Dexmedetomidine
Uitgangsvraag
Wat is de plaats van dexmedetomidine bij sedatie van volwassen patiënten buiten de OK?
Aanbeveling
Gebruik dexmedetomidine alleen voor PSA wanneer dit evidente voordelen biedt voor individuele patiënten.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
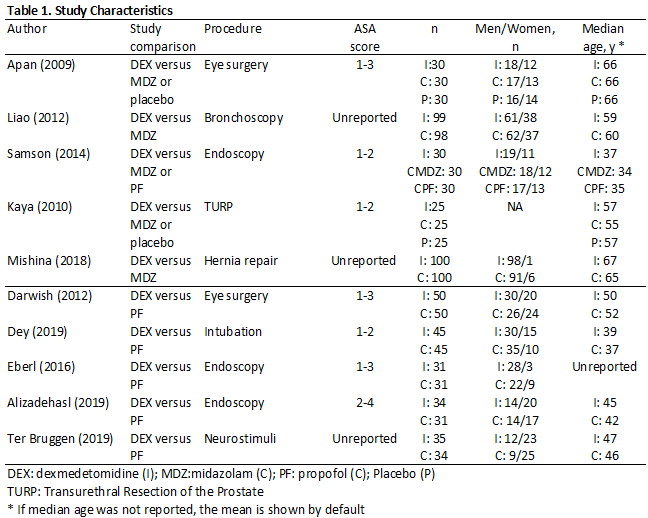
Er is literatuuronderzoek uitgevoerd om te kijken of dexmedetomidine voordelen heeft ten opzichte van propofol of midazolam bij volwassenen die PSA ondergaan. Er zijn 11 RCT’s gevonden met elk meer dan 60 deelnemers die voldeden aan de PICO. De bewijskracht viel uiteindelijk voor alle uitkomstmaten uit als laag tot zeer laag. De verklaring hiervoor is dat de trials geen eenduidige definities van gebruikte doses van sedativa bevatten, dat er verschillende definities van uitkomstmaten waren, die bovendien op verschillende tijdstippen zijn gemeten. Daarnaast was de mate van potentiële bias in de studies in min of meerdere mate aanwezig in alle studies (als blijkt uit de risk of bias assessment). Generaliseerbaarheid van de resultaten is in de GRADE waardering van bovengenoemd bewijs niet meegenomen. Er dient echter opgemerkt te worden dat de ASA-klasse in het merendeel van de trials ASA I-II was en dat ouderen in het merendeel van de trials geëxcludeerd werden.
In het merendeel van de trials werd geen verschil gezien in patiënt-tevredenheid, maar er was inconsistentie binnen de bevindingen. Eenzelfde beeld werd gezien voor operateur/anesthesioloog tevredenheid. De mate van sedatie leek er iets beter uit te komen voor de dexmedetomidine groep, versus de midazolam groep en was om en nabij hetzelfde wanneer dexmedetomidine werd vergeleken met propofol. Wederom is hier sprake van inconsistentie en imprecisie omdat de resultaten niet gepoold konden worden. Voor de uitkomst verkoevertijd was er wel inconsistentie tussen de resultaten, maar viel alle inconsistentie binnen de vooraf gestelde grens van klinische relevantie. De GRADE waardering viel hierom als laag uit voor zowel de vergelijking tussen dexmedetomidine en midazolam als voor dexmedetomidine en propofol. Voor de uitkomstmaat hypoxemie lijken de trial uitkomsten in het voordeel te zijn voor de dexmedetomidine groep en het effect is bovendien consistent. Voor hypotensie wordt een zeer inconsistent beeld gezien in de uitkomstmaat, waardoor er geen enkele uitspraak kan worden gegeven in hoeverre dexmedetomidine al dan niet meer hypotensie geeft dan midazolam of propofol bij PSA.
Kortom, ten gevolge van de matige/lage kwaliteit van het merendeel van de gevonden trials, is er geen harde uitspraak te geven over welk sedativum de voorkeur moet krijgen binnen het indicatiegebied PSA.
Ofschoon hierdoor sprake is van een kennislacune, dient opgemerkt te worden dat de patiënt-tevredenheid voor alle sedativa hoog was en dat ernstige bijwerkingen anders dan de hier genoemden niet/nauwelijks voorkwamen.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Voor de patiënt is het belangrijkste doel van het geven van PSA het verhogen van het comfort tijdens een pijnlijke of oncomfortabele procedure. Dit kan worden bereikt door sedatie, analgesie en amnesie of een combinatie hiervan. Daarnaast is het voor patiënten van belang dat de na-effecten van de PSA zo kort mogelijk duren. Een korte verkoevertijd en een gebrek aan hang-over-effect en misselijkheid of braken zijn waardevolle eigenschappen voor middelen die bij PSA gebruikt worden. Op het gebied van patiënttevredenheid kan de werkgroep in de huidige literatuur geen onderscheid maken tussen het gebruik van propofol of midazolam enerzijds en dexmedetomidine anderzijds.
Kosten (middelenbeslag)
De kosten van het gebruik van dexmedetomidine liggen hoger dan die van het gebruik van propofol of midazolam. Het gebrek aan gunstige effecten lijkt niet op te wegen tegen de hogere te maken kosten.
Aanvaardbaarheid, haalbaarheid en implementatie
Alle onderzochte middelen zijn probleemloos in Nederland verkrijgbaar voor het gebruik bij PSA. Voor alle middelen bestaat Europese goedkeuring voor het gebruik ervan voor PSA. Dexmedetomidine kan echter niet worden toegediend als intermitterende bolusinjectie zoals propofol en midazolam. Continue infusie van dexmedetomidine is complexer dan de infusie van propofol en midazolam omdat de initiële bolus van dexmedetomidine bij voorkeur over een periode van 10 minuten plaatsvindt.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
Het gebruik van dexmedetomidine in vergelijkingen met propofol of midazolam voor PSA is onderwerp geweest van veel gepubliceerde studies. De mate waarin deze studies uitsluitsel kunnen geven over relevante vragen over eventuele voordelen is echter zeer beperkt. De studies zijn doorgaans klein, van matige of slechte kwaliteit of kennen interferentie met andere middelen tijdens PSA. In de onderzochte studies komt dit effect echter in een veel kleinere orde van grote naar voren dan verwacht zou mogen worden op basis van de theorie. Voor de overige uitkomstmaten heeft de werkgroep geen evidente verschillen kunnen vinden in de beschikbare literatuur.
Daarnaast is dexmedetomidine een middel met een traag farmacologisch profiel (langere inwerktijd, langere afbouw). In het algemeen wordt bij PSA de voorkeur gegeven aan middelen met een snel farmacologisch profiel omdat dit titratie ten goede komt. Dat dit verschil in farmacologie in de studies niet ook leidde tot een andere uitkomst van de vergelijking kan wellicht worden verklaard door het gebruik van strikte protocollen voor de toediening. Of de toediening van dexmedetomidine in de klinische praktijk, buiten studieverband ook tot even grote tevredenheid zou kunnen leiden is daarmee zeer de vraag.
Het is denkbaar dat voor individuele patiënten of in geselecteerde omstandigheden er voordelen zijn voor het gebruik van dexmedetomidine. Het beperkte gevonden verschil in veiligheidsprofiel laat echter niet toe om dexmedetomidine te zien als een sedativum dat met beperkter bewakingsfaciliteiten kan worden gebruikt.
Dexmedetomidine is momenteel duurder in gebruik dan propofol en midazolam. Deze hogere kosten mogen ook een rol spelen in de keuze voor het middel bij PSA. De werkgroep verwijst voor het gebruik van dexmedetomidine voor PSA bij kinderen of voor sedatie op de intensive care naar de betreffende subrichtlijnen.
Onderbouwing
Achtergrond
Het indicatiegebied voor het gebruik van dexmedetomidine is recent door de EMA uitgebreid. Dexmedetomidine (toegediend via verschillende routes zoals intraveneus of nasaal) kan ook gebruikt worden voor procedurele sedatie en/of analgesie. Hoewel dexmedetomidine veelvuldig is onderzocht binnen dit indicatiegebied, is er geen consensus over eventuele voordelen ten opzichte van sedativa als midazolam en propofol. Het gebruik van dexmedetomidine bij PSA lijkt vooralsnog vooral gebaseerd op persoonlijke voorkeur en niet op een duidelijke onderbouwing in de literatuur.
Conclusies / Summary of Findings
Patient’s satisfaction
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on patient’s satisfaction when compared with midazolam in adult patients undergoing procedural sedation
Kaya (2010), Liao (2012), Samson (2014) |
Provider satisfaction
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on provider satisfaction when compared with midazolam in adult patients undergoing procedural sedation.
Kaya (2010), Liao (2012), Samson (2014) |
Sedation level
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on sedation level when compared with midazolam in adult patients undergoing procedural sedation. Dexmedetomidine may have little beneficial effect on sedation, but the evidence is very uncertain
Kaya (2010), Mishina (2018), Samson (2014) |
Recovery time
|
Low GRADE |
Dexmedetomidine may result in little to no difference in recovery time when compared with midazolam in adult patients undergoing procedural sedation
Apan (2009), Kaya (2010), Samson (2014) |
Hypoxemia
|
Low GRADE |
Dexmedetomidine may reduce hypoxemia slightly compared with midazolam in adult patients undergoing procedural sedation.
Kaya (2010), Liao (2012), Mishina (2018) |
Hypotension
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on hypotension when compared with midazolam in adult patients undergoing procedural sedation.
Kaya (2010), Liao (2012), Mishina (2018), Samson (2014) |
Conclusions For dexmedetomidine versus propofol
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on patient’s satisfaction when compared with propofol in adult patients undergoing procedural sedation
Sources: Alizadehasl (2019), Darwish (2012), Dey (2009), Eberl (2016), Ter Bruggen (2019) |
Provider satisfaction
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on provider satisfaction when compared with propofol in adult patients undergoing procedural sedation.
Sources: Alizadehasl (2019), Eberl (2016), Samson (2014), Ter Bruggen (2019) |
Sedation level
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on sedation level when compared with propofol in adult patients undergoing procedural sedation.
Sources: Alizadehasl (2019), Samson (2014), Ter Bruggen (2019) |
Recovery time
|
Low GRADE |
Dexmedetomidine may result in little to no difference in recovery time when compared with propofol in adult patients undergoing procedural sedation
Sources: Alizadehasl (2019), Darwish (2012), Eberl (2016), Samson (2014) |
Hypoxemia
|
Low GRADE |
Dexmedetomidine may reduce hypoxemia slightly compared with propofol in adult patients undergoing procedural sedation
Sources: Alizadehasl (2019), Dey (2009), Ter Bruggen (2019) |
Hypotension
|
Very Low GRADE |
The evidence is very uncertain about the effect of dexmedetomidine on hypotension when compared with propofol in adult patients undergoing procedural sedation
Sources: Alizadehasl (2019), Samson (2014), Ter Bruggen (2019) |
Samenvatting literatuur
Results
Two systematic reviews were included. The systematic review of Barends (2017) reviewed three clinical trials that randomized >60 participants and that compared dexmedetomidine with midazolam in adult patients up to June 20, 2016. Randomized trials of more than 60 participants that were published after this date and that compared dexmedetomidine with midazolam in adult patients were added. This led to one other trial that was included in the analysis of the literature.
The systematic review of Ter Bruggen (2017) reviewed one clinical trial that randomized >60 participants and that compared dexmedetomidine with propofol in adult patients up to March 2014. Additionally, there were four randomized clinical trials of more than 60 participants that were published after this date and that compared dexmedetomidine with propofol in adult patients. These trials were also added to this search of the PICO. One trial (Samson, 2014) compared dexmedetomidine with midazolam and dexmedetomidine with propofol. This trial is included in both the trial comparison of dexmedetomidine with midazolam and in the trial comparison of dexmedetomidine with propofol. Therefore, in total 10 trials are included in the analysis of the literature. Important study characteristics and results are summarized in table 1 and in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
The study characteristics are summarized in Table 1 and are fully shown in the Evidence table.
The included studies varied widely with respect to dosing regimens, procedures, and outcome measures. Also, not all studies reported in enough detail on these outcome measures. For this reason, a meta-analysis could not be performed.
Patient satisfaction
Eight studies reported results regarding patient satisfaction; including three studies for the comparison of dexmedetomidine versus midazolam (Kaya, 2010; Liao, 2012; Samson, 2014) and five studies for the comparison of dexmedetomidine versus propofol (Alizadehasl, 2019; Darwish, 2012; Dey, 2009; Eberl, 2016; Ter Bruggen, 2019). Definitions are provided in the evidence table.
Results:
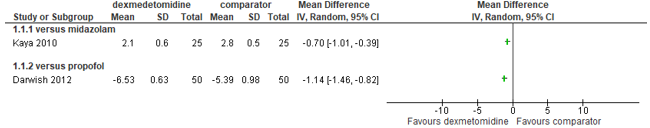
Dexmedetomidine versus midazolam
Kaya (2010) showed that for patient satisfaction, defined by postoperative pain assessed by the patient using a visual analogue scale (0 highest satisfaction, 10 lowest satisfaction) a mean difference of -0.7 (95% CI -1.01 to -0.39) points favoring dexmedetomidine over midazolam.
Liao (2012) showed that patient satisfaction, defined with a numerical rating scale (zero being most satisfied and 10 least satisfied) was similar in the dexmedetomidine group (median 0, IQR 0-0) as in the midazolam group (median 0, IQR 0-0)
Samson (2014) showed that patient satisfaction, defined with a categorical scale from 1-10, where category 1 was highest satisfaction, was higher in the midazolam group than in the dexmedetomidine group (RR 0.43; 95% CI, 0.27-0.67). This difference is clinically relevant
Dexmedetomidine versus propofol
Alizadehasl (2019) defined patient satisfaction from bad (grade 0) to perfect (grade 4). The perfect score was similar in the dexmedetomidine vs propofol group; RR 0.88 (95% CI, 0.70-1.11).
Darwish (2012) showed for patient satisfaction defined with a 7-point like verbal rating scale (0 lowest satisfaction, 7, highest satisfaction), a mean difference of -0.7 (95% CI -1.01 to -0.39) points favoring dexmedetomidine over propofol.
Dey (2009) defined patient satisfaction as endoscope intubation comfort score in which no discomfort was shown at time of intubation of the endoscope. The results were similar in the dexmedetomidine vs propofol group; RR 1.20 (95% CI, 0.78-1.84).
Eberl (2016) showed that for patient satisfaction, defined with how satisfied the patient was with the procedure (ranging from 1=very dissatisfied to 7=highly satisfied), the median level was 5.0 (IQR 4.4-5.8) in the dexmedetomidine group and 6.0 (IQR 5.4-6.0) in the propofol group (P<0.001 in advantage for propofol). This difference is clinically relevant.
Ter Bruggen defined patient satisfaction with the Patient Satisfaction with Sedation Index (PSSI) (with higher scores indicating higher patient satisfaction). The median outcome (IQR) was similar in the dexmedetomidine group (median 94.4; IQR 100-88.9]) as in the propofol group (median 88.9; IQR 100.0‐83.3); P=0.17
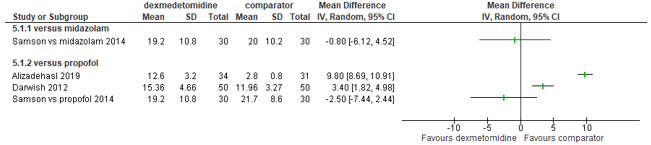
Continuous results with mean and SD are also shown in Figure 1A, and categorical outcomes are also shown in Figure 1B. Continuous results shown with a median are also shown in the Evidence Table.
Figure 1A. Forest plot of dexmedetomidine vs midazolam/propofol, outcome patient satisfaction (continuous outcome)
Figure 1B. Forest plot of dexmedetomidine vs midazolam/propofol, outcome patient satisfaction (categorical outcome)
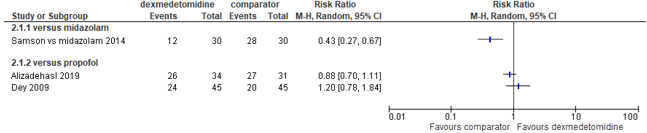
Provider satisfaction
Six studies reported results regarding provider satisfaction; including 3 studies for the comparison of dexmedetomidine versus midazolam (Kaya, 2010; Liao, 2012; Samson, 2014) and 4 studies for the comparison of dexmedetomidine versus propofol (Alizadehasl, 2019; Eberl, 2016; Samson, 2014; Ter Bruggen, 2019).
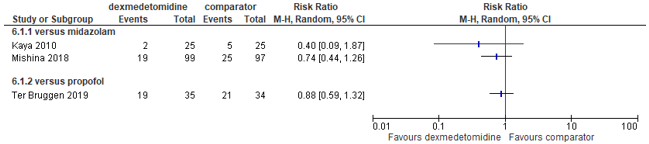
Dexmedetomidine versus midazolam
Kaya (2010) showed that for provider satisfaction, defined by a categorical scale from 1-3, where category 3 was highest satisfaction, results were similar for dexmedetomidine (median level 3, IQR 2-3) versus midazolam (median 3, IQR 2-3).
Liao (2012) showed that for provider satisfaction, defined with a categorical rating scale (zero being most satisfied and 10 least satisfied), results were similar for dexmedetomidine (median 3, IQR 2-5) as for midazolam (median 4, IQR 2-5).
Samson (2014) showed that patient satisfaction, defined with a categorical scale from 1-10, where category 1 was highest satisfaction, was higher in the dexmedetomidine group than in the midazolam group (RR 4.50; 95% 1.73-11.73). This difference is clinically relevant, but the result is imprecise as shown by the large confidence interval.
Dexmedetomidine versus propofol
Alizadehasl (2019) defined provider satisfaction from bad (grade 0) to perfect (grade 4) in view of the anesthesiologist. The perfect score was similar in the dexmedetomidine vs propofol group; RR 1.05 (95% CI, 0.86-1.28).
Eberl (2016) showed for provider satisfaction, defined with how satisfied the endoscopist was with the procedure (ranging from 1=very dissatisfied to 7=highly satisfied), that the median level was 5.0 (IQR 4.4-5.8) in the dexmedetomidine group and 6.25 (IQR 5.3-6.5) in the propofol group (P<0.001 in advantage for propofol). This difference is clinically relevant.
Samson (2014) showed that patient satisfaction, defined with a categorical scale from 1-10, where category 1 was highest satisfaction, was similar in the dexmedetomidine group versus the propofol group (RR 1.06; 95% 0.69-1.62).
Ter Bruggen defined provider satisfaction as operator's comfort throughout the procedure, measured as the response to the question "What score would you give to the comfort during the procedure?" — from 1 (bad) till 4 (excellent). Results were similar in the dexmedetomidine group (median 3.00, IQR 1.0) versus the propofol group (median 3.00, IQR 0.63).
Categorical outcomes are also shown in Figure 2. Continuous results shown with a median are also shown in the Evidence Table.
Figure 2. Forest plot of dexmedetomidine vs midazolam/propofol, outcome provider satisfaction (categorical outcome)
Procedure success rate
Sedation level
Six studies reported results regarding provider satisfaction; including 3 studies for the comparison of dexmedetomidine versus midazolam (Kaya, 2010; Samson, 2014; Mishina, 2018) and 3 studies for the comparison of dexmedetomidine versus propofol (Alizadehasl, 2019; Darwish, 2012; Samson, 2014; Ter Bruggen, 2019)
Dexmedetomidine versus midazolam
Kaya (2010) showed that for sedation level, defined with the Ramsay sedation score and where excessive sedation was reported as a level greater than 5/6, excessive sedation was more present in the midazolam group than in the dexmedetomidine group. This result is clinically relevant, but numbers are small and the confidence interval is wide (RR 0.40; 95% CI, 0.09-1.87).
Samson (2014) showed that sedation level, defined as dose of fentanyl used for breakthrough sedation (in mcg), was similar in the dexmedetomidine and midazolam group (mean difference -0.80; 95% CI, -6.12 to 4.52).
Mishina (2018) defined sedation level as number of patients who were in a state of conscious sedation (OAA/S Scale: 3–4) during the procedure, and found a relative risk of 0.74 (95% CI, 0.44-1.26) in favor of the dexmedetomidine group. This result is clinically relevant, but numbers were small and the confidence interval is wide.
Dexmedetomidine versus propofol
Alizadehasl (2019) defined sedation level as time from start sedation to TEE in minutes. The result showed a mean difference of 9.80 minutes (95% CI, 8.69-10.91) favoring propofol.
Darwish (2012) defined sedation level with the Richmond Agitation-Sedation Scale and bispectral index. The sedation level was provided as mean, minutes (SD), but was further undefined. Results showed a mean difference of 3.40 minutes (95% CI, 1.82-4.98) favoring propofol.
Samson (2014) showed that sedation level, defined as dose of fentanyl used for breakthrough sedation (in mcg), was similar in the dexmedetomidine and propofol group (mean difference –2.55; 95% CI, -7.44 to 2.44).
Ter Bruggen defined sedation level as total number of participants who received 1 or more rescue boluses of remifentanil 25 μg, which was similar in the dexmedetomidine vs propofol group (RR 0.88; 95% CI 0.59-1.32).
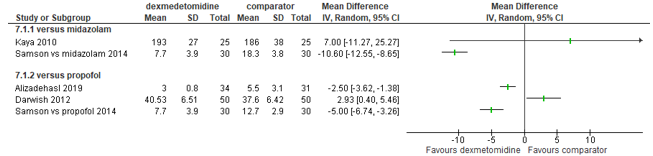
Continuous results with mean and SD are also shown in Figure 3a and results with a categorical outcome are shown in Figure 3 b. Continuous results shown with a median or mean (without SD) are also shown in the Evidence Table.
Figure 3a. Forest plot of dexmedetomidine vs midazolam/propofol, outcome sedation level (continuous outcome)
Figure 3a. Forest plot of dexmedetomidine vs midazolam/propofol, outcome sedation level (categorical outcome)
Recovery time
Six studies reported results regarding recovery time; including three studies for the comparison of dexmedetomidine versus midazolam (Apan, 2009; Kaya, 2010; Samson, 2014) and four studies for the comparison of dexmedetomidine versus propofol (Alizadehasl, 2019; Darwish, 2012; Eberl, 2016; Samson, 2014;)
Dexmedetomidine versus midazolam
Apan (2009) defined recovery time according to a 4-point rating scale in the recovery unit (1=patient
fully awake; 2=patient somnolent, but responds to verbal commands; 3=patient somnolent, but
responds to tactile stimuli; 4=patient asleep, but responds to pain), reported from 1-4 hours after operation, median. Results (shown as median) for dexmedetomidine were 2,1,1,1 and for midazolam 2,1,1,1 (no difference).
Kaya (2010) defined recovery time with the Modified Bromage Scale10 (0 = no paralysis; 1 = unable to raise
extended leg; 2 = unable to flex knee; 3 = unable to flex ankle). Motor block duration was the time (in minutes) for return to Modified Bromage Scale 1 which was better for the midazolam group (mean difference 7 minutes; 95% CI, -11.27 to 25.27) but numbers are small, and the confidence interval is large.
Samson (2014) assessed recovery time, by using the modified Aldrete score at 5 min after
removal of the endoscope and every 5 min thereafter until a discharge score of 10/10 was reached. The mean difference was -10.60 minutes (95% CI, -12.55 to -8.65) favoring dexmedetomidine.
Dexmedetomidine versus propofol
Alizadehasl (2019) reported recovery time as ‘full recovery from sedation’ in minutes and showed a mean difference of -2.50 minutes (95% CI, -3.62 to -1.38) favoring dexmedetomidine.
Eberl, reported recovery time as median Aldrete score 30-60 minutes after the end of sedation. Results are shown with a significance test i.e, ‘significantly lower in group dexmedetomidine’.
Samson (2014) assessed recovery time, by using the modified Aldrete score at 5 min after
removal of the endoscope and every 5 min thereafter until a discharge score of 10/10 was reached. The mean difference was -5.00 minutes (95% CI, -6.74 to -3.26)) favoring dexmedetomidine.
Continuous results with mean and SD are also shown in Figure 4. Continuous results shown with a median or mean (without SD) are also shown in the Evidence Table.
Figure 4. Forest plot of dexmedetomidine vs midazolam/propofol, outcome recovery time
Adverse events
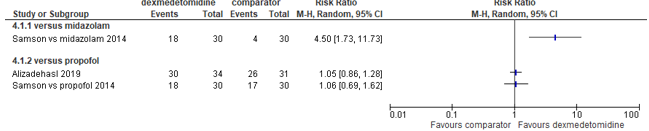
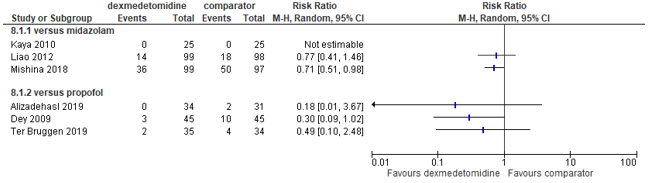
Hypoxemia
Seven studies reported results regarding hypoxemia; including three studies for the comparison of dexmedetomidine versus midazolam (Kaya, 2010; Liao, 2012; Mishina, 2018) and three studies for the comparison of dexmedetomidine versus propofol (Alizadehasl, 2019; Dey, 2009; Ter Bruggen, 2019).
Alizadehasl (2019), Dey (2009) and Ter Bruggen (2019) defined hypoxia as SpO2<90% during the procedure.
Kaya (2010) defined hypoxia as Et-CO2 >50 mmHg or RR<12 breaths/min.
Liao (2012) defined hypoxia as SpO2<90% for > 30 s during the procedure-discharge.
Mishina (2021) defined hypoxia as respiratory rate < 8 bpm, 25% decrease from before administration, SpO2
< 90%, decrease by 10% from before administration or oxygen administration.
The RRs from studies comparing dexmedetomidine to midazolam were 0.77 (95% CI 0.41 to 1.46) and 0.71 (95% CI 0.51 to 0.98) respectively, indicating a clinically relevant difference in favour of dexmedetomidine.
The RRs from studies comparing dexmedetomidine to propofol were 0.18 (95% CI 0.01 to 3.67), 0.30 (95% CI 0.09 to 1.02) and 0.49 (95% CI 0.10 to 2.48) respectively, indicating a clinically relevant difference in favour of dexmedetomidine. See Figure 5 for visualization of these results.
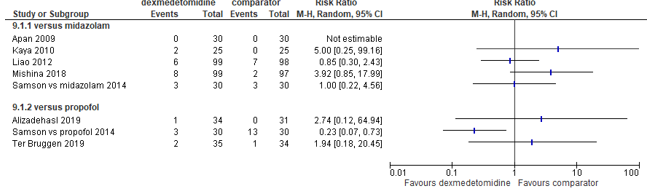
Figure 5. Forest plot of dexmedetomidine vs midazolam/propofol, outcome hypoxemia
Hypotension
Seven studies reported results regarding hypotension; including four studies for the comparison of dexmedetomidine versus midazolam (Kaya, 2010; Liao 2012; Samson 2014; Mishina, 2018) and four studies for the comparison of dexmedetomidine versus propofol (Alizadehasl, 2019; Apan, 2009; Samson, 2014; Ter Bruggen, 2019).
Alizadehasl (2019) defined hypotension as systolic arterial pressure < 90 mmHg. Apan (2009), Samson (2014), reported hypotension as a categorical (yes/no) outcome without a further definition. Kaya (2010) defined hypotension as a decrease in mean arterial pressure (MAP) below 20% of baseline or systolic pressure <90 mmHg. Liao (2012) defined hypotension as systolic arterial pressure < 90 mmHg or mean arterial pressure < 60 mmHg during the procedure. Mishina (2018) defined hypotension as systolic blood pressure < 80 mmHg, decrease by 30% from before administration or diastolic blood pressure < 50 mmHg. Ter Bruggen (2019) defined hypotension as mean arterial pressure < 60 mmHg during the procedure.
The results from studies comparing dexmedetomidine to midazolam were inconsistent. Two studies showed no clinically relevant difference (Liao, 2012: RR 0.85, 95% CI 0.30 to 2.43; Samson, 2014: RR 1.00, 95% CI 0.22 to 4.56). Two other studies showed a clinically relevant difference in favour of midazolam (Kaya, 2010: RR 5.00, 95% CI 0.25 to 99.16; Mishina, 2018: RR 3.92, 95% CI 0.85 to 17.99).
The RRs from studies comparing dexmedetomidine to propofol were also inconsistent. One study indicated
a clinically relevant difference in favour of dexmedetomidine (Samson, 2014: RR 0.23, 95% CI 0.07 to 0.73). Two studies indicated a clinically relevant difference in favour of propofol (Alizadehasl, 2019: RR 2.74, 95% CI 0.12 to 64.94; Ter Bruggen, 2019: RR 1.94, 95% CI 0.18 to 20.45). See Figure 6 for visualization of these results.
Figure 6. Forest plot of dexmedetomidine vs midazolam/propofol, outcome hypotension
Level of evidence of the literature
The level of evidence (GRADE method) is determined per comparison and outcome measure and is based on results from systematic review of randomized trials and therefore starts at level “high”. Subsequently, the level of evidence was downgraded if there were relevant shortcomings in one of the several GRADE domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias.
For dexmedetomidine versus midazolam
The level of evidence regarding the outcome measure patient’s satisfaction was downgraded by 3 levels because of risk of bias (-1 level because of study limitations), inconsistency (-1 level, conflicting results) and imprecision (-1 level low number of included patients).
The level of evidence regarding the outcome measure provider satisfaction was downgraded by 3 levels because of risk of bias (-1 level because of study limitations)inconsistency (-1 level, conflicting results) and imprecision (-1 level low number of included patients).
The level of evidence regarding the outcome measure sedation level was downgraded by 3 levels because of risk of bias (-1 levels because of study limitations), inconsistency (-1 level, conflicting results) and imprecision (-1 level low number of included patients).
The level of evidence regarding the outcome measure recovery time was downgraded by 2 levels because of risk of bias (-1 levels because of study limitations) and inconsistency (-1 level conflicting results.)
The level of evidence regarding the outcome measure hypoxemia was downgraded by 2 levels because of risk of bias (-1 level because of study limitations) and imprecision (-1 level small number of events).
The level of evidence regarding the outcome measure hypotension was downgraded by 3 levels because of risk of bias (-1 level because of study limitations), inconsistency (1 level, conflicting results) and imprecision (-1 level small number of events).
For dexmedetomidine versus propofol
The level of evidence regarding the outcome measure patient’s satisfaction was downgraded by 3 levels because of risk of bias (-1 level because of study limitations) , imprecision (-1 level low number of included patients), inconsistency (-1 level, conflicting results).
The level of evidence regarding the outcome measure provider satisfaction was downgraded by 3 levels because of risk of bias (-1 level because of study limitations), inconsistency (-1 level, conflicting results) and imprecision (-1 level low number of included patients).
The level of evidence regarding the outcome measure sedation level was downgraded by 3 levels because of risk of bias (-1 levels because of study limitations), inconsistency (-1 level, conflicting results) and imprecision (-1 level low number of included patients).
The level of evidence regarding the outcome measure recovery time was downgraded by 2 levels because of risk of bias (-1 levels because of study limitations) and inconsistency (-1 level conflicting results).
The level of evidence regarding the outcome measure hypoxemia was downgraded by 2 levels because of risk of bias (-1 level because of study limitations) and imprecision (-1 level small number of events).
The level of evidence regarding the outcome measure hypotension was downgraded by 1 level because of risk of bias (-1 level because of study limitations), inconsistency (1 level, conflicting results) and imprecision (-1 level small number of events).
Zoeken en selecteren
A systematic review of the literature was performed to answer the following 2 questions:
A) What is the effect of dexmedetomidine compared to midazolam on patient satisfaction, operator satisfaction and complications in adult patients undergoing procedural sedation?
P (Patients) = adult patients undergoing procedural sedation
I (Intervention) = dexmedetomidine
C (Comparison) = midazolam
O (Outcomes) = patient satisfaction, provider satisfaction, procedure success rate (sedation level,
recovery time), adverse events (hypoxemia, hypotension)
B) What is the effect of dexmedetomidine compared to propofol on patient satisfaction, operator satisfaction and complications in adult patients undergoing procedural sedation?
P (Patients) = adult patients undergoing procedural sedation
I (Intervention) = dexmedetomidine
C (Comparison) = propofol
O (Outcomes) = patient satisfaction, provider satisfaction, procedure success rate (sedation level, recovery time), adverse events (hypoxemia, hypotension)
Relevant outcome measures
The guideline development group considered patient satisfaction, provider satisfaction, procedure success rate (sedation level, recovery time), and adverse events (hypoxemia, hypotension) as outcomes for decision making. A-priori, no distinction was made between critical outcome measures and important outcome measures for decision making. A priori, the working group did not define the outcome measures listed above but used the definitions used in the studies.
The working group defined a limit of 25% difference for dichotomous outcomes (RR <0.8 or >1.25) and 10% for continuous outcomes as a minimal clinically (patient) important difference. For recovery time, a difference of 15 minutes was considered as clinically relevant.
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms until 3 June 2021. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 732 hits, including 99 systematic reviews and 633 randomized controlled trials (RCTs), which included all elements of the PICO:
- adult patients undergoing procedural sedation
- dexmedetomidine
- propofol or midazolam
- Investigated at least one of the outcomes as reported in the PICO
Studies in which dexmedetomidine, midazolam or propofol was given as part of intensive or critical care and any studies including children were excluded. Also excluded were studies where additional medication with sedative properties was given other than as rescue medication. The exclusion of these studies allowed for a more precise comparison of the effects of the sedative drugs that are defined in the PICO without accounting for numerous (unpredictable) pharmacological interactions. Only trials in which more than 60 participants were randomized were included. This decision led to exclusion of additionally 24 studies (see the table with reason for exclusion under the tab Methods).
A total of 29 articles were initially selected based on title and abstract screening. After reading the full text, 12 studies were excluded (see the table with reason for exclusion under the tab Methods), and 17 studies (including 2 systematic reviews) were included.
Referenties
- Alizadehasl A, Sadeghpour A, Totonchi Z, Azarfarin R, Rahimi S, Hendiani A. Comparison of sedation between dexmedetomidine and propofol during transesophageal echocardiography: A randomized controlled trial. Ann Card Anaesth. 2019 Jul-Sep;22(3):285-290. Doi: 10.4103/aca.ACA_42_18. PMID: 31274491; PMCID: PMC6639890.
- Apan A, Doganci N, Ergan A, Büyükkoçak U. Bispectral index-guided intraoperative sedation with dexmedetomidine and midazolam infusion in outpatient cataract surgery. Minerva Anestesiol. 2009 May;75(5):239-44. Epub 2008 Dec 17. PMID: 19088698.
- Barends CR, Absalom A, van Minnen B, Vissink A, Visser A. Dexmedetomidine versus Midazolam in Procedural Sedation. A Systematic Review of Efficacy and Safety. PloS One. 2017 Jan 20;12(1):e0169525. Doi: 10.1371/journal.pone.0169525. PMID: 28107373; PMCID: PMC5249234.
- Darwish A, Sami R, Raafat M, Aref R, Hisham M. Dexmedetomidine versus propofol for monitored anesthesia care in patients undergoing anterior segment ophthalmic surgery under peribulbar medial canthus anesthesia. Life Sci J. 2012;9:789-793.
- Dey S, Borah TJ, Sonowal J, Pradhan D, Yunus M, Dev P. Comparison of safety and efficacy of dexmedetomidine versus propofol sedation for elective awake fiber-optic intubation. J Pharmacol Pharmacother 2019;10:11-5
- Ioannidis JP. Why most published research findings are false. PloS Med. 2005 Aug;2(8):e124. Doi: 10.1371/journal.pmed.0020124. Epub 2005 Aug 30. PMID: 16060722; PMCID: PMC1182327.
- Kumari R, Jain K, Agarwal R, Dhooria S, Sehgal IS, Aggarwal AN. Fixed dexmedetomidine infusion versus fixed-dose midazolam bolus as primary sedative for maintaining intra-procedural sedation during endobronchial ultrasound-guided transbronchial needle aspiration: a double blind randomized controlled trial. Expert Rev Respir Med. 2021 Apr 25:1-7. Doi: 10.1080/17476348.2021.1918000. Epub ahead of print. PMID: 33849367.
- Liao W, Ma G, Su QG, Fang Y, Gu BC, Zou XM. Dexmedetomidine versus midazolam for conscious sedation in postoperative patients undergoing flexible bronchoscopy: a randomized study. J Int Med Res. 2012;40: 1371-1380. Pmid:22971488
- Mishina T, Aiba T, Hiramatsu K, Shibata Y, Yoshihara M, Aoba T, Yamaguchi N, Kato T. Comparison between dexmedetomidine and midazolam as a sedation agent with local anesthesia in inguinal hernia repair: randomized controlled trial. Hernia. 2018 Jun;22(3):471-478. Doi: 10.1007/s10029-017-1680-1. Epub 2017 Sep 30. PMID: 28965137.
- Samson S, George S, Vinoth B, et al. Comparison of dexmedtomidine, midazolam, and propofol as an optimal sedative for upper gastrointestinal endoscopy: A randomized controlled trial. J Dig Endosc 2014; 5: 51-57.
- Ter Bruggen FFJA, Eralp I, Jansen CK, Stronks DL, Huygen FJPM. Efficacy of Dexmedetomidine as a Sole Sedative Agent in Small Diagnostic and Therapeutic Procedures: A Systematic Review. Pain Pract. 2017 Jul;17(6):829-840. Doi: 10.1111/papr.12519. Epub 2016 Dec 30. PMID: 27862903.
- Ter Bruggen FFJA, Ceuppens C, Leliveld L, Stronks DL, Huygen FJPM. Dexmedetomidine vs propofol as sedation for implantation of neurostimulators: A single-center single-blinded randomized controlled trial. Acta Anaesthesiol Scand. 2019 Nov;63(10):1321-1329. Doi: 10.1111/aas.13452. Epub 2019 Aug 9. PMID: 31321763.
- Yusuf S, Collins R, Peto R. Why do we need some large, simple randomized trials? Stat Med. 1984 Oct-Dec;3(4):409-22. Doi: 10.1002/sim.4780030421. PMID: 6528136.
Evidence tabellen
This table is also suitable for diagnostic studies (screening studies) that compare the effectiveness of two or more tests. This only applies if the test is included as part of a test-and-treat strategy – otherwise the evidence table for studies of diagnostic test accuracy should be used.
Risk of bias table for intervention studies (randomized controlled trials; based on Cochrane risk of bias tool and suggestions by the CLARITY Group at McMaster University)
Research question:
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated? a
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?b
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?c
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded?
Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?d
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?e
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?f
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measureg
LOW Some concerns HIGH
|
|
Apan, 2009 |
Probably yes
Reason: The randomization procedure was performed by choosing sealed envelopes before the operation by one of the anesthetists. The study drugs were prepared, coded and stored by the hospital pharmacy, and the codes were broken after all data had been finalized. |
Probably yes;
Reason: The randomization procedure was performed by choosing sealed envelopes before the operation by one of the anesthetists. The study drugs were prepared, coded and stored by the hospital pharmacy, and the codes were broken after all data had been finalized. |
Probably yes
Reason: Patients, health care providers and outcome assessors blinded (blinding of data collectors and analysts not reported) |
Probably yes
Reason: Loss to follow-up was not mentioned but due to the design unlikely to have occurred often |
Probably no
Reason: no pre-published protocol available. Not all defined outcomes in the methods were reported as such in the results |
Definitely yes;
Reason: No other problems noted |
Some concerns
Reason: no pre-published protocol available. Not all defined outcomes in the methods were reported in the results
|
|
Liao, 2012 |
Definitely yes
The trial is described as double blind study, patients were allocated by using a computer generated randomization list |
Definitely yes
The trial is described as double blind study, patients were allocated by using a computer generated randomization list |
Unclear
How patients, health care providers outcome assessors, data collectors and analysts were blinded is not reported |
Probably yes
Reason: Loss to follow-up was not mentioned but due to the design unlikely to have occurred often |
Unclear
Reason: no pre-published protocol available. |
Definitely yes;
Reason: No other problems noted |
Some concerns
Reason: no pre-published protocol available.
|
|
Samson (2014) |
Definitely yes
The trial is described as double blind study, patients were allocated by using a a computer generated randomization list |
Definitely yes
The trial is described as double blind study, patients were allocated by using a a computer generated randomization list |
Unclear
How patients, health care providers outcome assessors, data collectors and analysts were blinded is not reported |
Definitely yes
There was no lost to follow-up |
Unclear
Reason: no pre-published protocol available.
Some outcomes reported as ‘non-significant’ |
Definitely yes;
Reason: No other problems noted |
Some concerns
Reason: no pre-published protocol available.
Some outcomes only reported as ‘non-significant’ |
|
Kaya (2010) |
Definitely yes
The trial is described as double blind study, patients were allocated by using a a computer generated randomization list |
Definitely yes
The trial is described as double blind study, patients were allocated by using a a computer generated randomization list |
Unclear
How patients, health care providers outcome assessors, data collectors and analysts were blinded is not reported |
Probably yes
Reason: Loss to follow-up was not mentioned but due to the design unlikely to have occurred often |
Probably no
Reason: no pre-published protocol available. Not all defined outcomes in the methods were reported as such in the results |
Definitely yes;
Reason: No other problems noted |
Some concerns
Reason: no pre-published protocol available. Not all defined outcomes in the methods were reported in the results
|
|
Mishina (2018) |
Probably yes
This is a single blind study in which only patients who were randomized were blinded from the treatment |
Probably no
Patients were randomly divided into two groups by the envelope method (prone to bias) |
Probably no
This was a single blind study where only the patients were unaware which treatment they received |
Probably yes Reason: Loss to follow-up was reported but occurred in <3% of the participants |
Probably yes
Reason: no pre-published protocol available, many outcomes reported (not all defined in the methods) |
Probably No
Some of the prespecified outcomes were ill defined |
High
Single blind study, allocation concealment not optimal, no pre-published protocol, ill-defined outcomes, chance of selective reporting is non-negligible
|
|
Darwish (2012) |
Unclear
The study is described as an RCT, but how randomization was performed is not provided in the article |
Unclear
The article does not mention how (or if) allocation of treatment was concealed |
Unclear
The study is described as an RCT, but how randomization was performed and how/if treatment allocation was concealed is not provided in the article |
Probably yes
Reason: Loss to follow-up was not mentioned but due to the design unlikely to have occurred often |
Probably yes
Reason: no pre-published protocol available, many outcomes reported (not all defined in the methods) |
Probably No
Some of the prespecified outcomes were ill defined |
High
Unclear randomization/ treatment allocation procedure, no pre-published protocol, ill-defined outcomes, chance of selective reporting is non-negligible
|
|
Dey (2009) |
Probably yes
This is a single blind study in which only patients who were randomized were blinded from the treatment |
Probably no
Patients were randomly divided into two groups by the envelope method (prone to bias) |
Probably no
This was a single blind study where only the patients were unaware which treatment they received |
Probably yes
Reason: Loss to follow-up was not mentioned but due to the design unlikely to have occurred often |
Probably no
Reason: no pre-published protocol available. Not all defined outcomes in the methods were reported as such in the results |
Definitely yes;
Reason: No other problems noted |
High
Reason: Single blind study, allocation concealment not optimal, no pre-published protocol available. Not all defined outcomes in the methods were reported in the results
|
|
Eberl (2016) |
Definitely yes
The trial is described as double blind study, patients were allocated by using a a computer generated randomization list |
Definitely yes
The trial is described as double blind study, patients were allocated by using a a computer generated randomization list |
Probably yes
All parties concerned (patient, endoscopist, endoscopy nurse and independent investigator), with the exception of the specialised anaesthesia nurse who administered the sedation, were blinded to the drug employed. |
Probably yes
Only one patient (in the dexmedetomidine group) was lost to follow-up. |
Definitely yes
Trial protocol was published before results were analyzed |
Probably No
No 95% CI’s or SDs provided. Chance of type I and/or type II errors could not be studied
|
Some concerns
Differences in outcomes only reported with p-values, making it impossible to quantify the analysis or determine if there are potential type I/ type II errors |
|
Alizadehasl 2019 |
Probably yes
This is a single blind study in which only patients who were randomized were blinded from the treatment |
Probably yes
The patients’ allocation list was referred to a 3rd person and was concealed from the researchers. |
Probably yes
The patients’ allocation list was referred to a 3rd person and was concealed from the researchers. |
Probably no
3 patients (10% of total) were lost to follow-up in the comparator group, which might have affected results |
Definitely yes
Trial protocol was published before results were analyzed |
Probably No
Small numbers making the trial prone to type I/II errors |
Some concerns
Single blind study, allocation concealment not optimal, small numbers |
|
Ter Bruggen (2019) |
Probably yes
This is a single blind study in which patients who were randomized were blinded from the treatment |
Probably yes
The assignment of patients to either the experimental group (i.e. receiving dexmedetomidine) or the group receiving propofol was randomized by the hospital pharmacy using a randomization list compiled by a statistician. To ensure blinding, the hospital pharmacy provided white lines for infusion and covering material for the syringe. |
Probably yes
Sedation was performed by an anesthesiologist who could not be blinded to the study group allocation. The patient and the operator however were blinded to the study group allocation. In addition, a blinded observer, not involved in the sedation or the interventional procedure, enrolled the patients and performed all perioperative study measurements. |
Probably yes
One patient (in the dexmedetomidine group) was lost to follow-up and 2 patients (in the propofol;l group) were lost to follow-up. |
Probably yes
Trial protocol was published before results were analyzed. The study makes clear that it was powered for the primary outcome (patient satisfaction) only. Not all results were defined in the methods |
Probably yes
No 95% CI’s or SDs for outcomes provided.
Outcome recovery time, not provided |
Some concerns
Not all results were defined in the methods. |
- Randomization: generation of allocation sequences have to be unpredictable, for example computer generated random-numbers or drawing lots or envelopes. Examples of inadequate procedures are generation of allocation sequences by alternation, according to case record number, date of birth or date of admission.
- Allocation concealment: refers to the protection (blinding) of the randomization process. Concealment of allocation sequences is adequate if patients and enrolling investigators cannot foresee assignment, for example central randomization (performed at a site remote from trial location). Inadequate procedures are all procedures based on inadequate randomization procedures or open allocation schedules..
- Blinding: neither the patient nor the care provider (attending physician) knows which patient is getting the special treatment. Blinding is sometimes impossible, for example when comparing surgical with non-surgical treatments, but this should not affect the risk of bias judgement. Blinding of those assessing and collecting outcomes prevents that the knowledge of patient assignment influences the process of outcome assessment or data collection (detection or information bias). If a study has hard (objective) outcome measures, like death, blinding of outcome assessment is usually not necessary. If a study has “soft” (subjective) outcome measures, like the assessment of an X-ray, blinding of outcome assessment is necessary. Finally, data analysts should be blinded to patient assignment to prevents that knowledge of patient assignment influences data analysis.
- If the percentage of patients lost to follow-up or the percentage of missing outcome data is large, or differs between treatment groups, or the reasons for loss to follow-up or missing outcome data differ between treatment groups, bias is likely unless the proportion of missing outcomes compared with observed event risk is not enough to have an important impact on the intervention effect estimate or appropriate imputation methods have been used.
- Results of all predefined outcome measures should be reported; if the protocol is available (in publication or trial registry), then outcomes in the protocol and published report can be compared; if not, outcomes listed in the methods section of an article can be compared with those whose results are reported.
- Problems may include: a potential source of bias related to the specific study design used (e.g. lead-time bias or survivor bias); trial stopped early due to some data-dependent process (including formal stopping rules); relevant baseline imbalance between intervention groups; claims of fraudulent behavior; deviations from intention-to-treat (ITT) analysis; (the role of the) funding body. Note: The principles of an ITT analysis implies that (a) participants are kept in the intervention groups to which they were randomized, regardless of the intervention they actually received, (b) outcome data are measured on all participants, and (c) all randomized participants are included in the analysis.
- Overall judgement of risk of bias per study and per outcome measure, including predicted direction of bias (e.g. favors experimental, or favors comparator). Note: the decision to downgrade the certainty of the evidence for a particular outcome measure is taken based on the body of evidence, i.e. considering potential bias and its impact on the certainty of the evidence in all included studies reporting on the outcome.
Table of excluded studies
|
Author and year |
Reason for exclusion |
|
Ding (2017) |
Language barrier |
|
Grados (2017) |
Language barrier |
|
Joung (2015) |
Does not fit PICO |
|
Tanriverdi (2019) |
Does not fit PICO |
|
Wang (2020) |
Language barrier |
|
Yektas (2015) |
Language barrier |
|
Kim (2021) |
Does not fit PICO |
|
Ahmed (2021) |
Only abstract available |
|
Goyal (2016) |
Does not fit PICO |
|
Shoukry (2016) |
Does not fit PICO |
|
Wang (2017) |
Does not fit PICO |
|
Kumari (2021) |
Does not fit PICO |
|
Muttu (2005) |
Not accessible |
|
Frolich (2013) |
Does not fit PICO |
|
Peng (2018) |
Issues with data-analysis (fi, unclear randomization) |
|
Allashemi (2006 |
Randomized < 60 participants |
|
Cheung (2007) |
Randomized < 60 participants |
|
Fan (2013) |
Randomized < 60 participants |
|
Ustun (2006) |
Randomized < 60 participants |
|
Demiran (2007) |
Randomized < 60 participants |
|
Hashiguchi (2008) |
Randomized < 60 participants |
|
Frolich (2011) |
Randomized < 60 participants |
|
Sriganesh (2014) |
Randomized < 60 participants |
|
Na (2011) |
Randomized < 60 participants |
|
Ghali (2011) |
Randomized < 60 participants |
|
Wang (2004) |
Randomized < 60 participants |
|
Dogan (2010) |
Randomized < 60 participants |
|
Tsai (2010) |
Randomized < 60 participants |
|
Taniyama (2009) |
Randomized < 60 participants |
|
Mishra (2016) |
Randomized < 60 participants |
|
Ma (2012) |
Randomized < 60 participants |
|
Lin (2020) |
Randomized < 60 participants |
|
Khalil (2017) |
Randomized < 60 participants |
|
Muller (2008) |
Randomized < 60 participants |
|
Karanth (2018) |
Randomized < 60 participants |
|
Loh (2016) |
Randomized < 60 participants |
|
Maurya (2020) |
Randomized < 60 participants |
|
Kumar (2017) |
Randomized < 60 participants |
|
Elkalla (2020) |
Randomized < 60 participants |
Verantwoording
Beoordelingsdatum en geldigheid
Laatst beoordeeld : 23-05-2024
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2020 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij sedatie en/of analgesie bij volwassen patiënten.
Werkgroep
- Prof. dr. B. Preckel (voorzitter), anesthesioloog, Amsterdam UMC locatie AMC, NVA
- dr. C.R.M. Barends, anesthesioloog, UMCG, NVA
- L.R.M. Braam, BSc. Sedatie Praktijk Specialist, Catharina Ziekenhuis, NVAM
- drs. R. Brethouwer, abortusarts, Beahuis & Bloemenhovekliniek Heemstede, NGvA
- dr. J.M. van Dantzig, cardioloog, Catharina Ziekenhuis, NVVC
- drs. V.A.A. Heldens, anesthesioloog, Maxima MC, NVA
-
dr. C. Heringhaus, SEH-arts/anesthesioloog, LUMC (t/m 12-2022), Medisch manager Hyperbare Zuurstoftherapie Goes, MCHZ (vanaf 01-2023), NVSHA
- T. Jonkergouw, MA. Adviseur Patiëntbelang, Patiëntenfederatie Nederland (tot april 2023)
- Broere, M. Junior beleidsadviseur, Patiëntenfederatie Nederland (vanaf april 2023)
- dr. M. Klemt-Kropp, MDL-arts, Noordwest Ziekenhuisgroep, NVMDL
- drs. B.M.F. van der Leeuw, anesthesioloog, Albert Schweitzer ziekenhuis, NVA
- S. Reumkens, MSc. Physician Assistant, Diakonessenhuis, NAPA
Klankbordgroep
- drs. T.E.A. Geeraedts, radioloog, Erasmus MC, NVvR
- drs. J. Friederich, gynaecoloog, Noordwest Ziekenhuisgroep, NVOG
- dr. E.H.F.M. van der Heijden, longarts, Radboud UMC, NVALT
- drs. J. de Hoog, oogarts, Amsterdam UMC locatie AMC, NOG
- drs. A. Kanninga, arts voor verstandelijk gehandicapten, Cordaan, NVAVG
- drs. H.W.N. van der Pas, tandarts, UMC Utrecht, VMBZ
- dr. ir. C. van Pul, klinisch fysicus, Maxima MC, NVKF
- dr. R.J. Robijn, MDL-arts, Rijnstate, NVMDL
- drs. W.S. Segers, klinisch Geriater, Catharina Ziekenhuis, NVKG
- Prof. dr. A. Visser, hoogleraar geriatrische tandheelkunde, UMCG en Radboud UMC, KNMT
Met ondersteuning van:
- dr. L. Wesselman, adviseur, Kennisinstituut van Medisch Specialisten
- dr. S.N. Hofstede, senior adviseur, Kennisinstituut van Medisch Specialisten
- drs. I. van Dusseldorp, senior literatuurspecialist, Kennisinstituut van Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Preckel |
Anesthesioloog, hoogleraar anesthesiologie (in het bijzonder veiligheid in het perioperatieve proces) Amsterdam Universitair Medische Centra locatie AMC |
Onbetaalde nevenwerkzaamheden – commissie-werkzaamheden:
Lid Patient Safety and Quality Committee of the European Society of Anesthesiologists;
Lid Patient Safety Committee van de World Federation of Societies of Anesthesiologists;
Lid Raad Wetenschap en Innovatie van de Federatie Medisch Specialisten FMS;
Lid Commissie Wetenschap & Innovatie van de Nederlandse Vereniging voor Anesthesiologie NVA
Representative Council European Association of Cardiothoracic Anesthesiology and Intensive Care (EACTAIC)
Hoger leidinggevend personeel (penningmeester) van de “Stichting ter bevordering van de wetenschap en opleiding in de anesthesiologie”;
|
Research grants: European Society of Anesthesiology and Intensive Care ESAIC ZonMw NovoNordisk Netherland
Advisory board Sensium Healthcare United Kingdom
Geen van de gemelde belangen heeft relatie met het onderwerp van het advies/de richtlijn
|
Geen actie vereist |
|
Barends |
Anesthesioloog in het Universitair Medisch Centrum Groningen |
Geen |
Geen |
Geen actie vereist |
|
Braam |
Sedatiepraktijkspecialist Catharina Ziekenhuis Eindhoven |
Lid sedatie commissie NVAM (onbetaald) |
Geen |
Geen actie vereist |
|
Brethouwer |
Abortusarts te Beahuis & Bloemenhovekliniek (0,56 fte) en SAA (0,22 fte), Medisch coördinator Beahuis&Bloemenhovekliniek (0,33 fte) |
Penningmeester van het Nederlands Genootschap van Abortusartsen (onbetaald) Voorzitter landelijke werkgroep PSA van het NGvA (onbetaald) Bestuurslid van FIAPAC, een Europese abortus organisatie (onbetaald) |
Geen |
Geen actie vereist |
|
Broere |
Junior beleidsadviseur Patiëntenbelang - fulltime |
geen |
geen |
Geen actie vereist |
|
van Dantzig |
Cardioloog vrij gevestigd, Catharina Ziekenhuis 100% |
Lid Plenaire Visitatie Commissie NVVC (onbetaald) |
Op onze afdeling wordt extern gefinancierd onderzoek uitgevoerd maar niet op het gebied van de werkgroep. |
Geen actie vereist |
|
Heldens |
Anesthesioloog Maxima MC |
Geen |
Geen |
Geen actie vereist |
|
Heringhaus |
Vanaf 01-2023 Medisch manager Hyperbare Zuurstoftherapie Goes, MCHZ
t/m 12-2022 SEH-arts KNMG |
Trainingen voor verschillende onderwerpen gerelateerd aan acute zorg, hyperbare geneeskunde, PSA |
Geen |
Geen actie vereist |
|
Jonkergouw |
Junior beleidsadviseur - Patiëntenfederatie Nederland - 32 tot 36 uur per week |
Vrijwilliger activiteiten - Diabetes Vereniging Nederland - Zeer incidenteel |
Geen |
Geen actie vereist |
|
Klemt-Kropp |
MDL-arts, Noordwest Ziekenhuisgroep Alkmaar - Schagen - Den Helder (0.9 fte) |
Secretaris Concilium Gastroenterologicum, NVMDL tot 11 april 2022 (niet betaald) Voorzitter PSA commissie NVMDL (niet betaald) Docent Teach the Teacher AUMC en Noordwest Ziekenhuisgroep cursussen voor aios en medisch specialisten (betaalde functie, ongeveer 40 Std. per jaar)
Voorzitter Stichting MDL Holland-Noord (KvK 56261225) vanaf okt. 2012 t/m 31-12-2019. De stichting heeft in de laatste 3 jaar grants ontvangen van de farmaceutische industrie en van de farmaceutische industrie gesponsorde onderzoeken gefaciliteerd:
1. Ondersteuning optimalisering van zorg voor IBD-patiënten. Therapeutic drugmonitoring en PROMs bij patiënten met IBD. Zorgverbetertraject. PhD student, looptijd van 2015 tot op heden. Tot 2018 grant van Dr. Falk Pharma. vanaf 2018 grant van Janssen Cilag Geen relatie met sedatie 2.Retrieval of patients chronically infected with Hepatitis B or Hepatitis C in Northern Holland. Afgesloten 2018. Project gefinancierd met grant van Gilead. Geen relatie met sedatie 3. SIPI. Screening op Infectieuze aandoeningen in Penitentiaire Inrichtingen. Project gefinancierd met grants van AbbVie, MSD en Gilead. Project begin 2019 afgesloten. Geen relatie met sedatie 4. 3DUTCH trial. Een observationeel onderzoek naar de effectiviteit van een behandeling van chronische hepatitis C met een combinatie van de antivirale middelen ombitasvir - paritaprevir /ritonavir, ± dasabuvir, ± ribavirine. Sponsor AbbVie. Studie afgesloten Jan. 2018 Geen relatie met sedatie 5. Remsima switch IFX9501 - An open-label, multicenter, non- inferiority monitoring program to investigate the quality of life, efficacy and safety in subjects with Crohn’s Disease (CD), Ulcerative Colitis (UC) in stable remission after switching from Remicade® (infliximab) to Remsima® (infliximab biosimilar) L016-048. Sponsor: Munipharma. Afgelsoten augustus 2018. Geen relatie met sedatie 6. NASH - NN9931-4296 Investigation of efficacy and safety of three dose levels of subcutaneous semaglutide once daily versus placebo in subjects with non-alcoholic steatohepatitis L016-061. Sponsor NovoNordisk. Studie afgesloten Feb. 2020. Geen relatie met sedatie 7. Randomized, Double-blind, Placebo-controlled, Parallel-group Efficacy and Safety Study of SHP647 as Induction Therapy in Subjects with Moderate to Severe Crohn's Disease (CARMEN CD 305). SHD-647-305. Sponsor Shire. Studie loopt sinds 2019. Geen relatie met sedatie 8. Randomized, Double-blind, Placebo-controlled, Parallel-group Efficacy and Safety Study of SHP647 as Maintenance Therapy in Subjects with Moderate to Severe Crohn's Disease (CARMEN CD 307). SHD-647-307. Sponsor Shire. Studie loopt sinds 2019. Geen relatie met sedatie 9. Estimating the prevalence of advanced liver fibrosis in a population cohort in care in Northern-Holland with the use of the non-invasive FIB-4 index. Grant van Gilead. Onderzoek afgesloten sept. 2019. Geen relatie met sedatie |
Incidenteel deelname aan advisory boards van de farmaceutische industrie (Gilead, Janssen Cilag, AbbVie: (hepatologische onderwerpen, vooral hepatitis C) Incidenteel voordrachten tijdens symposia gesponsord van de farmaceutische industrie (Gilead, AbbVie)
|
Geen actie vereist; meeste studies afgerond; nr. 1,7,8 lopen. Sponsoren (Dr. Falk Pharma & Shire) hebben geen relatie met sedatie. |
|
Reumkens |
Physician Assistant Anesthesiologie Radboud UMC |
Voorzitter vakgroep PA Anesthesiologie NAPA |
Geen |
Geen actie vereist |
|
Van der Leeuw |
Anesthesioloog |
Geen |
Geen |
Geen actie vereist |
|
Klankbordgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Robijn |
Mdl arts rijnstate ziekenhuis Arnhem |
Geen |
Geen |
Geen actie vereist |
|
Van der Heijden |
Longarts |
Voormalig Secretaris Sectie Interventie longziekten NVALT (onbezoldigd)
Lid Board of National Delegates European Association of Bronchology and International Pulmonology (namens NL, onbezoldigd)
|
Buiten het veld van deze richtlijn heeft mijn afdeling de afgelopen 3 jaar vergoedingen ontvangen voor de volgende activiteiten: - unrestricted research grants: Pentax Medical Europe, Philips, Astra Zeneca, Johnson&Johnson. - adviseur / consultant: Pentax Medical, Philips IGT, Johnson&Johnson. - spreker: Pentax Medical. |
Geen actie vereist |
|
Van der Pas |
Tandarts, UMC Utrecht |
Commissielid Horace Wells van de KNMT, stimulatie van de intercollegiale samenwerking bij tandheelkundige behandeling van bijzondere zorggroepen met farmacologische ondersteuning. Onbetaald. Voormalig commissielid Bijzondere Zorggroepen van de KNMT, toegankelijkheid van mondzorg voor kwetsbare zorggroep. Betaald via vacatiegelden. Gastdocent opleiding mondzorgkunde HU. Lezing mondzorg aan mensen met een verstandelijke beperking. Betaald. Gastdocent opleiding verpleegkundig-specialist GGZ. Lezing mondzorg in de geestelijke gezondheidszorg Betaald. Cursusleider lichte sedatie in de mondzorg, BT Academy. Meerdaagse cursus voor tandartsen en mondhygienisten om zich te bekwamen in lichte sedatie, m.n. training in de inhalatiesedatie met lachgas-zuurstof mengsel middels titratietechniek. Betaald. |
Geen |
Geen actie vereist |
|
De Hoog |
Oogarts in Amsterdam UMC (0,2 fte.) en Retina Operatie Centrum Amstelveen (0,4 fte.). Medisch manager Retina Operatie Centrum (0,2 fte.) |
Voorzitter Werkgroep Vitreoretinale Chirurgie Nederland (onbetaald) Lid redactieraad vaktijdschrift 'De Oogarts', uitgave van BPM-medica (onbezoldigd) Medeorganisator Eilanddagen (bijscholing uveïtis voor oogartsen, onbetaald) |
Geen |
Geen actie vereist |
|
Geeraedts |
Interventieradioloog Afdeling Radiologie en Nucleaire geneeskunde Erasmus Medisch Centrum, Rotterdam |
Geen |
Geen |
Geen actie vereist |
|
Van Pul |
Klinisch fysicus in Maxima Medisch Centrum |
Universitair Hoofd Docent aan de Technische Universiteit van Eindhoven (0,2 fte). Daar supervisor van PhD studenten bij HTSM (NWO-TTW gesubsidieerd) project waaraan ook een industriële partner deelneemt (https://www.nwo.nl/projecten/15345-0).
|
Geen |
Geen actie vereist |
|
Friederich |
Gynaecoloog NWZ Den Helder, Algemeen gynaecoloog met als aandachtsgebieden benigne gynaecologie, minimaal invasieve chirurgie en bekkenbodemproblematiek |
Vicevoorzitter calamiteitencommissie NVZ lid klachtencommissie NWZ Den Helder |
Geen |
Geen actie vereist |
|
Segers |
Klinisch geriater, St. Jans Gasthuis, Weert
|
Klinisch farmacoloog in opleiding, Catharina ziekenhuis, Eindhoven Onbetaald |
Geen |
Geen actie vereist |
|
Kanninga |
Arts Verstandelijk Gehandicapten (arts VG) bij Cordaan Amsterdam Anesthesioloog niet praktiserend |
Geen |
Geen |
Geen actie vereist |
|
Visser |
Hoogleraar geriatrische tandheelkunde fulltime (1 fte) - Afdeling Gerodontologie, Centrum voor Tandheelkunde en Mondzorgkunde, Universitair Medisch Centrum Groningen, Rijksuniversiteit Groningen, Nederland - Afdeling Gerodontologie, Faculteit Tandheelkunde, Radboud UMC, Radboud Universiteit Nijmegen, Nederland |
Geen |
Geen |
Geen actie vereist |
Inbreng patiëntenperspectief
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door het uitnodigen van de Patiëntenfederatie Nederland voor de invitational conference. Het verslag hiervan (zie aanverwante producten) is besproken in de werkgroep. Aanvullend heeft een afgevaardigde van de Patiëntenfederatie Nederland deelgenomen in de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de richtlijn. De conceptrichtlijn is tevens voor commentaar voorgelegd aan de Patiëntenfederatie Nederland en de aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijn is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming gedaan of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling zijn richtlijnmodules op verschillende domeinen getoetst (zie ook het hiervoor gebruikte stroomschema dat als uitgangspunt voor de beoordeling is gebruikt).
Uit de kwalitatieve raming blijkt dat er waarschijnlijk geen substantiële financiële gevolgen zijn. Een overzicht van uitkomsten van de kwalitatieve raming met bijbehorende toelichting vindt u in onderstaande tabel.
|
Module |
Uitkomst raming |
Toelichting |
|
Submodule Dexmedetomidine |
geen substantiële financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (>40.000 patiënten), volgt ook uit de toetsing dat het overgrote deel (±90%) van de zorgaanbieders en zorgverleners al aan de norm voldoet en het geen nieuwe manier van zorgverlening of andere organisatie van zorgverlening betreft, het geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners betreft en het geen wijziging in het opleidingsniveau van zorgpersoneel betreft. |
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor patiënten die procedurele sedatie en/of analgesie ondergaan. Tevens zijn er knelpunten aangedragen door de Nederlandse Vereniging voor Anesthesiologie, de Nederlandse Vereniging voor Heelkunde, de Nederlandse Vereniging voor Obstetrie en Gynaecologie, Nederlandse Vereniging voor Cardiologie, de Nederlandse Vereniging van Maag-Darm-Leverartsen, de Vereniging voor Keel-Neus-Oorheelkunde en Heelkunde van het Hoofd-Halsgebied, de Nederlandse Vereniging voor Intensive Care, de Nederlandse Internisten Vereniging, de Nederlandse Vereniging van Spoedeisende Hulp Artsen, het Nederlands Genootschap van Abortusartsen, de Nederlandse Vereniging van Anesthesiemedewerkers, de Verpleegkundigen & Verzorgenden Nederland, de Nederlandse Vereniging voor Mondziekten, Kaak- en Aangezichtschirurgie, de Vereniging Mondzorg voor Bijzondere Zorggroepen, Stichting Kind & Ziekenhuis, Inspectie Gezondheidszorg en Jeugd en de Vereniging van Artsen voor Verstandelijk Gehandicapten via een invitational conference. Een verslag hiervan is opgenomen onder aanverwante producten. Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. Review Manager 5.4 werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nul effect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
Zoekacties zijn opvraagbaar. Neem hiervoor contact op met de Richtlijnendatabase.