Chirurgische interventies bij vrouwen met stressincontinentie
Uitgangsvraag
Welke (minimaal) chirurgische interventie (synthetische suburethrale slings, fascie slings en het injecteren van bulkmaterialen) heeft de voorkeur bij vrouwen met stressincontinentie?
Aanbeveling
Aanbeveling-1
Bied vrouwen met stress urine-incontinentie een midurethrale sling aan als chirurgische behandeling. Er is geen bewijs voor superioriteit van een van de type slings.
Neem in de counseling voorafgaande aan de ingreep de specifiek bij deze interventie behorende complicaties en voor- en nadelen mee.
Welke chirurgische route wordt gekozen is een individuele afweging die op basis van patiëntkarakteristieken en ervaring van de operateur in samenspraak met de patiënt dient te worden gemaakt.
Aanbeveling-2
Bied vrouwen met stress urine-incontinentie die een zo minimaal mogelijk invasieve ingreep wensen bulking agents aan, met daarbij de opmerking dat dit minder effectief is, herhaal injecties nodig kunnen zijn en lange termijn resultaten nog niet bekend zijn.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
In totaal zijn er twee systematische reviews en vijf additionele RCTs beschreven in de literatuursamenvatting waarin een chirurgische interventie bij vrouwen met stressincontinentie wordt vergeleken met een andere chirurgische interventie. De geselecteerde studies bevatten over het algemeen een kleine studiepopulatie en vergelijken verschillende behandelingen. Indien mogelijk zijn de uitkomsten gepoold o.b.v. de definitie die is gesteld in het artikel van Imamura (2019) per vergelijking. Door deze beperkingen is de overall bewijskracht zeer laag, mede veroorzaakt door het aantal vergelijken waarbij soms slechts 1 studie (met een kleine studie populatie) is geïncludeerd.
Wanneer we specifiek naar de verschillende vergelijkingen kijken, kunnen we stellen dat retropubische, transobturator, single incision en fasciale slings even effectief zijn. De retropubische sling is effectiever in vergelijking met de interventie bulking agents bij vrouwen met stress-urine incontinentie op korte tot middellange termijn (12 maanden). De verschillen in uitkomsten tussen retropubische, transobturator en single incision slings zijn klein.
De uitkomstmaten complicaties en bijwerkingen zijn over het algemeen vaker gemeten in studies met een sling-interventie dan bij de andere vergelijkingen. Deze resultaten zijn inconsistent (d.w.z. de complicaties worden inconsistent bijgehouden) met brede 95% CI. Om een conclusie te geven m.b.t. complicaties en bijwerkingen is het noodzakelijk dat individuele studies gebruik maken van dezelfde gestandaardiseerde meetinstrumenten om uitkomsten tussen de studies te kunnen vergelijken.
De uitkomstmaat kwaliteit van leven geeft voor iedere behandeling een verbetering, maar over het verschil van deze verbetering bij de verschillende interventies kan geen conclusie worden getrokken. Slechts in enkele vergelijkingen van de huidige literatuursamenvatting wordt dit bestudeerd, omdat deze uitkomst niet is gerapporteerd in de SR van Imamura (2019). Deze uitkomstmaat wordt benoemd als kennislacune.
De klassieke retropubische- en transobturator slings zijn vergelijkbaar in uitkomsten en succespercentage, waarbij de uitkomsten verschillen t.a.v. liespijn, operatieduur en kans op blaasletsel. In de review van Imamura (2019) is de tension free vaginal tape (TVT)-secur is meegenomen in de vergelijkingen. Dit is een single incision sling waarvan de effectiviteit bewezen laag is. De TVT-secur is daarom ook niet meer op de markt. Met die reden kan de werkgroep dan ook geen goed antwoord geven met betrekking tot de effectiviteit van overige single incision slings. De werkgroep benadrukt dat nog slechts enkele typen (single incision) slings worden gebruikt in de Nederlandse praktijk. Het is gebleken uit de literatuur dat de wijze van verankering van de single incision sling grote invloed kan hebben op de uitkomsten. Dit is in mindere mate het geval bij de klassieke sling zonder verankeringsmechanisme (retropubisch dan wel transobturator) (Nambiar, 2014). Momenteel worden er geen studies uitgevoerd in de Nederlandse praktijk om dit hiaat te duiden. Dit punt wordt benoemd als kennislacune.
In de huidige literatuursamenvatting wordt injectie van bulkmaterialen in slechts 1 vergelijking meegenomen. Er is sinds 2011 geen nieuw vergelijkend onderzoek gepubliceerd m.b.t. injectie van bulkmaterialen versus midurethrale slings (Kirchin, 2017). Dit wordt beschouwd als een kennislacune. Andere internationale richtlijnen bevelen aan om aan vrouwen met stress urine-incontinentie die een zo min mogelijk invasieve ingreep wensen bulking agents aan te bieden (EAU Guidelines, 2022). De werkgroep merkt daarbij op dat dit minder effectief is, herhaal injecties nodig kunnen zijn en lange termijn resultaten nog niet bekend zijn.
Wij zien in de huidige Nederlandse praktijkvoering dat de laparoscopische en open colposuspensie niet frequent meer wordt uitgevoerd als eerste keuze van de chirurgische behandeling van stressincontinentie. Mogelijk is het een behandel optie voor residu- of recidief stressincontinentie, maar deze indicatie valt buiten de scoop van deze richtlijn.
De plaats van deze hoog complexe ingreep versus de laag complexe mogelijkheden in de vorm van midurethrale slings of bulking agents maakt dat de colposuspensie meer op de achtergrond is komen te staan. De werkgroep erkent dat in landen waar midurethrale slings op dit moment niet zijn toegestaan er internationale hernieuwde aandacht is voor de colposuspensie.
Voor- en nadelen interventies:
In de literatuur wordt beschreven dat het belangrijk is om alle voor- en nadelen van de verschillende chirurgische interventies met de patiënt te bespreken, zowel op de korte als op de lange termijn (Amin, 2018). De werkgroep heeft een overzichtstabel gemaakt, Tabel 1.
Tabel 1. Voordelen en nadelen van verschillende chirurgische interventies.
|
Interventie |
Voordelen |
Nadelen |
|
Retropubische sling |
Veel ervaring, mogelijk beter effect bij intrinsiek sfincter defect, effectief bij langdurige follow-up. |
Meer kans op blaas perforatie, langere operatieduur. Standaard cystoscopie |
|
Transobturator sling |
Minder kans op blaas-perforatie, geen standaard cystoscopie, bewezen effectief bij langdurige follow-up |
Meer kans op (lies)pijnklachten. |
|
Single incision sling |
Minder kans op blaas-perforatie, geen standaard cystoscopie. Mogelijk minder pijn, kortere operatieduur (sedatie mogelijkheid). |
Geen lange termijn follow-up in reviews. |
|
Bulking agents |
Geen narcose, korte ingreep Geen mesh materiaal Geen pijn |
Minder effectief.
|
|
Fasciale sling |
Geen mesh materiaal |
Even effectief, grotere ingreep met groter complicatie risico. |
Waarden en voorkeuren van patiënten (en eventueel hun verzorgers)
Het belangrijkste doel van de behandeling van stressincontinentie is geen of minder verlies van urine te hebben bij fysieke inspanning of bij verhoogde intra-abdominale druk met een zo gering mogelijk risico op complicaties ten gevolge van deze behandeling. De keuze voor behandeling wordt in eerste instantie bepaald door de hinder die de patiënt ervaart van haar urineverlies. Daarnaast zal de patiënt na uitvoerig te zijn geïnformeerd over de behandelingsmogelijkheden zelf de afweging moeten maken welke behandeling geschikt is voor haar. Uit literatuur is gebleken dat patiënten op basis van persoonlijke afwegingen niet altijd kiezen voor de behandeling met het hoogste succespercentage (Casteleijn, 2018). Tevens beïnvloedt de kans op postoperatieve pijn ook de keuze van de patiënt (Itkonen Freitas, 2019). Alle vormen van midurethrale sling kunnen worden verricht in dagbehandeling, sommige slings kunnen ook worden verricht onder sedatie en bulking agents kunnen poliklinisch (onder lokale verdoving) worden toegepast. Dat kan allemaal meewegen in de keuze die de patiënt maakt.
Aanvaardbaarheid, haalbaarheid en implementatie
De werkgroep is van mening dat de chirurgische behandeling van stressincontinentie m.b.v. mesh in de afgelopen jaren een aanzienlijke verandering heeft ondergaan: de aandacht voor de negatieve gevolgen van de mesh chirurgie (met name hernia chirurgie en POP) heeft ertoe geleid dat het aantal uitgevoerde operaties is afgenomen en dat het aantal operateurs dat deze chirurgie verricht, zowel gynaecologen als urologen, is afgenomen. Er wordt een verschuiving gezien richting de minislings, mogelijk omdat hierbij met minder mesh wordt gewerkt. Bovendien kan het zijn dat verankering van de sling binnen het kleine bekken zorgt voor sneller postoperatief herstel.
Er is geen wetenschappelijk bewijs voor superioriteit van één van de type slings. De retropubische versus de transobturator route of van de single incision versus de niet-single incision sling. Dat betekent dat de ervaring van de operateur van belang is op de effectiviteit en veiligheid en dat het wenselijk is dat iedere operateur inzicht kan geven in de eigen behandelresultaten. Bij de voorlichting van de patiënt over een invasieve behandeling voor stressincontinentie zal naast de sling chirurgie ook de bulkinjectietherapie moeten worden besproken en kan als de behandelaar deze techniek beheerst ook de fascie sling worden besproken.
Rationale van de aanbeveling
Behandel vrouwen met stress urine-incontinentie als een chirurgische interventie gewenst is bij voorkeur met het plaatsen van een midurethrale sling. Daarbij moeten vrouwen worden gecounseld over de te verwachten succespercentages, mogelijke complicaties en lange termijn uitkomsten. Over de keuze van het type sling dient transparant te worden gecounseld, waarbij voorkeur en ervaring van de operateur ook meetellen. Een retropubische sling of een single incision sling verdienen de voorkeur. De werkgroep constateert dat er bij gebruik van single incision slings minder postoperatieve pijnklachten zijn, minder mesh wordt gebruikt en er bij klachten een betere mogelijkheid tot volledige excisie is, met maar kleine verschillen in effectiviteit ten opzichte van transobturator tapes. Daarbij is de kans op blaasletsel bij een single-incision sling kleiner dan bij een retropubische sling waardoor er geen cystoscopie gedaan hoeft te worden en de operatietijd korter is. Hierbij wordt wel erkend dat er nog geen lange termijn resultaten zijn gepubliceerd.
Urethrale bulktherapie kan ook aangeboden worden als eerst behandelkeuze, met name bij vrouwen die een zo minimaal mogelijk invasieve ingreep wensen, een kinderwens hebben of bij kwetsbare ouderen. Echter is deze behandeling minder effectief, zijn herhaal injecties mogelijk nodig en zijn de lange termijn uitkomsten nog niet bekend.
Onderbouwing
Achtergrond
Uit een Nederlandse RCT is gebleken dat counseling voor een directe chirurgische behandeling bij stressincontinentie op zijn plaats is bij matig tot ernstige urine-incontinentie (Labrie, 2013). In de huidige situatie worden diverse midurethrale slings gebruikt als primaire chirurgische interventie voor stress-urine-incontinentie (SUI), ook kunnen bulking agents worden toegepast. Er is nog geen eenduidig advies over de plaats van autologe fascieslings voor stress urine-incontinentie. De laparoscopische en open colposuspensie worden niet frequent meer uitgevoerd als eerste keuze van de chirurgische behandeling van stressincontinentie.
Op dit moment is er veel praktijk variatie in het gebruik van de soort sling en de keus van de chirurgische route. Ook is er veel discussie in de media over het gebruik van mesh, zowel bij urine-incontinentie als prolapschirurgie. De effectiviteit en veiligheid van de midurethrale sling zijn goed onderzocht en gedocumenteerd. We willen een eenduidig advies kunnen geven over de chirurgische interventies bij SUI. Daarbij wordt in deze PICO bewust alleen naar de gangbare chirurgische interventies gekeken en niet naar bekkenfysiotherapie.
Conclusies / Summary of Findings
1. Transobturator MUS vs. retropubic MUS
Conclusions
|
Low GRADE |
The evidence suggests that transobturator MUS intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Elers, 2021; Imamura, 2019; Palos, 2018. |
|
Low GRADE |
The evidence suggests that a transobturator MUS intervention results in an increase in repeated surgery when compared to a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Moderate GRADE |
The risk on major vascular complications or voiding difficulty is probably lower in women with stress urinary incontinence treated with a transobturator MUS intervention, compared to a retropubic MUS intervention.
Sources: Imamura, 2019 |
|
Very low GRADE |
The evidence is uncertain about the effect of a transobturator MUS intervention on major bladder or urethral perforation when compared with a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019; Palos, 2018 |
|
Very low GRADE |
Evidence is uncertain about effects on de novo symptoms of urgency, perioperative complications or tape/mesh erosion or extrusion in women with stress urinary incontinence treated with a transobturator MUS intervention, compared to a retropubic MUS intervention.
Sources: Imamura, 2019 |
|
Moderate GRADE |
Operation time is probably shorter in women with stress urinary incontinence treated with a transobturator MUS intervention, compared to a retropubic MUS intervention.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that transobturator MUS intervention results in little to no clinically relevant difference in hospital stay when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that transobturator MUS intervention results in little to no clinically relevant difference in quality of life when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Palos, 2018 |
2. Fascial sling vs. retropubic MUS
Conclusions
|
Low GRADE |
The evidence suggests that fascial sling intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Very low GRADE |
Evidence is uncertain about the effect of a fascial sling intervention, compared to a retropubic MUS intervention on voiding difficulty in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that a fascial sling intervention results in a reduced risk on de novo symptoms or bladder or urethral perforation when compared to a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a fascial sling intervention, compared to a retropubic MUS intervention, in women with stress urinary incontinence on repeated surgery, operation time, hospital stay, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
3. Single incision sling vs. retropubic MUS
Conclusions
|
Low GRADE |
The evidence suggests that a single incision sling intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Very low GRADE |
Evidence is uncertain about the effect of a single incision sling intervention, compared to a retropubic MUS intervention, on voiding difficulty, bladder or urethral perforation, tape/mesh erosion or extrusion in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a single incision sling intervention, compared to a retropubic MUS intervention, in women with stress urinary incontinence on repeated surgery, operation time, hospital stay, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
4. Fascial sling vs. transobturator MUS
Conclusions
|
Low GRADE |
The evidence suggests that fascial sling intervention results in little to no clinically relevant difference in improving and/or curing symptoms related to stress incontinence when compared with a transobturator MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a fascial sling intervention, compared to a transobturaor MUS intervention, in women with stress urinary incontinence is on repeated surgery, operation time, hospital stay, adverse events, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
5. Single incision sling vs. transobturator MUS
Conclusions
|
Low GRADE |
The evidence suggests that a single incision sling intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a transobturator MUS in women with stress urinary incontinence.
Sources: Imamura, 2019; Maturana, 2020; Tieu, 2017 |
|
Very low GRADE |
The evidence is very uncertain about the risk on repeated surgery in women with stress urinary incontinence treated with single incision sling, compared to transobturator MUS.
Sources: Imamura, 2019 |
|
Very low GRADE |
The evidence is very uncertain about the risk on adverse events in women with stress urinary incontinence treated with single incision sling, compared to transobturator MUS.
Sources: Imamura, 2019 |
|
Low GRADE |
A single incision sling intervention may reduce the operation time when compared with a transobturator MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that a single incision sling intervention results in little to no clinically relevant difference in quality of life when compared with a transobturator MUS in women with stress urinary incontinence.
Sources: Maturana, 2020; Tieu, 2017 |
|
No GRADE |
No conclusion could be drawn about the effect of a single incision sling intervention, compared to a transobturaor MUS intervention, in women with stress urinary incontinence on hospital stay. This outcome measure was not studied in the included studies.
Sources: - |
6. Single incision sling vs. fascial sling
Conclusions
|
Very low GRADE |
The evidence is very uncertain about the effect of a single incision sling intervention, compared to a fascial sling intervention, in improving symptoms related to stress incontinence in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a single incision sling intervention, compared to a fascial sling intervention, in women with stress urinary incontinence on repeated surgery, operation time, hospital stay, adverse events, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
7. Urethral injection therapy vs. fascial sling
No data was available for this comparison since this was not provided by Imamura (2019).
8. Urethral injection therapy vs. retropubic MUS
Conclusions
|
Low GRADE |
The evidence suggests that a urethral injection therapy resulted in a lower cure rate and/or improvement of symptoms rate when compared with a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Itkonen Freitas, 2020 |
|
Very low GRADE |
The evidence is very uncertain about the effect of urethral injection therapy, compared to a retropubic MUS intervention, on adverse events (i.e., de novo symptoms, voiding difficulty, bladder or urethral perforation) in women with stress urinary incontinence.
Sources: Itkonen Freitas, 2020 |
|
Low GRADE |
The evidence suggests that a urethral injection therapy results in little to no clinically relevant difference in quality of life when compared with retropubic MUS intervention in patient population in women with stress urinary incontinence.
Sources: Itkonen Freitas, 2021 |
|
No GRADE |
No conclusion could be drawn about the effect of urethral injection therapy intervention, compared to a retropubic MUS intervention, in women with stress urinary incontinence on repeated surgery, operation time, or hospital stay. This outcome measure was not studied in the included studies.
Sources: - |
Samenvatting literatuur
Description of studies
The systematic review by Imamura (2019) investigated the effectiveness and safety of several surgical interventions for women with stress urinary incontinence. RCTs evaluating surgical intervention for treatment in women with stress urinary incontinence, were eligible for inclusion. The Cochrane Central Register of Controlled Trials (CENTRAL), Medline, Medline In-Process, Medline Epub Ahead of Print, CINAHL, ClinicalTrials.gov and WHO ICTRP, were searched to identify relevant studies until June 2017. The reference lists of relevant articles were also searched. Primary outcomes were “cure”, defined as resolution of incontinence symptoms, and “improvement”, defined as any improvement in incontinence symptoms from baseline, both at 12 months. Secondary outcomes were the number of women having repeated surgery for incontinence symptoms, adverse events, length of hospital stay, and operation time during the study period as reported by the trial investigators.
Data of 175 studies were included, 145 studies were from Cochrane reviews and 28 from additional searches. In total 21 intervention comparisons were made, see Table 1. Since two of the comparisons included only one surgical intervention arm, these comparisons were excluded from our analyses.
If possible, data was directly compared to estimate an overall odds ratio (OR) per comparison.
Table 1. Number of included studies per comparison, Imamura (2019)
|
Control group |
Intervention group |
Total number of randomized |
Number of studies |
|
Retropubic MUS |
Transobturator MUS |
8876 |
62 |
|
Retropubic MUS |
Open colposuspension |
1240 |
13 |
|
Retropubic MUS |
Laparoscopic colposuspension |
651 |
8 |
|
Retropubic MUS |
Fascial sling |
868 |
9 |
|
Retropubic MUS |
1092 |
12 |
|
|
Transobturator MUS |
Open colposuspension |
272 |
4 |
|
Transobturator MUS |
Laparoscopic colposuspension |
35 |
1 |
|
Transobturator MUS |
Fascial sling |
141 |
4 |
|
Transobturator MUS |
Single incision sling |
4612 |
56 |
|
Open colposuspension |
Laparoscopic colposuspension |
1402 |
12 |
|
Open colposuspension |
Fascial sling |
922 |
7 |
|
Open colposuspension |
Single incision sling |
639 |
7 |
|
Fascial sling |
Single incision sling |
72 |
2 |
|
Fascial sling |
Urethral injection therapy |
45 |
1 |
|
Fascial sling |
Bladder neck needle suspension |
20 |
1 |
MUS=mid-urethral sling
Elers (2021) performed a SR to investigate the effectiveness and safety after bottom-up tension-free vaginal tape (TVT) and inside-out tension-free vaginal tape - obturator (TVT-O) in the treatment of stress urinary incontinence in women. RCTs evaluating TVT compared to TVT-O for treatment in women with stress urinary incontinence, were eligible for inclusion. Medline, Embase, Cochrane Library, Cinahl, Guideline International network (GIN), Trip
Database and NICE (UK), were searched to identify relevant studies until January 2020. Primary outcomes were incontinence related quality of life, patient perceived effect, and re-operation evaluated at longest follow-up, minimum six months. Secondary outcomes were number of incontinence episodes, de novo urgency incontinence, leg pain, pelvic pain, de novo dyspareunia and change in sexual function evaluated at longest follow-up, minimum six months and infection and haematoma evaluated in 30 days postoperatively and bladder perforation evaluated perioperatively.
Data of 22 studies were included, 2 (Zhang, 2016; Feng, 2018) of them were not included in the study of Imamura (2019).
In addition, 5 RCTs were included. A short description is provided below.
Tieu (2017) investigated the effect of a single incision sling placement for treatment of stress urinary incontinence compared to transobturator sling placement in a RCT. Outcomes after 12 months were described for stress incontinence (i.e., voiding diary (total SUI episodes over 3 days), and self-reported ‘cured’), and quality of life (i.e., UDI-scores). In total, 98 patients were randomized to the transobturator group (n=49) or the single incision group (n=49). No differences were shown between the two groups at baseline. The study was limited by some aspects; it was a single centre study and patients, and assessors were not blinded to the treatment arm.
Palos (2018) investigated the efficacy and safety of a transobturator sling for treatment of stress urinary incontinence compared to a retropubic sling placement in a RCT. The efficacy was evaluated 12 months after surgery in terms of objective and subjective cure. Objective cure was defined as a negative pad test, i.e., pad-weight difference <2 g. Subjective cure was defined as the absence of patient complaints of SUI and patient satisfaction after surgery. Data about quality of life (i.e., measured with the UDI-6) and post-operative complications was also reported. In total, 92 patients underwent surgery, 47 were allocated to the transobturator group and 45 to the retropubic group. No differences were shown at baseline. The relatively small sample size of the study was a limitation.
Maturana (2020) investigated the effects of a single-incision mini sling for treatment of stress urinary incontinence compared to a transobturator sling placement in a RCT. The efficacy was evaluated 12 months after surgery in terms of objective and subjective cure. The subjective UI cures were evaluated through clinical complaints, and objective cures were evaluated by the simplified pad test. Data about quality of life (i.e., measured with the UDI-6) and post-operative complications was also reported. In total, 105 patients underwent surgery, 58 were allocated to the single-incision mini sling group and 47 to the transobturator group. No differences were shown at baseline. The small sample size of the study was a limitation.
Itkonen Freitas (2020;2021) investigated the effects of polyacrylamide hydrogel injection for treatment of stress urinary incontinence compared to a retropubic sling placement in a RCT. Objective and subjective cure outcomes were reported, even as perioperative complications (Itkonen Freitas, 2020). The 2021 publication by Itkonen Freitas reported outcomes on quality of life (i.e., measured with UDI-6). In total, 224 patients underwent treatment. Of them 113 were allocated to the injection group and 111 to the retropubic group. During the follow-up of 1 year some patients were lost to follow-up. Therefore, the intention to treat analysis included 107/113 patients in the injection group and 101/111 patients in the retropubic group.
Results
Data were extracted from the study of Imamura (2019), Elers (2021), Tieu (2017), Palos (2018), Maturana (2020) and Itkonen Freitas (2020;2021). Meta-analyses were performed where possible. All analyses were performed separately for different surgical interventions, as described in Table 1.
Outcomes were defined as follow in the ESTER SR (Imamura, 2019):
- ‘Cure of stress urinary incontinence symptoms; as resolution of incontinence symptoms. As a variety of measures were used to define cure, data based on a hierarchy of reported outcomes was combined. For cure, women’s self-report (subjective measure) was given priority if available, followed by a composite measure of self-report and objective indicators, and then by pad tests and urodynamic investigations (objective measures)’.
- ‘Improvement of stress urinary incontinence symptoms; as resolution of incontinence symptoms. As a variety of measures were used to define improvement, data based on a hierarchy of reported outcomes was combined. For improvement, women’s self-report
was preferred when available, followed by women’s satisfaction, pad tests, and urodynamic investigations. Cough stress tests and diaries were not considered reliable measures and were excluded. We considered assessments performed at 12 months or closest to 12 months as well as longer term assessments when available. We excluded studies if they only reported assessments within two weeks post-surgery’.
- ‘The number of women having repeated surgery for incontinence symptoms’.
- ‘Adverse events; major vascular complications, de novo symptoms, voiding difficulty, bladder or urethral perforation, tape/mesh erosion or extrusion, perioperative complications’.
- ‘Length of hospital stay; as reported by the trial investigators, in days’.
- ‘Operation time during the study period; as reported by the trial investigators, in minutes’.
As ORs were reported in the study of Imamura (2019), and relative risks (RRs) were of interest, it was first investigated if ORs were equal to RRs. This was not shown for the outcomes cure and improvement, since the “events” were common. For the other outcomes (e.g., adverse events) events were rare, and therefore the ORs could be interpretated as RRs. For continuous outcomes, standardized mean differences were adapted from the study of Imamura (2019).
The following comparisons are reported in the summary of literature:
1. Transobturator mid-urethral sling (MUS) vs. retropubic MUS
2. Fascial (i.e., traditional) sling vs. retropubic MUS
3. Single incision sling vs. retropubic MUS
4. Fascial sling vs. transobturator MUS
5. Single incision sling vs. transobturator MUS
6. Single incision sling vs. fascial sling
7. Urethral injection therapy vs. fascial sling
Additional data from the RCTs was added to the described comparison, and one comparison was added.
8. Urethral injection therapy vs. retropubic MUS
If possible, outcomes of the SRs and RCTs were pooled. In some analyses a reference is made to the article of ESTER SR (Brazzelli, 2019). The figures are provided in the article.
1. Transobturator MUS vs. retropubic MUS
1.1 Cure of stress urinary incontinence symptoms.
Data on cure of stress urinary incontinence symptoms were extracted from SRs and supplemented with RCTs.
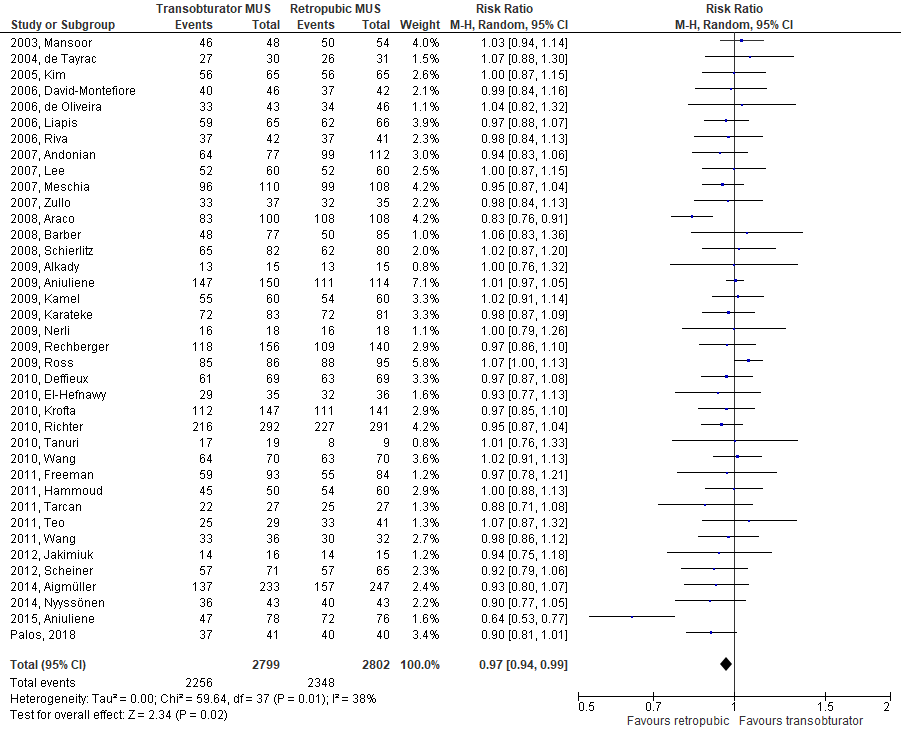
In women with stress urinary incontinence, a transobturator MUS intervention was slightly less effective for curing symptoms compared to a retropubic MUS intervention at post-test, the pooled RR was 0.97 (95%CI 0.95 to 0.99), based on evidence from 38 trials, see Figure 1. The risk difference was -0.03 (95%CI -0.05 to -0.01).
Figure 1. Transobturator MUS vs. retropubic MUS: cure
1.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from SRs and supplemented with RCTs.
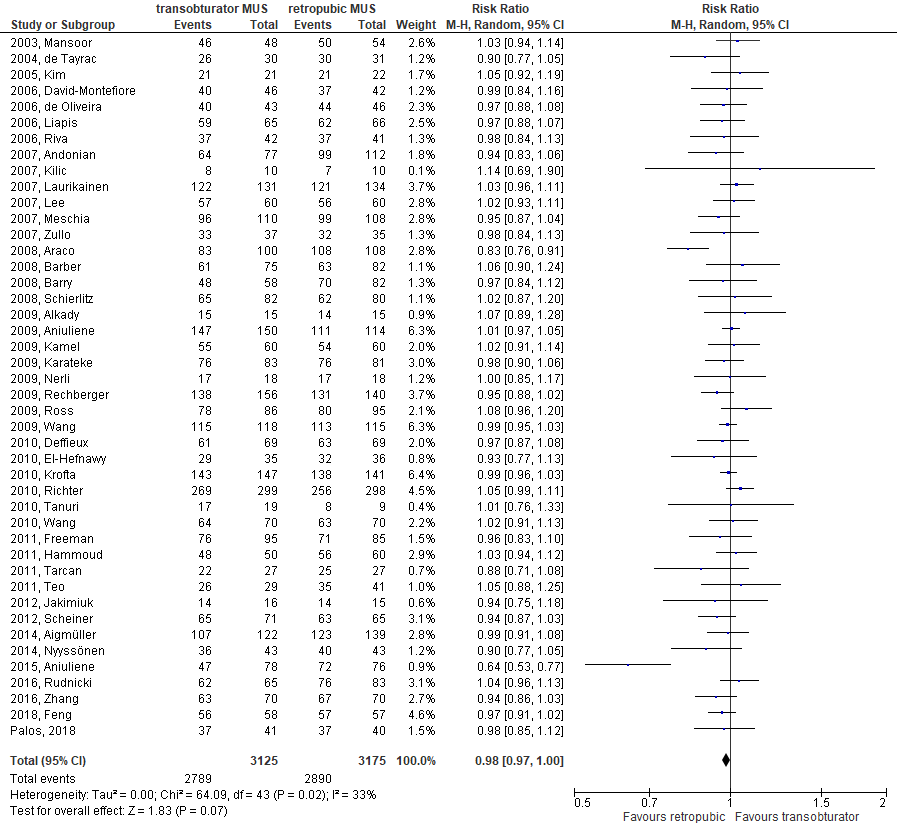
In women with stress urinary incontinence, transobturator MUS was slightly less effective for improving symptoms compared to retropubic MUS at post-test, the pooled RR was 0.98 (95%CI 0.96 to 1.00), based on evidence from 44 trials, see Figure 2. The risk difference was -0.02 (95%CI -0.04 to 0.00).
Figure 2. Transobturator MUS vs. retropubic MUS: improvement.
In the following sections (i.e., 1.3 and 1.4) ORs could be interpretated as RRs, since events were rare.
1.3 Repeated surgery
Data on repeated surgery were extracted from SR.
Analyses based on repeated surgery were performed, please see Figure 47 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, repeated surgery within 12 months was slightly more common in transobturator MUS compared to retropubic MUS, the pooled OR was 1.37 (95%CI 0.55 to 3.46), based on evidence from 7 trials.
In women with stress urinary incontinence, repeated surgery after 60 months was more common in transobturator MUS compared to retropubic MUS, the pooled OR was 4.06 (95%CI 0.80 to 20.74), based on evidence from 5 trials.
1.4 Adverse events
Data on adverse events were extracted from SR.
1.4.1 Adverse events – major vascular complications
Analyses based on adverse events (major vascular complications) were performed, please see Figure 49 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, major vascular complications were less common in transobturator MUS compared to retropubic MUS, the pooled OR was 0.36 (95%CI 0.21 to 0.64), based on direct evidence from 22 trials.
1.4.2 Adverse events – de novo symptoms
Analyses based on adverse events (de novo symptoms) were performed, please see Figure 51 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, de novo symptoms within 12 months were slightly less common in transobturator MUS compared to retropubic MUS, the pooled OR was 0.93 (95%CI 0.74 to 1.17), based on direct evidence from 28 trials.
1.4.3 Adverse events – voiding difficulty
Analyses based on adverse events (voiding difficulty) were performed, please see Figure 53 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, voiding difficulty was less common in transobturator MUS compared to retropubic MUS, the pooled OR was 0.51 (95%CI 0.40 to 0.64), based on direct evidence from 36 trials.
1.4.4 Adverse events – bladder or urethral perforation
Analyses based on adverse events (bladder or urethral perforation) were performed, please see Figure 54 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, bladder or urethral perforation was less common in transobturator MUS compared to retropubic MUS, the pooled OR was 0.15 (95%CI 0.09 to 0.24), based on direct evidence from 38 trials.
Palos (2018) reported that bladder perforation in 1/41 (2%) in the transobturator MUS group compared to 1/40 (2%) in the retropubic MUS group, without being significant different.
1.4.5 Adverse events – tape/mesh erosion or extrusion
Analyses based on adverse events (tape/mesh erosion or extrusion) were performed, please see Figure 55 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, tape/mesh erosion or extrusion were more common in transobturator MUS compared to retropubic MUS, the pooled OR was 1.10 (95%CI 0.71 to 1.70), based on direct evidence from 27 trials.
1.4.6 Adverse events – perioperative complications
Analyses based on adverse events (perioperative complications) were performed, please see Figure 63 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, perioperative complications were less common in transobturator MUS compared to retropubic MUS, the pooled OR was 0.81 (95%CI 0.55 to 1.19), based on direct evidence from 15 trials.
1.5 Operation time
Data on operation time were extracted from SR.
Analyses for the outcome operation time were performed, please see Figure 64 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, operation time was less in transobturator MUS compared to retropubic MUS, the pooled standardized mean difference was -1.02 (95%CI -1.29 to -0.74), based on direct evidence from 32 trials.
1.6 Hospital stay
Data on hospital stay were extracted from SR.
Analyses for the outcome hospital stay were performed, please see Figure 64 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, hospital stay was less in transobturator MUS compared to retropubic MUS, the pooled standardized mean difference was -0.38 (95%CI -0.70 to -0.06), based on direct evidence from 17 trials.
1.7 Quality of life
Palos (2018) measured quality of life with the UDI-6. Median scores were reported per treatment group before and after surgery. Median pre/post UDI-6 were 41.7/0 vs. 33.3/0 for transobturator MUS vs. retropubic MUS. These differences were not statistically significant.
It was not possible to calculate SMD, as only the median was reported.
Level of evidence of the literature
The level of evidence (GRADE method) is determined per comparison and outcome measure and is based on results from RCTs and therefore starts at level “high”. Subsequently, the level of evidence was downgraded if there were relevant shortcomings in one of the several GRADE domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias.
The level of evidence regarding the crucial outcome measure stress incontinence (i.e., cure and improvement) was downgraded by 2 levels because of imprecision (1 level, no clinically relevant effect (RR 0.75-1.25)), and inconsistency.
The level of evidence regarding the outcome measure complication (i.e., repeated surgery) was downgraded by 2 levels because of imprecision (2 level, 95%CI of the mean difference includes no significant effect (OR=1), no clinically relevant effect (OR 0.75-1.25)).
The level of evidence regarding the outcome measure adverse events (major vascular complications, voiding difficulty) was downgraded by 1 level because of risk of bias (1 level, due to risk of bias in the included studies).
The level of evidence regarding the outcome measure adverse events (, bladder or urethral perforation) was downgraded by 3 levels because of risk of bias (1 level, due to risk of bias in the included studies), imprecision and inconsistency.
The level of evidence regarding the outcome measure adverse events (de novo symptoms, perioperative complications, tape/mesh erosion or extrusion) was downgraded by 3 levels because of risk of bias (1 level, due to risk of bias in the included studies) and imprecision (2 level, 95%CI of the mean difference includes no significant effect (OR=1) and/or no clinically relevant effect (OR 0.75-1.25)).
The level of evidence regarding the outcome measure complication (i.e., operation time) was downgraded by 1 level because of risk of bias (1 level, due to risk of bias in the included studies).
The level of evidence regarding the outcome measure complication (i.e., hospital stay) was downgraded by 2 levels because of risk of bias (1 level, due to risk of bias in the included studies) and imprecision (1 level, 95%CI of the mean difference includes no clinically relevant effect (SMD<0.5)).
The level of evidence regarding the outcome measure quality of life was downgraded by 2 levels because of risk of bias (1 level, due to the lost to follow-ups, and that assessors and patients were not blinded to the intervention) and imprecision (1 level, optimal information size was not achieved (small sample size)).
Conclusions
|
Low GRADE |
The evidence suggests that transobturator MUS intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Elers, 2021; Imamura, 2019; Palos, 2018. |
|
Low GRADE |
The evidence suggests that a transobturator MUS intervention results in an increase in repeated surgery when compared to a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Moderate GRADE |
The risk on major vascular complications or voiding difficulty is probably lower in women with stress urinary incontinence treated with a transobturator MUS intervention, compared to a retropubic MUS intervention.
Sources: Imamura, 2019 |
|
Very low GRADE |
The evidence is uncertain about the effect of a transobturator MUS intervention on major bladder or urethral perforation when compared with a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019; Palos, 2018 |
|
Very low GRADE |
Evidence is uncertain about effects on de novo symptoms of urgency, perioperative complications or tape/mesh erosion or extrusion in women with stress urinary incontinence treated with a transobturator MUS intervention, compared to a retropubic MUS intervention.
Sources: Imamura, 2019 |
|
Moderate GRADE |
Operation time is probably shorter in women with stress urinary incontinence treated with a transobturator MUS intervention, compared to a retropubic MUS intervention.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that transobturator MUS intervention results in little to no clinically relevant difference in hospital stay when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that transobturator MUS intervention results in little to no clinically relevant difference in quality of life when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Palos, 2018 |
2. Fascial sling vs. retropubic MUS
2.1 Cure of stress urinary incontinence symptoms.
Data on cure of stress urinary incontinence symptoms were extracted from SR.
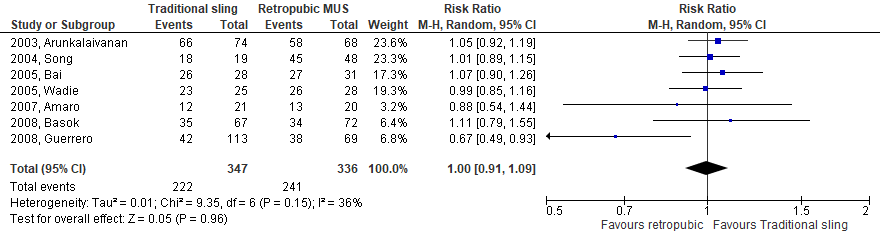
In women with stress urinary incontinence, no difference in effect for curing symptoms were shown between a fascial sling intervention and a retropubic MUS intervention at post-test, the pooled RR was 1.00 (95%CI 0.91 to 1.09), based on evidence from 7 trials, see figure 3. The risk difference was -0.01 (95%CI -0.07 to 0.06).
Figure 3. Fascial sling vs. retropubic MUS: cure.
2.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from SR.
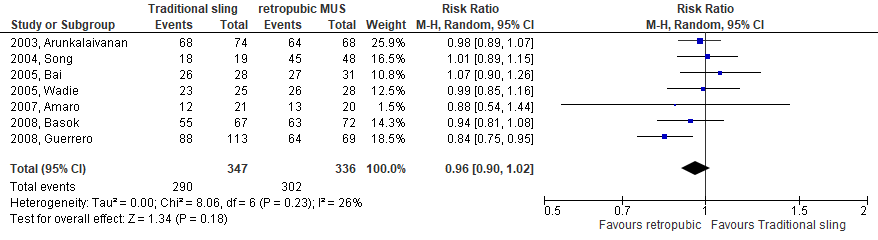
In women with stress urinary incontinence, no difference was found in effectivity of the fascial sling for improving symptoms compared to retropubic MUS at post-test. The pooled RR was 0.96 (95%CI 0.90 to 1.02), based on evidence from 7 trials, see figure 4. The risk difference was -0.04 (95%CI -0.09 to 0.01).
Figure 4. Fascial sling vs. retropubic MUS: improvement.
2.3 Adverse events
Data on adverse events were extracted from SR.
2.3.1 Adverse events – de novo symptoms
Analyses based on adverse events (de novo symptoms) were performed, please see Figure 51 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, de novo symptoms were more common in fascial sling compared to retropubic MUS, the pooled OR was 3.59 (95%CI 1.57 to 8.23), based on evidence from 4 trials.
2.3.2 Adverse events – voiding difficulty
Analyses based on adverse events (voiding difficulty) were performed, please see Figure 53 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, voiding difficulty was more common in fascial sling compared to retropubic MUS, the pooled OR was 1.46 (95%CI 0.84 to 2.53), based on evidence from 6 trials.
2.3.3 Adverse events – bladder or urethral perforation
Analyses based on adverse events (bladder or urethral perforation) were performed, please see Figure 54 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, bladder or urethral perforation was less common in fascial sling compared to retropubic MUS, the pooled OR was 0.50 (95%CI 0.26 to 0.98), based on evidence from 6 trials.
Level of evidence of the literature
The level of evidence regarding the outcome measures complications (i.e., repeated surgery, operation time, hospital stay), quality of life could not be assessed with GRADE. The outcome measures were not studied in the included studies.
The level of evidence regarding the outcome measure stress incontinence (i.e., cure and improvement) was downgraded by 2 level because of imprecision (1 level, 95%CI of the mean difference includes no significant effect (OR=1)) and inconsistency (1 level)
The level of evidence regarding the outcome measure adverse events (i.e., voiding difficulty) was downgraded by 3 levels because of risk of bias (1 level) and imprecision (2 level, 95%CI of the mean difference includes no significant effect (OR=1), no clinically relevant effect (OR 0.75-1.25), and wide 95%CI).
The level of evidence regarding the outcome measure adverse events (i.e., de novo symptoms, bladder or urethral perforation) was downgraded by 2 levels because of risk of bias (1 level), and imprecision (wide 95%CI).
Conclusions
|
Low GRADE |
The evidence suggests that fascial sling intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Very low GRADE |
Evidence is uncertain about the effect of a fascial sling intervention, compared to a retropubic MUS intervention on voiding difficulty in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that a fascial sling intervention results in a reduced risk on de novo symptoms or bladder or urethral perforation when compared to a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a fascial sling intervention, compared to a retropubic MUS intervention, in women with stress urinary incontinence on repeated surgery, operation time, hospital stay, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
3. Single incision sling vs. retropubic MUS
3.1 Cure of stress urinary incontinence symptoms.
Data on cure of stress urinary incontinence symptoms were extracted from SR.
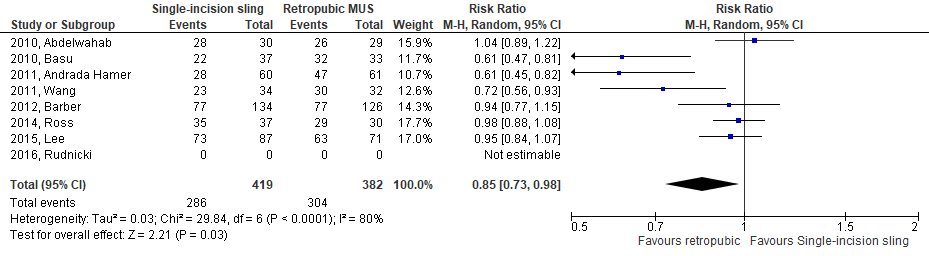
In women with stress urinary incontinence, a single incision sling intervention was slightly less effective for curing symptoms compared to a retropubic MUS intervention at post-test, the pooled RR was 0.85 (95%CI 0.73 to 0.98), based on evidence from 7 trials, see figure 5. The risk difference was -0.13 (95%CI -0.24 to -0.02).
Figure 5. Single incision sling vs. retropubic MUS: cure.
3.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from SR.
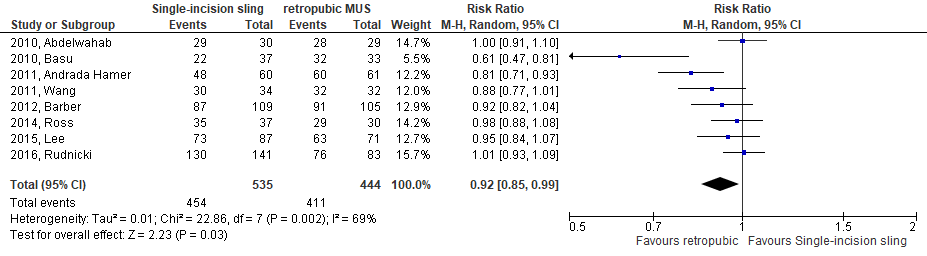
In women with stress urinary incontinence, single incision sling was slightly less effective for improving symptoms compared to retropubic MUS at post-test, the pooled RR was 0.92 (95%CI 0.85 to 0.99), based on evidence from 8 trials, see figure 6. The risk difference was -0.09 (95%CI -0.16 to -0.02).
Figure 6. Single incision sling vs. retropubic MUS: improvement.
3.3 Adverse events
Data on adverse events were extracted from SR.
3.3.1 Adverse events – voiding difficulty
Analyses based on adverse events (voiding difficulty) were performed, please see Figure 53 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, voiding difficulty was less common in single incision sling compared to retropubic MUS, the pooled OR was 0.39 (95%CI 0.09 to 1.69), based on direct evidence from only 3 trials.
3.3.2 Adverse events – bladder or urethral perforation
Analyses based on adverse events (bladder or urethral perforation) were performed, please see Figure 54 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, bladder or urethral perforation was less common in single incision sling compared to retropubic MUS, the pooled OR was 0.62 (95%CI 0.13 to 2.98), based on direct evidence from 4 trials.
3.3.3 Adverse events – tape/mesh erosion or extrusion
Analyses based on adverse events (tape/mesh erosion or extrusion) were performed, please see Figure 55 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, tape/mesh erosion or extrusion were more common in single incision sling compared to retropubic MUS, the pooled OR was 2.78 (95%CI 0.43 to 17.93), based on direct evidence from only 3 trials.
Level of evidence of the literature
The level of evidence regarding the outcome measures complications (i.e., repeated surgery, operation time, hospital stay), quality of life could not be assessed with GRADE. The outcome measures were not studied in the included studies.
The level of evidence regarding the outcome measure stress incontinence (i.e., cure and improvement) was downgraded by 2 levels because of imprecision (1 level, no clinically relevant effect (RR between 0.75-1.25)), and inconsistency (1 level).
The level of evidence regarding the outcome measure adverse events (i.e., voiding difficulty, bladder or urethral perforation, tape/mesh erosion or extrusion) was downgraded by 3 levels because of risk of bias (1 level) and imprecision (2 level, 95%CI of the mean difference includes no significant effect (OR=1), no clinically relevant effect (OR 0.75-1.25), and wide 95%CI).
Conclusions
|
Low GRADE |
The evidence suggests that a single incision sling intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a retropubic MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Very low GRADE |
Evidence is uncertain about the effect of a single incision sling intervention, compared to a retropubic MUS intervention, on voiding difficulty, bladder or urethral perforation, tape/mesh erosion or extrusion in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a single incision sling intervention, compared to a retropubic MUS intervention, in women with stress urinary incontinence on repeated surgery, operation time, hospital stay, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
4. Fascial sling vs. transobturator MUS
4.1 Cure of stress urinary incontinence symptoms.
Data on cure of stress urinary incontinence symptoms were extracted from SR.
In women with stress urinary incontinence, a fascial sling intervention was more effective for curing symptoms compared to a transobturator MUS intervention at post-test, the RR was 1.05 (95%CI 0.88 to 1.25), based on evidence from only 1 trial. The risk difference was 0.05 (95%CI -0.11 to 0.20).
4.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from SR and one RCT.
In women with stress urinary incontinence, fascial sling was more effective for improving symptoms compared to transobturator MUS at post-test, the RR was 1.05 (95%CI 0.88 to 1.25), based on evidence from only 1 trial. The risk difference was 0.05 (95%CI -0.11 to 0.20).
Level of evidence of the literature
The level of evidence regarding the outcome measures complications (i.e., repeated surgery, operation time, hospital stay), adverse events, quality of life could not be assessed with GRADE. The outcome measures were not studied in the included studies.
The level of evidence regarding the outcome measure stress incontinence (i.e., cure and improvement) was downgraded by 2 levels because of imprecision (2 levels, 95%CI of the mean difference includes no significant effect (RR=1) and not meeting OIS).
Conclusions
|
Low GRADE |
The evidence suggests that fascial sling intervention results in little to no clinically relevant difference in improving and/or curing symptoms related to stress incontinence when compared with a transobturator MUS in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a fascial sling intervention, compared to a transobturaor MUS intervention, in women with stress urinary incontinence is on repeated surgery, operation time, hospital stay, adverse events, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
5. Single incision sling vs. transobturator MUS
5.1 Cure of stress urinary incontinence symptoms.
Data on cure of stress urinary incontinence symptoms were extracted from SR and two RCTs.
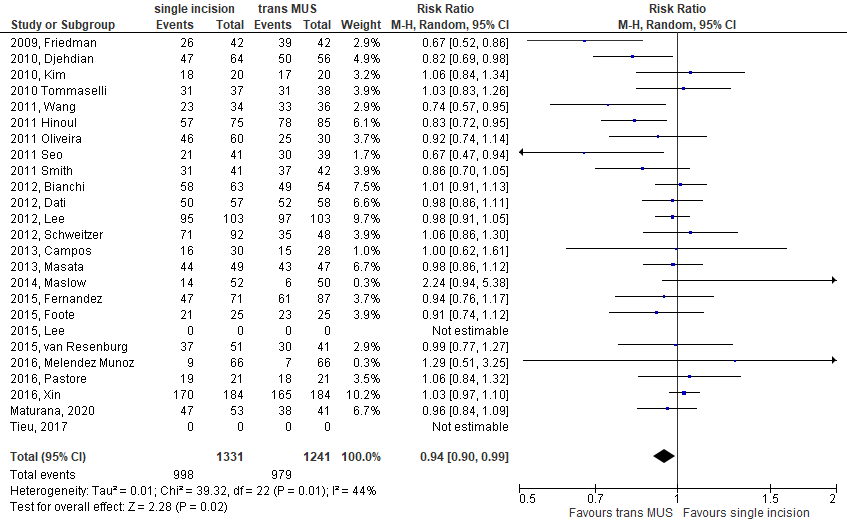
In women with stress urinary incontinence, a single incision sling intervention was slightly less effective for curing symptoms compared to a transobturator MUS intervention, the pooled RR was 0.94 (95%CI 0.90 to 0.99), based on evidence from 23 trials, see figure 7. The risk difference was -0.04 (95%CI -0.08 to -0.00).
Figure 7. Single incision sling vs. transobturator MUS: cure.
5.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from SR and two RCTs.
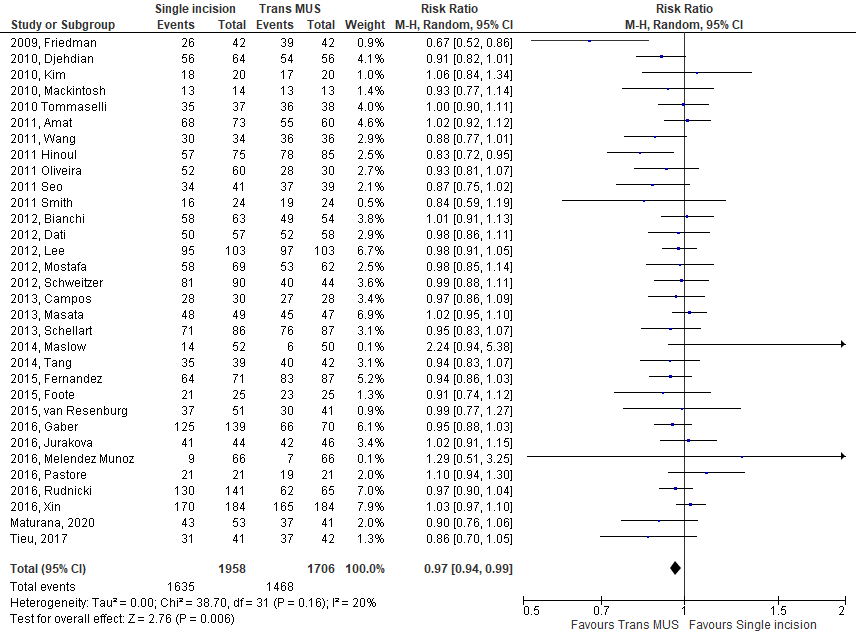
In women with stress urinary incontinence, single incision sling was slightly less effective for improving symptoms compared to transobturator MUS at post-test, the pooled RR was 0.97 (95%CI 0.94 to 0.99), based on evidence from 32 trials, see figure 8. The risk difference was -0.03 (95%CI -0.05 to -0.01).
Figure 8. Single incision sling vs. transobturator MUS: improvement.
5.3 Repeated surgery
Data on repeated surgery were extracted from one SR.
Analyses based on repeated surgery were performed, please see Figure 47 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, repeated surgery within 12 months was more common in single incision sling compared to transobturator MUS at post-test, the OR was 1.57 (95%CI 0.83 to 2.95), based on evidence from 10 trials.
5.4 Adverse events
Data on adverse events were extracted from one SR.
5.4.1 Adverse events – major vascular complications
Analyses based on adverse events (major vascular complications) were performed, please see Figure 49 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, major vascular complications were not different in single incision sling compared to transobturator MUS, the pooled OR was 1.01 (95%CI 0.21 to 4.94), based on evidence from 4 trials.
5.4.2 Adverse events – de novo symptoms
Analyses based on adverse events (de novo symptoms) were performed, please see Figure 51 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, de novo symptoms within 12 months were not different in single incision sling compared to transobturator MUS, the pooled OR was 0.98 (95%CI 0.66 to 1.49), based on evidence from 13 trials.
5.4.3 Adverse events – voiding difficulty
Analyses based on adverse events (voiding difficulty) were performed, please see Figure 53 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, voiding difficulty was less common in single incision sling compared to transobturator MUS, the pooled OR was 0.74 (95%CI 0.45 to 1.21), based on evidence from 13 trials.
5.4.4 Adverse events – bladder or urethral perforation
Analyses based on adverse events (bladder or urethral perforation) were performed, please see Figure 54 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, bladder or urethral perforation was not different in single incision sling compared to transobturator MUS, the pooled OR was 1.00 (95%CI 0.34 to 3.00), based on evidence from 8 trials.
5.4.5 Adverse events – tape/mesh erosion or extrusion
Analyses based on adverse events (tape/mesh erosion or extrusion) were performed, please see Figure 55 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, tape/mesh erosion or extrusion were more common in single incision sling compared to transobturator MUS, the pooled OR was 1.23 (95%CI 0.57 to 2.68), based on evidence from 7 trials.
5.5 Operation time
Data on operation time (i.e., in minutes) were extracted from one SR.
Analyses for the outcome operation time were performed, please see Figure 64 of the ESTER SR (Brazzelli, 2019).
In women with stress urinary incontinence, operation time was longer in single incision sling compared to transobturator MUS, the pooled standardized mean difference was -0.53 (95%CI -0.86 to -0.19), based on evidence from 18 trials.
5.6 Quality of life
Data on quality of life were extracted from two RCTs.
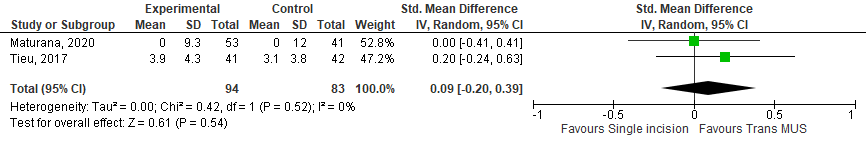
Tieu (2017) and Maturana (2020) measured quality of life with the UDI-6. Means with standard deviations were reported in both studies. Therefore, outcomes could be pooled. The mean difference was 0.09 (95%CI -0.20 to 0.39), see figure 13.
Figure 13. Single incision sling vs. transobturator MUS: quality of life.
Level of evidence of the literature
The level of evidence regarding the outcome measure hospital stay could not be assessed with GRADE. The outcome measures were not studied in the included studies.
The level of evidence regarding the outcome measure stress incontinence (i.e., cure and improvement) was downgraded by 2 levels because of imprecision (1 level, no clinically relevant effect (RR 0.75-1.25)), and inconsistency (1 level).
The level of evidence regarding the outcome measure repeated surgery was downgraded by 3 levels because of imprecision (2 levels, 95%CI of the mean difference includes no significant effect (OR=1), no clinically relevant effect (OR 0.75-1.25), and wide 95%CI) and inconsistency (1 level).
The level of evidence regarding the outcome measure adverse events was downgraded by 3 levels because of imprecision (2 levels, 95%CI of the mean difference includes no significant effect (OR=1), no clinically relevant effect (OR 0.75-1.25), and wide 95%CI) and inconsistency (1 level).
The level of evidence regarding the outcome measure operation time was downgraded by 2 levels because of risk of bias (1 level), and imprecision (95%CI crosses threshold of clinical relevance).
The level of evidence regarding the outcome measures quality of life was downgraded by 3 levels because of imprecision (2 levels, 95%CI of the mean difference includes no significant effect (mean difference=0) and no clinically relevant effect).
Conclusions
|
Low GRADE |
The evidence suggests that a single incision sling intervention results in little to no clinically relevant difference in curing and/or improving symptoms related to stress incontinence when compared with a transobturator MUS in women with stress urinary incontinence.
Sources: Imamura, 2019; Maturana, 2020; Tieu, 2017 |
|
Very low GRADE |
The evidence is very uncertain about the risk on repeated surgery in women with stress urinary incontinence treated with single incision sling, compared to transobturator MUS.
Sources: Imamura, 2019 |
|
Very low GRADE |
The evidence is very uncertain about the risk on adverse events in women with stress urinary incontinence treated with single incision sling, compared to transobturator MUS.
Sources: Imamura, 2019 |
|
Low GRADE |
A single incision sling intervention may reduce the operation time when compared with a transobturator MUS intervention in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
Low GRADE |
The evidence suggests that a single incision sling intervention results in little to no clinically relevant difference in quality of life when compared with a transobturator MUS in women with stress urinary incontinence.
Sources: Maturana, 2020; Tieu, 2017 |
|
No GRADE |
No conclusion could be drawn about the effect of a single incision sling intervention, compared to a transobturaor MUS intervention, in women with stress urinary incontinence on hospital stay. This outcome measure was not studied in the included studies.
Sources: - |
6. Single incision sling vs. fascial sling
6.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from the SR by Imamura (2019).
In women with stress urinary incontinence, a single incision sling intervention was more effective for improving symptoms compared to a fascial sling intervention at post-test, the pooled RR was 1.18 (95%CI 0.90 to 1.56), based on direct evidence from a single trial. The risk difference was -0.33 (95%CI -0.58 to -0.99).
Level of evidence of the literature
The level of evidence regarding the outcome measures complications (i.e., repeated surgery, operation time, hospital stay), adverse events, quality of life could not be assessed with GRADE. The outcome measures were not studied in the included studies.
The level of evidence regarding the outcome measure stress incontinence (i.e., improvement) was downgraded by 3 levels because of risk of bias (1 level) and imprecision (2 levels, 95%CI of the mean difference includes no significant effect (RR=1), no clinically relevant effect (RR 0.75-1.25), and not meeting OIS).
Conclusions
|
Very low GRADE |
The evidence is very uncertain about the effect of a single incision sling intervention, compared to a fascial sling intervention, in improving symptoms related to stress incontinence in women with stress urinary incontinence.
Sources: Imamura, 2019 |
|
No GRADE |
No conclusion could be drawn about the effect of a single incision sling intervention, compared to a fascial sling intervention, in women with stress urinary incontinence on repeated surgery, operation time, hospital stay, adverse events, or quality of life as measured with PROMs. This outcome measure was not studied in the included studies.
Sources: - |
7. Urethral injection therapy vs. fascial sling
No data was available for this comparison since this was not provided by Imamura (2019).
8. Urethral injection therapy vs. retropubic MUS
The study of Itkonen Freitas (2020) reported outcomes for the comparison urethral injection therapy (i.e., Polyacrylamide Hydrogel (Bulkamid)) vs. retropubic MUS.
8.1 Cure of stress urinary incontinence symptoms.
Data on cure of stress urinary incontinence symptoms were extracted from the additional RCT.
The outcome ‘cure’ was defined as negative cough stress test and pad test. In women with stress urinary incontinence 58/107 (54%) patients treated by urethral injection therapy achieved this endpoint compared to 92/101 (91%) patients treated by retropubic MUS at post-test. This resulted in an RR of 0.60 (95%CI 0.49 to 0.72). The risk difference was -0.37 (95%CI -0.48 to -0.26).
8.2 Improvement of stress urinary incontinence symptoms.
Data on improvement of stress urinary incontinence symptoms were extracted from the additional RCT.
The outcome ‘improvement’ was measured using a 5-point Likert-like scale with incontinence considered 1-cured, 2-improved, 3-no change, 4-worsened or 5-cannot answer. A score of 1 or 2 was defined as ‘improvement’. In women with stress urinary incontinence 98/107 (92%) patients treated by urethral injection therapy achieved this endpoint compared to 101/101 (100%) patients treated by retropubic MUS at post-test. This resulted in an RR of 0.92 (95%CI 0.86 to 0.97). The risk difference was -0.08 (95%CI -0.14 to -0.03).
8.3 Adverse events
Data on adverse events were extracted from the additional RCT.
8.3.1 Adverse events – de novo symptoms
The outcome ‘de novo symptoms’ was defined as the need for anticholinergic or mirabegron treatment. In women with stress urinary incontinence 10/107 (9%) patients treated by urethral injection therapy achieved this endpoint compared to 6/101 (6%) patients treated by retropubic MUS. This resulted in an RR of 1.57 (95%CI 0.59 to 4.17). The risk difference was 0.03 (95%CI -0.04 to 0.11).
8.3.2 Adverse events – voiding difficulty
The outcome ‘voiding difficulty’ was defined difficulty emptying the bladder. In women with stress urinary incontinence 0/107 (0%) patients treated by urethral injection therapy achieved this endpoint compared to 9/101 (9%) patients treated by retropubic MUS. This resulted in an RR of 0.05 (95%CI 0.00 to 0.84). The risk difference was -0.09 (95%CI -0.15 to -0.03).
8.3.3 Adverse events – bladder or urethral perforation
Bladder perforation was common in 0/107 (0%) patients treated by urethral injection therapy compared to 7/101 (7%) patients treated by retropubic MUS. This resulted in an RR of 0.06 (95%CI 0.00 to 1.09). The risk difference was -0.07 (95%CI -0.12 to -0.02).
8.4 Quality of life
Data on quality of life were extracted from the additional RCT.
Itkonen Freitas (2021) measured quality of life with the UDI-6 (i.e., total score (max 100)). Median scores were reported per treatment group before and after treatment. Mean pre/post UDI-6 were 34.6/19.0 vs. 31.5/7.9 for urethral injection therapy vs. retropubic MUS. This resulted in mean difference of 11.07 (95%CI 8.32 to 13.82) in favor patients treated by retropubic MUS, and a standardized mean difference of 1.08 (95%CI 0.79 to 1.37).
Level of evidence of the literature
The level of evidence regarding the outcome measures complications (i.e., repeated surgery, operation time, hospital stay), adverse events, quality of life could not be assessed with GRADE. The outcome measures were not studied in the included studies.
The level of evidence regarding the outcome measure stress incontinence (i.e., cure and improvement) was downgraded by 2 levels because of imprecision (1 level, not meeting OIS), and inconsistency.
The level of evidence regarding the outcome measure adverse events was downgraded by 3 levels because of risk of bias (1 level) and imprecision (2 levels, 2 level, 95%CI of the mean difference includes no significant effect (RR=1) and/or no clinically relevant effect (RR 0.75-1.25), and wide 95%CI, not meeting OIS).
The level of evidence regarding the outcome measure quality of life was downgraded by 2 levels because of risk of bias (1 level) and imprecision (1 level, not meeting OIS).
Conclusions
|
Low GRADE |
The evidence suggests that a urethral injection therapy resulted in a lower cure rate and/or improvement of symptoms rate when compared with a retropubic MUS intervention in women with stress urinary incontinence.
Sources: Itkonen Freitas, 2020 |
|
Very low GRADE |
The evidence is very uncertain about the effect of urethral injection therapy, compared to a retropubic MUS intervention, on adverse events (i.e., de novo symptoms, voiding difficulty, bladder or urethral perforation) in women with stress urinary incontinence.
Sources: Itkonen Freitas, 2020 |
|
Low GRADE |
The evidence suggests that a urethral injection therapy results in little to no clinically relevant difference in quality of life when compared with retropubic MUS intervention in patient population in women with stress urinary incontinence.
Sources: Itkonen Freitas, 2021 |
|
No GRADE |
No conclusion could be drawn about the effect of urethral injection therapy intervention, compared to a retropubic MUS intervention, in women with stress urinary incontinence on repeated surgery, operation time, or hospital stay. This outcome measure was not studied in the included studies.
Sources: - |
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
What is the effect of different and mutually comparable surgical interventions in women with stress incontinence?
P: Women with stress incontinence.
I: Synthetic midurethral slings, fascial slings, or urethral bulk injection.
C: See I.
O: Cure or improvement of stress incontinence symptoms, stress incontinence episodes, complications (e.g., repeated surgery, operation time, hospital days), adverse events, quality of life.
Relevant outcome measures
The guideline development group considered cure or improvement of stress incontinence symptoms and quality of life as a critical outcome measures for decision making; and complications, adverse events, and costs as important outcome measures for decision making.
A priori, the working group did not define the outcome measures listed above but used the definitions used in the studies.
If stress incontinence was measured with Urinary Distress Inventory (UDI), the working group defined a difference of 8 points as a minimal clinically (patient) important difference. In all other cases, a difference of 25% in the relative risk for dichotomous outcomes or a 0.5 standard deviation (reported as SMD) for continuous outcomes was taken as a minimal clinically important difference for other outcome measures.
Search and select (Methods)
Search strategy in 2011
The 2011 version of this guideline was an adaptation of the NICE guideline from 2006. Hence, the literature search was based on the search from the NICE Urinary incontinence guideline from 2006 (NICE, 2006) and the updated version of the ICS guideline from 2009 (Abrams, 2009), that was published during the project. In total, 36 RCTs were selected. 31 RCTs adhered to our current PICO and were included in the current literature selection below.
Search strategy in 2021
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms from 01-01-2008 to 09-03-2021. Studies were selected based on the following criteria:
- Women with stress urinary incontinence.
- Surgical intervention like synthetic midurethral slings, fascial slings or urethral bulk injection.
- Comparison with another surgical intervention.
- Investigated at least one of the outcomes as reported in the PICO.
First, a title abstract selection of all systematic reviews (SRs) (n=211) was performed. In total, 12 SR were initially selected based on title and abstract screening. After reading the full text, 10 SR were excluded (see Table of excluded studies), and 2 SR were included. After selecting the most relevant SRs, an updated version of the literature search was performed to select relevant RCTs that were published since the included SRs were published (i.e., searched from 01-01-2017 until 11-06-2021). A title abstract selection of 208 RCTs was performed. Initially, 12 RCTs were selected based on title and abstract screening. After reading the full text, 7 RCTs were excluded (see the table with reasons for exclusion under the tab Methods), and 5 RCTs were included.
The detailed search strategy is depicted under the tab Methods.
Results
Two SRs were included in the analysis of the literature. One of them included 120 studies regarding the effects of stress incontinence, and at least 5 studies for the effects of complications or side effects (Imamura, 2019). The other SR included 2 additional studies, which reported data on the effect of stress incontinence, complications, side effects and quality of life (Elers, 2021). Further, 5 additional RCTs were included studying different comparisons (Itkonen Freitas 2020;2021; Maturana, 2020; Palos, 2018; Tieu, 2017). Important study characteristics and results are summarized in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
Referenties
- Amin, K.A., Janssen, K. & Kobashi, K.C. AUA Guidelines on Stress Urinary Incontinence: What Is New in the Guidelines? Curr Bladder Dysfunct Rep 13, 85Ð92 (2018).
- Brazzelli M, Javanbakht M, Imamura M, Hudson J, Moloney E, Becker F, Wallace S, Omar MI, Shimonovich M, MacLennan G, Ternent L, Vale L, Montgomery I, Mackie P, Saraswat L, Monga A, Craig D. Surgical treatments for women with stress urinary incontinence: the ESTER systematic review and economic evaluation. Health Technol Assess. 2019 Mar;23(14):1-306.
- Casteleijn FM, Zwolsman SE, Kowalik CR, Roovers JPWR. Patients' perspectives on urethral bulk injection therapy and mid-urethral sling surgery for stress urinary incontinence. Int Urogynecol J. 2018 Sep;29(9):1249-1257.
- Elers J, Hornum Bing M, Birkefoss K, Rohde JF, Ussing A, Glavind K. TVT or TVT-O? - A systematic review and meta-analysis comparing efficacy, complications and re-operations. Eur J Obstet Gynecol Reprod Biol. 2021 Mar;258:146-151.
- EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam March 2022. ISBN 978-94-92671-16-5
- Imamura M, Hudson J, Wallace SA, MacLennan G, Shimonovich M, Omar MI, Javanbakht M, Moloney E, Becker F, Ternent L, Montgomery I, Mackie P, Saraswat L, Monga A, Vale L, Craig D, Brazzelli M. Surgical interventions for women with stress urinary incontinence: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2019 Jun 5;365:l1842.
- Itkonen Freitas AM, Mentula M, Rahkola-Soisalo P, Tulokas S, Mikkola TS. Tension-Free Vaginal Tape Surgery versus Polyacrylamide Hydrogel Injection for Primary Stress Urinary Incontinence: A Randomized Clinical Trial. J Urol. 2020 Feb;203(2):372-378.
- Itkonen Freitas AM, Mikkola TS, Rahkola-Soisalo P, Tulokas S, Mentula M. Quality of life and sexual function after TVT surgery versus Bulkamid injection for primary stress urinary incontinence: 1 year results from a randomized clinical trial. Int Urogynecol J. 2021 Mar;32(3):595-601.
- Itkonen Freitas AM, Rahkola-Soisalo P, Mikkola TS, Mentula M. Current treatments for female primary stress urinary incontinence. Climacteric. 2019 Jun;22(3):263-269. doi: 10.1080/13697137.2019.1568404. Epub 2019 Feb 18. PMID: 30773062.
- Kirchin V, Page T, Keegan PE, Atiemo KO, Cody JD, McClinton S, Aluko P. Urethral injection therapy for urinary incontinence in women. Cochrane Database Syst Rev. 2017 Jul 25;7(7):CD003881.
- Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, Vollebregt A, Schellart RP, Graziosi GC, van der Ploeg JM, Brouns JF, Tiersma ES, Groenendijk AG, Scholten P, Mol BW, Blokhuis EE, Adriaanse AH, Schram A, Roovers JP, Lagro-Janssen AL, van der Vaart CH. Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med. 2013 Sep 19;369(12):1124-33.
- Maturana AP, Palos CC, Ghersel FR, Fernandes CE, Oliveira E. Randomized controlled trial comparing mini-sling with transobturator sling for the treatment of stress urinary incontinence. Int Urogynecol J. 2020 Sep;31(9):1925-1931.
- Nambiar A, Cody JD, Jeffery ST. Single-incision sling operations for urinary incontinence in women. Cochrane Database Syst Rev. 2014 Jun 1;(6):CD008709. Updated in: Cochrane Database Syst Rev. 2017 Jul 26;7:CD008709. PMID: 24880654.
- Palos CC, Maturana AP, Ghersel FR, Fernandes CE, Oliveira E. Prospective and randomized clinical trial comparing transobturator versus retropubic sling in terms of efficacy and safety. Int Urogynecol J. 2018 Jan;29(1):29-35. Epub 2017 Oct 2. PMID: 28971224.
- Tieu AL, Hegde A, Castillo PA, Davila GW, Aguilar VC. Transobturator versus single incision slings: 1-year results of a randomized controlled trial. Int Urogynecol J. 2017 Mar;28(3):461-467. Epub 2016 Oct 6. PMID: 27714435.
Evidence tabellen
Research question: What is the effect of surgical interventions in women with stress incontinence?
Evidence table (systematic reviews)
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C)
|
Follow-up |
Outcome measures and effect size |
Comments |
|
Elers, 2021 |
SR and meta-analysis of RCTs
Literature search up to January, 2020 *only 2 studies
A: Feng, 2018 B: Zhang, 2016
Study design: RCT
Setting and Country:
A: China. B: China.
Source of funding and conflicts of interest: A: - B: -
|
In- and exclusion criteria according to PICO:
P: Women with urinary stress incontinence referred for operation, aged 18 or older, who have not previously been operated for stress urinary incontinence I: Retropubic mid-urethral sling operation bottom-up type C: Transobturator mid-urethral sling operation, inside-out type O: Primary outcomes (critical outcomes) Incontinence related quality of life, patient perceived effect, and re-operation evaluated at longest follow-up, minimum six months. Secondary outcomes (important) Number of incontinence episodes, de novo urgency incontinence, leg pain, pelvic pain, de novo dyspareunia and change in sexual function evaluated at longest follow-up, minimum six months and infection and haematoma evaluated in 30 days postoperatively and bladder perforation evaluated perioperatively
Important patient characteristics at baseline:
N, mean age A: 148, 52.5 B: 140, 53
Sex: A: 100% women B: 100% women
Groups comparable at baseline? Yes, RCT |
Describe intervention:
A: transobturator MUS (TVT-O) B: transobturator MUS (TVT-0) |
Describe control:
A: retropubic MUS (TVT) B: retropubic MUS (TVT)
|
End-point of follow-up:
A: 12 months after surgery B: 12 months after surgery
For how many participants were no complete outcome data available? (intervention/control) A: 22 B: 20
|
Outcome measure-1 Defined as none post operative complications and discomfort.
Effect measure: RR [95% CI]: A: 0.94 (95%CI 0.75 to 1.18) B: 0.78 (95%CI 0.60 to 1.03)
Pooled effect (random effects model): 0.87 (95% CI 0.73 to 1.04) favoring TVT-O, less changes on no complications in TVT
Outcome measure-2 PISQ-12 Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire Short Form
Effect measure: RR [95% CI]: A: 0.50 (95%CI -0.81 to 1.81) B: 1.00 (95%CI -5.63 to 1.81)
Pooled effect (random effects model): 0.52 (95% CI -0.77 to 1.81)
|
Facultative:
Conclusion: “With the current evidence of moderate quality based on comparison of efficacy, complications and re-operations between bottom-up TVT versus inside-out TVT-O, which favors TVT, we recommend use of TVT when surgery for SUI is needed. We would not recommend routine use of TVT-O because of the increased risk of leg pain after TVT-O. Furthermore, some evidence indicates better long-term results after TVT with less need of re-operation due to recurrent SUI.”(Elers, 2021)
Level of evidence: only Risk of Bias via GRADE method, RoB was low for Zhang, 2016, and moderate for Feng, 2018.
Sensitivity analyses (excluding small studies; n/a only two studies
Heterogeneity: n/a, only two studies. |
|
Imamura, 2019
|
SR and meta-analysis of RCTS
Literature search up to June, 2017
Please see, Brazzelli 2019.
Study design: RCTs
Setting and Country: Please see, Brazzelli 2019.
Source of funding and conflicts of interest: The National Institute for Health Research Health Technology Assessment programme.
|
Inclusion criteria SR: in short; randomised controlled trials or quasi-randomised controlled trials (e.g., alternate allocation), women with stress urinary incontinence or mixed urinary incontinence with predominant symptoms of stress urinary incontinence (diagnosis as defined by trial investigators), and comparison of two or more surgical interventions. For detailed information, please see, Brazzelli 2019.
Exclusion criteria SR: For detailed information, please see, Brazzelli 2019.
175 studies included
Important patient characteristics at baseline: For detailed information, please see, Brazzelli 2019
N, mean age Sample sizes were generally small (median 91 participants per trial, range 15-655). For detailed information, please see, Brazzelli 2019
Sex: Only females.
Groups comparable at baseline? Yes, RCT |
Describe intervention:
For detailed information, please see, Brazzelli 2019.
*21 comparisons Retropubic MUS vs. Transobturator MUS Retropubic MUS vs. Open colposuspension Retropubic MUS vs. Laparoscopic colposuspension Retropubic MUS vs. Fascial sling Retropubic MUS vs. Single incision sling Retropubic MUS vs. Anterior repair Transobturator MUS vs. Open colposuspension Transobturator MUS vs. Laparoscopic colposuspension Transobturator MUS vs. Fascial sling Transobturator MUS vs. Single incision sling Transobturator MUS vs. Anterior repair Transobturator MUS vs. Pelvic floor muscle training Open colposuspension vs. Laparoscopic colposuspension Open colposuspension vs. Fascial sling Open colposuspension vs. Bladder neck needle suspension Open colposuspension vs. Anterior repair Open colposuspension vs. Pelvic floor muscle training Fascial sling vs. Single incision sling Fascial sling vs. Urethral injection therapy Fascial sling vs. Bladder neck needle suspension Bladder neck needle suspension vs. Anterior repair
|
Describe control:
For detailed information, please see, Brazzelli 2019.
|
End-point of follow-up:
Most studies (134/175, 76%) also had a short duration of follow up (median 12 months, range 1-126 months), with only 41 studies (23%) having a mean follow-up of three years or longer. For detailed information, please see, Brazzelli 2019
For how many participants were no complete outcome data available? (intervention/control) For detailed information, please see, Brazzelli 2019.
|
Outcome measure-1 the number of women with cure, defined as resolution of incontinence symptoms, Effect measure: OR [95% CI]: For detailed information, please see, Brazzelli 2019.
Pooled effect (random effects) **comparisons including more than 3 studies. * transobturator MUS vs. retropubic MUS 0.83 (0.71 to 0.97) * open colposuspension vs. retropubic MUS * fascial sling vs. retropubic MUS * single incision vs. transobturator MUS 0.74 (0.43 to 1.30)
Outcome measure-2 The number of women with improvement, defined as any improvement in incontinence symptoms from baseline, including cure **comparisons including more than 3 studies. * transobturator MUS vs. retropubic MUS 0.86 (0.70 to 1.06) * open colposuspension vs. retropubic MUS * fascial sling vs. retropubic MUS * single incision vs. transobturator MUS 0.93 (0.58 to 1.48)
Effect measure: OR [95% CI]: For detailed information, please see, Brazzelli 2019.
Secondary outcomes were the number of women having repeated surgery for incontinence symptoms, adverse events, length of hospital stay, and operation time during the study period as reported by the trial investigators. * For detailed information, please see, Brazzelli 2019.
|
Facultative:
Brief description of author’s conclusion ‘Retropubic MUS, transobturator MUS, traditional sling, and open colposuspension are more effective than other procedures for stress urinary incontinence in the short to medium term. Data on long term effectiveness and adverse events are, however, limited, especially around the comparative adverse events profiles of MUS and non-MUS procedures. A better understanding of complications after surgery for stress urinary incontinence is imperative.’
Personal remarks on study quality, conclusions, and other issues (potentially) relevant to the research question *only data of the direct comparison will be used in the current summary of literature.
Level of evidence: GRADE (per comparison and outcome measure) including reasons for down/upgrading: As we decided to use only data of the direct comparisons, the level of evidence was not adapted.
Sensitivity analyses (excluding small studies; excluding studies with short follow-up; excluding low quality studies; relevant subgroup-analyses); mention only analyses which are of potential importance to the research question
Heterogeneity: clinical and statistical heterogeneity; explained versus unexplained (subgroup analysis); n.a. subgroup analysis per comparisons are only performed. |
Table of quality assessment (systematic reviews)
Based on AMSTAR checklist (Shea, 2007) and PRISMA checklist (Moher, 2009)
|
Study
First author, year |
Appropriate and clearly focused question?
Yes/no/unclear |
Comprehensive and systematic literature search?
Yes/no/unclear |
Description of included and excluded studies?
Yes/no/unclear |
Description of relevant characteristics of included studies?
Yes/no/unclear |
Appropriate adjustment for potential confounders in observational studies?
Yes/no/unclear/not applicable |
Assessment of scientific quality of included studies?
Yes/no/unclear |
Enough similarities between studies to make combining them reasonable? Yes/no/unclear |
Potential risk of publication bias taken into account?
Yes/no/unclear |
Potential conflicts of interest reported?
Yes/no/unclear |
|
Elers, 2021 |
Yes |
Yes |
Unclear |
No |
Not applicable |
Yes |
Yes |
Yes |
No |
|
Imamura, 2019 |
Yes |
Yes |
Yes |
Yes |
Not applicable |
Yes |
Yes |
Yes |
Yes |
Evidence table (RCTs)
|
Study reference |
Study characteristics |
Patient characteristics 2 |
Intervention (I) |
Comparison / control (C) 3
|
Follow-up |
Outcome measures and effect size 4 |
Comments |
|
Maturana, 2020 |
Type of study: RCT
Setting and country: Hospitals in Sao Paulo, Brazil.
Funding and conflicts of interest: None. |
Inclusion criteria: age > 18 years, absence of associated neurological diseases, clinical diagnosis of stress predominantly UI and urodynamic study demonstrating SUI and absence of detrusor overactivity.
Exclusion criteria: were absence of urodynamic changes that suggested SUI, findings suggestive of infravesical obstruction and detrusor overactivity, coagulopathies, pregnancy, history of foreign body sensitivity (i.e., polypropylene), acute cystitis, vulvovaginitis, previous surgery for the treatment of SUI and history of treatment with pelvic radiotherapy.
N total at baseline: Intervention: SIMS; n=58 Control: TOT sling; n=47
Important prognostic factors2: N.A.
Groups comparable at baseline? Yes
|
Describe intervention (treatment/procedure/test):
SIMS = single-incision minislings
The experimental group, underwent a surgical procedure performed with SIMS (i.e., Ophira Minisling System™; Promedon, Cordoba, Argentina).
|
Describe control (treatment/procedure/test):
TOT = tension-free transobturator tape
The control group was the sling TOT (i.e., Unitape T Plus™ or Safyre T Plus™; Promedon, Cordoba, Argentina) group.
|
Length of follow-up: 12 months
Loss-to-follow-up: Intervention: N=5 (9%) Reasons; Patient-led withdrawal (n=4 ), Cardiac Death (n=1 )
Control: N=6 (13%) Reasons; Patient-led withdrawal (n=6 )
Incomplete outcome data: n.a.
|
Outcome measures and effect size (include 95%CI and p-value if available):
Objective cure: SIMS: n=47 (88.7%)
Subjective cure: SIMS: n=43 (81.1%)
Quality of life: UDI-6 à no significant differences between de groups.
|
* small sample size |
|
Itkonen Freitas, 2020 |
Type of study: controlled noninferiority clinical trial
Setting and country: Hospitals in Helsinki, Finland
Funding and conflicts of interest:
Supported by a Helsinki University Hospital research grant, Finnish Society of Gynecological Surgery and Helsinki University Hospital grants (AMIF), Finnish Cultural Foundation grants (MM), Finnish Medical Foundation grants (PR-S) and Finnish Society of Gynecological Surgery and Helsinki University grants (ST). The funders of the study had no influence in the study design, data collection, data analysis, |
Inclusion criteria:
SUI not responsive to conservative treatment, patient age greater than 18 years, no previous incontinence procedure, a positive cough stress test without urge-type leakage, PVR volume less than 100 ml and bladder capacity greater than 300 ml.
Exclusion criteria: body mass index greater than 35 kg/m2, neurogenic disease, use of anticholinergics or mirabegron, illness or another condition causing a risk of complications during the TVT operation, active malignancy, urinary tract infection, more than second degree urogenital prolapse, pregnancy or future plans for pregnancy, or inability to understand the purpose of the study
N total at baseline: Intervention: PAHG; n=108 Control: TVT; n=104
Important prognostic factors2: N.A.
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
PAHG (Bulkami) was injected with the patient under local anaesthesia with periurethral lidocaine (10 ml) injections.
|
Describe control (treatment/procedure/test):
As a mid-urethral sling we used the Gynecare TVT Exac system as originally described. Retropubic
|
Length of follow-up: 12 months
Loss-to-follow-up: Intervention: N 1 (1%) Reasons; only interviewed by telephone.
Control: N 3 (3%) Reasons; only interviewed by telephone (2), and unable to contact (1)
Incomplete outcome data: See loss to follow up
|
Outcome measures and effect size (include 95%CI and p-value if available):
Objective: Cough stress + pad tests neg Intervention: 58 (54.2) Control: 92 (92.1) P<0.01
Improve or cured: Intervention: 98 (91.6) Control: 101 (100) P<0.01
Difficulty emptying bladder: Intervention: 0 Control: 9 (9) <0.01
De novo urgency Intervention: 10 (9) Control: 6 (6) 0.36 |
The procedures were done by urogynaecologists with a strong background in SUI treatment, particularly TVT |
|
Palos, 2018 |
Type of study: controlled and randomized prospective clinical trial with a noninferiority analysis
Setting and country: Hospital in Sao Paulo, Brazil
Funding and conflicts of interest: None. |
Inclusion criteria: Women diagnosed with SUI using a urodynamic test.
Exclusion criteria: complaints of mixed urinary incontinence (MUI), previous surgery for UI, any type of voiding dysfunction on the urodynamic test, presence of urinary tract infection (UTI), and contraindications for the surgical procedure or anesthesia.
N total at baseline: Intervention: 47 Control: 45
Important prognostic factors2: N.A.
Groups comparable at baseline? Yes |
Describe intervention (treatment/procedure/test):
Transobturator MUS
|
Describe control (treatment/procedure/test):
Retropubic MUS
|
Length of follow-up: 12 months
Loss-to-follow-up: Intervention: N 6(13%) Reasons; lost to follow up (5), died (1)
Control: N 5(11%) Reasons; lost to follow up
Incomplete outcome data: See loss to follow up. |
Outcome measures and effect size (include 95%CI and p-value if available):
Objective cure: Trans: n=38/41 (93%) Retro: n=40/40 (100%)
Subjective cure: Trans: n=37/41 (90%)
Pain: Trans: 1.5 0.48
Bladder perforation: Trans: 1 (2.4%) 1.00
De novo urgency: Trans: 1 (2.4%) 1.00
Quality of life: UDI-6 à no significant differences between de groups.
|
Relative small sample size |
|
Tieu, 2017 |
Type of study: RCT
Setting and country: Female Pelvic Medicine and Reconstructive Surgery Section at Cleveland Clinic Florida in Weston, Florida.
Funding and conflicts of interest: None. |
Inclusion criteria: symptomatic patients with SUI confirmed objectively by urodynamics.
Exclusion criteria: a history of incontinence surgery, a diagnosis of intrinsic sphincter deficiency or low pressure urethra made by urodynamic testing (Valsalva leak point pressure <60 cmH2O and/or maximal urethral closure pressure <40 cmH2O) and mixed incontinence with a predominance of detrusor overactivity.
N total at baseline: Intervention: 49 Control: 49
Important prognostic factors2: N.A.
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
Single incision sling
|
Describe control (treatment/procedure/test):
Transobturator MUS. |
Length of follow-up: 12 months
Loss-to-follow-up: Intervention: N 8(16%) Reason; lost to follow up.
Control: N 7(14%) Reason; lost to follow up.
Incomplete outcome data: See loss to follow up. |
Outcome measures and effect size (include 95%CI and p-value if available):
Subjective cured: Single: 31 (76%) 0.20
De novo urgency: Single: 2 (0.5%) 1.0
Voiding dairy: Single: 0 (0-9) 0.80
|
Not designed to address pain.
Single centre, not blinded. |
|
Itkonen Freitas, 2021 |
Type of study: controlled noninferiority clinical trial
Setting and country: Hospitals in Helsinki, Finland
Funding and conflicts of interest:
Supported by a Helsinki University Hospital research grant, Finnish Society of Gynecological Surgery and Helsinki University Hospital grants (AMIF), Finnish Cultural Foundation grants (MM), Finnish Medical Foundation grants (PR-S) and Finnish Society of Gynecological Surgery and Helsinki University grants (ST). The funders of the study had no influence in the study design, data collection, data analysis, |
Inclusion criteria:
SUI not responsive to conservative treatment, patient age greater than 18 years, no previous incontinence procedure, a positive cough stress test without urge-type leakage, PVR volume less than 100 ml and bladder capacity greater than 300 ml.
Exclusion criteria: body mass index greater than 35 kg/m2, neurogenic disease, use of anticholinergics or mirabegron, illness or another condition causing a risk of complications during the TVT operation, active malignancy, urinary tract infection, more than second degree urogenital prolapse, pregnancy or future plans for pregnancy, or inability to understand the purpose of the study
N total at baseline: Intervention: PAHG; n=108 Control: TVT; n=104
Important prognostic factors2: N.A.
Groups comparable at baseline? Yes. |
Describe intervention (treatment/procedure/test):
PAHG (Bulkami) was injected with the patient under local anesthesia with periurethral lidocaine (10 ml) injections.
|
Describe control (treatment/procedure/test):
As a mid urethral sling we used the Gynecare TVT Exac system as originally described. Retropubic
|
Length of follow-up: 12 months
Loss-to-follow-up: Intervention: N 1 (1%) Reasons; only interviewed by telephone.
Control: N 3 (3%) Reasons; only interviewed by telephone (2), and unable to contact (1)
Incomplete outcome data: See loss to follow up
|
Outcome measures and effect size (include 95%CI and p-value if available):
UDI-6; post scores Intervention: 18.96 ± 13.20 (95% CI 16.43–21.50) Control: 7.89 ± 7.65 (95% CI 6.38–9.40)
Difference: < 0.001 (95% CI -3.37–1.95)
|
Post hoc analyses; |
Risk of bias table (RCTs)
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measure
Low Some concerns High
|
|
Maturana, 2020 |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Probably no
Reason: Group assignment was concealed in consecutively numbered, sealed, opaque envelopes that were opened in the operating room just before the procedure. No information about blinding of patients and if data analyses were performed blinded. |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group. Also per protocol analyses were performed. |
Definitely yes;
Reason: All relevant outcomes were reported |
Definitely yes;
Reason: No other problems noted |
Low |
|
Itkonen Freitas, 2020 |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Probably no
Reason: Not mentioned. |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group. |
Definitely yes;
Reason: All relevant outcomes were reported |
Definitely yes;
Reason: No other problems noted |
Low |
|
Palos, 2018 |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Probably no
Reason: Group assignment was concealed in consecutively numbered, sealed, opaque envelopes that were opened in the operating room just before the procedure. No information about blinding of patients and if data analyses were performed blinded. |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group. Also per protocol analyses were performed. |
Definitely yes;
Reason: All relevant outcomes were reported |
Definitely yes;
Reason: No other problems noted |
Low |
|
Tieu, 2017 |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Probably no
Reason: Not mentioned. |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group. |
Definitely yes;
Reason: All relevant outcomes were reported |
Definitely yes;
Reason: No other problems noted |
Low |
|
Itkonen Freitas, 2021 |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Definitely yes;
Reason: Central randomization with computer generated random numbers |
Probably no
Reason: Not mentioned. |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group. |
Definitely yes;
Reason: All relevant outcomes were reported |
Definitely yes;
Reason: No other problems noted |
Low |
Table of excluded studies
|
Author and year |
Reason for exclusion |
|
Amin, 2018 |
AUA guideline, for considerations |
|
Dogan, 2018 |
Follow up |
|
Emami, 2019 |
Not according to PICO |
|
Fusco, 2017 |
More recent SR included |
|
Huang, 2018 |
Not according GRADE, Elers 2021 more recent |
|
Kirchin, 2017 |
Taken into account in Imamura |
|
Maggiore, 2015 |
Other, more recent, SR included |
|
Maggiore, 2017 |
Other, more recent, SR included |
|
Melendez, 2019 |
Wrong comparison, single vs. modified-trans |
|
Mostafa, 2015 |
Not according GRADE, more recent SR included |
|
Rudnicki, 2017 |
Trans and retropubic as control |
|
Saraswat, 2020 |
Outcomes of 4 additional studies not in line with PICO |
|
Schellart, 2018 |
Follow-up |
|
Song, 2020 |
Outcome not in line with PICO |
|
Szymański, 2020 |
No RCT |
|
Zhang, 2015 |
Other, more recent, SR included |
|
Zullo, 2020 |
Wrong comparison, trans vs. modified-trans |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 13-11-2023
Beoordeeld op geldigheid : 07-11-2023
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodules.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodules zijn in 2020 per module schrijvers en meelezers benoemd. Deze personen werden aangewezen als vertegenwoordigers door de relevante beroepsgroepen die betrokken zijn bij de in de module beschreven zorg (zie hiervoor de Samenstelling van de werkgroep). Alle schrijvers van modules vallend onder één richtlijn vormden samen een schrijfgroep. Alle meelezers van modules vallend onder één richtlijn vormden samen een clusterwerkgroep. In totaal resulteerde dit dus in zes werkgroep en zes clusterwerkgroepen.
Voorzitter project (technisch voorzitter)
Timmermans A. (Anne), gynaecoloog, AmsterdamUMC, NVOG
Werkgroep Urine-incontinentie bij vrouwen
Engberts M.K. (Marian), urogynaecoloog, Isala Ziekenhuis te Zwolle, NVOG
Klerkx W.M. (Wenche), urogynaecoloog, St. Antonius Ziekenhuis te Utrecht, NVOG
Koldewijn E.L. (Evert), uroloog, Catharina Ziekenhuis te Eindhoven, NVU
Labrie J. (Julien), gynaecoloog, Spaarne Gasthuis te Haarlem, NVOG
Martens F. (Frank), uroloog, Radboudumc te Nijmegen, NVU
Steures P. (Pieternel), urogynaecoloog, Jeroen Bosch Ziekenhuis te Den Bosch, NVOG
Clusterwerkgroep Urine-incontinentie bij vrouwen
Adamse C. (Corine), geregistreerd bekkenfysiotherapeut en klinisch epidemioloog, Antonius Ziekenhuis Sneek, docent Master opleiding Bekkenfysiotherapie, SOMT Amersfoort, NVFB/KNGF
Bosch M. (Marlies), patiëntvertegenwoordiger, Bekkenbodem4all
Dos Santos A. (Ana), bekkenfysiotherapeut MSc, PelviCentrum te Leiden, NVFB/KNGF
Lagro-Janssen A.L.M. (Toine), prof, huisarts n.p., RadboudUMC Nijmegen, NHG
Teunissen T.A.M. (Doreth), huisarts, RadboudUMC te Nijmegen, NHG
Ondersteuning project
Abdollahi M. (Mohammadreza), adviseur Kennisinstituut van de Federatie van Medisch Specialisten
Labeur Y.J. (Yvonne), adviseur, Kennisinstituut van de Federatie Medisch Specialisten
Sussenbach A.E. (Annelotte), junior adviseur Kennisinstituut van de Federatie van Medisch Specialisten
Verhoeven M. (Maxime), adviseur, Kennisinstituut van de Federatie van Medisch Specialisten
Projectleiding
Augustus 2022- nu Mostovaya I.M. (Irina) (projectleider), senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten
April 2020 tot augustus 2021: Bijlsma-Rutte A. (Anne), adviseur, Kennisinstituut van de Federatie van Medisch Specialisten
September 2021 tot januari 2022: Venhorst K. (Kristie), adviseur, Kennisinstituut van de Federatie van Medisch Specialisten
Februari 2022 tot juni 2022: Göthlin M. (Mattias), adviseur, Kennisinstituut van de Federatie van Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoek financiering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Timmermans (technisch voorzitter van het project) |
Gynaecoloog, Amsterdam UMC (0.5 fte) |
Commissie kwaliteitsdocumenten NVOG (onbetaald); projectgroep Gynae Goes Green NVOG (onbetaald) |
Geen |
Geen actie |
|
Urine-incontinentie bij vrouwen - werkgroep |
||||
|
Engberts |
Urogynaecoloog ISALA |
Trainer Altis ® Sling voor Coloplast, betaald |
Geen |
Niet betrokken bij de besluitvorming rondom (fasci)slings. |
|
Klerkx |
Urogynaecoloog, St. Antonius Ziekenhuis |
Geen |
Geen |
Geen actie |
|
Koldewijn |
Uroloog 100% Catharina ziekenhuis Eindhoven |
Voorzitter Stichting Opleidingen Medici (SOM). Stichting acquireert gelden voor promotieonderzoek: onbetaald |
Geen |
Geen actie |
|
Labrie |
Gynaecoloog Spaarne Gasthuis |
Medisch Manager vakgroep gynaecologie gevaceerd |
Geen |
Geen actie |
|
Martens |
Uroloog, radboudumc |
Geen |
OASIS trial, implantaat PTNS, BlueWind, multicenter, PI Nijmegen. |
Geen trekker van module over PTNS/TENS. |
|
Steures |
Urogynaecoloog Jeroen Bosch Ziekenhuis, Den Bosch |
Geen |
Geen |
Geen actie |
|
Urine-incontinentie bij vrouwen - clusterwerkgroep |
||||
|
Adamse |
Geregistreerd bekkenfysiotherapeut en klinisch epidemioloog, Antonius Ziekenhuis Sneek. |
Commissielid Wetenschapscommissie NVFB Commissielid Richtlijn chronische bekkenpijn FMS Docent Master opleiding Bekkenfysiotherapie, SOMT Amersfoort |
Geen |
Geen actie |
|
Bosch |
Zie boven |
Zie boven |
Zie boven |
Zie boven |
|
Dos Santos |
Geregistreerd bekkenfysiotherapeut MSc bij PelviCentrum - Centrum voor Bekkenfysiotherapie Leiden |
Lid van NVFB Wetenschappelijke Commissie. Vergoeding van de reiskosten en bijwonen van vergaderingen. |
Deelname aan het ontwikkelen van de richtlijn kan ervoor zorgen dat collega vaker gaan verwijzen naar mijn praktijk vanwege meer bekendheid. Mogelijk belangen bij bescherming positie bekkenfysiotherapie. |
Geen actie |
|
Lagro-Janssen |
Geen werkgever |
Adviseur centrum Seksueel Geweld Gelderland-Zuid en Midden (onbetaald) |
Geen |
Geen actie |
|
Teunissen |
Huisarts, zelfstandig 0,6 fte Docent, senior onderzoeker Radboudumc afdeling eerstelijnsgeneeskunde 0,4 fte |
Huisarts -> huisartswerkzaamheden (betaald) Radboudumc -> docent senior onderzoeker (betaald) |
Geen |
Geen actie |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door het uitnodigen van Patiëntenfederatie Nederland en Stichting Bekkenbodem4All voor de schriftelijke knelpunteninventarisatie en voor deelname aan de clusterwerkgroepen. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De richtlijn is voor commentaar voorgelegd aan Patiëntenfederatie Nederland en Stichting Bekkenbodem4All en de eventueel aangeleverde commentaren worden bekeken en verwerkt.
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld volgens de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerden de werkgroep de knelpunten in de zorg en de actualiteit van de aanbevelingen beschreven in de te reviseren modules. Tevens zijn er knelpunten aangedragen door de Nederlandse Vereniging voor Obstetrie en Gynaecologie (NVOG), de Nederlandse Vereniging van Maag-Darm-Leverartsen (NVMDL), Vereniging Klinische Genetica Nederland (VKGN), Inspectie Gezondheidszorg en Jeugd (IGJ), Koninklijke Nederlandse Organisatie van Verloskundigen (KNOV), Nederlands Huisartsen Genootschap (NHG), Nederlandse Vereniging voor Bekkenfysiotherapie (NVFB) / Koninklijk Nederlands Genootschap voor Fysiotherapie (KNGF), Nederlandse Vereniging van Ziekenhuizen (NVZ), Patiëntenfederatie Nederland (PFN), Zorginstituut Nederland (ZiNL), Zelfstandige Klinieken Nederland (ZKN) en Zorgverzekeraars Nederland (ZN) via een schriftelijke knelpunteninventarisatie.
Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Ook definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur en de beoordeling van de risk-of-bias van de individuele studies is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Hultcrantz, 2017; Schünemann, 2013).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nul effect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE-methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Volgens de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren worden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren wordt de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule wordt aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en akkoord.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwaliteit.
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013.
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, Williams JW Jr, Kunz R, Craig J, Montori VM, Bossuyt P, Guyatt GH; GRADE Working Group. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008 May 17;336(7653):1106-10. Erratum in: BMJ. 2008 May 24;336(7654).
Wessels M, Hielkema L, van der Weijden T. How to identify existing literature on patients' knowledge, views, and values: the development of a validated search filter. J Med Libr Assoc. 2016 Oct;104(4):320-324.
Zoekverantwoording
Literatuur zoekstrategie
Algemene informatie
|
Richtlijn: Richtlijn urine-incontinentie bij vrouwen >> herziening 4 modules in het ’24 modules project’ |
|
|
Uitgangsvraag: Welke (minimaal) chirurgische interventie (synthetische suburethrale tapes, fascie slings en het injecteren van bulkmaterialen) heeft de voorkeur bij vrouwen met stressincontinentie? |
|
|
Database(s): Medline (OVID), Embase |
Datum: 09-03-2021 (SR’s) en 11-06-2021 (RCT’s) |
|
Periode: >2008 voor SR’s en > 2017 voor RCT’s |
Talen: Engels, Nederlands |
|
Literatuurspecialist: Laura Boerboom |
|
|
BMI zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting en opmerkingen:
→ Voor deze vraag is gezocht op de elementen stressincontinentie (in het blauw) en Chirurgische interventie (synthetische suburethrale tapes, fascie slings en het injecteren van bulkmaterialen (in het groen).
→ De werkgroep had drie sleutelpublicaties (RCT’s). Het artikel van Sung (2019) zat in de resultaten, maar de artikelen van Labrie (2013) en Nilsson (2013) vielen buiten onderstaande search vanwege het publicatiejaar.
|
|
|
Te gebruiken voor richtlijnen tekst: In de databases Embase (via embase.com) en Medline (via OVID) is op 09-03-2021 met relevante zoektermen gezocht naar systematische reviews en op 11-6-2021 naar RCT’s over welke chirurgische interventie de voorkeur heeft bij vrouwen met stressincontinentie. De literatuurzoekactie leverde 419 unieke treffers op. |
|
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SRs |
181 |
158 |
211 |
|
RCTs |
168 |
112 |
208 |
|
Totaal |
349 |
270 |
419 |
Zoekstrategie
|
Database |
Zoektermen |
|||||||||||||||||||||
|
Embase
|
|
|||||||||||||||||||||
|
Medline (OVID)
|
1 exp *Urinary Incontinence, Stress/ or ((stress or mixed) adj3 incontinence).ti. (10407) 2 exp Suburethral Slings/ or ((suburethral or midurethral or surgery) adj3 (tape* or sling*)).ti,ab,kf. or (bulk* adj3 (injection* or material or agent*)).ti,ab,kf. or 'tension free vaginal tape*'.ti,ab,kf. or 'single incision mini sling*'.ti,ab,kf. or 'fascial sling*'.ti,ab,kf. or 'fascia sling*'.ti,ab,kf. or exp Hyaluronic Acid/ or 'hyaluronic acid'.ti,ab,kf. or 'glutaraldehyde collagen'.ti,ab,kf. or silicone.ti,ab,kf. or 'carbon coated zirconium'.ti,ab,kf. (69030) 3 1 and 2 (3334) 4 limit 3 to ((english or dutch) and yr="2008 -Current") (2133) 5 (meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf.) not (comment/ or editorial/ or letter/ or ((exp animals/ or exp models, animal/) not humans/)) (483208) 6 4 and 5 (158) – SR’s |
|
Database |
Zoektermen |
||||||||||||||||||||||||
|
Embase
|
|
||||||||||||||||||||||||
|
Medline (OVID)
|
1 exp *Urinary Incontinence, Stress/ or ((stress or mixed) adj3 incontinence).ti. (10534) 2 exp Suburethral Slings/ or ((suburethral or midurethral or surgery) adj3 (tape* or sling*)).ti,ab,kf. or (bulk* adj3 (injection* or material or agent*)).ti,ab,kf. or 'tension free vaginal tape*'.ti,ab,kf. or 'single incision mini sling*'.ti,ab,kf. or 'fascial sling*'.ti,ab,kf. or 'fascia sling*'.ti,ab,kf. or exp Hyaluronic Acid/ or 'hyaluronic acid'.ti,ab,kf. or 'glutaraldehyde collagen'.ti,ab,kf. or silicone.ti,ab,kf. or 'carbon coated zirconium'.ti,ab,kf. (70210) 3 1 and 2 (3381) 4 limit 3 to ((english or dutch) and yr="2017 -Current") (680) 5 (exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw.) not (animals/ not humans/) (2128269) 6 4 and 5 (NOT SR’s) (112) – RCT’s |