Calcaneus fracturen
Uitgangsvraag
Welke behandeling reduceert de meest voorkomende negatieve gevolgen (korte en lange termijn) van calcaneus fracturen?
Aanbeveling
Overweeg een operatieve behandeling van een calcaneusfractuur enkel indien de patiënt- en fractuurkarakteristieken (hoogte verlies >5 mm, verbreding >5 mm, step off posterieure subtalaire gewricht >2 mm, varus >5 graden, valgus > 10 graden, Böhler < 15 graden, fibulair impingement) hier aanleiding toe geven.
Behandel een patiënt met een calcaneusfractuur zo minimaal invasief mogelijk. Denk hierbij aan een operatie met percutane schroefosteosynthese of middels minimaal invasieve plaatosteosynthese (sinus tarsi benadering)
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Er is literatuuronderzoek gedaan naar de optimale behandelstrategie van calcaneus fracturen. Hierbij is gezocht naar studies waarbij een vergelijking werd gemaakt tussen operatieve en conservatieve behandeling. Er werd één systematische review gevonden (Selim, 2022), waarin negen relevante RCTs waren geïncludeerd, en 1 additionele RCT (Hussain, 2022). Op basis van dit bewijs lijkt er geen verschil te zijn tussen operatieve en conservatieve behandeling op de patiënt-gerapporteerde functionele uitkomst (AOFAS; cruciale uitkomstmaat). Het gevonden bewijs suggereert echter ook dat operatieve behandeling mogelijk een groter risico geeft op complicaties (belangrijke uitkomstmaat). Dit verhoogde risico op complicaties is logisch te verklaren gezien de aard van de interventie, waarbij een behandeling met gips van nature een lager risico op complicaties geeft dan een chirurgische behandeling. De resultaten suggereren dat er mogelijk geen verschil is in het risico op artritis/artrose, de resultaten zijn echter niet eenduidig. Ook over de effecten op de hoek van Bohler kunnen geen uitspraken worden gedaan. De bewijskracht voor de gevonden effecten is laag mede vanwege heterogeniteit in de resultaten. Daarnaast doorkruizen de 95% betrouwbaarheidsintervallen (BI) de grenzen voor klinische besluitvorming, waardoor er onzekerheid blijft of het gevonden effect ten faveure van operatief of ten faveure van conservatieve behandeling is. Ondanks de lage bewijskracht, lijkt er een voorzichtig voordeel te zijn voor conservatieve behandeling gezien het mogelijk lagere risico op complicaties en het gelijke effect op functionele uitkomst.
De studie van Selim (2022) includeerde naast gerandomiseerde trials ook prospectieve cohort studies en kwam daarmee tot de conclusie dat er geen verschil in morbiditeit (complicaties) te vinden was tussen de operatief en conservatief behandelde fracturen. Naast de effecten op de vooraf gedefinieerde uitkomstmaten, werd (op basis van zowel het gerandomiseerde onderzoek, als de prospectieve cohort studies) gerapporteerd dat operatief behandelde patiënten minder problemen hadden met de schoeibaarheid van de voet en dat patiënten vaker terugkwamen op hun oude activiteitenniveau (Odds Ratio: 2.87, 95% BI: 1.03 tot 8.00).
De werkgroep is dan ook van mening dat er in specifieke situaties een meerwaarde te verwachten valt van een operatieve interventie. Met name gezonde patiënten waarbij de fractuur significante laterale comminutie/verbreding laat zien, of een verlaagde hoek van Bohler of fibulair impingment kunnen potentieel profijt hebben van een operatieve behandeling. Dit om de kans op schoeibaarheid en terugkomen op het oude activiteitenniveau gunstig te beïnvloeden (Selim, 2022). Hierbij is de werkgroep van mening dat een operatie overwogen dient te worden bij de volgende fractuur kenmerken (Linsenmaier 2003; Selim, 2022; Dickenson 2021)
- Hoogte verlies >5mm
- Laterale communitie of verbreding >5 mm
- Step off posterieure subtalaire gewricht >2 mm
- Varus >5 graden
- Valgus > 10 graden
- Bohler < 15 graden
- Fibulair impingement
Vanwege het risico op complicaties, is bij patiënten met een verhoogd risico en/of slechte functionele uitkomst conservatieve behandeling te prefereren. Hierbij moet gedacht worden aan patiënten met diabetes mellitus, perifeer vaatlijden, overgewicht, roken, alcoholmisbruik, verlate presentatie al dan niet met slechte toestand van de weke delen of ernstige bijkomende letsels (Selim, 2022). Bij deze patiëntengroep is de kans op complicaties als gevolg van de operatie of post-traumatische artritis/artrose dermate groot, dat er geen meerwaarde van een operatieve interventie te verwachten valt.
Een tweede vergelijking die werd onderzocht in de literatuur was de vergelijking van percutane (PRF) of sinus tarsi (STA) benadering (ook wel; minimaal invasieve technieken) met een extended laterale benadering (ELA). Er werden twee systematische reviews en zeven aanvullende RCTs gevonden. Afzonderlijke vergelijkingen tussen STA en ELA, en tussen PRF en ELA laten vergelijkbare resultaten zien. Zowel voor de STA, als PRF werd er nauwelijks tot geen verschil gevonden in functionele uitkomst (AOFAS; cruciale uitkomstmaat), wanneer vergeleken met ELA (GRADE low en, GRADE moderate, respectievelijk). Daarentegen is het aannemelijk dat met minimaal invasieve technieken (PRF en ELA) het risico op complicaties lager is, dan wanneer er met de ELA benadering wordt behandeld (absoluut risico verschil: -0.23, 95% BI: -0.36 tot -0.11, GRADE moderate en absoluut risico verschil: -0.18, 95% BI -0.23 tot -0.12, GRADE moderate, respectievelijk). De effecten op de hoek van Bohler (belangrijke uitkomstmaat) lijken vergelijkbaar te zijn voor de minimaal invasieve technieken en ELA. Over de effecten op artritis (cruciale uitkomstmaat), malunion en nonunion (belangrijke uitkomstmaten) werd slechts bewijs met een zeer lage bewijskracht, of zelfs geen bewijs gevonden. Redenen voor de (zeer) lage bewijskracht zijn onder andere beperkingen in de studieopzet, waaronder een gebrek aan blindering of onduidelijkheden ten aanzien van randomisatie en allocatie procedure. Ook werden de studies gekenmerkt door een kleine studiepopulatie en een laag aantal cases met als gevolg brede 95% betrouwbaarheidsintervallen. Hierdoor bestaat er ook voor deze vergelijking onzekerheid over de daadwerkelijke effecten van PRF en STA of ELA. Samenvattend lijkt een minimaal invasieve benadering (PRF en STA) tot dezelfde functionele uitkomsten te leiden als een ELA. Daar staat tegenover dat het aannemelijk is dat een minimaal invasieve benadering minder post-operatieve complicaties kent.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Primaire voorkeur voor de patiënt ligt in een zo vlot mogelijk functioneel herstel, met zo min mogelijk operatieve behandelingen. Hierbij zijn met name (chronische) pijnklachten van de voet een belangrijke graadmeter, alsmede het kunnen blijven doen van werk en/of sportactiviteiten. Secundair wordt vaak de schoeibaarheid van de voet op prijs gesteld, waarbij mensen de voorkeur geven aan normale confectie schoenen tegenover orthopedisch schoeisel.
Het voordeel van een operatieve behandeling ten aanzien van activiteiten hervatting en schoeibaarheid maakt dat deze behandeling voor patiënten de voorkeur kan genieten. Het merendeel van de calcaneus fracturen ontstaat bij werkzaamheden en sport. Deze groep patiënten is veelal jong en heeft nog veel arbeidsjaren te gaan. Een kleiner deel van de patiënten krijgt een calcaneus fractuur bij minimaal trauma o.b.v. osteoporose en/of diabetes. Bij deze groep dient het wel of niet opereren in samenspraak met de patiënt worden afgewogen te worden tegen het toegenomen risico op postoperatieve complicaties, en het niet aangetoonde functionele verschil of het verschil in post-traumatische artrose. De patiënt moet voldoende worden geïnformeerd over de behandelopties en verwachting t.a.v. het herstel.
Indien er samen met patiënt gekozen wordt voor een operatieve behandeling is hij of zij gebaat bij een zo laag mogelijk risico op complicaties hetgeen bereikt wordt met een minimaal invasieve behandeling (percutane schroeven of sinus tarsi benadering).
Kosten (middelenbeslag)
Calcaneus fracturen hebben een zeer hoge financiële belasting (Schepers, 2008). Het opereren van calcaneus fracturen, welke aan de criteria zoals eerder genoemd voldoen, leidt naar alle waarschijnlijkheid tot een significante reductie in kosten (Albin, 2020; Brauer, 2005). Er zijn groepen waarbij de risico’s van een operatie te groot zijn (bijv. diabetische calcaneus fracturen), hierbij dient sterk te worden overwogen om een conservatief beleid te voeren indien mogelijk.
Aanvaardbaarheid, haalbaarheid en implementatie
Hiervoor wordt terugverwezen naar module organisatie van zorg. In deze module wordt zeer uitvoerig ingegaan op de relatie tussen volume en postoperatieve morbiditeit in operatief behandelde calcaneusfracturen. In deze module komt het precaire evenwicht tussen patiënten die wel of niet baat hebben bij een operatieve interventie. Dit vergt van de behandelaar expertise op het gebied van de operatieve maar ook de conservatieve behandeling. Daar komt bij dat indien een patiënt om wat voor reden dan ook een operatieve behandeling aan gaat dit bij voorkeur gedaan dient te worden middels een minimaal invasieve benadering. Ook hiervoor geldt dat een uitgebreide ervaring nodig is om middels een minimaal invasieve behandeling een goede reductie te bewerkstelligen.
Rationale
Aanbeveling-1
De meta-analyse van deze richtlijn laat potentieel een beperkt voordeel zien voor de niet-operatieve behandeling van calcaneus fracturen. Zeker bij patiënten waarbij de kans op complicaties en/of slechte functionele uitkomst groot is, is een conservatieve behandeling te prefereren. Dit omdat de kans op complicaties als gevolg van de operatie of post-traumatische artritis/artrose dermate groot zijn dat er geen meerwaarde van een operatieve interventie te verwachten valt. De bewijskracht ten faveure van een conservatieve behandeling is laag.
Bij de behandeling van calcaneusfracturen is er ook plaats voor operatieve interventies.
Met name gezonde patiënten waarbij de fractuur significante laterale comminutie/verbreding laat zien, of een verlaagde hoek van Bohler of fibulair impingment kunnen potentieel profijt hebben van een operatieve behandeling. De werkgroep is van mening dat een operatie overwogen dient te worden bij een aantal fractuur kenmerken (Linsenmaier 2003; Selim, 2022; Dickenson 2021). Bespreek met de patiënt de voor- en nadelen en verwachtingen betreffende het herstel van de operatie ten opzichte van afwachtend beleid en kom door middel van samen beslissen tot een keuze.
Bespreek daarnaast ook wanneer het belangrijk is dat de arts te patiënt ziet en of dat het eventueel ook online kan.
Aanbeveling-2
Ondanks dat een minimaal invasieve behandeling (PRF of STA) geen meerwaarde heeft voor de functionele uitkomst (AOFAS) bij patiënten met een calcaneusfractuur vergeleken met een extended laterale benadering (ELA), laat het gevonden bewijs zien dat er aanvullende argumenten zijn ten faveure van minimaal invasieve behandeling. Patiënten die een operatieve behadeling moeten ondergaan hebben, met welke techniek dan ook, voor deze fractuur wel een aanmerkelijke kans op complicaties, zoals bijvoorbeeld post-operatieve (fractuur gerelateerde) wondinfectie of perifeer zenuwletsel. Deze kans wordt mogelijk tot 20% verkleind indien er een minimaal invasieve behandelmethode wordt verkozen boven ELA.
Onderbouwing
Achtergrond
Tot dusver laten gerandomiseerde studies wisselende uitkomsten zien ten faveure van operatieve of conservatieve behandeling. Zo geeft een operatieve behandeling wellicht minder kans op post-traumatische artrose, maar wel risico op complicaties van de behandeling (bv. wondgenezingsstoornissen). Naast de vraag wat de meest optimale behandeling is, is er ook onduidelijkheid over hoe de operatieve behandeling het beste uitgevoerd kan worden (extended lateraal, sinus tarsi benadering, of percutane repositie en schroeven).
Conclusies / Summary of Findings
PICO A: Operative fixation versus conservative treatment
Functional outcome (AOFAS)
|
Low GRADE |
Operative management may result in little to no difference in patient reported functional outcome, compared with conservative treatment in patients with displaced intra-articular calcaneal fractures.
Source: Selim (2022) |
Arthritis
|
Low GRADE |
Operative management may result in little to no difference in arthritis compared with conservative treatment in patients with displaced intra-articular calcaneus fractures.
Source: Selim (2022) |
Bohler’s angle
|
Very Low GRADE |
The evidence is very uncertain about the effect of operative treatment on Bohler’s angle, when compared with conservative treatment in patients with displaced intra-articular calcaneal fractures.
Source: Hussain (2022) |
Complications
|
Low GRADE |
Operative management may result in an increase in complications (e.g. (wound) infections, rebleeding or nerve damage) compared with conservative treatment in patients with displaced intra-articular calcaneus fractures.
Source: Selim (2022) |
|
- GRADE |
No evidence was found regarding the effect of operative fixation on the outcomes nonunion and malunion when compared with conservative treatment in patients with displaced intra-articular calcaneus fractures.
Source: - |
PICO B: Percutaneous and sinus tarsi approach versus extended lateral approach
1. PERCUTANEOUS FIXATION (PRF) VS EXTENDED LATERAL APPROACH (ELA)
Functional outcome (AOFAS)
|
Low GRADE |
Percutaneous fixation (PRF) may result in little to no difference in functional outcome (AOFAS) when compared with extended lateral approach (ELA) in patients with displaced intra-articular calcaneus fractures.
Source: Chen, 2011; Giray Batibay, 2020; Li, 2020; Vora, 2022 |
Arthritis
|
Very Low GRADE |
The evidence is very uncertain about the effect of percutaneous fixation (PRF) on development of arthritis, when compared with extended lateral approach (ELA) in patients with displaced intra-articular calcaneus fractures.
Source: Jiao, 2021 |
Bohler’s angle
|
Low GRADE |
Percutaneous fixation (PRF) may result in little to no difference in Bohler’s Angle when compared with extended lateral approach (ELA) in patients with displaced intra-articular calcaneus fractures.
Source: Chen, 2011; Sampath Kumar, 2014; Giray Batıbay; Li, 2020; Vora, 2022; Zhai, 2021 |
Complications
|
Moderate GRADE |
Percutanous fixation (PRF) likely decreases the risk of complications when compared with extended lateral approach (ELA) in patients with displaced intra-articular calcaneus fractures.
Source: Chen, 2011; Sampath Kumar, 2014; Lu, 2015; Giray Batibay, 2020; Jiao, 2021; Li, 2020; Vora, 2022; Zhai, 2021 |
Malunion
|
Very low GRADE |
The evidence is very uncertain about the effect of PRF on the outcome malunion, when compared with ELA in patients with displaced intra-articular calcaneus fractures.
Source: Vora, 2022 |
Nonunion
|
- GRADE |
No evidence was found regarding the effect of PRF on nonunion when compared with ELA in patients with displaced intra-articular calcaneus fractures.
Source: - |
2. SINUS TARSI APPROACH (STA) VS EXTENDED LATERAL APPROACH (ELA)
Functional outcome (AOFAS)
|
Moderate GRADE |
Sinus tarsi approach (STA) likely results in little to no difference in functional outcome AOFAS when compared with ELA in patients with displaced intra-articular calcaneus fractures.
Source: Basile, 2016; Cheng, 2017; Li, 2016; Park, 2021; Zhang, 2020; Zhu, 2013; |
Bohler’s angle
|
Low GRADE |
Sinus tarsi approach (STA) may result in little to no difference in Bohler’s Angle, when compared with extended lateral approach (ELA) in patients with displaced intra-articular calcaneus fractures.
Source: Bin Jia, 2017; Cheng, 2017; Li, 2016; Park, 2021; Rastegar, 2021; Xia, 2014; Zhang, 2020; Zhu, 2013 |
Complications
|
Moderate GRADE |
Sinus tarsi approach (STA) likely decreases the risk of complications, when compared with extended lateral approach (ELA) in patients with displaced intra-articular calcaneus fractures.
Source: Basile, 2016; Bin Jia, 2017; Cheng, 2017; Li, 2016; Xia, 2014; Zhang, 2020; Dai, 2022; Park, 2021; Rastegar, 2021 |
Malunion
|
Very Low GRADE |
The evidence is very uncertain about the effect of PRF on the outcome malunion, when compared with ELA in patients with displaced intra-articular calcaneus fractures.
Source: Zhang, 2020 |
Nonunion, arthritis
|
- GRADE |
No evidence was found regarding the effect of STA on nonunion and arthritis when compared with ELA in patients with displaced intra-articular calcaneus fractures.
Source: - |
Samenvatting literatuur
Description of studies
PICO A: Operative fixation versus conservative treatment
Selim (2022) performed a systematic review on the management of displaced intra-articular calcaneal fractures. Studies comparing operative management with non-operative management were eligible for inclusion. The databases Medline, Embase and the Cochrane library were searched for relevant articles published until December 2021. Inclusion criteria were: RCTs and prospective comparative studies, comparing non-operative and operative management of displaced intra-articular calcaneal fractures were included. Cadaveric studies, studies published in non-English language and biomechanical studies of treatment options were excluded. In total, thirteen trials were included in the systematic review, of which nine were considered relevant for the purpose of this guideline (Agren, 2013; Bahari Kashani 2013; Buckley, 2002; Dickenson, 2021; Griffin, 2014; Ibrahim, 2007; Nouraei, 2011; Parmar, 1993; Thordarson, 1996). The baseline characteristics of these studies are presented in Table 1. Studies that were not considered relevant for this guideline were excluded because the studies did not report any of the predefined outcomes (Sharma, 2011) or because of an observational study design (O’Farell, 1993; Rodriguez-Merchan, 1999; Kamath, 2021). Outcomes that were reported included AOFAS-score, complications (types of complications not further specified) and development of arthritis. Risk of bias in the individual studies was assessed with the Cochrane Risk of Bias tool. There was no blinding of the study participants and personnel in all studies.
Table 1: baseline characteristics of the studies included in Selim (2022) that were considered relevant for the purpose of this guideline.
|
|
Country |
Size study population (OF/C) |
Mean age, years (OF/C) |
% male (total population) * |
Follow-up, years (OF/C) |
|
Agren 2013 |
Sweden |
39/37 |
49/48 |
not reported |
12/12 |
|
Bahari Kashani 2013 |
Iran |
84/56 |
not reported |
79 |
not reported |
|
Buckely 2002 |
Canada |
206/218 |
41/39 |
90 |
3/3 |
|
Dickenson 2021 |
UK |
52/66 |
45 |
not reported |
5/5 |
|
Griffin 2014 |
UK |
73/78 |
45/48 |
not reported |
2/2 |
|
Ibrahim 2007 |
UK |
15/11 |
61/58 |
91 |
15/15 |
|
Nouraei 2011 |
Iran |
31/30 |
46/52 |
Not reported |
3/3 |
|
Parmar 1993 |
England |
25/31
|
48/48 |
86 |
2/2
|
|
Thorardson 1996 |
USA |
15/11 |
35/36
|
91 |
1/1 |
Abbreviations: OF = operative fixation, C = conservative treatment
*% not specified for intervention/control group
Hussain (2022) performed a randomized controlled trial to make a comparison between functional results in intra-articular calcaneal fractures which are treated conservatively and those which are treated operatively. The study was executed in a hospital in Pakistan. Patients presenting at the hospital with displaced intra-articular calcaneal fractures were randomized by computer-generated random numbers, to operative treatment (n = 16) or conservative treatment (n = 16). All patients had Sander’s type II (52%) and type III (48%) calcaneal fractures, that were less than 3 weeks old. Patients with calcaneal fractures connected with spinal injuries, pathological fractures, peripheral vasculopathy or any medical contraindication to surgery were excluded. Bohler’s Angle at 1 year follow-up was reported as an outcome.
PICO B: Percutaneous and sinus tarsi approach versus extended lateral approach
This main comparison was subdivided into two sub-comparisons, based on approach that was used for fixation.
- Comparison 1: Percutaneous Fixation (PRF) versus Extended Lateral Approach (ELA)
- Comparison 2: Sinus Tarsi Approach (STA) versus Extended Lateral Approach (ELA)
1. PERCUTANEOUS FIXATION (PRF) VERSUS EXTENDED LATERAL APPROACH (ELA)
The studies mentioned below were extracted from the systematic review of Shi (2020). In this systematic review, a network meta-analysis was performed to evaluate the radiographic characteristics, clinical effectiveness and incision complications of non-operative treatment, open-reduction and internal fixation, minimally invasive reduction and fixation. In this review, a literature search was conducted until 30 December 2019. Studies comparing PRF with ELA were considered relevant for this sub comparison. Since Shi (2020) only reported pooled results, and no data per individual study that was included, it was decided to retrieve the required data from the original papers (Chen, 2011; Sampath Kumar, 2014; Lu, 2015). As the trials from Qi (2009) and Qi (2013) were only published in Chinese, the relevant data could not be extracted.
Chen (2011; from Shi, 2020) performed a randomized controlled trial to compare the outcome of percutaneous reduction, cannulated screw fixation and calcium sulphate cement (CSC) grafting, with the outcomes of traditional open reduction and internal fixation (ORIF), through an extended lateral approach in patients with displaced intra-articular calcaneus fractures. Patients presenting at a Chinese hospital with displaced intra-articular calcaneal fractures including Sanders Type IIB, Type IIC and some Type III were eligible to participate. Additional inclusion criteria were: operative treatment possible within 7 days of injury (some patients with significant swelling could wait for two weeks), closed fractures and unilateral fractures. Patients with known local or systemic infection, medical contraindications or patients with Sanders Type IV and Sanders Type IIA and open fractures were excluded. Patients were randomly divided to percutaneous reduction + CSC (n = 38) or ORIF trough ELA (n = 40). The average time from trauma to operation was 5 days (range 0 to 7), the mean follow-up duration was 24 months (range 18 – 30). Outcomes included Böhler’s angle, AOFAS and infection.
Sampath Kumar (2014; from Shi, 2020) performed a randomized controlled trial to compare minimally invasive percutaneous fixation, with ORIF with an extended lateral approach. Patients with displaced intra-articular fractures of the calcaneus and who presented within 3 weeks after the injury at a hospital in India were included in the trial. Exclusion criteria were: patients with open wound, peripheral vascular disease, skin infection, signs of compartment syndrome, patients with neurologic deficit following head injury or spinal injury and patients with fractures involving other bones of the other limb. Patients were randomized to minimally invasive percutaneous fixation (n = 22) or ORIF (n = 23), by lottery method. Bilateral fractures were included and randomized by individual fracture. Patients had Sanders Type II, Sanders Type III and Sanders Type IV fractures. Outcomes were assessed at 1.5, three, six- and twelve-months follow-up. One patient from the minimally invasive group, and two patients from the ORIF group were lost to follow-up. Outcomes that were reported included wound complications, including infection. The improvement in Böhler’s angle was also reported.
Lu (2015; from Shi 2020) conducted a prospective parallel controlled study to compare ORIF through ELA vs. minimally invasive manipulative reduction with percutaneous k-wire fixation. This trial included 96 patients with closed calcaneal fractures who were admitted to a Chinese hospital. Both groups consisted of 48 patients. Exclusion criteria were: patients of age <18 years or >65 years, simple non-displaced calcaneal fractures, severe collapsed comminuted fractures, patients with severe liver and kidney disorders, psychiatric disorders or accompanied with other severe trauma and open fractures. Patients had Sanders Type II and Type III fractures, consisting of tongue type fractures and compression fractures. Reported outcomes were complications after six months of follow-up (unstable internal fixation, neural and vascular injuries, unfavorable healing).
RCTs published after Shi (2020)
Giray Batıbay (2020) performed a randomized controlled trial to compare closed reduction using dual-point distraction and PRF with ELA. In total, 35 patients with calcaneal fractures who presented to the emergency department (Turkey) between January 2017 and February 2018 were included in the trial. Seventeen patients received PRF treatment and 18 patients received treatment via ELA. Randomization was performed by creating a variable block schedule on a computer system. Patients with diabetes mellitus, osteoporosis and a history of osteoporosis drug therapy, previous ipsilateral foot surgery or fracture, chronic fracture and open fracture were excluded. Patients had Sanders type II, type III and type IV fractures. Outcomes of the study included complication rate (wound complications and postoperative peroneal tendinopathy), AOFAS at 6 months and final follow-up visit, and pre- and postoperative Böhler’s angle.
Li (2020) conducted a randomized controlled trial in which the operation techniques percutaneous reduction and hollow screw fixation (group A) was compared with ORIF with L-shaped lateral approach (group B) among patients with displaced intra-articular calcaneal fractures. In total, 71 patients with calcaneal fractures admitted to a Chinese trauma center from July 2015 to December 2018 were recruited. Twelve patients were excluded since they were followed up for shorter than 12 months. Other exclusion criteria were patients with previous history of calcaneal fracture, other fractures in addition to calcaneal fractures, long-term smoking and diabetes which may affect the prognosis. The final analytical sample was composed of 59 patients, with 31 patients in group A and 28 patients in group B. Patients in both groups had Sanders type II, III, and IV calcaneal fractures. Reported outcomes were AOFAS hindfoot score, pre- and postoperative Böhler’s angle and soft tissue complications (superficial infection, deep infection, wound edge necrosis, and sural nerve injury).
Vora (2022) conducted a hospital-based, double-blind, prospective, randomized, comparative clinical study at the department of Orthopedics, of a tertiary medical hospital in India. In total, 30 patients with closed displaced intra-articular calcaneal fractures with at least 2 mm displacement, were recruited from December 2017 to September 2019, and either received closed reduction using the Essex Lopresti technique (n=15) or ORIF with plating, using the lateral universal approach of calcaneum (n=15). Exclusion criteria were patients with pathological fractures, Gustilo grade III open fracture, and those with neurological deficits. Follow-ups were done at 6 weeks, 2 months, 3 months, and 6 months postoperatively. Reported outcomes were AOFAS hindfoot score, pre- and post-operative Böhler’s angle (at each follow-up visit), and complications (malunion, infection, wound dehiscence).
A randomized controlled trial was conducted by Zhai 2021, in which the effect of closed reduction with cannulated screw internal fixation with plate internal fixation was compared in patients with calcaneal fractures. In total, 60 patients with calcaneal fractures admitted to a Chinese hospital between April 2015 and April 2019 were enrolled in the study and randomly divided in two groups. Thirty patients in group A were operated with closed reduction with hollow screw internal fixation, and 30 patients in group B received open reduction with special-shaped plate internal fixation. Exclusion criteria were patients with open fracture or dated fracture, patients with ankle fracture or tarsal fracture, patients with the history of ankle injury, patients with the ankle dysfunction in the affected limb prior to the fracture, patients with the pathological fracture due to the primary osteogenic tumor, osteoid lesion, cystic pathogenic damage or bone metastases, patients with diseases in nervous system or mental disease. Follow-ups were conducted between three and 15 months after surgery. Reported outcomes were pre- and postoperative Böhler’s angle, intraoperative and postoperative complications (nerve damage, wound infection, marginal necrosis of skin, subtalar arthritis).
2. SINUS TARSI APPROACH (STA) VERSUS EXTENDED LATERAL APPROACH (ELA)
Peng (2021) executed a systematic review and meta-analysis on the STA compared with the ELA. A search was performed in the PubMed, Embase and Cochrane databases on June 2019, for studies comparing STA with ELA in the surgical treatment of calcaneal fractures using internal fixation. Studies in adult calcaneal fracture patients, comparing postoperative outcomes of calcaneal fractures via STA and ELA were included. Eligible study designs were prospective cohort studies, controlled clinical trials and RCTs. Animal or cadaveric studies, and studies from which valid data could not be extracted or converted were excluded from the review. In total, 18 studies were included in the systematic review, of which six were considered relevant for the purpose of this guideline (Basile, 2016; Bin Jia, 2017; Cheng, 2017; Li, 2016; Xia, 2014; Zhu, 2013). The baseline characteristics of these studies are presented in Table 2. The other studies included in the review were not considered relevant as these were observational studies, or non-randomized trials. The relevant trials compared STA and plate fixation with ELA and plate fixation. Outcomes that were reported included Bohler’s Angle, AOFAS-score and complications (wound infections and nerve injury). Risk of bias of the individual studies was assessed with the Jadad Risk of Bias tool for RCTs. The author’s evaluated that most included studies had a low risk of bias. However, after consulting the full text articles of the included studies, there appears to be some inconsistency in the information reported in the review. This introduces some concerns regarding the quality of the systematic review.
Table 2: baseline characteristics of the studies included in Peng (2021) that were considered relevant for the purpose of this guideline.
|
|
Size Study population (STA/ELA) |
Mean age, years (STA/ELA) |
Female (n) (STA/ELA) |
Follow-up, months |
fixation type (STA/ELA) |
|
Basile 2016 |
18/20 |
|
5/5 |
24 |
Plates/plates |
|
Bin Jia 2017 |
60/60 |
38.6 / 35.8 |
20/23 |
12 |
Plates/plates |
|
Cheng 2017 |
33/33 |
36.2 / 35.1 |
8/11 |
Not reported |
Plates/plates |
|
Li 2016 |
32/32 |
40 / 41 |
86* |
12 |
Plates/plates |
|
Xia 2014 |
53/64 |
38 / 37 |
38/37 |
28 |
Plates/plates |
|
Zhu 2013 |
18/20 |
36.6 / 36.4 |
5/7 |
15 |
Plates/plates |
Abbreviations: STA = Sinus Tarsi Approach, ELA = Extended Lateral Approach
*not specified for intervention/control group
RCTs published after Peng (2021)
Park (2021) executed a randomized controlled trial to evaluate the hypothesis that a STA would lead to fewer wound complications than ELA in Sanders Type II calcaneal fractures. The study was executed in a South-Korean hospital. Inclusion criteria were: adult patients (>18 years), Sanders Type 2A and 2B calcaneal fractures, surgery by a single surgeon and patients followed-up for more than one year. Patients with open or bilateral calcaneal fractures were excluded, as well as patients with concomitant head or neurovascular injury. In total 64 patients met the inclusion criteria and were randomized to either STA (n = 32) or ELA (n = 32). Outcomes were assessed at six and at twelve months follow-up. All patients completed the twelve-month follow-up. The primary outcome was wound complications, including both minor and major complications. Minor complications were defined as superficial infections and superficial marginal wound necroses that could be managed without reoperation or with small procedures (minor injuries). Major wound complications included deep infection and deep marginal wound necrosis involving the implants and the bones requiring reoperation. Additional outcomes that were reported included AOFAS, Böhlers Angle and the presence of sural nerve injury.
Rastegar (2021) performed a randomized controlled trial to compare minimally invasive techniques (STA) with ELA in patients with calcaneus fractures. The study was executed in two hospitals in Iran. Patients aged 18-75 years, with intra-articular fractures of the calcaneus (displacement > 2 mm) were eligible to participate, except for patients with open fractures or Sanders Type 4 fractures. Exclusion criteria were: patients with a history of surgery, osteoarthritis, inflammatory arthritis in the foot and ipsilateral ankle, patients with major comorbidities or patients with fractures due to secondary causes at the operation site. Patients were randomly allocated to the minimally invasive approach (n = 15) or ELA (n =15), according to an allocation sequence that was generated by statistical software. Follow-up was at three, six and twelve months. Patients without adequate follow-up were excluded from the study population. The reported outcomes, at twelve months follow-up, were Bohler’s angle and soft tissue complications, including surgical site infection, surgical wound dehiscence, bread union or delayed union, erythema, or cellulitis. Additionally, it was reported that AOFAS was assessed, however, data on this measure were not reported in the article.
Zhang (2020) performed a randomized controlled trial to compare the efficacy of the tarsal sinus approach and the lateral extended approach on intra-articular calcaneal fractures. Patients presenting at a Chinese hospital with closed, Sanders Type II or Type III intra-articular calcaneal fractures were eligible to participate. Patients with extra-articular fractures, bilateral fractures, contra-indications, comorbidities, or foot deformities were excluded. In total 53 patients were randomized to undergo STA, and 53 patients were randomized to ELA. The follow-up duration was six months. Outcomes included AOFAS, Böhler’s angle, complications (infection and nerve injury) and delayed union.
Results
PICO A: Operative fixation versus conservative treatment
Functional outcome (AOFAS)
Four studies from the systematic review by Selim (2022) reported the outcome AOFAS (Agren, 2013; Griffin, 2014; Ibrahim, 2007; Thorardson, 1996). The results were pooled in a meta-analysis. The Mean Difference (MD) between the operative group (n = 142) and the conservative group (n = 137) was 6.68 (95% CI: -3.38 to 17.24), see Figure 1. This was not considered clinically relevant.
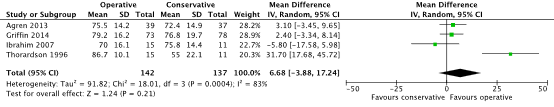
Figure 1. Forest plot showing the comparison of operative fixation with conservative treatment for calcaneal fractures on Functional outcome (AOFAS-score). Pooled relative risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
(Osteo)arthritis
Six studies from the systematic review by Selim (2022) reported the outcome arthritis (Agren, 2013; Bahari Kashani, 2013; Dickenson, 2021; Griffin, 2014; Ibrahim, 2007; Nouraei 2011). The results were pooled in a meta-analysis. The pooled number of patients experiencing arthritis was 81/294 (27.5%) in the operative group, compared to 49/278 (17.6%) in the conservative group. The Risk Ratio (RR) was 1.16 (95% CI 0.54 to 2.50), see figure 2. The pooled Risk Difference (RD) was 0.03 (95% CI -0.11 to 0.16), see figure 3.
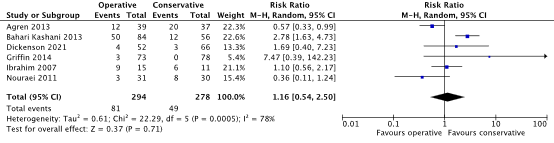
Figure 2. Forest plot showing the comparison of operative with conservative management for calcaneal fractures on the outcome arthritis. Pooled relative risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
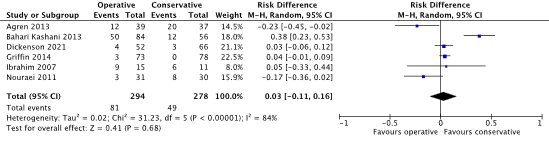
Figure 3. Forest plot showing the comparison of operative with conservative management for calcaneal fractures on the outcome arthritis. Risk difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
Böhler’s angle
One study reported the outcome Böhler’s angle (Hussain, 2022). It was reported that in the operative treatment group (n = 16), at 1-year follow-up Böhler’s angle (mean) was 29.22. In the opposite ‘healthy’ side Böhler’s angle was 31.01. In the conservative treatment group (n= 16), Bohler’s angle (mean) was 11.21. In the opposite ‘healthy’ side, Böhler’s angle was 25.
Complications
Six studies from the systematic review by Selim (2022) reported the outcome complications, (Agren, 2013; Bahari Kashani, 2013; Buckley, 2002; Griffin, 2014; Parmar, 1993; Thorardson, 1996). Bahari Kashani (2013), reported tenosynovitis as complication. The other studies reported complications including (wound) infections, rebleeding or nerve damage. The results were pooled in a meta-analysis. The pooled number of complications was 93/407 (22.9%) in the operative group, compared to 63/431 (14.7%) in the conservative group. The RR was 1.91 (95% CI 0.61 to 6.94), see Figure 4. The pooled RD was 0.12 (95% CI: -0.05 to 0.29), see Figure 5.
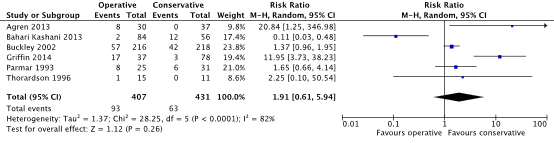
Figure 4. Forest plot showing the comparison of operative with conservative management for calcaneal fractures on the outcome complications. Pooled relative risk ratio, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
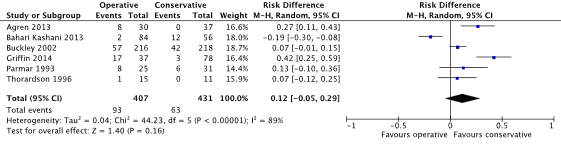
Figure 5. Forest plot showing the comparison of operative with conservative management for calcaneal fractures on the outcome complications. Risk difference, random effects model. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
Malunion
None of the included studies reported the outcome malunion after operative fixation compared to conservative treatment in patients with displaced intra-articular calcaneus fractures.
Nonunion
None of the included studies reported the outcome nonunion after operative fixation compared to conservative treatment in patients with displaced intra-articular calcaneus fractures.
PICO B: Percutaneous and sinus tarsi approach versus extended lateral approach
First, results on the predefined outcomes were presented for the sub comparison 1. percutaneous fixation versus extended lateral approach were presented. Next the results were presented for the sub comparison 2. sinus tarsi approach versus extended lateral approach.
1. PERCUTANEOUS FIXATION (PRF) VERSUS EXTENDED LATERAL APPROACH (ELA)
Functional outcome (AOFAS)
Four studies, of which one was included in the review by Shi (2020), reported functional outcome with the AOFAS (Chen, 2011; Giray Batibay, 2020; Li, 2020; Vora, 2022). Due to heterogeneity in reporting, the result could not be pooled in a meta-analysis. The results of the individual papers are presented in Table 3.
Table 3: AOFAS-scores reported in the studies comparing Percutaneous Fixation and Extended Lateral Approach for patients with calcaneal fractures
|
|
PRF group Mean AOFAS + SD |
ELA group Mean AOFAS + SD |
Mean difference (95% CI) |
|
Chen (2011) |
91.7 (n = 38) |
85.8 (n = 40) |
Can’t be assessed due to lack of SD |
|
Giray Batibay (2020) |
90 ± 2.8 (n = 17) |
78 ± 6.3 (n = 18) |
12.00 (95% CI: 8.80 to 15.20) |
|
Li (2020) |
88.3 (n = 31) |
86.4 (n = 28) |
Can’t be assessed due to lack of SD |
|
Vora (2022) |
78.5 ± 9 (n = 15) |
87.7 ± 5.5 (n = 15) |
-9.20 (95% CI: -14.52 to -3.88) |
Abbreviations: PRF = percutaneous fixation; ELA = extended lateral approach; SD = Standard Deviation; 95% CI = 95% Confidence interval
(Osteo)arthritis
One study reported the outcome subtalar arthritis (Zhai, 2021). In the study of Zhai (2021), 2/32 (6.25%) patients in the PRF group experienced subtalar arthritis, compared to 0/31 (0%) patients in the ELA group. The RD was 0.06 (95% CI: -0.04 to 0.16).
Böhler’s angle
Six studies, of which two were included in the review by Shi (2020), reported the outcome postoperative Böhler’s angle (Chen, 2011; Sampath Kumar, 2014; Giray Batıbay; Li, 2020; Vora, 2022; Zhai, 2021). After surgery, the mean Böhler’s angle in the PRF group ranged between 22 degrees (Vora, 2022) and 33.52 degrees (Zhai, 2021). The mean Böhler’s angle in the ELA group ranged between 28.2 degrees (Giray Batibay, 2020) and 33.09 degrees (Zhai, 2021).
The results from four studies were pooled in a meta-analysis. The pooled MD between the PRF group (n = 93) and the ELA group (n = 91) was -1.51 (95% CI: -3.64 to 0.62), (see Figure 6). As in Chen (2011) no SD’s were reported, the results could not be pooled.
The study of Sampath Kumar (2014) reported an improvement in Böhler’s angle of 18.1 degrees in the PRF group (n = 22) compared to 17.5 degrees in the ELA group (n = 23). Since the mean Böhler’s angle in both groups was not presented, the results of this study could not be pooled.
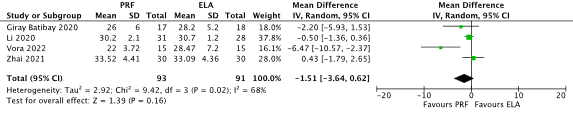
Figure 6. Forest plot showing the comparison percutaneous fixation (PRF) versus extended lateral approach (ELA), for calcaneal fractures on the outcome Böhler’s angle. PRF: percutaneous fixation, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
Complications
Seven studies, of which three were included in the review by Shi (2020), reported the outcome complications (Chen, 2011; Sampath Kumar, 2014; Lu, 2015; Giray Batibay, 2020; Li, 2020; Vora, 2022; Zhai, 2021). The majority of studies reported the overall number of patients with any complication (i.e. wound healing problems, nerve damage, wound necrosis, unstable internal fixation, and peroneal tendinopathy). One study specified the type of complications (infection). The pooled number of complications was 16/203 (7.9%) in the PRF group, compared to 63/203 (31.0%) in the ELA group. The pooled RR was 0.28 (95% CI: 0.17 to 0.46), see Figure 7. The pooled RD was -0.23 (95% CI: -0.36 to -0.11), see Figure 8.
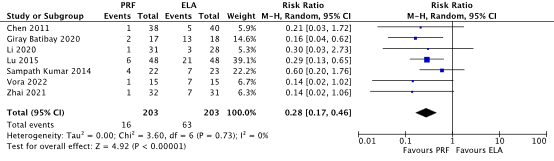
Figure 7. Forest plot showing the comparison percutaneous fixation (PRF) versus extended lateral approach (ELA), for calcaneal fractures on the outcome complications. Pooled Risk Ratio. random effects model. PRF: percutaneous fixation, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; M-H, Mantel Haenszel; CI: confidence interval.
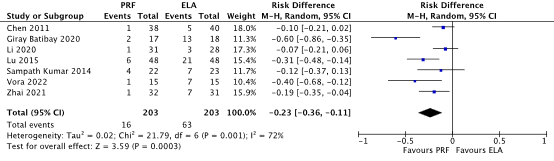
Figure 8. Forest plot showing the comparison percutaneous fixation (PRF) versus extended lateral approach (ELA), for calcaneal fractures on the outcome complications. Pooled Risk Difference. random effects model. PRF: percutaneous fixation, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; M-H, Mantel Haenszel; CI: confidence interval.
Malunion
One study reported the outcome malunion (Vora, 2022). In the study of Vora (2022), 6/15 (40%) patients in the PRF group experienced malunion, compared to 3/15 (20%) patients in the ELA group. The RR was 2.00 (95% CI 0.61 to 6.55).
Nonunion
None of the included studies reported the outcome nonunion for PRF compared to ELA in patients with displaced intra-articular calcaneus fractures.
2. SINUS TARSI APPROACH (STA) VERSUS EXTENDED LATERAL APPROACH (ELA)
Functional outcome (AOFAS)
Six studies, of which four were included in the review by Peng (2021), reported functional outcome with the AOFAS (Basile, 2016; Cheng, 2017; Li, 2016; Zhu, 2013; Park, 2021; Zhang, 2020). The results of the studies were pooled in a meta-analysis. The pooled MD between the STA group (n = 188) and the ELA group (n = 188) was 0.74 (95% CI: -0.44 to 1.91), see Figure 9.
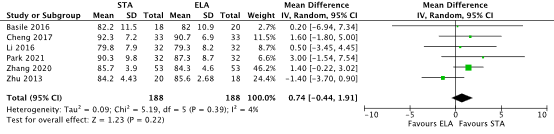
Figure 9. Forest plot showing the comparison Sinus Tarsi Approach (STA) versus extended lateral approach (ELA), for calcaneal fractures on functional outcome (AOFAS). Pooled mean difference, random effects model. STA: Sinus Tarsi Approach, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
(Osteo)arthritis
None of the included studies reported the outcome nonunion for STA compared to ELA in patients with displaced intra-articular calcaneus fractures.
Böhler’s angle
Eight studies, of which four were included in the review by Peng (2021), reported the outcome postoperative Böhler’s angle (Bin Jia, 2017; Cheng, 2017; Li, 2016; Park, 2021; Rastegar, 2021; Xia, 2014; Zhang, 2020; Zhu, 2013). After surgery, the mean Böhler’s angle in the STA group ranged between 21 degrees (Park 2021) and 48.7 degrees (Rastegar 2021). The mean Böhler’s angle in the ELA group ranged between 21 degrees (Park 2021) and 40.5 degrees (Rastegar 2021).
The results were pooled in a meta-analysis. The pooled MD between the STA group (n = 309) and the ELA group (n = 292) was 1.19 (95% CI: -0.44 to 2.81), see Figure 10.
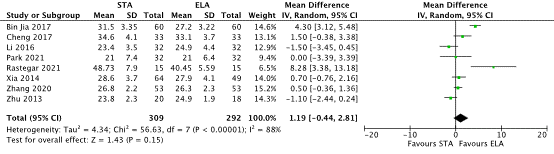
Figure 10. Forest plot showing the comparison Sinus Tarsi Approach (STA) versus extended lateral approach (ELA), for calcaneal fractures on the outcome Böhler’s angle. STA: Sinus Tarsi Approach, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; SD: standard deviation; I2; statistical heterogeneity; CI: confidence interval.
Complications
Eight studies, of which four were included in the review by Peng (2021), reported the outcome complications (Basile, 2016; Bin Jia, 2017; Cheng, 2017; Li, 2016; Park, 2021; Rastegar, 2021; Xia, 2014; Zhang, 2020). Complications that were reported included soft tissue complications, wound infection, flap necrosis or (sural) nerve injury. The pooled number of complications was 10/307 (3.26%) in the STA group, compared to 66/298 (22.1%) in the ELA group. The pooled RR was 0.22 (95% CI: 0.12 to 0.39), see figure 11. The pooled RD was -0.18 (95% CI: -0.23 to -0.12), see figure 12.
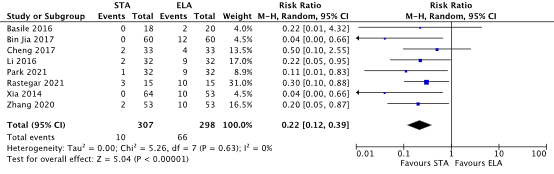
Figure 11. Forest plot showing the comparison Sinus Tarsi Approach (STA) versus extended lateral approach (ELA), for calcaneal fractures on the outcome complications. Pooled risk ratio, random effects model. STA: Sinus Tarsi Approach, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; M-H, Mantel Haenszel; CI: confidence interval.
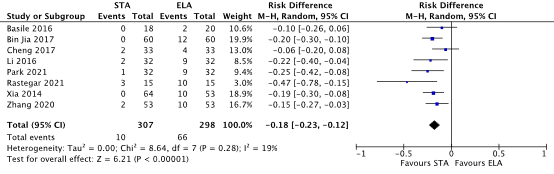
Figure 12. Forest plot showing the comparison Sinus Tarsi Approach (STA) versus extended lateral approach (ELA), for calcaneal fractures on the outcome complications. Pooled risk difference, random effects model. STA: Sinus Tarsi Approach, ELA: Extended Lateral Approach. Z: p-value of overall effect; df: degrees of freedom; I2; statistical heterogeneity; M-H, Mantel Haenszel; CI: confidence interval.
Malunion
One study reported the outcome delayed union (Zhang, 2020). In the study of Zhang (2020), 1/53 (1.89%) patients in the STA group experienced delayed union, compared to 2/53 (3.77%) patients in the ELA group. The RD was -0.02 (95% CI -0.08 to 0.04).
Nonunion
None of the included studies reported the outcome nonunion for STA compared to ELA in patients with displaced intra-articular calcaneus fractures.
Level of evidence of the literature
PICO A: Operative fixation versus conservative treatment
The level of evidence regarding the outcome measure functional outcome (AOFAS) was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including lack of blinding of the participants (-1 risk of bias); and conflicting results (-1 inconsistency). The final level of evidence was graded ‘low’.
The level of evidence regarding the outcome measures complications and arthritis was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of conflicting results (-1 inconsistency) and the 95% confidence intervals crossing the boundaries of clinical decision making (-1 imprecision). The final level of evidence was graded ‘low’.
The level of evidence regarding the outcome measure Böhler’s angle was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of study limitations including lack of similarity of baseline characteristics between intervention and control group (-1 risk of bias); and low number of included patients (-2 imprecision). The final level of evidence was graded ‘very low’
The level of evidence regarding the outcomes nonunion and malunion was not graded as it was not reported in the included studies.
PICO B: Percutaneous and sinus tarsi approach versus extended lateral approach
1. PERCUTANEOUS FIXATION (PRF) VS EXTENDED LATERAL APPROACH (ELA)
The level of evidence regarding the outcome measure functional outcome (AOFAS) was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including lack of blinding of the participants (-1 risk of bias); and conflicting results (-1 inconsistency) The final level of evidence was graded ‘low’.
The level of evidence regarding the outcome measure arthritis was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including unclear randomization procedure (-1 risk of bias) and small sample size and low number of cases (-2 imprecision). The final level of evidence was graded ‘very low’.
The level of evidence regarding the outcome measure Böhler’s angle was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including unclear randomization and allocation procedures (-1 risk of bias); and small sample size (-1 imprecision). The final level of evidence was graded ‘low’.
The level of evidence regarding the outcome measure complications was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by one levels because of study limitations including unclear randomization procedure (-1 risk of bias); The final level of evidence was graded ‘moderate’.
The level of evidence regarding the outcome measure malunion was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by three levels because of study limitations including unclear randomization procedure (-1 risk of bias); and the 95% CI crossing both boundaries of clinical decision making (-2 imprecision). The final level of evidence was graded ‘very low’.
The level of evidence regarding the outcomes nonunion was not graded as it was not reported in the included studies.
2. SINUS TARSI APPROACH (STA) VS EXTENDED LATERAL APPROACH (ELA)
The level of evidence regarding the outcome measure functional outcome (AOFAS) was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by one level because of study limitations including lack of blinding of the participants (-1 risk of bias). The final level of evidence was graded ‘moderate’.
The level of evidence regarding the outcome measure Böhler’s angle was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including unclear randomization and allocation procedures (-1 risk of bias); and large variety in post-operative scores between the individual studies (-1 inconsistency). The final level of evidence was graded ‘low’.
The level of evidence regarding the outcome measure complications was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including unclear randomization procedure (-1 risk of bias). The final level of evidence was graded ‘moderate’.
The level of evidence regarding the outcome measure malunion was retrieved from randomized controlled trials and therefore started high. The level of evidence was downgraded by two levels because of study limitations including unclear randomization procedure (-1 risk of bias), and small sample size and low number of cases (-2 imprecision). The final level of evidence was graded ‘very low’.
The level of evidence regarding the outcomes nonunion and arthritis was not graded as it was not reported in the included studies.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
PICO A: Operative fixation versus conservative treatment
What are the risks and benefits of operative fixation compared to conservative treatment of displaced intra-articular calcaneal fractures?
P: Patients with displaced intra-articular calcaneal fractures
I: Operative management
C: Conservative management
O: Böhler’s Angle, functional outcome (AOFAS), complications (infection, rebleed, nerve damage), malunion, nonunion, (osteo)arthritis
PICO B: Percutaneous and sinus tarsi approach versus extended lateral approach
What are the risks and benefits of surgery via minimal invasive approaches such as percutaneous or sinus tarsi approaches compared to the extend lateral approach in displaced intra-articular calcaneal fractures?
P: Patients with displaced intra-articular calcaneal fractures
I: Percutaneous and sinus tarsi approach (operative fixation)
C: Extended lateral approach (operative fixation)
O: Böhler’s Angle, functional outcome (AOFAS), complications (infection, rebleed, nerve damage), malunion, nonunion, (osteo)arthritis
Relevant outcome measures
The guideline development group considered functional outcome and arthritis
as critical outcome measures for decision making and complications, malunion and nonunion as important outcome measures for decision making.
A priori, the guideline development group defined functional outcome as measured with the American Orthopaedic Foot and Ankle Society (AOFAS) score. For the other outcome measures listed above, the guideline development group decided to use the definitions used in the studies.
For the predefined outcomes the guideline development group defined the minimal clinically (patient) important differences as follows:
- Bohler’s Angle: 15 degrees
- Functional outcome (AOFAS): 10 points
- Dichotomous outcomes (complications, malunion, nonunion of arthritis): Risk Ratio (RR) <0.80 and >1.25 or risk difference (RD) 10%
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms until the 11th of January 2023. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 591 hits. Studies were selected based on the following criteria: systematic reviews and randomized controlled trials comparing A) operative management with conservative management or B) percutaneous and sinus tarsi approach with extended lateral approach. Thirty-five studies were initially selected based on title and abstract screening. After reading the full text, 24 studies were excluded (see the table with reasons for exclusion under the tab Methods), and eleven studies were included.
Results
Three systematic reviews (describing eighteen relevant trials) and eight RCTs were included in the analysis of the literature. Important study characteristics and results are summarized in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
Referenties
- Albin SR, Bellows BK, Van Boerum DH, Hunter S, Koppenhaver SL, Nelson RE, Marcus R, Dibble L, Cornwall M, Fritz JM. Cost-Effectiveness of Operative Versus Nonoperative Management of Patients With Intra-articular Calcaneal Fractures. J Orthop Trauma. 2020 Jul;34(7):382-388. doi: 10.1097/BOT.0000000000001731. PMID: 31917759.
- Bat?bay SG, Bayram S. Comparing open reduction and internal fixation versus closed reduction using dual-point distraction and percutaneous fixation for treating calcaneal fractures. Jt Dis Relat Surg. 2020;31(2):193-200. doi: 10.5606/ehc.2020.72236. Epub 2020 Mar 26. PMID: 32584714; PMCID: PMC7489151.
- Brauer CA, Manns BJ, Ko M, Donaldson C, Buckley R. An economic evaluation of operative compared with nonoperative management of displaced intra-articular calcaneal fractures. J Bone Joint Surg Am. 2005 Dec;87(12):2741-2749. doi: 10.2106/JBJS.E.00166. PMID: 16322625.
- Hussain, Farukh & Bhutto, Ali & Palh, Hussain & Maher, Ahmed & Laghari, Ahmed & Keerio, Hussain & Publication, Professional. A Comparison Between Functional Results in Intra-Articular Displaced Calcaneus Fractures Managed with Conservative and Operative Treatment: A Randomized Controlled Trial. Pakistan Journal of Medical and Health Sciences. 2022. 16. 633. 10.53350/pjmhs22168633.
- Li M, Lian X, Yang W, Ding K, Jin L, Jiao Z, Ma L, Chen W. Percutaneous Reduction and Hollow Screw Fixation Versus Open Reduction and Internal Fixation for Treating Displaced Intra-Articular Calcaneal Fractures. Med Sci Monit. 2020 Nov 4;26:e926833. doi: 10.12659/MSM.926833. PMID: 33147205; PMCID: PMC7650089.
- Park CH, Yan H, Park J. Randomized comparative study between extensile lateral and sinus tarsi approaches for the treatment of Sanders type 2 calcaneal fracture. Bone Joint J. 2021 Feb;103-B(2):286-293. doi: 10.1302/0301-620X.103B.BJJ-2020-1313.R1. Epub 2021 Jan 3. PMID: 33390020.
- Peng C, Yuan B, Guo W, Li N, Tian H. Extensile lateral versus sinus tarsi approach for calcaneal fractures: A meta-analysis. Medicine (Baltimore). 2021 Aug 6;100(31):e26717. doi: 10.1097/MD.0000000000026717. PMID: 34397810; PMCID: PMC8341246.
- Rastegar S, Ravanbod H, Moradi M, Moradi N. Extensile approach versus minimally invasive technique in management of calcaneus fractures. Int J Burns Trauma. 2021 Feb 15;11(1):27-33. PMID: 33824782; PMCID: PMC8012877.
- Schepers T, van Lieshout EM, van Ginhoven TM, Heetveld MJ, Patka P. Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop. 2008 Oct;32(5):711-5. doi: 10.1007/s00264-007-0385-y. Epub 2007 Jun 13. PMID: 17564705; PMCID: PMC2551728.
- Selim A, Ponugoti N, Chandrashekar S. Systematic Review of Operative vs Nonoperative Treatment of Displaced Intra-articular Calcaneal Fractures. Foot Ankle Orthop. 2022 May 26;7(2):24730114221101609. doi: 10.1177/24730114221101609. PMID: 35655706; PMCID: PMC9152199.
- Shi F, Wu S, Cai W, Zhao Y. Comparison of 5 Treatment Approaches for Displaced Intra-articular Calcaneal Fractures: A Systematic Review and Bayesian Network Meta-Analysis. J Foot Ankle Surg. 2020 Nov-Dec;59(6):1254-1264. doi: 10.1053/j.jfas.2020.03.021. Epub 2020 Aug 20. PMID: 32828631.
- Vora, Sapan, and Sandeep Patil. "Comparative Evaluation of Functional and Radiological Outcomes of Open Reduction Internal Fixation (ORIF) with Plating versus Percutaneous Surgical Procedures in the Management of Displaced Intra-Articular Calcaneal Fractures." NeuroQuantology 20.10. 2022. 5483.
- Zhai, L., Huang, K., Lin, B., Guo, Q., Liu, Y., Shen, L., & Ma, G. Application Comparison of Closed Reduction with Hollow Screw Internal Fixation and Open Reduction with Special Shaped Plate Internal Fixation in Calcaneal Fracture. Indian Journal of Pharmaceutical Sciences. 2021 83, 155-160.
- Zhang, Kai, Ruiqing Liu, and Zonggeng Wang. "Comparison of the efficacy of surgeries on intra-articular calcaneal fracture via tarsal sinus approach and lateral extended approach." INTERNATIONAL JOURNAL OF CLINICAL AND EXPERIMENTAL MEDICINE 13.6. 2020: 4421-4425.
Evidence tabellen
Evidence table for systematic review of RCTs and observational studies (intervention studies)
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C)
|
Follow-up |
Outcome measures and effect size |
Comments |
|
Selim 2022
Study characteristics and results are extracted from the SR (unless stated otherwise)
PICO 1 |
SR and meta-analysis of RCTs and observational studies
Literature search up to December 2021
a: Agren, 2013 b: Bahari Kashani, 2013 c: Buckley, 2002 d: Dickenson, 2021 e: Griffin, 2014 f: Ibrahim, 2007 g: Nouraei, 2011 h: Parmar, 1993 i: Sharma, 2011 j: Thordarson , 1996
Study design: a t/m j: RCT
Setting and Country: a: , Sweden b: , Iran c: , Canada d: , UK e: , UK f: , UK g: , Iran h: , England i: , India j: , USA Source of funding and conflicts of interest: Only reported for the systematic review – no conflicts of interest
|
Inclusion criteria SR: - studies directly comparing nonoperative and operative management of intraarticular calcaneal fractures - RCT and prospective comparative - studies in English - studies in human
Exclusion criteria SR: - cadaveric studies - biomechanical studies of treatment options - abstracts, case reports, systematic reviews and retrospective studies
13 studies included in the review, of which 10 were considered relevant (a t/m j)
Important patient characteristics at baseline:
Total population i/c a: 39/37 b: 84/56 c: 206/218 d: 52/66 e: 73/78 f: 15/11 g: 31/30 h: 25/31 i: 15/15 j: 15/11
Mean age i/c (% male) a: 49/48 (not reported) b: not reported (79) c: 41/39 (90) d: 45 (not reported) e: 45/48 (not reported) f: 61/58 (91) g: 46/52 (not reported) h: 48/48 (86) i: 28/29 (70) j: 35/36 (91)
Groups comparable at baseline? Probably yes |
Operative (ORIF)
|
Conservative
|
End-point of follow-up: “The mean follow-up period in the included studies was 4.1 years”
Follow-up (years) a: 12/12 b: not reported c: 3/3 d: 5/5 e: 2/2 f: 15/15 g: 3/3 h: 2/2 i: 2/2 j: 1/1 |
Outcome measure-1 AOFAS
Effect measure: mean difference [95% CI]: a: -3,1 (95% CI: -9.65, 3.45) e: -2.40 (95% CI: -8.14, 3,34) f: 5,8 (95% CI: -5,98, 17,58) j: -31,7 (95% CI: -45,72, -17,68)
Pooled effect (random effects model): 6.68 (95% CI: -3.88, 17.24) favoring operative
Outcome measure-2 complications Effect measure: RR [95% CI]: a: 20.84 (95% CI: 1.25, 346.98) b: 0.11 (95% CI: 0.03, 0.48) c: 1.37 (95% CI: 0.96, 1.95) e: 11.95 (95% CI: 3.73, 38.23) h: 1.65 (95% CI: 0.66, 4.14) NA j: 2.25 (95% CI: 0.10, 50.54)
Pooled effect (random effects model): 1.91 (95% CI: 0.61, 5.94), favouring conservative
Outcome measure-3 arthritis Effect measure: RR [95% CI]: a: 0.57 (95% CI: 0.33, 0.99) b: 2.78 (95% CI: 1.63, 4.73) d: 1.69 (95% CI: 0.40, 7.23) e: 7.47 (95% CI: 0.39, 142.23) f: 1.10 (95% CI: 0.56, 2.17)
g: 0.36 (95% CI: 0.11, 1.24) Pooled effect (random effects model): 1.16 (0.54 – 2.50) favouring conservative
|
The author’s concluded that: “DIACF management should be individualized, and opera- tive treatment has to be reserved for selected cases with cer- tain patient factors and fracture patterns. (…)Fracture patterns with fibular impingement, significant lat- eral comminution, and large Böhler angle show better out- comes with the operative treatment”
Sensitivity analyses “The AOFAS-score favored the ORIF group when Ibrahim et al’s study was removed; however, the study was well conducted and demonstrated a low risk of bias in the quality assessment. Therefore, no good reason was noted to exclude it from the results”
“Complications demonstrated a statistically significant result, favoring the conservative treatment when Bahari Kashani et al’s study was removed”
The studies that were not considered relevant for the purpose of this guideline were excluded based on studies design (observational studies).
One study did not report any of the predefined outcome measures i - Sharma) |
|
Peng 2021
Study characteristics and results are extracted from the SR (unless stated otherwise)
PICO 2 |
SR and meta-analysis of RCTs and observational studies
Literature search up to June 2019
a: Bin Jia, 2017 b: Cheng, 2017 c: Li, 2016 d: Xia, 2014 e: Zhu, 2013
b + e: full tekst of individual study not available
Study design: a t/m e: RCT
Setting: not reported
Source of funding and conflicts of interest: Only reported for the systematic review – no conflicts of interest
|
Inclusion criteria SR: - adult calcaneal fracture patients - studies comparing postoperative functional outcomes of calcaneal fractures via ELA and STA - studies reporting at least 1 of the following outcomes postoperative calcaneal height, postoperative calcaneal width, complications (marginal necrosis, postoperative infection, and nerve injury), operative time, length of hospital stay, postoperative Böhler angle, postoperative Gissane angle, and AOFAS-scores; - Cohort studies, controlled clinical trials and RCTs
Exclusion criteria SR: - animal cadaveric studies - studies in which valid data cannot be extracted or converted - case reports, systematic reviews and meta-analyses, conference papers without full text.
18 studies included in the review, of which 5 were considered relevant (a t/m e)
Important patient characteristics at baseline:
Total population n i/c a: i: 60/ c: 60; b: i: 33/ c:33; c: i: 32/ c:32; d: i: 64/ c:53; e: i: 18/ c:20;
Mean age i/c a: i: 38.6 / c: 35.8 b: i: 36.2 / c: 35.1 c: i: 40 / c: 41 d: i: 38 / c: 37 e: i: 36.6 / c: 36.4 |
a: Sinus tarsi approach; plates b: sinus tarsi approach; plates c: sinus tarsi approach; plates d: sinus tarsi approach; plates e: sinus tarsi approach; plates |
a: Extended lateral approach; plates b: Extended lateral approach; plates c: Extended lateral approach; plates d: Extended lateral approach; plates e: Extended lateral approach; plates |
Duration of follow-up: a: 12 months b: not reported c: 12 months d: 28 months e: 15 months |
Outcome measure 1: Bohler’s angle MD (95% CI) a: 4.30 (95% CI: 3.12, 5.48) b: 1.50 (95% CI: -0.38, 3.38) c: -1.50 (95% CI: -3.45, 0.45) d: 0.70 (95% CI: -0.76, 2.16) e: -1.10 (95% CI: -2.44, 0.24) pooled effect: 0.82 (95%CI: -1.47, 3.11)
Outcome measure 2: AOFAS MD (95% CI) b: 1.60 (95% CI: -1.80, 5.00) c: 0.50 (95% CI: -3.45, 4.45) e: -1.40 (95% CI: -3.70, 0.90) pooled effect: -0.21 (95%CI: -2.06, 1.64)
Outcome measure 3 complications RR (95% CI) Wound infection a: 0.33 (95% CI: 0.04, 3.11) b: 0.50 (95% CI: 0.10, 2.55) c: 0.40 (95% CI: 0.08, 1.91) d: 0.17 (95% CI: 0.01, 3.39)
Nerve injury a: 0.11 (95% CI: 0.01, 2.02)
pooled effect: 0.34 (95% CI: 0.14, 0.84) |
The author’s concluded that: “compared with ELA, an STA is superior in the treatment of calcaneal fractures, due to effective anatomical reduction of the calcaneus, effective reduction of the incidence of incision complications, and shortened operative time and postoperative hospital stay”
The studies that were not considered relevant for the purpose of this guideline were excluded based on studies design (observational studies).
The author’s of the review stated that Basile 2016 was a RCT, however after consulting the full text, the trial appeared to be non-randomized.
Jadad Quality score for RCT a: 5 b: 4 c: 6 d: 5 e: 3
Some concerns regarding the quality of the systematic review. After consulting some of the full text papers, there appear to be some inconsistencies |
Evidence table for intervention studies (randomized controlled trials and non-randomized observational studies [cohort studies, case-control studies, case series])1
This table is also suitable for diagnostic studies (screening studies) that compare the effectiveness of two or more tests. This only applies if the test is included as part of a test-and-treat strategy – otherwise the evidence table for studies of diagnostic test accuracy should be used.
Research question: calcaneus fractures
|
Study reference |
Study characteristics |
Patient characteristics 2 |
Intervention (I)
|
Comparison / control (C) 3
|
Follow-up |
Outcome measures and effect size 4 |
Comments |
|
PICO A |
|||||||
|
Hussain 2022 |
Type of study: RCT
Setting and country: Single Centre, Pakistan 2021 to 2022
Funding and conflicts of interest: none |
Inclusion criteria - Patients with displaced intra-articular calcaneal fractures
Exclusion criteria - patients with calcaneal fractures connected with spinal injuries, pathological fractures, peripheral vasculopathy or any medical contraindication to surgery
N total at baseline: I: n = 16 C: n = 16
Important prognostic factors: All patients had Sander’s type II and III closed fractures that were less than 3 weeks old.
Age i: 40 years c: 42 years
Sex M/F In total study population: 11/32 (34%) female
Groups comparable at baseline? Probably yes
|
Operative treatment
Group B |
Conservative treatment
Group A |
Length of follow-up: 1 year
Loss-to-follow-up: No loss-to-follow-up was reported
|
Böhler’s angle, mean I: 29.22 (opposite ‘healthy’ site: 31.1) C: 11.21 (opposite ‘healthy’ site: 25) à No standard deviations reported
di |
Author’s conclusion: “operative treatment is a better and more effective method to treat displaced intra-articular calcaneal fractures” |
|
PICO B: PRF vs ELA |
|||||||
|
Chen 2011
(from Shi 2020) |
Type of study: RCT
Setting and country: Single Centre, USA 2006 - 2008
Funding and conflicts of interest: None |
Inclusion criteria: - Displaced intra-articular calcaneal fracture (more than 2 mm) - operative treatment possible within 7 days of injury - unilateral fracture - closed fracture
Exclusion criteria: - Patients with known local or systemic infection, - medical contraindication - Sanders type IV, Sanders type IIA and open fractures
N total at baseline: PR + CSC: 38 ORIF, ELA: 40
Important prognostic factors2: age: PR + CSC: 31.1 ORIF, ELA: 32.7
Sex: M/F PR + CSC: 20/18 ORIF, ELA: 24/16
Sanders Type II/III: PR + CSC: 29/9 ORIF, ELA: 32/8
Groups comparable at baseline? Probably yes |
Percutaneous reduction (PR), cannulated screw fixation and calcium sulphate cement (CSC) grafting
PR + CSC
In the percutaneous treatment group, we crossed the tuberosity with a 6.5-mm Schanz pin via stab incision to reduce the height and length of calcaneus. Then, we introduced a 6.5-mm Schanz pin into the fragment with the displaced posterior facet and levered the compressed facet under fluoroscopic guidance. In Sanders Type III fractures, another Schanz pin was introduced percutaneously through the lateral cortex of the inferior calcaneus to unlock and push up any remaining depressed parts of the subtalar joint surface of the calcaneus. Once the Böhler’s angle and articular surface were reduced, two Kirschner wires were inserted from the lateral side to the sustentaculum to sustain the reduced joint surface. Then another two Kirschner wires were introduced from the tuberosity to the anterior part of calcaneus in different directions to fix the primary and secondary fracture line. After the closed reduction and provisional fixation were done, the Kirschner wires were replaced by 6.5- and 3.5-mm cannulated screws percutaneously guided by fluoroscopy. The CSC (Wright Medical Technology, Arlington, TN) was placed into the delivery syringe. The delivery needle was advanced through the channel made by the original Schanz pin under fluoroscopic guidance into the bone void in the body created after the reduction. The cement was then slowly and carefully injected into the bone void under fluoroscopic guidance while the needle was gradually withdrawn. If the surgeon felt resistance, the injection was stopped to prevent the cement from entering the subtalar joint through the fracture line. |
Open Reduction and Internal Fixation (ORIF) through an extensile lateral approach
OR(IF) ELA
The reduction was accomplished under direct visualization. The fracture was fixed with a combination of screws and a calcaneal plate. The wound was sutured carefully with a suction drain. The intraoperative blood loss and postoperative wound blood loss were calculated. |
Length of follow-up: 24 (range 18 – 30) months
Loss-to-follow-up: It was stated that 12 patients were lost to follow-up. These patients were excluded from the analysis
|
Böhler’s angle, mean Postoperative PR + CSC: 32.1 ORIF, ELA: 30.6 MD: unclear (no SD)
AOFAS-score, mean Postoperative PR + CSC: 91.7 ORIF, ELA: 85.8 MD: unclear (no SD)
Complications Infection PR + CSC: 1/38 (2.6%) ORIF, ELA: 5/40 (12.5%) RR: 0.21 (95% CI: 0.03, 1.72)
|
Author’s conclusion: “compared with ORIF, the percutaneous reduction, fixation and CSC grafting for treatment of DIACF might allow accelerated weight bearing activity, reduce joint stiffness and improve the patients’ satisfaction.”
|
|
Sampath Kumar, 2014
(from Shi 2020) |
Type of study: RCT
Setting and country: Tertiary care centre, India, 2010-2011
Funding and conflicts of interest: None |
Inclusion criteria: - Displaced intra-articular calcaneal fracture – evident on radiographs - reporting within 3 weeks of injury
Exclusion criteria: - open wound, peripheral vascular disease, skin infection, signs of compartment syndrome, - patients with neurologic deficit following head injury or spinal injury - patients with fractures involving other bones of the lower limb
N total at baseline: MIRPF: 22 ORIF: 23
Important prognostic factors2: age ± SD: MIRPF: 31.5 ± 11.71 ORIF: 30.7 ± 10.07
Sex: M/F MIRPF: 17/5 ORIF: 18/5
Sanders Type II/III/IV (%) MIRPF: 8.7 / 43.5 / 47.8 ORIF: 31.8 / 40.9 / 27.3
Groups comparable at baseline? Probably yes |
Minimally invasive reduction and percutaneous fixation (MIRPF) The procedure involved disimpaction of fracture fragments with a Steinmann pin inserted mediolaterally from the posteroinferior part of the medial calcaneal tuberosity. Traction was applied along the long axis of the foot, with alternating varus and valgus stress to disimpact fracture fragments. In joint-depression fractures, a stab incision was made in the sole of the foot, and a bone punch was advanced through the primary fracture line into the body of the calcaneus under image guidance. In cases in which bone punch could not be negotiated through the body, a pilot track was drilled over a guidewire placed beneath the depressed fragment under image guidance. The bone punch was inserted into this tract and the depressed fragment elevated by gentle blows of a mallet. Care was taken to avoid entering the subtalar joint. In tongue-type fractures, a Steinmann pin inserted lateral to the Achilles tendon into the tuberosity fragment was used to lever and elevate the displaced fragment. In complex fractures, both techniques were combined as necessary. If reduction was not anatomical after all possible manoeuvres, the procedure was converted to the open method. If reduction was anatomical, the heelwas compressed manually to lock the reduced fragments in position. Temporary fixation was achieved using K-wires or guidewires. Cannulated cancellous screws (4 mm) were used for fragment fixation. A minimum of three screws was used for fixation: two running in the posteroanterior direction and the third running lateral to medial, lying just below the posterior facet in the lateral view and engaging the sustentaculum tali in the axial view. Care was taken to avoid intra-articular screw placement. Additional screws were placed as necessary. |
Open reduction and internal fixation (ORIF) Open reduction was performed using a modified lateral approach with an L-shaped incision; skin subcutaneous tissue and periosteum were raised as a single, thick flap. K-wires were placed in lateral malleolus, talus and cuboid positions and bent to act as curved retractors. Peroneal tendons were elevated off the peroneal tubercle and reflected dorsally, while the calcaneofibular ligament was detached from the calcaneus. After subtalar capsulotomy, the entire lateral calcaneus, including the anterior process that forms the calcaneocuboid joint, was exposed, as necessary. The lateral wall of the calcaneus was then opened like a window to allow access to the articular fragment. Any varus/ valgus deformity of the heel was corrected. Calcaneus length was restored to normal by traction. Fragments were reduced carefully and temporarily fixed using K-wires. Immense care was taken to reconstruct the articular surface, especially of the posterior facet. Autologous bone graft from the iliac crest was used when considered necessary, without adding antibiotics. The lateral wall of the calcaneus was reduced, and a calcaneal locking plate was used for fracture fixation after satisfactory reduction, and locking screws were applied. Additional screws were applied as necessary. Hemostasis was achieved, and the wound was closed over a suction drain. |
Length of follow-up: Patients were followed-up at 1.5, 3, 6 and 12 months postoperatively
Loss-to-follow-up: MIRPF: n = 1 ORIF: n = 2 |
Böhler’s angle, mean ± SD Improvement in Böhler’s angle MIRPF: 18.1 ± 5.4 ORIF: 17.5 ± 6.5 P-value 0.734
Complications Infection MIRPF: 4/22 (31.8%) ORIF: 0/23 (0%)
Wound healing problems MIRPF: 0/22 (0%) ORIF: 7/23 (30.4%) P-value 0.005
|
Author’s conclusion: “minimally invasive reduction and percutaneous fixation is associated with fewer wound-healing problems, better functional outcome and earlier return to work, compared with ORIF”
Bilateral fractures were included and randomization was done separately for each calcaneal fracture |
|
Lu 2015
(from Shi 2020) |
Type of study: RCT
Setting and country: China, July 2012 and July 2014
Funding and conflicts of interest: None |
Inclusion criteria: · cases conforming to the diagnostic criteria for calcaneal fracture; · Closed fracture within two weeks; · CT scan and X-ray examination confirmed Sanders II and Sanders III fractures or compression fracture and tongue type fracture classified by Essex-Lopresti system
Exclusion criteria: · patients of age <18 or >65 years · simple non-displaced calcaneal fractures · severe collapsed comminuted fractures · patients with severe liver and kidney disorders · psychiatric disorders or accompanied with other severe trauma and open fractures
N total at baseline: n = 96 patients PRF: 48 (n=62 feet) ORIF: 48 (n=58 feet)
Important prognostic factors2: age ± SD PRF: 45.12 ± 5.16 years ORIF, ELA: 43.25 ± 4.26 years
Sex: PRF: 75% M ORIF, ELA: 79.2% M
Sanders type II/III fracture PRF: 37/25 feet ORIF, ELA: 34/24 feet
Groups comparable at baseline? Probably yes |
Minimally invasive manipulative reduction using percutaneous poking K-wire fixation (manipulation group, PRF)
The procedures were performed with the patients being in lateral decubitus position under spinal anesthesia. Guided by fluoroscopy, the first K-wire was inserted from the superior external side of the calcaneal tuberosity and advanced to the forefoot without crossing the fracture line. With the forefoot in dorsiflexion position, the K-wire was pulled and poked towards the plantar, and reduction was performed to allow for calcaneal inversion and eversion, as well as flexion and extension of the ankle. Fluoroscopy confirmed that Böhler’s angle was restored within the range of 25°-40° and the length and height of the calcaneus were restored. The K-wire was inserted into the talus after restoring the subtalar joint surface. A second K-wire was inserted at 1-2 cm inferior to the first K-wire and in the direction parallel to the inferior of the calcaneus, for fracture fragments stabilization as well as fixation and support between the tarlus and the calcaneus. The heel was squeezed to reduce the calcaneal width. Finally, the fixation was completed by inserting a third K-wire from the posterior of the calcaneus, traversing the fractured fragments of the subtalar joint and reaching the tarsal bones. Lateral fluoroscopic view demonstrated that the three K-wires formed a ≠ structure. The external end of K-wire was trimmed to 1cm.
|
ORIF (plate group, ELA)
The surgery was performed with patients being in lateral decubitus position under spinal anesthesia. After sterilization, a lateral L-shaped incision was made on the affected foot followed by fracture reduction. Bone grafting was performed if required. Internal fixation was performed using a calcaneal plate (Smith & Nephew, Memphis, TN, USA). Subsequently, a drainage tube was placed, incision was then closed and cast immobilization was performed. |
Length of follow-up: Follow-up at 6 months
|
Complications, n (%) Unstable internal fixation PRF: 4/48 (8.33) ORIF: 0/48 (0)
Neural and vascular injuries PRF: 0/48 (0) ORIF: 5/48 (10.4)
Unfavorable healing PRF: 2/48 (4.17) ORIF: 16/48 (33.3)
|
Author’s conclusion: “lower incidence of adverse reactions and surgical complications was achieved using minimally manipulative reduction with poking k-wire reduction (PRF).”
Manipulative reduction with poking k-wire fixation is suitable for the treatment of Sanders type II tongue type fracture and compression fracture as well as Sanders type III tongue type fracture, with lower cost, rapid recovery and smaller wound. This approach can be employed in clinical practice when surgical indications are met. |
|
Giray Batıbay 2020 |
Type of study: RCT
Setting and country: Turkey, January 2017 and February 2018
Funding and conflicts of interest: None |
Inclusion criteria: · Patients aged >18 years with a minimum one-year follow-up · Unilateral and acute calcaneus fractures
Exclusion criteria: Patients with · Diabetes mellitus · Osteoporosis (T-score <-2.5) ·A history of osteoporosis drug therapy · Previous ipsilateral foot surgery or fracture · Chronic fracture · Open fracture
N total at baseline: n = 35 patients PRF: n = 17 ELA: n = 18
Important prognostic factors2: For example age ± SD PRF: 40.2 ± 10 years ELA: 39.2 ± 9 years
Sex: 62.9% M Information not available per treatment group
Groups comparable at baseline? Probably yes |
PRF This procedure was performed using regional anesthesia without using a tourniquet. The patients were placed in the lateral decubitus position with the injured foot placed on a leg holder in an upper and strictly horizontal position. A free approach to the whole foot was essential to mount the distraction device appropriately and position the fluoroscope optimally. Two Kirschner (K)-wires were used for distraction, with the first pin inserted in the anterior process of the talus and second pin inserted in the distal plantar region of the tuber calcaneus. The entry points of the pins were marked using the lateral view. After manual correction of the varus with distraction, distraction was applied using the lateral and axial views until an adequate length reduction was achieved. As indicated by the bending of K-wires, significant traction was needed to successfully reduce the fractures. We used an angle-stable, single-point distraction device on the medial side. The tension in the foot ligaments (particularly the plantar fascia) can help raise the longitudinal arch through ligamentotaxis as the calcaneal length is restored. For the fixation of the axis, length and height, two 6.5-mm cannulated fully threaded screws were used (Figure 2b). Parallel screws in the central zone can be considered beams supporting the fractured joint fragments above. Local soft-tissue complications significantly reduced with the use of an entry point above the upper border of the Achilles tendon insertion. Reduction of the central joint fragments of the posterior facet was achieved with the lift. Kirschner wires were inserted for the preparation for the insertion of 4.0-mm sustentaculum screws. All patients were evaluated postoperatively with CT. |
ELA This approach was used under regional anesthesia using a tourniquet. The patients were placed in the supine position, and an incision was performed starting 2 cm above the lateral malleolus parallel to the Achilles tendon at the posterior sural nerve continuing distally towards the sole of the foot. Then, the incision was turned anteriorly and continued at the junction between the lateral dorsal normal skin and plantar skin until the calcaneocuboid joint; thereafter, a dorsal turn of 1 cm was performed. The whole layer of the skin flap was separated to fully expose the lateral wall of the calcaneus, subtalar joint and calcaneocuboid joint. A K-wire was drilled to restore the articular surface and fracture reduction. An artificial bone was used to fill the bone defects. When the reduction was satisfactory, as observed by fluoroscopy, a steel plate was inserted for ORIF. The fracture end, calcaneal plate and screw location were confirmed using fluoroscopy |
Length of follow-up: PRF: 23.2 months ELA: 25.3 months
Loss-to-follow-up: None, patients without at least one year follow-up were excluded |
Böhler’s angle, mean ± SD Preoperative PRF: 11.2 ± 5 ELA: 13.1 ± 6.1 P-value 0.41
Postoperative PRF: 26 ± 6 ELA: 28.2 ± 5.2 P-value 0.12
AOFAS, mean ± SD 6 months follow-up PRF: 90 ± 2.8 ELA: 78 ± 6.3 P-value <0.001
Complications Peroneal tendinopathy PRF: 2/17 ELA: 10/18 P-value 0.01
Wound complications PRF: 0/17 ELA: 3/18 P-value 0.03
|
Authors conclusion: “Closed reduction using dual-point distraction can be preferred owing to many advantages including a considerably decreased risk of wound complications, sickness absence period and length of hospital stay as well as superior postoperative rehabilitation with a low pain score.”
Limitations: · Small sample size · Only 24 months of follow-up. Longer follow-up is needed to assess arthritic changes in the subtalar joint, which are the most common complications. · Patient-specific covariates such as smoking habit and medical comorbidities were not evaluated |
|
Li 2020 |
Type of study: RCT
Setting and country: China, trauma center, July 2015 to December 2018
Funding and conflicts of interest: No conflicts of interest. Information about funding not reported. |
Inclusion criteria: · 18-60 years old · with unilateral, closed intra-articular calcaneal fractures displaced >2 mm · with Sanders type II, III, or IV fractures according to CT scans · Patients accepting the treatment plan designated using a random number table
Exclusion criteria: · Patients with previous history of calcaneal fracture · Other fractures in addition to DIACFs · Long-term smoking and diabetes · Patients who were followed up for <12 months
N total at baseline: n = 59 patients Group A: n = 31 Group B: n = 28
Important prognostic factors2: age ± SD Group A: 39.3 ± 9.6 years Group B: 39.1 ± 8.6 years
Sex M/F (n): Group A: 24/7 Group B: 21/7
Sanders type II/III/IV (n): Group A: 9/13/9 Group B: 8/11/9
Groups comparable at baseline? Probably yes |
Percutaneous reduction and hollow screw fixation (PRHCF, group A) One 3.5-mm Steinmann pin was first inserted at the calcaneal tubercle transversely from the medial to lateral sides and was used as the traction pin. The pin was then pulled along the axis of the posterior part of the calcaneus to primarily restore the height and length. Another 3.5-mm Steinmann pin was introduced from the superoposterior portion of the calcaneus into the fracture fragment along its axis to reduce the posterior facet. The pin tip was placed on the major fracture fragment and not beyond the fracture line. Subsequently, the surgeon performed repeated percutaneous leverage by using the pins inserted sagittally through the calcaneus fragment. The reduction was assessed under fluoroscopic control. If satisfactory reduction could not be achieved after repeated leverage, a 0.3-cm stab incision was made at the bottom side of the calcaneus below the lateral malleolus. The top of the vascular forceps or a 3.5-mm Kirchner wire was placed under the collapsed articular bone, which was pulled up to correct the angular malformation of the calcaneus and reduce the collapsed articular surface. Thereafter, the calcaneal width was restored by manually squeezing the surface of both sides of the calcaneal bone, and the 2.0-mm Kirchner wire was used for temporary fixation. After satisfactory reduction confirmed using the C-arm fluoroscopy intensifier, a guide pin was inserted adjacent to the lateral edge of the Achilles tendon from the superoposterior portion of the calcaneal tubercle to the distal part of the fracture. Another guide needle was inserted percutaneously from the site 0.5 cm below the insertion point of the Achilles tendon across the fracture line to the anterior part of the calcaneus. After the satisfactory position of the guide pin was confirmed radiologically, a 6.5-mm diameter hollow screw was inserted to achieve the axial support fixation of the calcaneus. If the fracture of the lateral wall of the calcaneus expanded outwards, 1 to 3 guide pins were inserted percutaneously at the bone block of the lateral side of the calcaneus below the lateral malleolus, and a 4.0-mm hollow screw was inserted to maintain the calcaneal width. Gaskets were used for incomplete bone block. |
ORIF with ELA, group B A curvilinear, L-shaped incision was made at the affected foot. Once the lateral wall of the calcaneus and the subtalar joints were exposed, the full-thickness flap was held in place with three 2.0-mm Kirschner wires (1 each in the fibula, talar neck, and navicular). A Steinmann pin or traction bow was used for reducing the displaced articular surface to allow restoration of the calcaneal shape. After satisfactory reduction, a lateral plate designed for the calcaneus was generally used for rigid fixation. The rubber drains were then inserted into the incision, and the incision was closed in a layered fashion followed by compression bandaging. |
Length of follow-up: Patients were seen for follow-up at one, 3, 6, and 12 months postoperatively and then yearly thereafter.
Loss-to-follow-up: No loss-to-follow-up, since patients who were followed-up for <12 months were excluded from the analysis
|
Böhler’s angle, mean ± SD Preoperative Group A: 10.1 ± 1.7 Group B: 10.4 ± 1.2 P value 0.428
Postoperative Group A: 30.2 ± 2.1 Group B: 30.7 ± 1.2 P value 0.261
AOFAS hindfoot score, mean Postoperative Group A: 88.3 Group B: 86.4 P value 0.08 MD unclear, since SDs were not reported
Soft tissue complications, n (%) Total Group A: 1/31 (3.2) Group B: 3/28 (10.8) P value 0.337 OR=0.28 (95% CI, 0.03;2.84)
Superficial infection Group A: 1/31 (3.2) Group B: 1/28 (3.6)
Deep infection Group A: 0/31 (0) Group B: 1/28 (3.6)
Wound edge necrosis Group A: 0/31 (0) Group B: 1/28 (3.6)
Sural nerve injury Group A: 0/31 (0) Group B: 0/28 (0)
|
Author’s conclusion: “ Percutaneous reduction and hollow screw fixation can achieve comparable reduction and functional outcomes to ORIF in treating DIACFs. Percutaneous reduction and hollow screw fixation can minimize damage to the surrounding tissues, which can subsequently result in shorter operative time and hospital stay, and reduced intraoperative blood loss, postoperative pain, and complication rates. Therefore, percutaneous reduction and hollow screw fixation is a safe and effective treatment choice for DIACFs, and a further randomized controlled trial with a larger sample size is warranted”
Limitations · Small sample size · Differences in surgeons’ performances might have decreased the ability to extrapolate the results of this study · Validated PROMs were not included in initial study design |
|
Vora 2022 |
Type of study: RCT
Setting and country: Hospital in India, December 2017 to September 2019
Funding and conflicts of interest: No information |
Inclusion criteria: · 16-75 years old · Reporting to the Orthopedics OPD/casualty section with closed DICF · with >2 mm displacement, as per Essex Lopresti classification
Exclusion criteria: · Patients with pathological fractures · Gustilo grade III open fracture · neurological deficits
N total at baseline: n = 30 patients Group P: n = 15 Group O: n = 15
Important prognostic factors2: age ± SD Group P: 41 ± 11.70 years Group O: 41.4 ± 11.25 years
Sex M/F (n): Group P: 12/3 Group O: 12/3
Joint depression/tongue type fracture (n): Group P: 7/8 Group O: 8/7
Groups comparable at baseline? Yes, but not for hospitalization duration |
Percutaneous surgery (PS, group P) The patients were treated with closed reduction (PS) using the Essex Lopresti technique. Patients were placed prone on an operating table with their foot protruding. To achieve reduction, one or two ST pins were inserted from the calcaneal tuberosity towards the subtalar joint, under image intensifier control. Stress over the axis was given onto the pins down the distal side to correct Bohler’s angle. Final fixation and stabilization were done using Steinman pins alone or K wires with percutaneous screws. |
ORIF with plating, using the lateral universal approach of calcaneum, group O The patients were placed in a lateral decubitus position on a radiolucent operating table, with the foot elevated on an appropriate support. A full-thickness, L-shaped, lateral incision was made, with a gentle curve between the two segments. The fracture was reduced and temporarily fixed with K-wires under radiographic guidance. Various types of calcaneal plates like simple reconstruction plates, Y-reconstruction plates, H-plates and anatomical calcaneal plates were used for final stabilization. |
Length of follow-up: Patients were seen for follow-up at 6 weeks, 2 months, 3 months and 6 months postoperatively
Loss-to-follow-up: Not reported
|
Böhler’s angle, mean ± SD Preoperative Group P: 8.73 ± 4.94 Group O: 5.93 ± 4.98 P value 0.1331
6 months postoperative Group P: 22 ± 3.72 Group O: 28.47 ± 7.20 P value 0.0056
AOFAS hindfoot score, mean ± SD 6 months postoperative Group P: 78.53 ± 8.98 Group O: 87.73 ± 5.46 P value 0.0021
Complications, n (%) Infection Group P: 1/15 (6.67) Group O: 3/15 (20) P value 0.5957
Wound dehiscence Group P: 0/15 (0) Group O: 4/15 (26.67) P value 0.1004
Malunion, n (%) Group P: 6/15 (40) Group O: 3/15 (20) P value 0.4138
|
Author’s conclusion “ORIF was found to be associated with better functional and radiological outcomes compared to PS”
Limitations Single center approach with small sample size |
|
Zhai 2021 |
Type of study: RCT
Setting and country: Hospital in China, April 2015 to April 2019
Funding and conflicts of interest: No information about funding, no conflicts of interest |
Inclusion criteria: · Patients with fresh, closed, calcaneus fracture · Patients who underwent the regular X-ray examination, computed tomography (CT) scanning and 3-dimensional reconstruction · Patients who took the symptomatic treatment, including fixation, raising and detumescence of affected limb, and active treatment for the complications of fracture
Exclusion criteria: · Patients with open fracture, or dated fracture · Patients with ankle fracture or tarsal fracture · Patients with the history of ankle injury · Patients with the ankle dysfunction in the affected limb prior to the fracture · Patients with the pathological fracture due to the primary osteogenic tumor, osteoid lesion, cystic pathogenic damage, or bone metastases · Patients with diseases in nervous system or mental disease.
N total at baseline: n = 60 patients Group A: n = 30 (32 feet) Group B: n = 30 (31 feet)
Important prognostic factors2: age ± SD Group A: 36.85 ± 7.42 years Group B: 37.26 ± 7.38 years
Sex M/F (n): Group A: 21/9 Group B: 23/7
Sanders fracture type II/III (n): Group A: 19/11 Group B: 18/12
Groups comparable at baseline? Yes |
closed reduction with hollow screw internal fixation, group A Patients were anesthetized in supine position by the combined spinal and epidural analgesia, followed by the sanitization and draping and surgical treatment under the C-type arm. Punctuating point and direction were selected upon the preoperative X-ray examination and CT examination. From the posterior and lower calcaneal tuberosity, a 4.0 Steinmann pin was drilled vertically and flipped to tract to correct the varus and shortening of calcaneus. Then, under the guidance of C-type arm, a guide pin was inserted percutaneously from the calcaneus tuberosity to fix the site of fracture. Later, in the lateral side of the Achilles tendon, a Steinmann pin was drilled on the top of the calcaneal tuberosity, where the pin tip was advanced to the fracture space and then lifted up to support the bone on the articular surface to correct the Bohler angle and Gissane angle, while the bone at the fracture site was fixed by the 1 or 2 pins drilled beneath the lifted pin. Otherwise, 1 or 2 cannulated screws were inserted along the pin, and the pin was then taken out, followed by suture and plaster external fixation. |
Surgical open reduction and internal fixation of irregular steel plates, group B Patients were anesthetized in lateral position of the non-affected side by the combined spinal and epidural analgesia. An L-shape incision was made on the lateral calcaneus and in the middle of Achilles's tendon and fibula and the boundary between the dorsal and pedis of foot skin, a longitudinal and horizontal incision was made respectively. Then, the incision of the calcaneocuboid joint slightly leaned against the dorsal side. During the surgery, incision should reach the surface of bone, where the electrotome was only suggested for hemostasis. To expose the tendon of peroneus longus, the tissues from the skin to the periosteal flap were flicked over, and then 3 kirschner wires were inserted into the astragalus to fix the flaps. Thereafter, paries lateralis was open to expose the lower joint surface which was then turned over by 90°, and then the sclerites in collapse were poked to restore the Gissane angle. The middle to lower joint surface, if necessary, could be exposed by removing the fat in the tarsal canal, while since the anterior to the lower joint surface was hardly to be exposed, a kirschner wire was inserted transversely through the calcaneus tuberosity and dragged downwards to restore the Bohler angle. Thereafter, along the calcaneal axis, a kirschner wire was used to poke to restore the calcaneus height and then inserted directly into the astragalus for restoration and to widen the calcaneus by suppressing longitudinally the paries lateralis of calcaneus. Under the C-shape arm, Bohler angle was adjusted to 30° and after the joint restoration, the artificial bone or iliac bone was inserted in the space of calcaneus according to the defect of subarticular surface bone. A suitable, plastic plate was placed on the paries lateralis of calcaneus, where the screw should be inserted into the sustentaculum tali. Finally, the kirschner wires were taken out, with the thorough hemostasis and a drainage tube was inserted, followed by the suture and compressed dressing. |
Length of follow-up: All patients were followed up for 3-15 months, average follow-up 10.15 ± 2.67 months
Loss-to-follow-up: Not reported
|
Böhler’s angle, mean ± SD Preoperative Group A: 14.19 ± 2.47 Group B: 14.08 ± 2.35 P value 0.857
3 months postoperative Group A: 33.52 ± 4.41 Group B: 33.09 ± 4.36 P value 0.0056
Complications, n (%) Nerve damage Group A: 0/32 (0) Group B: 0/31 (0)
Superficial wound infection Group A: 1/32 (3.13) Group B: 3/31 10.0)
Deep infection Group A: 0/32 (0) Group B: 1/31 (3.23)
Marginal necrosis of skin Group A: 0/32 (0) Group B: 3/31 (10.0)
Subtalar arthritis, n (%) Group A: 2/32 (6.25) Group B: 0/31 (0)
|
Author’s conclusion: “closed replacement and internal fixation of cannulated screw and surgical open reduction and internal fixation of irregular steel plates can both gain promising outcomes in terms of the replacement and postoperative recovery of foot function for calcaneal fracture, while the former is excellent in the mild surgical trauma and low incidence of postoperative complications.”
Limitations Small sample size No information about loss-to-follow-up |
|
PICO B: STA vs ELA |
|||||||
|
Park 2021 |
Type of study: RCT
Setting and country: Single centre, South-Korea, 2013 to 2018
Funding and conflicts of interest: None, non-commercial grant. |
Inclusion criteria: - adult patients aged > 18 years - Sanders type 2A and 2B calcaneal fracture - surgery by a single surgeon - follow-up of patients > 1year
Exclusion criteria: - open calcaneal fracture - bilateral intra-articular calcaneal fracture - Sanders Type 1, 2C, 3 and 4 - concomitant head or neurovascular injury
N total at baseline: STA: 32 ELA: 32
Important prognostic factors2: age ± SD: STA: 50.4 ± 13.9 ELA: 48.8 ± 11.9
Sex: M/F STA: 28/4 ELA: 29/3
Only Sanders type II included.
Groups comparable at baseline? Probably yes |
Sinus Tarsi Approach (STA)
A 4 cm incision was made from the tip of the lateral malleolus to the level of the calcaneum joint toward the fifth metatarsal. After exposing the fracture site, the impacted posterolateral fragment was elevated using a curette. Calcaneal alignment and height were restored by valgus and downward stress using the Steinmann pin that was inserted into the calcaneal tuberosity. Calcaneal width was restored by compressing the heel by applying force to the lateral aspect. After reducing the posterolateral fragment, Kirschner wires were temporarily fixed to the medial fragment and definite fixation of the posterolateral fragment was performed using two 2.7 mm cortical screws. Fixation between the anterior process and posterior facet fragment was then performed using two or three 7.0 mm cannulated screws. |
Extensile lateral approach (ELA)
A vertical limb incision was made along the lateral edge of the Achilles tendon and a horizontal limb incision was made along the junction of plantar skin and skin of lateral aspect of the foot skin. The lateral wall was retracted inferiorly to expose the fracture site. After reducing the posterolateral fragment, fixation of the posterolateral fragment was performed using two 2.7 mm cortical screws. After restoration of the length and height of the calcaneus, a calcaneal locking plate (DePuy Synthes, West Chester, Pennsylvania, USA) was applied to stabilize the anterior process and posterior facet fragment). |
Length of follow-up: Follow-up at 6 and 12 months
Loss-to-follow-up: STA: n = 0 ELA: n = 0 |
Böhler’s angle, mean ± SD STA: 21 ± 7.4 ELA: 21 ± 6.4
AOFAS-score, mean ± SD 12 months follow-up STA: 90.3 ± 9.8 ELA: 87.3 ± 8.7
Complications, n (%) Wound complications: STA: 0/32 (0) ELA: 4/32 (12.5)
Sural Nerve injury STA: 1/32 (3.1) ELA: 3/32 (9.4)
|
Author’s conclusion: “The extensile lateral approach showed higher frequency of wound complications than the sinus tarsi approach for Sanders type 2 calcaneus fractures, even though there was no statistical significance. -- The sinus tarsi approach showed better short-term clinical results and shorter operation time than the extensile lateral approach.”
Wound complications included minor and major complications. Minor complications: superficial infections and superficial marginal wound necroses that could be managed without reoperation or with small procedures (minor injuries). Major complications: deep infection and deep marginal wound necrosis involving the implants and the bones requiring reoperation. |
|
Rastegar 2021 |
Type of study: RCT
Setting and country: Two centres in Iran, in 2019
Funding and conflicts of interest: None |
Inclusion criteria: - patients aged 18 - 75 - intra-articular fracture of the calcaneus with a displacement (more than 2 mm)
Exclusion criteria: - previous history of surgery, osteoarthritis, and inflammatory arthritis in the foot and ipsilateral ankle, absence of major comorbidities, smoking - patients with fractures due to secondary causes at the operation site
N total at baseline: n = 30 STA: 15 ELA: 15
Important prognostic factors2: age ± SD: STA: 41.6 ± 7.5 ELA: 35.3 ± 11.7
Sex: M/F STA: 11/4 ELA: 12/3
Groups comparable at baseline? Probably yes |
STA
Minimally invasive technique
The patient was placed in a lateral position. The tourniquet was closed above the ankle and left on for up to 2 hours. The incision was given from the site of the lateral malleolus to the base of the fourth metatarsus. With the help of this method, posterior facet and, if necessary, anterior and calcaneocuboid joint facets could be seen and reduced. |
Extensile lateral approach (ELA)
In the second group, the patient was placed in the lateral position. The tourniquet was closed above the ankle and left on for up to 2 hours. The patient underwent surgery using a large L-shaped incision in the lateral ankle according to Benirshcke and Sangeorzan methods. All surgeries were performed by a single orthopedic surgeon and the same surgical team. |
Length of follow-up: Follow-up at 3, 6, and 12 months
Loss-to-follow-up: None, patients without adequate follow-up at 12 months were excluded |
Böhler’s angle, mean ± SD STA: 48.73 ± 7.9 ELA: 40.45 ± 5.59
Complications, n (%) Soft tissue complications STA: 3/15 (20) ELA: 10/15 (66.7)
|
Author’s conclusion: “The extensile approach was associated with lower pain, lower Boehler angle and better quality of reduction compared to minimally invasive technique but also higher operation duration and surgical site complication”
The incidence of soft tissue complications such as surgical site infection, surgical wound dehiscence, bread union or delayed union, erythema or cellulitis were recorded by the orthopedic surgeon during 12 months of follow-up. |
|
Zhang 2020 |
Type of study: RCT
Setting and country: Single Centra, China, 2017 to 2019
Funding and conflicts of interest: None |
Inclusion criteria: - patients with Sanders types II and III intra-articular calcaneal fracture - closed fractures - single foot
Exclusion criteria: - extra-articular calcaneal fractures, - Sanders type IV - surgical contraindications - foot deformities - congenital diseases - abnormal foot function
N total at baseline: n = 106 STA: 53 ELA: 53
Important prognostic factors2: age ± SD total population: 41.57 ± 2.63, 24-58 years
Sex: M/F In total: 59/47
Sanders type II/III fractures Total population 55 cases type II 51 cases type III
Groups comparable at baseline? Probably yes |
Tarsal sinus approach (group A, STA)
That is, an incision about 3 cm long was cut along the long axis of fibula, 1-2 cm below the ankle in order to expose the tarsal sinus, and then the fracture site was adjusted using a Steinmann pin. After that, the fracture site was fixed temporarily using 2-3 Kirschner wires. The calcaneus was repositioned by manipulation, and after the reposition standard was met, a hollow screw was inserted into the tarsal sinus for fixation.
|
Lateral Extended approach (group B, ELA)
That is, the standard surgical method of lateral incision was used, the skin of the foot was cut open to the heel, about 1 cm above the junction between the instep and sole, the periosteum was stripped, the fractured end of calcaneus was opened and repositioned using a medical stripper. The articular surface was observed using X-ray. When the reposition standard was met, the fracture site was fixed with a medical screw and a medical steel plate. |
Length of follow-up: Follow-up at 6 months
Loss-to-follow-up: None, patients without adequate follow-up at 6 months were excluded |
Böhler’s angle, mean ± SD STA: 26.8 ± 2.2 ELA: 26.3 ± 2.3 P value 0.316
AOFAS hindfoot score, mean ± SD 6 months follow-up STA: 85.7 ± 3.9 ELA: 84.3 ± 4.6 P value 0.108
Complications, n (%) Wound infection: STA: 1/53 (1.9) ELA: 4/53 (7.6)
Nerve injury STA: 0/53 (0) ELA: 1/53 (1.9)
Delayed union STA: 1/53 (1.9%) ELA: 2/53 (3.8%)
|
Author’s conclusion: “both surgeries via the tarsal sinus approach and the lateral extended approach have a good efficacy on intra-articular calcaneal fracture. However, compared with the lateral extended approach, the tarsal sinus approach has less intraoperative blood loss, shorter getting out-of-bed time, shorter length of stay and fewer postoperative complications.” |
Risk of bias table for intervention studies (randomized controlled trials; based on Cochrane risk of bias tool and suggestions by the CLARITY Group at McMaster University)
Research question: UV3 calcaneus
|
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated?
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measure
LOW Some concerns HIGH
|
||
|
|
Hussain 2022 PICO A |
Probably yes;
Reason: it was stated that computer generated random number tables were used
|
No information on allocation concealment |
Probably no;
Reason: no information, however due to the nature of the intervention blinding is unlikely |
Probably yes
Reason: there were no patients reported to be lost to follow-up |
Probably yes;
Reason: outcomes stated in the method section were reported |
Probably no;
Reason: it is not clear if the intervention and control group had similar baseline characteristics as Böhlers Angle in the healthy foot was 31.01 versus 25 degrees respectively |
Some concerns for the outcomes Bohlers angle |
||
|
STA vs ELA |
||||||||||
|
|
Chen 2011 (from Shi 2020 ) PICO B |
No information on allocation sequence generation (but it was stated that patients were randomly assigned) |
No information on allocation concealment |
Probably no;
Reason: it was stated that examinations were blinded as participants were not directly involved with the care of patients in either group. Additional information on blinding procedures was not provided |
Probably yes
Reason: 12 patients were lost to follow-up, these were excluded from the analysis. Not clear from which group. |
Probably yes;
Reason: outcomes stated in the method section were reported |
Probably yes;
Reason: no other sources of bias could be identified |
Some concerns for all outcomes
Unclear randomization and blinding procedure |
||
|
|
Sampath Kumar 2014 (from Shi, 2020) PICO B |
Definitely yes;
Reason: randomisation by lottery method |
No information |
Definitely no
Reason: it was stated that blinding methods were not feasible |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group (n =1 and n = 2) |
Definitely yes
Reason: outcomes stated in the method section were reported |
Probably no
Reason: bilateral fractures were included. Infection occurred in three fractures from two patients |
Some concerns for functional outcome
High for infection. |
||
|
|
Lu 2015 (from Shi, 2020) PICO B |
No information on allocation sequence generation (but it was stated that patients were randomly divided into two groups) |
No information on allocation concealment |
Probably no;
Reason: No information, however due the nature of the intervention it is likely that there was no blinding |
No information on loss to follow-up |
Probably yes;
Reason: outcomes stated in the method section were reported
|
Probably yes;
Reason: no other sources of bias could be identified |
High for all outcomes
Problems with blinding, unclear randomization, unclear loss to follow-up |
||
|
|
Giray Batıbay 2020 PICO B |
Definitely yes
Reason: A variable block schedule was created on a computer system for randomization |
Definitely yes
Reason: The list containing the resulting treatment groups was stored in sealed non-transparent envelopes. |
Probably no
Reason: No information, however, due to the nature of the intervention, it is likely that there was no blinding |
Definitely yes
Reason: Patients without adequate follow-up were excluded from the study population |
Definitely yes
Reason: Outcomes stated in the method section were reported |
Definitely yes
Reason: no other sources of bias could be identified |
Some concerns for AOFAS (patient-reported outcome) Low for Böhler’s angle and complications (both hard outcomes)
Problems with blinding |
||
|
|
Li 2020 PICO B |
Definitely yes
Reason: a random number table was used |
No information |
Probably yes
Reason: outcomes were assessed by an orthopedic surgeon who was blind to the patient grouping. No information about blinding of patients. |
Probably yes
Reason: in total, 12 patients were lost to follow-up and were excluded from the analysis, but not clear from which group. It is likely that 4 patients in group A were excluded and 8 patients in group B (or vice versa), given that 71 patients were enrolled in the study. |
Definitely yes
Reason: Outcomes stated in the method section were reported |
Definitely yes
Reason: no other sources of bias could be identified |
Low for Böhler’s angle and complications
|
||
|
|
Vora 2022 PICO B |
No information |
No information |
Probably yes
Reason: it was stated that the study was double blind, but given the nature of the intervention, this is questionable. |
No information |
Definitely yes
Reason: Outcomes stated in the method section were reported |
Probably no
Reason: “… double-blind study”, so researcher and patients are blinded, but how is this possible? |
High for all outcomes
Outcomes AOFAS hindfoot score, Böhler’s angle, complications
Reason: no information about allocation sequence generation, allocation concealment, loss-to-follow-up |
||
|
|
Zhai 2021 PICO B |
No information, but it was stated that patients were randomized |
No information |
No information |
No information |
Definitely yes
Reason: Outcomes stated in the method section were reported |
Definitely yes
Reason: no other sources of bias could be identified |
High for all outcomes
Reason: no information about crucial elements to judge RoB (randomization method, allocation concealment, blinding, loss-to-follow-up) |
||
|
|
STA vs ELA |
|||||||||
|
|
Park 2021, PICO B |
No information on allocation sequence generation (but it was stated that patients were randomly assigned) |
No information on allocation concealment |
Probably no;
Reason: No information, however due the nature of the intervention it is likely that there was no blinding |
Probably yes;
Reason: it was stated that no patients were lost to follow-up |
Probably yes;
Reason: outcomes stated in the method section were reported
|
Probably yes;
Reason: no other sources of bias could be identified |
Some concerns for all outcomes
Unclear randomization and blinding procedure |
||
|
|
Rastegar 2021 PICO B |
Definitely yes;
Reason: allocation sequence was generation with random allocation software |
No information |
Probably no;
Reason: No information, however due the nature of the intervention it is likely that there was no blinding |
Probably yes;
Reason: patients without adequate follow-up were excluded from the study population |
Definitely no;
Reason: in the method section it is stated that AOFAS and VAS were reported as an outcome, but these were not reported in the result section |
Probably yes;
Reason: no other sources of bias could be identified |
High for all outcomes
No blinding and selective outcome reporting. |
||
|
|
Zhang 2020 PICO B |
No information on allocation sequence generation (but it was stated that patients were randomly assigned) |
No information on allocation concealment |
Probably no;
Reason: No information, however due the nature of the intervention it is likely that there was no blinding |
Probably yes;
Reason: patients without adequate follow-up were excluded from the study population |
Probably yes;
Reason: outcomes stated in the method section were reported
|
Probably yes;
Reason: no other sources of bias could be identified |
Some concerns outcomes
Unclear randomization and blinding procedure |
||
Table of excluded studies
|
Reference |
Reason for exclusion |
|
Bai L, Hou YL, Lin GH, Zhang X, Liu GQ, Yu B. Sinus tarsi approach (STA) versus extensile lateral approach (ELA) for treatment of closed displaced intra-articular calcaneal fractures (DIACF): A meta-analysis. Orthop Traumatol Surg Res. 2018 Apr;104(2):239-244. doi: 10.1016/j.otsr.2017.12.015. Epub 2018 Feb 2. PMID: 29410159. |
More recent + complete SR available (Lv 2021 / Peng 2021), RCTs and comparative retrospective studies |
|
Bruce J, Sutherland A. Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. Cochrane Database Syst Rev. 2013 Jan 31;(1):CD008628. doi: 10.1002/14651858.CD008628.pub2. Update in: Cochrane Database Syst Rev. 2023 Nov 7;11:CD008628. PMID: 23440830. |
More recent, and higher quality SR's available (Selim 2022) |
|
Dai F, Xu YF, Yu ZH, Liu JT, Zhang ZG. Percutaneous Prodding Reduction and K-Wire Fixation Via Sinus Tarsi Approach Versus ORIF for Sanders Type III Calcaneal Fractures: A Prospective Case-Controlled Trial. J Foot Ankle Surg. 2022 Jan-Feb;61(1):37-42. doi: 10.1053/j.jfas.2021.06.005. Epub 2021 Jun 18. PMID: 34253433.
|
Wrong intervention: percutaneous prodding reduction and k-wire fixation versus ORIF |
|
Fan B, Zhou X, Wei Z, Ren Y, Lin W, Hao Y, Shi G, Feng S. Cannulated screw fixation and plate fixation for displaced intra-articular calcaneus fracture: A meta-analysis of randomized controlled trials. Int J Surg. 2016 Oct;34:64-72. doi: 10.1016/j.ijsu.2016.08.234. Epub 2016 Aug 30. PMID: 27565242. |
Article in Chinese |
|
Gougoulias N, Khanna A, McBride DJ, Maffulli N. Management of calcaneal fractures: systematic review of randomized trials. Br Med Bull. 2009;92:153-67. doi: 10.1093/bmb/ldp030. PMID: 19734165. |
More recent, and higher quality SR's available (Selim 2022) |
|
Jiang N, Lin QR, Diao XC, Wu L, Yu B. Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. Int Orthop. 2012 Aug;36(8):1615-22. doi: 10.1007/s00264-012-1563-0. Epub 2012 May 11. PMID: 22576080; PMCID: PMC3535025. |
More recent, and higher quality SR's available (Selim 2022) |
|
Jiao L, Li H, Liao T, Han Z, Wu H, Jiang L. Impact of percutaneous poking reduction combined with minimally invasive plate internal fixation on foot function and complications of patients with Sanders type II and III calcaneal fractures. Am J Transl Res. 2021 May 15;13(5):5329-5335. PMID: 34150126; PMCID: PMC8205695.
|
Wrong intervention: percutaneous poking reduction and minimally invasive plate internal fixation versus |
|
Luo X, Li Q, He S, He S. Operative Versus Nonoperative Treatment for Displaced Intra-Articular Calcaneal Fractures: A Meta-Analysis of Randomized Controlled Trials. J Foot Ankle Surg. 2016 Jul-Aug;55(4):821-8. doi: 10.1053/j.jfas.2016.01.035. Epub 2016 Apr 15. PMID: 27150233. |
More recent, and higher quality SR's available (Selim 2022) |
|
Ma D, Huang L, Liu B, Liu Z, Xu X, Liu J, Chu T, Pan L. Efficacy of Sinus Tarsal Approach Compared With Conventional L-Shaped Lateral Approach in the Treatment of Calcaneal Fractures: A Meta-Analysis. Front Surg. 2021 Jan 15;7:602053. doi: 10.3389/fsurg.2020.602053. PMID: 33585545; PMCID: PMC7873930. |
Only retrospective studies were included in the analysis. |
|
Majeed H, Barrie J, Munro W, McBride D. Minimally invasive reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular calcaneal fractures: A systematic review of the literature. EFORT Open Rev. 2018 Jul 11;3(7):418-425. doi: 10.1302/2058-5241.3.170043. PMID: 30233817; PMCID: PMC6129959. |
More recent + complete SR available (Lv 2021 / Peng 2021) |
|
Meena S, Gangary SK, Sharma P. Review Article: Operative versus nonoperative treatment for displaced intra-articular calcaneal fracture: a meta-analysis of randomised controlled trials. J Orthop Surg (Hong Kong). 2016 Dec;24(3):411-416. doi: 10.1177/1602400328. PMID: 28031517. |
Duplicate |
|
Meena S, Hooda A, Sharma P, Mittal S, Sharma J, Chowdhury B. Operative versus Non operative treatment of displaced intra-articular fracture of calcaneum: a meta-analysis of randomized controlled trials. Acta Orthop Belg. 2017 Dec;83(1):161-169. PMID: 29322909. |
More recent, and higher quality SR's available (Selim 2022) |
|
Mehta CR, An VVG, Phan K, Sivakumar B, Kanawati AJ, Suthersan M. Extensile lateral versus sinus tarsi approach for displaced, intra-articular calcaneal fractures: a meta-analysis. J Orthop Surg Res. 2018 Sep 24;13(1):243. doi: 10.1186/s13018-018-0943-6. PMID: 30249288; PMCID: PMC6154938. |
More recent + complete SR available (Lv 2021 / Peng 2021) |
|
Nosewicz TL, Dingemans SA, Backes M, Luitse JSK, Goslings JC, Schepers T. A systematic review and meta-analysis of the sinus tarsi and extended lateral approach in the operative treatment of displaced intra-articular calcaneal fractures. Foot Ankle Surg. 2019 Oct;25(5):580-588. doi: 10.1016/j.fas.2018.08.006. Epub 2018 Aug 28. PMID: 30321924. |
More recent + complete SR available (Lv 2021 / Peng 2021) |
|
Seat A, Seat C. Lateral Extensile Approach Versus Minimal Incision Approach for Open Reduction and Internal Fixation of Displaced Intra-articular Calcaneal Fractures: A Meta-analysis. J Foot Ankle Surg. 2020 Mar-Apr;59(2):356-366. doi: 10.1053/j.jfas.2019.08.007. PMID: 32131003. |
More techniques than only Sinus Tarsi approach / RCT en observational studies |
|
Shi F, Wu S, Cai W, Zhao Y. Comparison of 5 Treatment Approaches for Displaced Intra-articular Calcaneal Fractures: A Systematic Review and Bayesian Network Meta-Analysis. J Foot Ankle Surg. 2020 Nov-Dec;59(6):1254-1264. doi: 10.1053/j.jfas.2020.03.021. Epub 2020 Aug 20. PMID: 32828631. |
Only overall effect measures presented, no presentation of data per individual study |
|
Wang Q, Zhang N, Guo W, Wang W, Zhang Q. Cannulated screw fixation versus plate fixation in treating displaced intra-articular calcaneus fractures: a systematic review and meta-analysis. Int Orthop. 2021 Sep;45(9):2411-2421. doi: 10.1007/s00264-021-05141-y. Epub 2021 Aug 9. PMID: 34370059. |
Comparison of two fixation techniques: cannulated screw fixation versus plate fixation |
|
Wei N, Yuwen P, Liu W, Zhu Y, Chang W, Feng C, Chen W. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: A meta-analysis of current evidence base. Medicine (Baltimore). 2017 Dec;96(49):e9027. doi: 10.1097/MD.0000000000009027. PMID: 29245290; PMCID: PMC5728905. |
More recent, and higher quality SR's available (Selim 2022) |
|
Wu MH, Sun WC, Yan FF, Hou ZQ, Feng F, Cai L. [Minimally invasive sinus tarsal approach versus conventional L-shaped lateral approach in treating calcaneal fractures: a Meta-analysis]. Zhongguo Gu Shang. 2017 Dec 25;30(12):1118-1126. Chinese. doi: 10.3969/j.issn.1003-0034.2017.12.009. PMID: 29457434. |
Article in Chinese |
|
Yao H, Liang T, Xu Y, Hou G, Lv L, Zhang J. Sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. J Orthop Surg Res. 2017 Mar 14;12(1):43. doi: 10.1186/s13018-017-0545-8. PMID: 28288661; PMCID: PMC5348794. |
More recent + complete SR available (Lv 2021 / Peng 2021) |
|
Yu T, Xiong Y, Kang A, Zhou H, He W, Zhu H, Yang Y. Comparison of sinus tarsi approach and extensile lateral approach for calcaneal fractures: A systematic review of overlapping meta-analyses. J Orthop Surg (Hong Kong). 2020 Jan-Apr;28(2):2309499020915282. doi: 10.1177/2309499020915282. PMID: 32314645. |
Systematic review of overlapping meta-analyses Five reviews included: Yao 2017, Zhang 2017, Bai 2018, Metha 2018, Nosewitcz 2018. No usefull presentation of the results. |
|
Zeng Z, Yuan L, Zheng S, Sun Y, Huang F. Minimally invasive versus extensile lateral approach for sanders type II and III calcaneal fractures: A meta-analysis of randomized controlled trials. Int J Surg. 2018 Feb;50:146-153. doi: 10.1016/j.ijsu.2017.12.034. Epub 2018 Jan 11. PMID: 29337175. |
More techniques than only sinus tarsi approach |
|
Zhang F, Tian H, Li S, Liu B, Dong T, Zhu Y, Zhang Y. Meta-analysis of two surgical approaches for calcaneal fractures: sinus tarsi versus extensile lateral approach. ANZ J Surg. 2017 Mar;87(3):126-131. doi: 10.1111/ans.13869. Epub 2017 Jan 25. PMID: 28122417. |
More recent + complete SR available (Lv 2021 / Peng 2021) |
|
Zhang W, Lin F, Chen E, Xue D, Pan Z. Operative Versus Nonoperative Treatment of Displaced Intra-Articular Calcaneal Fractures: A Meta-Analysis of Randomized Controlled Trials. J Orthop Trauma. 2016 Mar;30(3):e75-81. doi: 10.1097/BOT.0000000000000446. PMID: 26371619. |
More recent, and higher quality SR's available (Selim 2022) |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 17-10-2024
Beoordeeld op geldigheid : 10-09-2024
Algemene gegevens
De ontwikkeling van deze richtlijn werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in februari 2022 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met traumatisch complexe voetletsels.
Werkgroep
- Dhr. dr. T. (Tim) Schepers (voorzitter werkgroep); traumachirurg, Amsterdam UMC, Nederlandse Vereniging voor Heelkunde (NVvH)
- Dhr. prof. dr. M. (Martijn) Poeze; traumachirurg, Maastricht UMC, Nederlandse Vereniging voor Heelkunde (NVvH)
- Dhr. dr. S.D. (Stijn) Nelen; traumachirurg, Radboud UMC Nijmegen, Nederlandse Vereniging voor Heelkunde (NVvH)
- Dhr. drs. B.E. (Bastiaan) Steunenberg; radioloog, Elisabeth-TweeSteden Ziekenhuis Tilburg, Nederlandse Vereniging voor Radiologie (NVvR)
- Dhr. drs. H.H. (Erik) Dol; SEH-arts, Jeroen Bosch Ziekenhuis, Nederlandse Vereniging van Spoedeisende Hulp Artsen (NVSHA)
- Dhr. drs. M.W. (Menno) Bloembergen; orthopedisch-chirurg, Reinier Haga Orthopedisch Centrum en Hagaziekenhuis, Nederlandse Orthopaedische Vereniging (NOV)
- Dhr. drs. J.P.S. (Joris) Hermus; orthopedisch-chirurg, Maastricht UMC, Nederlandse Orthopaedische Vereniging (NOV)
- Dhr. E. (Erik) Wink; registerpodoloog/podotherapeut/fysiotherapeut, podologic/stichting Reyery, Koninklijk Nederlands Genootschap Fysiotherapie (KNGF) en stichting LOOP (Landelijk Overkoepelend Orgaan Podologie)
- Dhr. drs. P.W.A. (Peter) Muitjens; revalidatiearts, Adelante Zorggroep, Nederlandse Vereniging van Revalidatieartsen (VRA)
Met ondersteuning van
- Mw. dr. A.C.J. (Astrid) Balemans, senior adviseur, Kennisinstituut van Medisch Specialisten.
- Mw. MSc. D.G. (Dian) Ossendrijver, junior adviseur, Kennisinstituut van Medisch Specialisten.
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
Belangentabel richtlijnwerkgroep complexe voetletsels
|
Werkgroeplid |
Functie |
Nevenwerkzaamheden |
Gemelde Persoonlijke Financiële Belangen |
Gemelde Persoonlijke Relaties |
Extern gefinancierd onderzoek |
Gemelde Intell. belangen en reputatie |
Gemelde Overige belangen |
Ondernomen actie |
|
Tim Schepers (voorzitter richtlijn complexe voetletsels) |
Traumachirurg voltijd Amsterdam UMC
|
Voet-enkel expert groep van de Arbeitsgemeinschaft für Osteosynthesefragen (AO)
|
Geen |
Geen |
Ja: wifi2 studie naar wondinfecties bij voet+enkel operaties (verwijderen schroeven/plaat): https://www.amc.nl/web/research-75/trials-collaborations/wifi-2.htm. De studie richt zich op de effectiviteit van antibiotica op het voorkomen van infecties. Rol als projectleider. Gefinancierd roor ZonMW, direct aan Amsterdam Medical Research |
Geschat +/- 200 publicaties over voet- enkelletsel
|
Geen |
Geen restricties; geen van de modules gaat over het onderwerp van de wifi2 studie |
|
Stijn Nelen |
Traumachirurg Radboud UMC Nijmegen |
ATLS-instructeur |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Martijn Poeze |
Traumachirurg Maastricht UMC |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Bastiaan Steunenberg |
Radioloog Isala Zwolle |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Erik Dol |
SEH-arts KNMG |
ATLS-instructeur |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Menno Bloembergen |
Orthopedisch chirurg |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Joris PS Hermus |
Orthopedisch chirurg-traumatoloog |
Voet-enkel expert groep van de Arbeitsgemeinschaft für Osteosynthesefragen (AO)
Council member & honorary secretary European Foot and Ankle Society |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Erik Wink |
Registerpodoloog podotherapeut bij podologic |
Fysiotherapeut bij reyerey, langebaan schaatsploeg |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
|
Peter Muitjens |
Revalidatiearts 0,8 fte, betaald |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen |
Geen restricties |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door het uitnodigen van Patiëntenfederatie Nederland (PFN) voor de schriftelijke knelpuntenanalyse. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voor commentaar voorgelegd aan Patiëntenfederatie Nederland en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijnmodule is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd om te beoordelen of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling is de richtlijnmodule op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Module |
Uitkomst raming |
Toelichting |
|
Module calcaneus fracturen |
Geen financiële gevolgen |
Uit de toetsing volgt dat de aanbeveling(en) niet breed toepasbaar zijn (<5.000 patiënten) en daarom naar verwachting geen substantiële financiële gevolgen zullen hebben voor de collectieve uitgaven. |
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor patiënten met traumatisch complex voetletsel. Tevens zijn er knelpunten aangedragen door middel van een schriftelijke knelpuntenanalyse. Een verslag hiervan is opgenomen onder aanverwante producten.
Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model (Review Manager 5.4) werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
|
Cluster/richtlijn: NVvH Traumatisch complexe voetletsels |
|
|
Uitgangsvraag/modules: UV3 Welke behandeling reduceert de meest voorkomende gevolgen (korte en lange termijn) van Calcaneus fracturen? |
|
|
Database(s): Ovid/Medline, Embase.com |
Datum: 11 januari 2023 |
|
Periode: geen restrictie |
Talen: geen restrictie |
|
Literatuurspecialist: Alies van der Wal |
|
|
BMI-zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting: Voor deze vraag is gezocht op de elementen:
Sleutelartikelen worden gevonden met deze search Sensitief filter gebruikt voor RCTs |
|
Zoekopbrengst
|
|
EMBASE |
OVID/MEDLINE |
Ontdubbeld |
|
SRs |
138 |
101 |
149 |
|
RCT |
411 |
213 |
442 |
|
Observationele studies |
1353 |
1104 |
1676 |
|
Totaal |
549 |
314 |
591* |
*Opgenomen in Rayyan
Zoekstrategie
Embase.com
|
No. |
Query |
Results |
|
#15 |
#4 AND #10 NOT (#11 OR #13) = observationeel |
1353 |
|
#13 |
#4 AND #7 NOT #11 = RCT |
411 |
|
#11 |
#4 AND #5 = SR |
138 |
|
#10 |
#8 OR #9 |
15551918 |
|
#9 |
'case control study'/de OR 'comparative study'/exp OR 'control group'/de OR 'controlled study'/de OR 'controlled clinical trial'/de OR 'crossover procedure'/de OR 'double blind procedure'/de OR 'phase 2 clinical trial'/de OR 'phase 3 clinical trial'/de OR 'phase 4 clinical trial'/de OR 'pretest posttest design'/de OR 'pretest posttest control group design'/de OR 'quasi experimental study'/de OR 'single blind procedure'/de OR 'triple blind procedure'/de OR (((control OR controlled) NEAR/6 trial):ti,ab,kw) OR (((control OR controlled) NEAR/6 (study OR studies)):ti,ab,kw) OR (((control OR controlled) NEAR/1 active):ti,ab,kw) OR 'open label*':ti,ab,kw OR (((double OR two OR three OR multi OR trial) NEAR/1 (arm OR arms)):ti,ab,kw) OR ((allocat* NEAR/10 (arm OR arms)):ti,ab,kw) OR placebo*:ti,ab,kw OR 'sham-control*':ti,ab,kw OR (((single OR double OR triple OR assessor) NEAR/1 (blind* OR masked)):ti,ab,kw) OR nonrandom*:ti,ab,kw OR 'non-random*':ti,ab,kw OR 'quasi-experiment*':ti,ab,kw OR crossover:ti,ab,kw OR 'cross over':ti,ab,kw OR 'parallel group*':ti,ab,kw OR 'factorial trial':ti,ab,kw OR ((phase NEAR/5 (study OR trial)):ti,ab,kw) OR ((case* NEAR/6 (matched OR control*)):ti,ab,kw) OR ((match* NEAR/6 (pair OR pairs OR cohort* OR control* OR group* OR healthy OR age OR sex OR gender OR patient* OR subject* OR participant*)):ti,ab,kw) OR ((propensity NEAR/6 (scor* OR match*)):ti,ab,kw) OR versus:ti OR vs:ti OR compar*:ti OR ((compar* NEAR/1 study):ti,ab,kw) OR (('major clinical study'/de OR 'clinical study'/de OR 'cohort analysis'/de OR 'observational study'/de OR 'cross-sectional study'/de OR 'multicenter study'/de OR 'correlational study'/de OR 'follow up'/de OR cohort*:ti,ab,kw OR 'follow up':ti,ab,kw OR followup:ti,ab,kw OR longitudinal*:ti,ab,kw OR prospective*:ti,ab,kw OR retrospective*:ti,ab,kw OR observational*:ti,ab,kw OR 'cross sectional*':ti,ab,kw OR cross?ectional*:ti,ab,kw OR multicent*:ti,ab,kw OR 'multi-cent*':ti,ab,kw OR consecutive*:ti,ab,kw) AND (group:ti,ab,kw OR groups:ti,ab,kw OR subgroup*:ti,ab,kw OR versus:ti,ab,kw OR vs:ti,ab,kw OR compar*:ti,ab,kw OR 'odds ratio*':ab OR 'relative odds':ab OR 'risk ratio*':ab OR 'relative risk*':ab OR 'rate ratio':ab OR aor:ab OR arr:ab OR rrr:ab OR ((('or' OR 'rr') NEAR/6 ci):ab))) |
13761684 |
|
#8 |
'major clinical study'/de OR 'clinical study'/de OR 'case control study'/de OR 'family study'/de OR 'longitudinal study'/de OR 'retrospective study'/de OR 'prospective study'/de OR 'comparative study'/de OR 'cohort analysis'/de OR ((cohort NEAR/1 (study OR studies)):ab,ti) OR (('case control' NEAR/1 (study OR studies)):ab,ti) OR (('follow up' NEAR/1 (study OR studies)):ab,ti) OR (observational NEAR/1 (study OR studies)) OR ((epidemiologic NEAR/1 (study OR studies)):ab,ti) OR (('cross sectional' NEAR/1 (study OR studies)):ab,ti) |
6767914 |
|
#7 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
3302394 |
|
#5 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
733409 |
|
#4 |
#3 NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) |
3796 |
|
#3 |
#1 AND #2 |
4360 |
|
#2 |
'fracture fixation'/exp OR 'bone implant'/exp OR osteosynthes*:ti,ab,kw OR 'surgery'/exp OR surger*:ti,ab,kw OR surgical*:ti,ab,kw OR operation*:ti,ab,kw OR operative*:ti,ab,kw OR reduction:ti,ab,kw OR orif:ti,ab,kw OR 'mini invasive':ti,ab,kw OR 'minimally invasive':ti,ab,kw OR 'minimal invasive':ti,ab,kw OR mipo:ti,ab,kw OR palmer:ti,ab,kw OR zadravecz:ti,ab,kw OR forgon:ti,ab,kw OR 'sinus tarsi':ti,ab,kw OR 'extended lateral':ti,ab,kw OR 'extensile lateral':ti,ab,kw OR (((screw* OR plate OR plates OR plating OR internal) NEAR/3 (fixat* OR lock* OR percutaneous)):ti,ab,kw) |
8346707 |
|
#1 |
'calcaneus fracture'/exp OR diacf:ti,ab,kw OR iacf:ti,ab,kw OR 'tongue type':ti,ab,kw OR sanders*:ti,ab,kw OR ('calcaneus'/exp AND ('fracture'/exp OR 'dislocation'/exp OR 'bone injury'/exp)) OR (((calcan* OR hindfoot OR 'hind foot' OR heel* OR 'os calcis') NEAR/3 (fractur* OR broken OR dislocat* OR displac*)):ti,ab,kw) |
7297 |
Ovid/Medline
|
# |
Searches |
Results |
|
12 |
(4 and 9) not (10 or 11) = observationeel |
1104 |
|
11 |
(4 and 5) not 10 = RCT |
213 |
|
10 |
4 and 6 = SR |
101 |
|
9 |
7 or 8 |
7090773 |
|
8 |
Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) |
5330423 |
|
7 |
Epidemiologic studies/ or case control studies/ or exp cohort studies/ or Controlled Before-After Studies/ or Case control.tw. or cohort.tw. or Cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or Longitudinal.tw. or Retrospective*.tw. or prospective*.tw. or consecutive*.tw. or Cross sectional.tw. or Cross-sectional studies/ or historically controlled study/ or interrupted time series analysis/ |
4336620 |
|
6 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
641766 |
|
5 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2540677 |
|
4 |
3 not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
2575 |
|
3 |
1 and 2 |
2656 |
|
2 |
exp Fracture Fixation/ or Surgical Procedures, Operative/ or Orthopedic Procedures/ or exp General Surgery/ or exp Orthopedics/ or surger*.ti,ab,kf. or surgical*.ti,ab,kf. or operation*.ti,ab,kf. or operative*.ti,ab,kf. or reduction.ti,ab,kf. or orif.ti,ab,kf. or osteosynthes*.ti,ab,kf. or exp Minimally Invasive Surgical Procedures/ or 'mini invasive'.ti,ab,kf. or 'minimally invasive'.ti,ab,kf. or 'minimal invasive'.ti,ab,kf. or MIPO.ti,ab,kf. or palmer.ti,ab,kf. or zadravecz.ti,ab,kf. or forgon.ti,ab,kf. or 'sinus tarsi'.ti,ab,kf. or 'extended lateral'.ti,ab,kf. or 'extensile lateral'.ti,ab,kf. or ((screw* or plate or plates or plating or internal) adj3 (fixat* or lock* or percutaneous)).ti,ab,kf. |
4217287 |
|
1 |
(diacf or iacf or 'tongue type' or sanders*).ti,ab,kf. or (exp Calcaneus/ and (exp Fractures, Bone/ or exp Fracture Dislocation/)) or ((calcan* or hindfoot or 'hind foot' or heel* or 'os calcis') adj3 (fractur* or broken or dislocat* or displac*)).ti,ab,kf. |
4934 |
