, and mortality), and cost-effectiveness.
Based on title and abstract 29 studies were selected, all from the initial search. After examination of full text, 27 studies were excluded, leaving 2 studies to be included in the literature summary. Reasons for exclusion are described in the exclusion table.
Results
Two studies were included in the literature analysis: one meta-analysis and one non-randomized controlled study. the most important study characteristics and results are included in the evidence tables. The evidence tables and assessment of individual study quality are included.
Referenties
- Berger, E.D., Bader, B.D., Bosker, J. et al, Contrast media-induced kidney failure cannot be prevented by hemodialysis [German]. Dtsch Med Wochenschr. 2001;126:162166.
- Cruz DN, Goh CY, Marenzi G, et al. Renal replacement therapies for prevention of radiocontrast-induced nephropathy: a systematic review. Am J Med. 2012;125(1):66-78.e3.
- Frank, H., Werner, D., Lorusso, V. et al, Simultaneous hemodialysis during coronary angiography fails to prevent radiocontrast-induced nephropathy in chronic renal failure. Clin Nephrol. 2003;60:176182.
- Gabutti L, Marone C, Monti M, et al. Does continuous venovenous hemodiafiltration concomitant with radiological procedures provide a significant and safe removal of the iodinated contrast ioversol? Blood Purif. 2003;21(2):152-7.
- Hsieh, Y.C., Ting, C.T., Liu, T.J. et al, Short- and long-term renal outcomes of immediate prophylactic hemodialysis after cardiovascular catheterizations in patients with severe renal insufficiency. Int J Cardiol. 2005;101:407413.
- Lee, P.T., Chou, K.J., Liu, C.P. et al, Renal protection for coronary angiography in advanced renal failure patients by prophylactic hemodialysis (A randomized controlled trial) . J Am Coll Cardiol. 2007;50:10151020.
- Lehnert, T., Keller, E., Gondolf, K. et al, Effect of haemodialysis after contrast medium administration in patients with renal insufficiency. Nephrol Dial Transplant. 1998;13:358362.
- Marenzi G, Assanelli E, Marana I, et al. N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med. 2006 Jun 29;354(26):2773-82.
- Marenzi G, Marana I, Lauri G, et al. The prevention of radiocontrast-agent-induced nephropathy by hemofiltration. N Engl J Med. 2003 Oct 2;349(14):1333-40.
- Reinecke, H., Fobker, M., Wellmann, J. et al, A randomized controlled trial comparing hydration therapy to additional hemodialysis or N-acetylcysteine for the prevention of contrast medium-induced nephropathy: the Dialysis-versus-Diuresis (DVD) Trial. Clin Res Cardiol. 2007;96:130139.
- Spini V, Cecchi E, Chiostri M, et al. Effects of two different treatments with continuous renal replacement therapy in patients with chronic renal dysfunction submitted to coronary invasive procedures. J Invasive Cardiol. 2013;25(2):80-4.
- Sterner, G., Frennby, B., Kurkus, J., et al. Does post-angiographic hemodialysis reduce the risk of contrast-medium nephropathy?. Scand J Urol Nephrol. 2000;34:323326.
- Vogt, B., Ferrari, P., Schonholzer, C. et al, Prophylactic hemodialysis after radiocontrast media in patients with renal insufficiency is potentially harmful. Am J Med. 2001;111:692698.
Evidence tabellen
Table: Exclusion after revision of full text
|
Author and year |
Reason for exclusion |
|
Chang, 2013 |
Does not fulfill selection criteria |
|
Choi, 2014 |
Does not fulfill selection criteria |
|
Cruz, 2006 |
Does not fulfill selection criteria |
|
Cruz, 2008 |
Does not fulfill selection criteria |
|
Deray, 2006 |
Does not fulfill selection criteria |
|
Frank, 2003 |
Already included in systematic review Cruz, 2012 |
|
Furukawa, 1996 |
Does not fulfill selection criteria |
|
Gabutti, 2003 |
Does not fulfill selection criteria |
|
Ghani, 2011 |
Does not fulfill selection criteria |
|
Hsieh, 2005 |
Already included in systematic review Cruz, 2012 |
|
Huber, 2002 |
Does not fulfill selection criteria |
|
Joannidis, 2010 |
Does not fulfill selection criteria |
|
Lee, 2007 |
Already included in systematic review Cruz, 2012 |
|
Lehnert, 1998 |
Already included in systematic review Cruz, 2012 |
|
Marenzi, 2003 |
Already included in systematic review Cruz, 2012 |
|
Marenzi, 2004 |
Does not fulfill selection criteria |
|
Marenzi, 2006 |
Already included in systematic review Cruz, 2012 |
|
Marenzi, 2007 |
Does not fulfill selection criteria |
|
Moon, 1995 |
Does not fulfill selection criteria |
|
Ono, 2004 |
Does not fulfill selection criteria |
|
Reinecke, 2007 |
Already included in systematic review Cruz, 2012 |
|
Schindler, 2001 |
Does not fulfill selection criteria |
|
Shinoda, 2002 |
Does not fulfill selection criteria |
|
Song, 2010 |
Does not fulfill selection criteria |
|
Song, 2011 |
Does not fulfill selection criteria |
|
Sterner, 2000 |
Already included in systematic review Cruz, 2012 |
|
Vogt, 2001 |
Already included in systematic review Cruz, 2012 |
Table of quality assessment for systematic reviews of RCTs and observational studies
Based on AMSTAR checklist (Shea et al.; 2007, BMC Methodol 7: 10; doi:10.1186/1471-2288-7-10) and PRISMA checklist (Moher et al 2009, PLoS Med 6: e1000097; doi:10.1371/journal.pmed1000097)
|
Study
First author, year |
Appropriate and clearly focused question?1
Yes/no/unclear |
Comprehensive and systematic literature search?2
Yes/no/unclear |
Description of included and excluded studies?3
Yes/no/unclear |
Description of relevant characteristics of included studies?4
Yes/no/unclear |
Appropriate adjustment for potential confounders in observational studies?5
Yes/no/unclear/notapplicable |
Assessment of scientific quality of included studies?6
Yes/no/unclear |
Enough similarities between studies to make combining them reasonable?7
Yes/no/unclear |
Potential risk of publication bias taken into account?8
Yes/no/unclear |
Potential conflicts of interest reported?9
Yes/no/unclear |
|
Cruz, 2012 |
Yes |
Yes |
No |
Yes |
No |
Yes |
Yes |
No |
No |
- Research question (PICO) and inclusion criteria should be appropriate and predefined
- Search period and strategy should be described; at least Medline searched; for pharmacological questions at least Medline + EMBASE searched
- Potentially relevant studies that are excluded at final selection (after reading the full text) should be referenced with reasons
- Characteristics of individual studies relevant to research question (PICO), including potential confounders, should be reported
- Results should be adequately controlled for potential confounders by multivariate analysis (not applicable for RCTs)
- Quality of individual studies should be assessed using a quality scoring tool or checklist (Jadad score, Newcastle-Ottawa scale, risk of bias table etc.)
- Clinical and statistical heterogeneity should be assessed; clinical: enough similarities in patient characteristics, intervention and definition of outcome measure to allow pooling? For pooled data: assessment of statistical heterogeneity using appropriate statistical tests (e.g. Chi-square, I2)?
- An assessment of publication bias should include a combination of graphical aids (e.g., funnel plot, other available tests) and/or statistical tests (e.g., Egger regression test, Hedges-Olken). Note: If no test values or funnel plot included, score “no”. Score “yes” if mentions that publication bias could not be assessed because there were fewer than 10 included studies.
- Sources of support (including commercial co-authorship) should be reported in both the systematic review and the included studies. Note: To get a “yes,” source of funding or support must be indicated for the systematic review AND for each of the included studies.
Risk of bias table for intervention studies (randomized controlled trials)
Research question:
|
Study reference
(first author, publication year) |
Describe method of randomisation1 |
Bias due to inadequate concealment of allocation?2
(unlikely/likely/unclear) |
Bias due to inadequate blinding of participants to treatment allocation?3
(unlikely/likely/unclear) |
Bias due to inadequate blinding of care providers to treatment allocation?3
(unlikely/likely/unclear) |
Bias due to inadequate blinding of outcome assessors to treatment allocation?3
(unlikely/likely/unclear) |
Bias due to selective outcome reporting on basis of the results?4
(unlikely/likely/unclear) |
Bias due to loss to follow-up?5
(unlikely/likely/unclear) |
Bias due to violation of intention to treat analysis?6
(unlikely/likely/unclear) |
|
Spini, 2013 |
Not randomised |
Unlikely |
Unclear |
Unclear |
Unclear |
Unlikely |
Unlikely |
Unclear |
- Randomisation: generation of allocation sequences have to be unpredictable, for example computer generated random-numbers or drawing lots or envelopes. Examples of inadequate procedures are generation of allocation sequences by alternation, according to case record number, date of birth or date of admission.
- Allocation concealment: refers to the protection (blinding) of the randomisation process. Concealment of allocation sequences is adequate if patients and enrolling investigators cannot foresee assignment, for example central randomisation (performed at a site remote from trial location) or sequentially numbered, sealed, opaque envelopes. Inadequate procedures are all procedures based on inadequate randomisation procedures or open allocation schedules..
- Blinding: neither the patient nor the care provider (attending physician) knows which patient is getting the special treatment. Blinding is sometimes impossible, for example when comparing surgical with non-surgical treatments. The outcome assessor records the study results. Blinding of those assessing outcomes prevents that the knowledge of patient assignement influences the proces of outcome assessment (detection or information bias). If a study has hard (objective) outcome measures, like death, blinding of outcome assessment is not necessary. If a study has “soft” (subjective) outcome measures, like the assessment of an X-ray, blinding of outcome assessment is necessary.
- Results of all predefined outcome measures should be reported; if the protocol is available, then outcomes in the protocol and published report can be compared; if not, then outcomes listed in the methods section of an article can be compared with those whose results are reported.
- If the percentage of patients lost to follow-up is large, or differs between treatment groups, or the reasons for loss to follow-up differ between treatment groups, bias is likely. If the number of patients lost to follow-up, or the reasons why, are not reported, the risk of bias is unclear
- Participants included in the analysis are exactly those who were randomized into the trial. If the numbers randomized into each intervention group are not clearly reported, the risk of bias is unclear; an ITT analysis implies that (a) participants are kept in the intervention groups to which they were randomized, regardless of the intervention they actually received, (b) outcome data are measured on all participants, and (c) all randomized participants are included in the analysis.
Risk of bias table for intervention studies (observational: non-randomized clinical trials, cohort and case-control studies)
Evidence table for systematic review of RCTs and observational studies (intervention studies)
Research question:
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C) |
Follow-up |
Outcome measures and effect size |
Comments |
|
Cruz, 2012
individual study characteristics deduced from [1st author, year of publication
PS., study characteristics and results are extracted from the SR (unless stated otherwise) |
SR and meta-analysis of RCTs / cohort studies
Literature search up to March 2011
A: Lee, 2007 B: Reinecke, 2007 C: Marenzi, 2006 D: Hsieh, 2005 E: Marenzi, 2003 F: Frank, 2003 G: Gabutti, 2003 H: Vogt, 2001 I: Sterner, 2000 J: Berger, 2001 K: Lehnert, 2008
Study design: A: Randomized trial B: Randomized trial C: Randomized trial D: Observational E: Randomized trial F: Randomized trial G: Observational H: Randomized trial I: Randomized trial J: Randomized trial K: Randomized trial
Setting and Country: Italy
Source of funding: No funding
|
Inclusion criteria SR: 1) studies that ecaluated the use of periprocedural renal replacement therapy (RRT) for the prevention of radiocontrast induced nephropathy (RCIN) as compared with standard medical treatment (SMT) 2) 10 or more human subjects 3) primary outcome: RCIN (sCR ≥0.5mg/dL / 44 umol/L); secondary outcomes: need for temporary acute RRT, need for permanent RRT, long-term changes in renal function, death
Exclusion criteria SR:
11 studies included
Important patient characteristics at baseline: Number of patients; characteristics important to the research question and/or for statistical adjustment (confounding in cohort studies); for example, age, sex, bmi, ...
Number of patients , age (years) A: 82; 65-66 B: 424; 67-68 C: 92; 71-72 D: 40; 66-69 E: 114; 69 F: 17; 58-67 G: 49; 70 H: 113; 69-70 I:32; 65-72 J: 15; 62-68 K: 30; 60-63
Sex: not reported
Groups comparable at baseline? Unclear |
Describe intervention:
A: hemodialysis (HD) B: HD C: HD D: HD E: HD F: HD G: HD H: HD I: Hemofiltration (HF) J: HF K: Hemodiafiltration
|
Describe control:
For all studies: Standard medical therapy, depending on hospital either pre-hydration or pre- and posthydration
|
End-point of follow-up:
Not reported
For how many participants were no complete outcome data available? Not reported
|
Outcome measure-1 Defined as RCIN Reported for CKD stage 4-5 patients only
Effect measure: RR [95% CI]: J: 3.43 (0.45 – 25.93) G: 1.56 (0.66 – 3.72) D: 0.33 (0.01 – 7.72) E: 0.12 (0.05 – 0.32) C: 0.48 (0.27 – 0.88) I: 1.70 (0.59 – 4.90) H: 1.27 (0.80 – 2.01)
Pooled effect (random effects model): 0.81 [95% CI 0.37 to 1.76] favoring RRT. Heterogeneity (I2): 79%
Outcome measure-2 Risk for acute RRT
HDF/HF G: 2.89 (0.12 – 67.75) E: 0.14 (0.03 – 0.58) C: 0.16 (0.05 – 0.55) Pooled effect (random effects model): 0.22 [95% CI 0.06 to 0.74] favoring RRT. Heterogeneity (I2): 36%
HD A: 0.07 (0.01 – 0.49) B: 2.05 (0.29 – 14.41) H: 2.81 (0.70 – 10.06) Pooled effect (random effects model): 0.78 [95% CI 0.07 to 8.43] favoring RRT. Heterogeneity (I2): 83%
Outcome measure-3 Risk for chronic RRT
HDF/HF E: 0.32 (0.03 – 3.00)
HD F: 1.43 (0.26 – 7.86) D: 1.33 (0.34 – 5.21) A: 0.09 (0.00 – 1.52) H: 2.11 (0.20 – 22.61) Pooled effect (random effects model): 0.87 [95% CI 0.33 to 2.29] favoring RRT. Heterogeneity (I2): 19%
Outcome measure-4 Mortality Not reported per study. Pooled analysis for 5 studies. I: 2.6% C: 3.7% RR: 0.65, 95% CI: 0.17 – 2.49 |
Facultative:
Brief description of author’s conclusion: In this updated meta-analysis periproceural RRT did not decrease the incidence of RCIN compared with SMT. HD appears to actually increase RCIN risk.
Personal remarks on study quality, conclusions, and other issues (potentially) relevant to the research question: In our own literature analysis the observational studies were excluded from the systematic review and only the RCTs with patients CKD stage 4-5 were included.
Level of evidence: GRADE Low to Very low for most studies due to high risk of bias in several studies, wide confidence intervals (imprecision) and heterogeneity of included studies |
CIN: contrast induced nephropathy; NAC: N-acetyl-cysteine; NR: not reported
Evidence table for intervention studies (randomized controlled trials and non-randomized observational studies [cohort studies, case-control studies, case series])1
This table is also suitable for diagnostic studies (screening studies) that compare the effectiveness of two or more tests. This only applies if the test is included as part of a test-and-treat strategy – otherwise the evidence table for studies of diagnostic test accuracy should be used.
Research question:
|
Study reference |
Study characteristics |
Patient characteristics 2 |
Intervention (I) |
Comparison / control (C) 3
|
Follow-up |
Outcome measures and effect size 4 |
Comments |
|
Spini, 2013 |
Type of study: prospective controlled trial
Setting: cardiac stepdown
Country: Italy
Source of funding: not reported |
Inclusion criteria: patients admitted to the cardiac stepdown at the participating hospital -eGFR <30mL/min -needed to be submitted to percutaneous intervention
Exclusion criteria: -
N total at baseline: 46 Intervention: 25 Control: 21
Important prognostic factors2: For example age ± SD: I: 73 ± 11 C: 74 ± 8
Sex: I: 84% M C: 67% M
Groups comparable at baseline? Yes |
Describe intervention (treatment/procedure/test):
Continuous renal replacement therapy (CRRT) at least 6 hours before and 24 hours after contrast medium administration
|
Describe control (treatment/procedure/test):
CRRT only after percutaneous intervention |
Length of follow-up: Creatinine levels – 72 hours Mortality 12 months, 18 months
Loss-to-follow-up: not reported
Incomplete outcome data: Not reported
|
Outcome measures and effect size (include 95%CI and p-value if available):
Contrast induced nephropathy (CIN): I: 0/25 (0%) C: 13/21 (62%) p-value not reported
Worsening renal failure: I: 3/25 (12%) C: 9/25 (43%) p-0.042
Dialysis: I: 2/25 (8%) C: 9/21 (19%) P=0.50
Long-term mortality: I: 4/25 (16%) I: 12/21 (57%) P0.009
Cardiovascular deaths: I: 0/25 (0%) C: 5/21 (24%) p-value not reported |
A limitation of using PC-AKI / CIN as an endpoint, is that creatinine, which forms the base of the PC-AKI definition, is removed by RRT. However, creatinine is removed by CRRT. |
Notes:
- Prognostic balance between treatment groups is usually guaranteed in randomized studies, but non-randomized (observational) studies require matching of patients between treatment groups (case-control studies) or multivariate adjustment for prognostic factors (confounders) (cohort studies); the evidence table should contain sufficient details on these procedures
- Provide data per treatment group on the most important prognostic factors [(potential) confounders]
- For case-control studies, provide sufficient detail on the procedure used to match cases and controls
- For cohort studies, provide sufficient detail on the (multivariate) analyses used to adjust for (potential) confounders
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 08-01-2018
Beoordeeld op geldigheid : 01-11-2017
Validity
The board of the Radiological Society of the Netherlands will determine at the latest in 2023 if this guideline (per module) is still valid and applicable. If necessary, a new working group will be formed to revise the guideline. The validity of a guideline can be shorter than 5 years, if new scientific or healthcare structure developments arise, that could be seen as a reason to commence revisions. The Radiological Society of the Netherlands is considered the keeper of this guideline and thus primarily responsible for the actuality of the guideline. The other scientific societies that have participated in the guideline development share the responsibility to inform the primarily responsible scientific society about relevant developments in their field.
Initiative
Radiological Society of the Netherlands
Authorization
The guideline is submitted for authorization to:
- Association of Surgeons of the Netherlands
- Dutch Association of Urology
- Dutch Federation of Nephrology
- Dutch Society Medical Imaging and Radiotherapy
- Dutch Society of Intensive Care
- Netherlands Association of Internal Medici
- Netherlands Society for Clinical Chemistry and Laboratory Medicine
- Netherlands Society of Cardiology
- Netherlands Society of Emergency Physicians
- Radiological Society of the Netherlands
Algemene gegevens
General Information
The guideline development was assisted by the Knowledge Institute of Medical Specialists (https://www.kennisinstituut.nl) and was financed by the Quality Funds for Medical Specialists (Kwaliteitsgelden Medisch Specialisten: SKMS).
Doel en doelgroep
Goal of the current guideline
The aim of the Part 1 of Safe Use of Iodine-containing Contrast Media guidelines is to critically review the present recent evidence with the above trend in mind, and try to formulate new practical guidelines for all hospital physicians to provide the safe use of contrast media in diagnostic and interventional studies. The ultimate goal of this guideline is to increase the quality of care, by providing efficient and expedient healthcare to the specific patient populations that may benefit from this healthcare and simultaneously guard patients from ineffective care. Furthermore, such a guideline should ideally be able to save money and reduce day-hospital waiting lists.
Users of this guideline
This guideline is intended for all hospital physicians that request or perform diagnostic or interventional radiologic or cardiologic studies for their patients in which CM are involved.
Samenstelling werkgroep
Working group members
A multidisciplinary working group was formed for the development of the guideline in 2014. The working group consisted of representatives from all relevant medical specialization fields that are involved with intravascular contrast administration.
All working group members have been officially delegated for participation in the working group by their scientific societies. The working group has developed a guideline in the period from October 2014 until July 2017.
The working group is responsible for the complete text of this guideline.
Working group
Cobbaert C., clinical chemist, Leiden University Medical Centre (member of advisory board from September 2015)
Danse P., interventional cardiologist, Rijnstate Hospital, Arnhem
Dekker H.M., radiologist, Radboud University Medical Centre, Nijmegen
Geenen R.W.F., radiologist, Noordwest Ziekenhuisgroep (NWZ), Alkmaar/Den Helder
Hoogeveen E.K., nephrologist, Jeroen Bosch Hospital, ‘s-Hertogenbosch
Kooiman J., research physician, Leiden University Medical Centre, Leiden
Oudemans - van Straaten H.M., internist-intensive care specialist, Free University Medical Centre, Amsterdam
Pels Rijcken T.H., interventional radiologist, Tergooi, Hilversum
Sijpkens Y.W.J., nephrologist, Haaglanden Medical Centre, The Hague
Vainas T., vascular surgeon, University Medical Centre Groningen (until September 2015)
van den Meiracker A.H., internist-vascular medicine, Erasmus Medical Centre, Rotterdam
van der Molen A.J., radiologist, Leiden University Medical Centre, Leiden (chairman)
Wikkeling O.R.M., vascular surgeon, Heelkunde Friesland Groep, location: Nij Smellinghe Hospital, Drachten (from September 2015)
Advisory board
Demir A.Y., clinical chemist, Meander Medical Center, Amersfoort, (member of working group until September 2015)
Hubbers R., patient representative, Dutch Kidney Patient Association
Mazel J., urologist, Spaarne Gasthuis, Haarlem
Moos S., resident in Radiology, HAGA Hospital, The Hague
Prantl K., Coordinator Quality & Research, Dutch Kidney Patient Association
van den Wijngaard J., resident in Clinical Chemistry, Leiden University Medical Center
Methodological support
Boschman J., advisor, Knowledge Institute of Medical Specialists (from May 2017)
Burger K., senior advisor, Knowledge Institute of Medical Specialists (until March 2015)
Harmsen W., advisor, Knowledge Institute of Medical Specialists (from May 2017)
Mostovaya I.M., advisor, Knowledge Institute of Medical Specialists
Persoon S., advisor, Knowledge Institute of Medical Specialists (March 2016 – September 2016)
van Enst A., senior advisor, Knowledge Institute of Medical Specialists (from January 2017)
Belangenverklaringen
Conflicts of interest
The working group members have provided written statements about (financially supported) relations with commercial companies, organisations or institutions that are related to the subject matter of the guideline. Furthermore, inquiries have been made regarding personal financial interests, interests due to personal relationships, interests related to reputation management, interest related to externally financed research and interests related to knowledge valorisation. The statements on conflict of interest can be requested at the administrative office of the Knowledge Institute of Medical Specialists and are summarised below.
|
Member |
Function |
Other offices |
Personal financial interests |
Personal relationships |
Reputation management |
Externally financed research |
Knowledge-valorisation |
Other potential conflicts of interest |
Signed |
|
Workgroup |
|||||||||
|
Burger |
Advisor, Knowledge Institute of Medical Specialists |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Cobbaert |
Member, physician clinical chemistry |
Head of clinical chemistry department in Leiden LUMC. Tutor for post-academic training of clinical chemists, coordinator/host for the Leiden region Member of several working groups within the Dutch Society for Clinical Chemistry and member of several international working groups for clinical chemistry |
None |
None |
Member of several working groups within the Dutch Society for Clinical Chemistry and member of several international working groups for clinical chemistry |
None |
None |
None |
Yes |
|
Danse |
Member, cardiologist |
Board member committee of Quality, Dutch society for Cardiology (unpaid) Board member Conference committee DRES (unpaid) |
None |
None |
None |
None |
None |
None |
Yes |
|
Dekker |
Member, radiologist |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Geenen |
Member, radiologist |
Member Contrast Media Safety Committee of the European Society of Urogenital Radiology (unpaid, meetings are partially funded by CM industry))) |
None |
None |
None |
None |
None |
Has been a public speaker during symposia organised by GE Healthcare about contrast agents (most recently in June 2014) |
Yes |
|
Hoogeveen |
Member, nephrologist |
Member of Guideline Committee of Dutch Federation of Nephrology |
None |
None |
Member of Guideline Committee of Dutch Society for Nephrology |
Grant from the Dutch Kidney Foundation to study effect of fish oil on kidney function in post-MI patients |
None |
None |
Yes |
|
Kooiman |
Member, research physician |
Resident in department of gynaecology & obstetrics |
None |
None |
None |
None |
None |
None |
Yes |
|
Mostovaya |
Advisor, Knowledge Institute of Medical Specialists |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Oudemans – van Straaten |
Member, intensive care medical specialist Professor Intensive Care |
none |
None |
None |
None |
None |
None |
None |
Yes |
|
Pels Rijcken |
Member, interventional radiologist |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Sijpkens |
Member, nephrologist |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Vainas |
Member, vascular surgeon |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Van den Meiracker |
Member, internist vascular medicine |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Van der Molen |
Chairman, radiologist |
Member Contrast Media Safety Committee of the European Society of Urogenital Radiology (unpaid,CMSC meetings are partially funded by CM industry)) |
None |
None |
Secretary section of Abdominal Radiology; Radiological Society of the Netherlands (until spring of 2015) |
None |
None |
Receives Royalties for books: Contrast Media Safety, ESUR guidelines, 3rd ed. Springer, 2015 Received speaker fees for lectures on CM safety by GE Healthcare, Guerbet, Bayer Healthcare and Bracco Imaging (2015-2016) |
Yes |
|
Wikkeling |
Member, vascular surgeon |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Advisory Board |
|||||||||
|
Demir |
Member, physician clinical chemistry |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Hubbers |
Member, patient’s representative, Dutch Society of Kidney Patients |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Mazel |
Member, urologist |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Prantl |
Member, policy maker, Dutch Society of Kidney Patients |
None |
None |
None |
None |
None |
None |
None |
Yes |
|
Van den Wijngaard |
Member, resident clinical chemistry |
Reviewer for several journals (such as American Journal of Physiology) |
None |
None |
None |
None |
None |
None |
Yes |
Inbreng patiëntenperspectief
Patients’ perspective was represented, firstly by membership and involvement in the advisory board of a policy maker and a patients’ representative from the Dutch Kidney Patient Association. Furthermore, an online survey was organized by the Dutch Kidney Patient Association about the subject matter of the guideline. A summary of the results of this survey has been discussed during a working group meeting at the beginning of the guideline development process. Subjects that were deemed relevant by patients were included in the outline of the guideline. The concept guideline has also been submitted for feedback during the comment process to the Dutch Patient and Consumer Federation, who have reported their feedback through the Dutch Kidney Patient Association.
Methode ontwikkeling
Evidence based
Implementatie
In the different phases of guideline development, the implementation of the guideline and the practical enforceability of the guideline were taken into account. The factors that could facilitate or hinder the introduction of the guideline in clinical practice have been explicitly considered. The implementation plan can be found with the Related Products. Furthermore, quality indicators were developed to enhance the implementation of the guideline. The indicators can also be found with the Related Products.
Werkwijze
AGREE
This guideline has been developed conforming to the requirements of the report of Guidelines for Medical Specialists 2.0; the advisory committee of the Quality Counsel. This report is based on the AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II) (www.agreetrust.org), a broadly accepted instrument in the international community and on the national quality standards for guidelines: “Guidelines for guidelines” (www.zorginstituutnederland.nl).
Identification of subject matter
During the initial phase of the guideline development, the chairman, working group and the advisor inventory the relevant subject matter for the guideline. Furthermore, an Invitational Conference was organized, where additional relevant subjects were suggested by the Dutch Kidney Patient Association, Dutch Society for Emergency Physicians, and Dutch Society for Urology. A report of this meeting can be found in Related Products.
Clinical questions and outcomes
During the initial phase of guideline development, the chairman, working group and advisor identified relevant subject matter for the guideline. Furthermore, input was acquired for the outline of the guideline during an Invitational Conference. The working group then formulated definitive clinical questions and defined relevant outcome measures (both beneficial land harmful effects). The working group rated the outcome measures as critical, important and not important. Furthermore, where applicable, the working group defined relevant clinical differences.
Strategy for search and selection of literature
For the separate clinical questions, specific search terms were formulated and published scientific articles were sought after in (several) electronic databases. Furthermore, studies were looked for by cross-referencing other included studies. The studies with potentially the highest quality of research were looked for first. The working group members selected literature in pairs (independently of each other) based on title and abstract. A second selection was performed based on full text. The databases search terms and selection criteria are described in the modules containing the clinical questions.
Quality assessment of individual studies
Individual studies were systematically assessed, based on methodological quality criteria that were determined prior to the search, so that risk of bias could be estimated. This is described in the “risk of bias” tables.
Summary of literature
The relevant research findings of all selected articles are shown in evidence tables. The most important findings in literature are described in literature summaries. When there were enough similarities between studies, the study data were pooled.
Grading the strength of scientific evidence
A) For intervention questions
The strength of the conclusions of the scientific publications was determined using the GRADE-method. GRADE stands for Grading Recommendations Assessment, Development and Evaluation (see http://www.gradeworkinggroup.org/) (Atkins, 2004).
GRADE defines four gradations for the quality of scientific evidence: high, moderate, low or very low. These gradations provide information about the amount of certainty about the literature conclusions. (http://www.guidelinedevelopment.org/handbook/).
B) For diagnostic, etiological, prognostic or adverse effect questions, the GRADE-methodology cannot (yet) be applied. The quality of evidence of the conclusion is determined by the EBRO method (van Everdingen, 2004)
Formulating conclusion
For diagnostic, etiological, prognostic or adverse effect questions, the evidence was summarized in one or more conclusions, and the level of the most relevant evidence was reported. For intervention questions, the conclusion was drawn based on the body of evidence (not one or several articles). The working groups weighed the beneficial and harmful effects of the intervention.
Considerations
Aspects such as expertise of working group members, patient preferences, costs, availability of facilities, and organization of healthcare aspects are important to consider when formulating a recommendation. These aspects were discussed in the paragraph Considerations.
Formulating recommendations
The recommendations answer the clinical question and were based on the available scientific evidence and the most relevant considerations.
Constraints (organization of healthcare)
During the development of the outline of the guideline and the rest of the guideline development process, the organization of healthcare was explicitly taken into account. Constraints that were relevant for certain clinical questions were discussed in the Consideration paragraphs of those clinical questions. The comprehensive and additional aspects of the organization of healthcare were discussed in a separate chapter.
Development of quality indicators
Internal (meant for use by scientific society or its members) quality indicators are developed simultaneously with the guideline. Furthermore, existing indicators on this subject were critically appraised; and the working group produces an advice about such indicators. Additional information on the development of quality indicators is available by contacting the Knowledge Institute for Medical Specialists. (secretariaat@kennisinstituut.nl).
Knowledge Gaps
During the development of the guideline, a systematic literature search was performed the results of which help to answer the clinical questions. For each clinical question the working group determined if additional scientific research on this subject was desirable. An overview of recommendations for further research is available in the appendix Knowledge Gaps.
Comment- and authorisation phase
The concept guideline was subjected to commentaries by the involved scientific societies. The commentaries were collected and discussed with the working group. The feedback was used to improve the guideline; afterwards the working group made the guideline definitive. The final version of the guideline was offered for authorization to the involved scientific societies, and was authorized.
References
Atkins D, Eccles M, Flottorp S, et al. GRADE Working Group. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv Res. 2004 Dec 22;4(1):38.
Van Everdingen JJE, Burgers JS, Assendelft WJJ, et al. Evidence-based richtlijnontwikkeling. Bohn Stafleu van Loghum. Houten, 2004
Zoekverantwoording
|
Database |
Search terms |
Total |
|
Medline
1995-okt. 2015
English |
1 exp Contrast Media/ or ((contrast adj3 iodine) or (contrast adj3 medi*)).ti,ab. (113850) 2 exp Kidney Diseases/ or (((kidney or renal) adj2 (disease* or injur* or failure*)) or nephropath* or (renal adj2 (insufficienc* or function* or disease* or failure*))).ti,ab. (543550) 3 (((contrast* or ci) adj2 (nephropath* or 'kidney injury' or aki or nephrotoxicity)) or cin or ciaki).ti,ab. (9272) 4 1 and 2 (9076) 5 (((contrast* or ci) adj2 (nephropath* or 'kidney injury' or aki or nephrotoxicity)) or cin or ciaki).ti,ab. (9272) 6 4 or 5 (16764) 7 exp Hemofiltration/ or exp Renal Dialysis/ (103123) 8 (Hemofiltrat* or Haemofiltrat* or Haemodiafiltrat* or Hemodiafiltrat* or Dialysis or hemodialysis or haemodialysis).ti,ab. (130690) 9 7 or 8 (153364) 10 6 and 9 (918) 11 (prophyla* or prevent*).ti,ab. or pc.fs. (1907859) 12 10 and 11 (356) 13 limit 12 to (english language and yr="1995 -Current") (302) 14 (meta-analysis/ or meta-analysis as topic/ or (meta adj analy$).tw. or ((systematic* or literature) adj2 review$1).tw. or (systematic adj overview$1).tw. or exp "Review Literature as Topic"/ or cochrane.ab. or cochrane.jw. or embase.ab. or medline.ab. or (psychlit or psyclit).ab. or (cinahl or cinhal).ab. or cancerlit.ab. or ((selection criteria or data extraction).ab. and "review"/)) not (Comment/ or Editorial/ or Letter/ or (animals/ not humans/)) (254827) 15 13 and 14 (59) 16 (exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).mp. or comparative study.pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw.) not (animals/ not humans/) [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (2605774) 17 13 and 16 (149) 18 The prevention of radiocontrast-agent-induced nephropathy by hemofiltration.m_titl. (1) 19 Effects of two different treatments with continuous renal replacement therapy in patients with chronic renal dysfunction submitted to coronary invasive procedures.m_titl. (1) 20 "Renal replacement therapies for prevention of radiocontrast-induced nephropathy: a systematic review.".m_titl. (1) 21 18 or 19 or 20 (3) 22 15 or 17 (166) 23 21 and 22 (3) 24 17 not 15 (107) 25 remove duplicates from 15 (56) 26 remove duplicates from 24 (104) |
194 |
|
Embase |
'contrast induced nephropathy'/exp/dm_pc OR ((contrast* OR ci) NEAR/2 (nephropath* OR 'kidney injury' OR aki OR nephrotoxicity)):ab,ti OR ciaki:ab,ti OR ('contrast medium'/exp OR (contrast NEAR/3 iodine):ab,ti OR (contrast NEAR/3 medi*):ab,ti AND ('kidney disease'/exp OR 'kidney function'/exp OR (kidney NEAR/2 (disease* OR injur* OR failure*)):ab,ti OR nephropath*:ab,ti OR (renal NEAR/2 (insufficienc* OR function* OR disease* OR failure*)):ab,ti)) AND [english]/lim AND [1995-2015]/py AND ('hemofiltration'/exp/mj OR 'hemodialysis'/exp/mj OR hemofiltrat*:ab,ti OR haemofiltrat*:ab,ti OR haemodiafiltrat*:ab,ti OR hemodiafiltrat*:ab,ti OR hemodialysis:ab,ti OR haemodialysis:ab,ti) AND ('prophylaxis'/exp OR prophyla*:ab,ti OR prevent*:ab,ti OR prevention:lnk)
'meta analysis'/de OR cochrane:ab OR embase:ab OR psychlit:ab OR cinahl:ab OR medline:ab OR (systematic NEAR/1 (review OR overview)):ab,ti OR (meta NEAR/1 analy*):ab,ti OR metaanalys*:ab,ti OR 'data extraction':ab OR cochrane:jt OR 'systematic review'/de NOT ('animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp NOT 'human'/exp)) (26) – 9 uniek
AND ('clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti) NOT 'conference abstract':it - (57) – 25 uniek |
