Wondirrigatie
Uitgangsvraag
Wat is het effect van verschillende oplossingen voor profylactische, intra-operatieve, incisionele wondirrigatie op het risico van postoperatieve wondinfecties bij chirurgische patiënten?
Aanbeveling
Onderstaande aanbevelingen hebben betrekking op de wondholte en niet op de preoperatieve huiddesinfectie:
- Gebruik een (steriel) antisepticum opgelost in water (niet in alcohol) voor profylactische, intra-operatieve, incisionele wondirrigatie ter preventie van postoperatieve wondinfecties.*#
* Tenzij er bij specifieke operaties, kans is op weefselschade of als de patiënt bekend is met allergie.
# Voor schone chirurgische interventies kan geen specifieke aanbeveling worden gedaan.
- Gebruik geen antibioticum/antibiotica opgelost in water wegens lagere bewijskracht, risico op resistentie ontwikkeling, en gelijk effect aan antiseptica.
- Gebruik niet enkel een zoutoplossing wegens beperkte effectiviteit.
Houd bij het prioriteren van chirurgische wonden voor wondirrigatie rekening met de a priori kans op POWI.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Bij de nieuwste inzichten voor de GRADE methodologie wordt rekening gehouden met klinische relevantie van een effect, waarbij voor- en nadelen tegen elkaar af worden gewogen. Deze methode verschilt hierin met de GRADE zoals toegepast op de andere modules binnen de richtlijn. Toelichting op de gehanteerde methode is te vinden in GRADE assessment onder het tabblad 'Evidence tabellen'. Uit deze door Groenen et al. gehanteerde methode volgt een hoge bewijskracht voor een klinisch significant effect van wondirrigatie met antiseptica opgelost in water op het verminderen van postoperatieve wondinfecties (POWI) ten opzichte van spoelen met zoutoplossing of niet spoelen.
Voor wondirrigatie met antibiotica opgelost in water is redelijke bewijskracht ten opzichte van spoelen met zoutoplossing en lage bewijskracht ten opzichte van niet spoelen dan de wond voor reductie van POWI. Daarnaast is er redelijk bewijs dat er weinig tot geen verschil is in effect tussen wondirrigatie met zoutoplossing en niet irrigeren. Er is weinig tot geen verschil in effect op POWI tussen wondirrigatie met antiseptica en antibiotica opgelost in water, maar de bewijskracht hiervoor is zeer laag.
Alleen in de subgroep voor niet gecontamineerde chirurgie werden afwijkende resultaten gevonden. Binnen deze subgroep werd alleen voor wondirrigatie met antiseptica opgelost in water ten opzichte van wondirrigatie met zoutoplossing een significant effect gevonden. De bewijskracht van de effecten binnen deze subgroep is echter niet vastgesteld door gebrek aan data.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
Het spoelen van de wond is geen voorkeursgevoelige beslissing. Echter, indien er bekende specifieke (huid)reacties van de patiënt op een bepaald antisepticum zijn, dient hier rekening mee te worden gehouden. Controleer daarom altijd of er bekende huidreacties zijn op een antisepticum.
Kosten (middelenbeslag)
Er is geen kosteneffectiviteitsanalyse beschikbaar. Echter is POWI een kostbare complicatie en draagt de reductie hiervan meer bij aan kostenbesparing dan de minimale individuele extra kosten voor een antisepticum opgelost in water.
Aanvaardbaarheid, haalbaarheid en implementatie
De interventie wordt reeds in wisselende mate ingezet, afhankelijk van soort ingreep, centrum en voorkeur operateur. Er zijn geen zorgen over de aanvaardbaarheid, haalbaarheid en implementatie. De antiseptica die voor wondirrigatie gebruikt kunnen worden moeten in water opgelost zijn. Deze producten zijn als oplossing in water beschikbaar en verkrijgbaar. In de statements on method of wound irrigation is te zien welke verschillende oplossingen er gebruikt zijn in de studies voor bijvoorbeeld povidone-iodine worden concentraties tussen de 0,35 en 10% gehanteerd.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
Deze netwerk meta-analyse laat een significant voordeel zien van intra-operatieve, incisionele wondirrigatie met zowel een antisepticum als een antibioticum ter preventie van postoperatieve wondinfecties, vergeleken met wondirrigatie met zoutoplossing en geen wondirrigatie.
Wondirrigatie met een antisepticum opgelost in water geniet de voorkeur boven antibioticum opgelost in water om de volgende redenen:
- Het effect van antiseptica kent een hogere bewijskracht;
- Er is weinig tot geen verschil in effect op POWI tussen irrigatie met antibiotica en antiseptica;
- er zijn serieuze zorgen over de bacteriële resistentie tegen antibiotica. Daarentegen zijn er geen tekenen dat bacteriële gevoeligheid voor jodium of chloorhexidine over de tijd afneemt.
In de subgroep voor schone chirurgie werd alleen voor wondirrigatie met antiseptica opgelost in water ten opzichte van wondirrigatie met zoutoplossing een significant effect gevonden. De andere vergelijkingen laten zeer brede betrouwbaarheidsintervallen zien, hoogstwaarschijnlijk als gevolg van het uitdunnen van data (slechts 11/41 geïncludeerde RCTs analyseren schone chirurgie) en daarmee het verlies aan statistische kracht, wat het moeilijk maakt om conclusies op subgroep niveau te trekken. Bovendien is een meta-regressie analyse niet mogelijk met de gebruikte methode (frequentist methode).
Onderbouwing
Achtergrond
Postoperatieve wondinfecties (POWI’s) zijn verantwoordelijk voor het merendeel van de complicaties na een operatie. Ze zijn geassocieerd met extra morbiditeit, mortaliteit, kosten en een verlengde opnameduur.1,2 Het risico op een POWI kan worden verminderd door gebruik van profylactische intra-operatieve irrigatie van de incisiewond (pIOWI), waarbij vuil, stofwisselingsafval en exsudaat, mogelijk besmet met micro-organismen, voorafgaand aan het sluiten van de wond worden weggespoeld.3 Er is een variëteit aan spoelvloeistoffen en toepassingsmethoden.
Internationale richtlijnen m.b.t. de preventie van POWI’s en eerder gepubliceerde (netwerk) meta-analyses geven tegenstrijdige aanbevelingen met betrekking tot het gebruik van pIOWI. Sinds de publicatie van de internationale richtlijnen zijn er veel RCTs over dit onderwerp gepubliceerd.
Conclusies / Summary of Findings
Surgical site infections (SSI)
Antibiotic vs antiseptic
|
Very low GRADE |
Antibiotic solutions may have little to no effect on SSI when compared with antiseptic solutions in surgical patients, but the evidence is very uncertain. |
Antibiotic vs saline
|
Moderate GRADE |
Antibiotic solutions likely reduce SSI when compared with saline in surgical patients. |
Antibiotic vs no irrigation
|
Low GRADE |
Antibiotic solutions may result in a reduction of SSI when compared with no irrigation in surgical patients. |
Antiseptic vs saline
|
High GRADE |
Antiseptic solutions result in a reduction of SSI when compared with saline in surgical patients. |
Antiseptic vs no irrigation
|
High |
Antiseptic solutions result in a reduction of SSI when compared with no irrigation in surgical patients. |
Saline vs no irrigation
|
Moderate GRADE |
Saline solutions likely result in little to no difference in SSI when compared with no irrigation in surgical patients. |
Samenvatting literatuur
Description of studies
We included 41 RCTs in our systematic review and 37 RCTs in the network meta-analysis, due to lack of events in all arms in four studies. The study characteristics of the RCTs included in the systematic review are listed in study characteristics. Irrigation solutions were grouped into antiseptic, antibiotic, or saline solutions.
The antibiotics applied in a solution in the different studies were cefazolin, gentamicin, rifampicin, imipenem, clindamycin, ceftriaxone, metronidazole and bacitracin. All but two studies described the antibiotic solutions to be aqueous. All antiseptic solutions studied were aqueous. Most antiseptic solutions were iodine based, with 18 RCTs nvestigating iodine solutions ranging from 0.1% to 10% in concentration. Other antiseptics in the included RCTs were polyhexanide, chlorhexidine, hydrogen peroxide and ESAAS (Electrolyzed Strongly Acidic Aqueous Solution). In the saline irrigation group, all studies described irrigation with saline 0.9%, except for one RCT in which Ringers’ lactate was used. Volume of irrigation and application method varied among all studies and irrigation groups (Statements on method of wound irrigation).
Results
In total, 17,188 patients were included in the systematic review, reporting 1,328 SSI corresponding to an overall incidence of 7.7%. Figure 1 shows the forest plot for the efficacy of the different types of irrigation solutions compared to no irrigation; the league table for this data is presented in Table 1. Antibiotic (RR 0.46 [95% CI 0.29 - 0.73]) and antiseptic (RR 0.60 [0.95% CI 0.44 - 0.81]) solutions both showed a significant effect in reducing SSI when compared to no irrigation. Saline irrigation showed no significant effect (RR 0.83 [95% CI 0.63 - 1.09]) compared to no irrigation. The effects on SSI reduction of antibiotic solutions and antiseptic solutions were not significantly different (RR 0.77; 95% CI 0.50 - 1.19).
Results from the subgroup- and sensitivity analyses can be found in subgroup and sensitivity analyses .
Level of evidence of the literature
Full evaluation of the certainty of evidence and considerations for grading are detailed in Table 2 and GRADE assessment . GRADE assessment, incorporating minimally important difference, resulted in a high certainty of evidence for two comparisons (antiseptic versus saline irrigation and antiseptic versus no irrigation) and moderate certainty for two comparisons (antibiotic versus saline irrigation and saline versus no irrigation). Low certainty of evidence was found for the comparison of antibiotic versus no irrigation, and very low certainty for antibiotic versus antiseptic irrigation.
Study characteristics
|
Study |
SSI / N total |
Treatment 1 |
Treatment 2 |
Type of surgery |
Wound class § |
SAP |
ROB |
Follow-up |
SSI definition |
|
Antibiotic vs Antiseptic (RR 0.77; 95% CI 0.50 – 1.19) |
|||||||||
|
Inojie 2023 |
8 / 80 |
Gentamicin in saline |
3.5% PI |
Open spine surgery |
1 |
Yes |
Some concerns |
30 days |
CDC |
|
Karuserci 2022*
|
2 / 200 |
Rifampicin in saline |
10% PI |
Caeserean section |
2 |
Yes |
Some concerns |
30 days |
CDC |
|
Nguyen 2021 |
11 / 88 |
Cefazolin, gentamicin, and bacitracin in saline |
0.05% chlorhexidine gluconate |
Bilateral mastectomy with tissue expander reconstruction |
1 |
Yes |
Some concerns |
28 days |
CDC |
|
Karuserci 2020*
|
28 / 200 |
Rifampicin in saline |
10% PI |
Gynecologic oncology surgery |
2 |
Yes |
High |
30 days |
CDC |
|
Karusersi 2019*
|
7 / 200 |
Rifampicin in saline |
10% PI |
Benign gynecologic surgery |
2 |
Yes |
Some concerns |
30 days |
¶a |
|
Antibiotic vs Saline (RR 0.56; 95% CI 0.37 – 0.83) |
|||||||||
|
Zeb 2023 |
12 / 106 |
Imipenem in saline |
Saline |
Open appendectomy |
2 – 4 |
Yes |
Some concerns |
3 weeks |
NR |
|
Karuserci 2022*
|
6 / 200 |
Rifampicin in saline |
Saline |
Caeserean section |
2 |
Yes |
Some concerns |
30 days |
CDC |
|
Shah 2021
|
14 / 80 |
Imipenem in saline |
Saline |
Appendectomy |
3 – 4 |
NR |
Some concerns |
NR |
NR |
|
Okunlola 2021
|
3 / 132 |
Ceftriaxone in saline |
Saline |
Neurosurgery |
1 |
Yes |
Some concerns |
30 days |
¶b |
|
Karuserci 2020*
|
28 / 200 |
Rifampicin in saline |
Saline |
Gynecologic oncology surgery |
2 |
Yes |
High |
30 days |
CDC |
|
Emile 2020*
|
17 / 150 |
Gentamicin in saline |
Saline |
Open appendectomy |
1 – 3 |
Yes |
Some concerns |
6 weeks |
CDC |
|
Karusersi 2019*
|
13 / 200 |
Rifampicin in saline |
Saline |
Benign gynecologic surgery |
2 |
Yes |
Some concerns |
30 days |
¶a |
|
Oller 2015 |
0 / 51 |
I. Gentamicin in saline |
Saline |
Axillary lymph node dissection in breast cancer |
1 |
Yes |
Some concerns |
2 weeks |
NR |
|
Ruiz-Tovar 2013¤ |
0 / 40 |
Gentamicin in saline |
Saline |
Elective axillary lymph node dissection due to axillary metastasis |
1 |
Yes |
Some concerns |
NR |
NR |
|
Etaati 2012*
|
5 / 100 |
Cefazolin in saline |
Saline |
Caeserean section |
2 |
Yes |
High |
1 week |
¶c |
|
Mirsharifi 2008
|
12 / 102 |
Cefazolin |
Saline |
Open cholecystectomy |
2 – 3 |
NR |
Some concerns |
6 weeks |
¶d |
|
Bhargava 2006
|
28 / 60 |
Metronidazole in saline |
Saline |
Exploratory laparotomy |
4 |
Yes |
High |
30 days |
¶e |
|
Antibiotic vs No irrigation (RR 0.46; 95% CI 0.29 – 0.73) |
|||||||||
|
Emile 2020*
|
17 / 150 |
Gentamicin in saline |
No irrigation |
Open appendectomy |
1 – 3 |
Yes |
Some concerns |
6 weeks |
CDC |
|
Etaati 2012*
|
5 / 150 |
Cefazolin in saline |
No irrigation |
Caeserean section |
2 |
Yes |
High |
1 week |
¶c |
|
Köşüş 2010
|
12 / 1272 |
Rifamycin |
No irrigation |
Caeserean section |
2 |
Yes |
Some concerns |
30 days |
CDC |
|
Antiseptic vs No irrigation (RR 0.60; 95% CI 0.44 – 0.81) |
|||||||||
|
Mueller 2023* |
44 / 394 |
0.04% polyhexanide |
No irrigation |
Emergency and elective abdominal laparotomy |
2 – 4 |
Yes |
Low |
30 days |
CDC |
|
Al-Abdulla 2021* |
16 / 80 |
1% PI |
No irrigation |
Open appendectomy |
3 – 4 |
Yes |
Some concerns |
10 days |
¶f |
|
Haider 2018
|
43 / 600 |
1% PI |
No irrigation |
Clean elective surgery |
1 |
Yes |
Some concerns |
4 weeks |
¶f |
|
Mahomed 2016 |
291 / 3270 |
10% PI |
No irrigation |
Caeserean section |
2 |
Yes |
Some concerns |
4 weeks |
CDC |
|
Iqbal 2015 |
25 / 166 |
1% PI
|
No irrigation |
Open appendectomy |
3 |
Yes |
Some concerns |
30 days |
¶f |
|
Kokavec 2008 |
2 / 162 |
3.5% PI |
No irrigation |
Orthopedic surgery of proximal femur, hip and pelvis in pediatric patients |
1 |
Yes |
Some concerns |
2 months |
¶g |
|
Antiseptic vs Saline (RR 0.72; 95% CI 0.57 – 0.93) |
|||||||||
|
Mueller 2023* |
68 / 587 |
0.04% polyhexanide |
Saline
|
Emergency and elective abdominal laparotomy |
2 – 4 |
Yes |
Low |
30 days |
CDC |
|
Maemoto 2023
|
60 / 950 |
10% PI |
Saline |
Elective gastroenterological surgery |
2 |
Yes |
Some concerns |
30 days |
CDC |
|
Zhao 2023
|
20 / 340 |
1% PI |
Saline |
Radical gastrectomy |
2 |
Yes |
Some concerns |
30 days |
CDC |
|
Karuserci 2022*
|
6 / 200 |
10% PI |
Saline |
Caeserean section |
2 |
Yes |
Some concerns |
30 days |
CDC |
|
Maghsoudipour 2022 |
0 / 50 |
3% hydrogen peroxide |
Saline |
Rhinoplasty |
1 |
NR |
Some concerns |
8 weeks |
¶h |
|
Al-Abdulla 2021* |
14 / 80 |
1% PI
|
Saline |
Open appendectomy |
3 – 4 |
Yes |
Some concerns |
10 days |
¶f |
|
Cohen 2020¤
|
3 / 173 |
0.35% PI |
Saline |
Pediatric posterior spinal fusion |
1 |
Yes |
Some concerns |
90 days |
CDC |
|
Akhavan - Sigari 2020 |
26 / 936 |
3.5% PI |
Saline |
Spinal fusion surgery |
1 |
Yes |
Some concerns |
12 months |
CDC |
|
Karuserci 2020*
|
28 / 200 |
10% PI |
Saline |
Gynecologic oncology surgery |
2 |
Yes |
High |
30 days |
CDC |
|
Strobel 2020 |
111 / 456 |
0.04% polyhexanide
|
Saline |
Elective abdominal laparotomy |
2 – 3 |
Yes |
Some concerns |
30 days |
CDC |
|
Karusersi 2019*
|
18 / 200 |
10% PI |
Saline |
Benign gynecologic surgery |
2 |
Yes |
Some concerns |
30 days |
¶a |
|
Vinay 2019 |
16 / 180 |
5% PI
|
Saline |
Elective laparotomy |
2 |
Yes |
Some concerns |
4 weeks |
CDC |
|
De Luna 2017 |
3 / 50 |
3% PI |
Saline |
Spine surgery |
1 |
Yes |
Some concerns |
30 days |
CDC |
|
Fei 2017 |
12 / 80 |
0.1% PI |
Saline |
Posterior lumbar interbody fusion surgery |
1 |
NR |
Some concerns |
NR |
NR |
|
Neeff 2016 |
41 / 197 |
0.04% polyhexanide |
Ringer’s solution |
Colorectal surgery |
2 – 4 |
NR |
Some concerns |
NR |
NR |
|
Takesue 2011 |
48 / 400 |
Electrolyzed Strongly Acidic Aqueous Solution |
Saline |
Elective colorectal surgery |
2 – 3 |
Yes |
Some concerns |
30 days |
¶a |
|
Chang 2006 |
6 / 244 |
0.35% PI |
Saline |
Lumbosacral posterolateral fusion surgery |
1 |
Yes |
Some concerns |
14 months |
NR |
|
Cheng 2005
|
7 / 414 |
0.35% PI |
Saline |
Spine surgery |
1 |
Yes |
Some concerns |
6 months |
¶i |
|
Saline vs No Irrigation (RR 0.83; 95% CI 0.63- 1.09) |
|||||||||
|
Mueller 2023* |
50 / 397 |
Saline |
No irrigation |
Emergency and elective abdominal laparotomy |
2 – 4 |
Yes |
Low |
30 days |
CDC |
|
Gomaa 2022
|
221 / 2890 |
Saline |
No irrigation |
Caeserean section |
2 |
NR |
Some concerns |
30 days |
¶j |
|
Al-Abdulla 2021*
|
18 / 80 |
Saline |
No irrigation |
Open appendectomy |
3 – 4 |
Yes |
Some concerns |
10 days |
¶f |
|
Gül 2021
|
18 / 230 |
Saline |
No irrigation |
Caeserean section |
2 |
Yes |
Some concerns |
7 days |
¶k |
|
Emile 2020*
|
17 / 150 |
Saline |
No irrigation |
Open appendectomy |
1 – 3 |
Yes |
Some concerns |
6 weeks |
CDC |
|
Aslan 2018
|
25 / 204 |
Saline |
No irrigation |
Caeserean section |
2 |
Yes |
Some concerns |
30 days |
NR |
|
Etaati 2012*
|
5 / 150 |
Saline |
No irrigation |
Caeserean section |
2 |
Yes |
High |
1 week |
¶c |
|
Güngördük 2010
|
36 / 520 |
Saline |
No irrigation |
Caeserean section |
2 |
Yes |
Some concerns |
6 weeks |
¶l |
|
Al-Ramahi 2006
|
21 / 206 |
Saline |
No irrigation |
Abdominal gynecologic surgery |
2 |
Yes |
High |
1 month |
¶m |
|
Platt 2003
|
0 / 30 |
Saline |
No irrigation |
Bilateral breast reduction |
1 |
NR |
Some concerns |
8 weeks |
NR |
|
Cervantes-Sánchez 2000 |
12 / 255 |
Saline |
No irrigation |
Appendectomy |
1 – 3 |
Yes |
Some concerns |
4 weeks |
¶n |
|
* Studies compare three wound irrigation solutions ¤ SSI secondary outcome, thus not adequately powered to detect SSI § 1: Clean, 2: Clean-contaminated, 3: Contaminated, 4: Dirty
SSI definitions, other than CDC: ¶a: National Nosocomial Infections Surveillance System (NNIS).1 ¶b: a modified scoring system: grade 0, normal healing; grade I, normal healing with mild erythema or epidermolysis; grade II, superficial wound infection with galeal/fascia intact; grade III, deep wound infection below the galeal/fascia but with intact dural; grade IIIa, no osteomyelitis; grade IIIb, with osteomyelitis; grade IIIc, with pachy meningitis; grade IV, meningitis without tissue breakdown excluding chemical meningitis; grade V, meningitis with breakdown of dural and fascia; grade VI, intracranial or intraspinal intradural abscess; grade Via, subdural empyema; grade Vib, intraparenchymal abscess; grade Vic, intraventricular abscess; grade Vid, combination. ¶c: at the time of discharge, the patients of all groups were trained to go to the hospital if they had fever or if they saw any erythema, swelling or discharge at the surgical site. Then, the patients were daily followed by telephone to see if they had signs of symptoms of SSIs. ¶d: infection was defined according to clinical symptoms: purulent discharge, pain, heat, swelling or erythema at site of the wound. Final diagnosis was made by the surgeon. ¶e: postoperatively, the wound was inspected after 48 h for any discharge, soakage, erythema, tenderness and pain. ¶f: Southampton grading: grade 0, healing is normal; grade I, normal healing + mild bruising; grade II, erythema / tenderness / heat; grade III, serous discharge; grade IV, purulent discharge. ¶g: infection was assumed when there was unexpected or increased pain, redness, swelling, increased temperature or discharge from the wound. ¶h: presence of infection was examined and reported as positive or negative. ¶i: infection was suspected when unusual pain, tenderness, erythema, induration, fever, or wound drainage was noted. Such findings were investigated with measurement of erythrocyte sedimentation rate, C-reactive protein, and bacteriological cultures from the operative site or blood. ¶j: tenderness, redness, hotness, swelling, purulent discharge. ¶k: purulent discharge or erythema, fever, induration, and tenderness in the surgical site, which required separation of the incision, indicated an infection. ¶l: wound infection was diagnosed when a wound drained purulent material or serosanguineous fluid in association with induration, warmth and tenderness. Suspected wound infections were opened for confirmation and wound cultures were taken. Haematoma, seroma, or wound breakdown in the absence of the previously discussed signs was not considered a wound infection. ¶m: defined as wound discontinuation associated with purulent discharge from the wound and local tenderness, hotness, and/or redness within 1 month of surgery. ¶n: a wound was considered to be infected accordingly to Krukowski et al.2 when there was a collection of pus or a positive bacteriologic culture from a wound discharge (as described by Ljunqvist3).
CDC, Centers for Disease Control and Prevention; N, number of patients; NR, not reported; PI, povidone iodine; ROB, risk of bias; RR, relative risk; SAP, systemic antibiotic prophylaxis; SSI, surgical site infection; 95% CI, 95% confidence interval
1 Emori, T. G. et al. National nosocomial infections surveillance system (NNIS): description of surveillance methods. Am J Infect Control 19, 19-35, doi:10.1016/0196-6553(91)90157-8 (1991). 2 Krukowski, Z. H., Irwin, S. T., Denholm, S. & Matheson, N. A. Preventing wound infection after appendicectomy: a review. Br J Surg 75, 1023-1033, doi:10.1002/bjs.1800751023 (1988). 3 Ljungqvist, U. Wound Sepsis after Clean Operations. Lancet 1, 1095-1097, doi:10.1016/s0140-6736(64)91291-7 (1964).
|
|||||||||
Statements on method of wound irrigation
|
Study |
Statements on method of wound irrigation
|
|
Mueller 2023 |
After randomization, patients received IOWI with 1000 ml of a 0·04% PHX solution, IOWI with 1000 ml NaCl 0·9%, or no irrigation. The wound was rinsed carefully with the respective solution and the excess was removed by suction. Debris and blood clots were removed from the wound using irrigation and suction. The wound was left moistened with the irrigation solution to ensure sufficient contact time (> 10 min). |
|
Maemoto 2023 |
IOWI is performed for one minute with 40 mL of aqueous 10% PVP-I (POVIDONE-IODINE solution 10% “MEIJI”; Meiji Seika Pharma Co., Ltd., Tokyo, Japan) in the study group, and the same procedure is performed with 100 mL of saline (Isotonic Sodium Chloride Solution “Hikari”; Hikari Pharmaceutical Co., Ltd., Tokyo, Japan) in the control group. |
|
Zhao 2023 |
After closing the peritoneal sutures with size 0 VICRYL Plus (Johnson & Johnson - Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA), the wound was irrigated with either 500 mL of 1% PVI solution or 500 ml of 0.9% NS. Size 4-0 VICRYL Plus intradermic sutures were used in all patients. |
|
Inoje 2023 |
Patients randomized into Group A had their spine wound irrigated with saline containing gentamicin solution (a liter of normal saline mixed with 80 mg of gentamicin injection) in a quantity sufficient to fill the wound to the level of the skin without overflow. The saline containing gentamicin solution was maintained in the incision for 3 minutes, after which the wound was flushed with the remaining saline containing gentamicin solution. Group B patients’ wounds were irrigated with a liter of 3.5% diluted PI solution. The surgical wound was filled with PI in a volume sufficient to fill the wound to the level of the skin without overflow. The PI solution was maintained in the incision for 3 minutes, after which the wound was flushed with the remaining dilute PI solution. |
|
Zeb 2023 |
Before the wound was stitched up, the tissues in group I were irrigated with one litre of saline containing one gramme of imipenem (1 mg/ml), while group II received one litre of regular saline. |
|
Karuserci 2022 |
All subcutaneous tissues were irrigated with 250 ml of saline. Then 3–5ml 10% povidone-iodine in group 2 and 250 mg/3 ml rifampicin in group 3 was applied directly on the subcutaneous tissue without diluting. The excess liquid was cleaned off and the subcutaneous tissue scrubbed with gauze. |
|
Gomaa 2022 |
Subcutaneous irrigation by 200cc saline before closure of the skin.
|
|
Maghsoudipour 2022 |
Irrigation with hydrogen peroxide or placebo was performed right before closure of the surgical site with sutures, using irrigation syringes prepared by a pharmacist at the time they were needed. In the intervention group, hydrogen peroxide 3% solution was used, while 0.9% sodium chloride solution was used in the placebo group. |
|
Al-Abdulla 2021 |
In this study group A, before skin closure, subcutaneous tissue was irrigated by 1% povidone iodine using 10cc syringe, kept there for 2 to 3 minute and then aspirated. Group B the subcutaneous tissue was washed by normal saline using 10cc syringe. Group C no irrigation was done. |
|
Shah 2021 |
NR
|
|
Nguyen 2021 |
TAS contained 1 g of cefazolin, 50,000 U of bacitracin, and 80 mg of gentamicin in 500 mL of normal saline. Both the Tissue Expander and mastectomy pocket were bathed in the respective solutions, and a 1-minute dwell time was employed based on data presented on the IrriSept website reporting similar efficacy with 1- or 5-minute exposure times for most organisms. |
|
Okunlola 2021 |
The patients in the subject group received 2 g of intravenous ceftriaxone (Roche-Rocephin) at induction of anaesthesia followed by 1 g 12 hourly for 24 h post-operatively and intra-operative wound irrigation with 250 mg/ml of ceftriaxone in normal saline. The patients in the control group received 2 g of intravenous (Roche-Rocephin) at induction of anaesthesia followed by 1 g 12 hourly for 24 h post-operatively and intraoperative wound irrigation with plain normal saline. The irrigation was done by jet and or droplets from 50 ml syringe. |
|
Gül 2021 |
The subcutaneous tissue was irrigated with 200 ml of saline solution (0.9% NaCl) in patients in the experimental group (Group 1, n=115), and not irrigated in those in the control group (n=115) before the skin was closed. |
|
Cohen 2020 |
After the initial culture collection, nonviable tissues were debrided and the wound was soaked for 3 minutes with enough 0.35% PVP-I or sterile saline to be in contact with the entire wound. No antibiotics were added to sterile saline. The wound was then irrigated with 2 L of saline regardless of randomization to limit confounding, since PVP-I must be irrigated with saline. |
|
Akhavan - Sigari 2020 |
Before bone grafting, the surgical wounds in the normal ssaline group were filled and soaked with 0.9% normal saline, suction was performed; the irrigation being repeated three times. In the PVI group, surgical wounds were irrigated with PVI 3% to fill and soak the wound for two minutes followed by normal saline irrigation. |
|
Karuserci 2020 |
All subcutaneous tissues were irrigated with 250 mL of saline. Then 10 mL of 10 % povidone-iodine in Group 2 and 500 mg/6 mL of rifampicin in Group 3 was applied directly on the subcutaneous tissue without being diluted. The excess liquid was cleaned off and the subcutaneous tissue scrubbed with a gauze. |
|
Strobel 2020 |
At the end of the operation, the peritoneal cavity was rinsed routinely with 0.9% sodium chloride solution at body temperature (Braun, Melsungen, Germany). Before closure of fascia, instruments and gloves were changed. After the closure of fascia, subcutaneous irrigation with 250mL 0.9% saline (Braun, Melsungen, Germany) or 250mL antiseptic 0.04% polyhexanide solution (Serasept2, Serag-Wiessner) was done according to the randomization list. The application time for polyhexanide was 10 minutes and for saline as biologically inactive agent 1 minute. |
|
Emile 2020 |
In group I, upon closure of the peritoneum gentamicin-saline solution (160 mg of gentamicin in 400 ml of normal saline 0.9%) was used by a 20-cm syringe for irrigation of every layer of the wound before its closure. The first layer was between the peritoneal membrane and the internal oblique muscles, the second layer was between the approximated internal oblique muscles and the external oblique aponeurosis, and finally the third layer (the subcutaneous space) after closure of the external oblique aponeurosis (Fig. 1). In group II, layer by layer irrigation of the wound with normal saline solution was performed in a similar manner. In group III, layer-by-layer closure of the surgical wound with polyglactin 2/0 sutures took place without irrigation. |
|
Karuserci 2019 |
All subcutaneous tissues were irrigated with 250 ml of saline. Then 500 mg/6 ml of rifampicin in group 2 and 10 ml of povidone iodine in group 3 was applied directly on the subcutaneous tissue without dilution. The excess liquid was cleaned off and the subcutaneous tissue scrubbed with gauze. |
|
Vinay 2019 |
In Group A, the incision site was treated with 400 ml, 0.9% normal saline and 100 ml 5% povidone-iodine solution. In Group B, the incision site was treated with 500 ml 0.9% normal saline solution. |
|
Haider 2018 |
In group A, before skin closure subcutaneous tissues were irrigated with 5 ml 1 % PVI solution in normal saline. The solution was kept in wound for five minutes then aspirated. In group B, no irrigation was done. |
|
Aslan 2018 |
Before the subcutaneous tissue closure in the saline group the subcutaneous saline irrigation was performed with a 200cc of saline (0.9%NaCl). No subcutaneous irrigation was applied in the control group before the skin closure. |
|
De Luna 2017 |
In group A, before applying the bone graft, low-pressure irrigation (Bio Pulse, Leader Medica) with PVP-I diluted to a 3% concentration (30 g/l) in 2 litres of saline for between 5 and 10 minutes was performed and then washed out by 1 litre of sodium chloride solution through a pulse irrigation device. In group B, low-pressure irrigation with 2 litres of saline solution for between 5 and 10 minutes was performed before applying bone graft. |
|
Fei 2017 |
The incision was flushed with 0.1% iodine solution (volume: 200 ml) and soaked for 2 min, then the incisions were flushed with normal saline under adequate hemostasis conditions. The incisions were flushed with saline solution in the usual way. |
|
Mahomed 2016 |
The intervention was wound irrigation with about 50 mls of 10% aqueous PVI solution (Betadine group). The solution in a bowl was poured in and around the incision site. |
|
Neeff 2016 |
NR
|
|
Oller 2015 |
All patients underwent a first lavage of the axillary surgical bed with physiologic saline. Group 1 underwent a second lavage with saline. Group 2 had a second lavage with a 240-mg gentamicin solution (Group 2), and Group 3 had a second lavage with a 600-mg clindamycin solution. |
|
Iqbal 2015 |
In the study group A, before skin closure, the subcutaneous tissue was irrigated with 4-5 cc of 1% diluted povidone-iodine solution. The solution was sprayed into the subcutaneous wound with the help of a 5cc syringe, kept there for 2-3 minutes and was then aspirated. However, in the control group B, no irrigation was done. |
|
Ruiz-Tovar 2013 |
In both groups, prior to the lavage, a microbiological sample from the surgical bed was obtained with a swab (sample 1), followed by a lavage with 500 ml normal saline. After aspiration of the saline, a new microbiological sample was obtained (sample 2). In Group 1 a second lavage with 500 ml normal saline was performed, while in Group 2 the second lavage was performed with an antibiotic solution, including gentamicin (240 mg) dissolved in 500 ml normal saline. |
|
Etaati 2012 |
In one group, after the surgery and before closing up the patients, 2 grams of cefazolin in 5 cc of distilled water were used to irrigate the patients. In the second group, 150 cc of normal saline was used to irrigate the patients and in the last group, no irrigation was used. |
|
Takesue 2011 |
In the ESAAS group the surgical wound was irrigated with at least 500 mL of ESAAS after the completion of fascial suture. In the saline solution group, the same amount of saline solution was used for wound irrigation. |
|
Güngördük 2010 |
In the study group, before skin closure, the subcuticular tissue was irrigated with 100 ml of sterile saline with a 30–60 ml syringe. The skin was then closed using a 3-0 Vicryl suture. In the control group, the subcuticular tissue was not irrigated with sterile saline and the skin was closed using a 3-0 Vicryl suture. |
|
Köşüş 2010 |
In the second group subcutaneous tissue was irrigated with rifamycin SV/ 250 mg, before closure of subcutaneous tissue. |
|
Kokavec 2008 |
Approximately 1 ml of betadine was diluted by adding approx. 30 ml of sterile saline solution to a concentration of about 0.35% povidone iodine for perioperative use (2-3 minutes) |
|
Mirsharifi 2008 |
One gram of injectable cefazolin was used to wash the wound after the surgery and just before closing the incision site, and the control group was without topical antibiotic. |
|
Bhargava 2006 |
In group A the wound was irrigated with normal saline and in group B 50–100mL of metronidazole (from a single manufacturer). The concentration used was 500 mg/100 mL, which was infiltrated in the subcutaneous tissues making sure that the area of infiltration exceeds that of the incision. |
|
Chang 2006 |
In group 1 composed of patients with odd serial numbers (study group), wounds were irrigated with 0.35% povidone-iodine solution to soak for 3 min, followed by an irrigation with 2000 c.c. of normal saline to remove povidone-iodine solution. No more wound irrigation was given after. In contrast, group 2 with patients even numbered (control group) was wound irrigated only with 2000 c.c. of normal saline. |
|
Al-Ramahi 2006 |
The 104 patients in the odd number group (group 1), underwent wound irrigation with 50 mL of normal saline solution (NaCl 0.9%) following surgery and before skin closure. The 102 patients in the even-number group (group 2) received no wound irrigation. |
|
Cheng 2005 |
The commercially available betadine solution used had a concentration of 10% povidoneiodine (100 mg of povidoneiodine per 1 mL of solution). Approximately 5 mL of povidoneiodine was diluted with normal saline to achieve a 0.35% povidoneiodine (3.5% betadine) solution for use during operation. The wound was irrigated with copious amounts of normal saline (2000 mL) after betadine solution irrigation. In group 2, irrigation with copious normal saline (2000 mL) was performed alone. |
|
Platt 2003 |
Each breast was preinfiltrated with 300 mL saline containing adrenaline diluted to 1:500,000, lignocaine, and hyaluronidase (Hyalase; CP Pharmaceuticals Ltd, Wrexham, UK). Infiltration was performed uniformly throughout the breast using a spinal needle and syringe, sparing the pedicle. |
|
Cervantes-Sánchez 2000 |
Group I (control) was treated with surgery and prophylactic systemic antibiotics and group II (experimental) was treated with surgery, antibiotics, and wound syringe pressure irrigation as follows: after closure of the fascial planes, we irrigated the subcutaneous fat tissue with 300 ml of normal saline solution, delivered with a 20-ml syringe with a 19-gauge intravenous (IV) catheter, applying to the embolus the force of one hand, at a distance of 2 cm from the wound tissues, aspirating the fluid collected in the wound with a bulb syringe. |
|
ESAAS, Electrolyzed Strongly Acidic Aqueous Solution; IOWI, intraoperative wound irrigation; NaCl, sodiumchloride; NR, not reported PHX, polyhexanide; PI, povidone-iodine; PVI, povidone-iodine; PVP-I, povidone-iodine; TAS, Triple Antibiotic Solution; NR, not reported |
|
Subgroup and sensitivity analyses
The forest plots show the network relative risks (RR) with corresponding 95% confidence intervals (CI) compared with no irrigation.
In the lower triangle of the league tables the network RR with corresponding 95% CI are shown. The upper triangle shows the RR of only the direct comparisons (comparable with a regular pairwise meta-analysis).
For instance, in Bijlage 6.a, the first column (in the lower triangle) shows the network RR with corresponding 95% CI of antibiotic compared with the other irrigation solutions. The last column (upper triangle) shows the direct RR with corresponding 95% CI of no irrigation compared with the other irrigation solutions.
A. Only clean surgery (CDC wound classification I)
Forest plot

League table
|
Antibiotic |
1.29 [0.34; 4.84] |
2.00 [0.15; 27.20] |
- |
|
1.95 [0.59; 6.42] |
Antiseptic |
0.17 [0.07; 0.43] |
0.65 [0.21; 2.04] |
|
0.40 [0.10; 1.60] |
0.21 [0.08; 0.51] |
Saline |
- |
|
1.26 [0.24; 6.59] |
0.65 [0.21; 2.04] |
3.12 [0.73; 13.35] |
No irrigation |
B. Excluding studies with only clean surgery
Forest plot

League table
|
Antibiotic |
1.04 [0.41; 2.60] |
0.55 [0.36; 0.84] |
0.19 [0.06; 0.58] |
|
0.61 [0.39; 0.95] |
Antiseptic |
0.79 [0.62; 1.02] |
0.81 [0.56; 1.17] |
|
0.52 [0.35; 0.77] |
0.85 [0.67; 1.07] |
Saline |
0.77 [0.57; 1.03] |
|
0.42 [0.27; 0.66] |
0.68 [0.52; 0.90] |
0.80 [0.63; 1.03] |
No irrigation |
C. Only upper-middle and high income countries
Forest plot

League table
|
Antibiotic |
0.82 [0.37; 1.84] |
0.45 [0.19; 1.10] |
0.04 [0.00; 0.74] |
|
0.63 [0.31; 1.27] |
Antiseptic |
0.68 [0.50; 0.92] |
0.81 [0.48; 1.35] |
|
0.46 [0.23; 0.92] |
0.73 [0.54; 0.97] |
Saline |
0.76 [0.48; 1.18] |
|
0.39 [0.18; 0.83] |
0.61 [0.41; 0.92] |
0.85 [0.58; 1.24] |
No irrigation |
D. Only low and lower-middle income countries
Forest plot

League table
|
Antibiotic |
7.00 [0.80; 61.57] |
0.63 [0.37; 1.08] |
0.25 [0.07; 0.91] |
|
0.97 [0.46; 2.03] |
Antiseptic |
0.56 [0.24; 1.31] |
0.68 [0.34; 1.37] |
|
0.62 [0.37; 1.03] |
0.64 [0.35; 1.15] |
Saline |
0.71 [0.40; 1.25] |
|
0.50 [0.26; 0.95] |
0.51 [0.29; 0.90] |
0.80 [0.50; 1.30] |
No irrigation |
E. Excluding studies with high risk of bias
Forest plot

League table
|
Antibiotic |
0.79 [0.30; 2.09] |
0.59 [0.32; 1.09] |
0.18 [0.05; 0.63] |
|
0.72 [0.42; 1.24] |
Antiseptic |
0.68 [0.51; 0.91] |
0.76 [0.51; 1.14] |
|
0.54 [0.32; 0.90] |
0.74 [0.57; 0.97] |
Saline |
0.72 [0.50; 1.03] |
|
0.43 [0.24; 0.76] |
0.60 [0.43; 0.82] |
0.80 [0.59; 1.09] |
No irrigation |
F. Only studies with adequate description of systemic antibiotic prophylaxis
Forest plot

League table
|
Antibiotic |
1.06 [0.49; 2.30] |
0.52 [0.30; 0.91] |
0.18 [0.06; 0.61] |
|
0.73 [0.44; 1.21] |
Antiseptic |
0.67 [0.49; 0.92] |
0.75 [0.46; 1.21] |
|
0.52 [0.32; 0.83] |
0.71 [0.53; 0.95] |
Saline |
0.71 [0.47; 1.06] |
|
0.41 [0.24; 0.70] |
0.56 [0.39; 0.80] |
0.79 [0.56; 1.11] |
No irrigation |
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
What is the effect of prophylactic intra-operative incisional wound irrigation using antiseptic, antibiotic or saline solutions (i) versus other solutions in adult patients undergoing surgical procedures (p) in the prevention of SSI?
P: Adults undergoing any surgical procedure
I: Prophylactic intra-operative incisional wound irrigation using antiseptic, antibiotic or saline solutions
C: Prophylactic intra-operative incisional wound irrigation using other antiseptic, antibiotic or saline solutions or no irrigation
O: SSI
Relevant outcome measures
The guideline development group considered occurrence of SSI as a crucial outcome measure for decision making. The working group defined thresholds for clinically relevant outcomes in accordance with current GRADE guidance and methodology.
Search and select (Methods)
The databases Medline (PubMed), Excerpta Medica Database (EMBASE) and Cochrane Central Register of Controlled Trial (CENTRAL) were searched with relevant search terms until June 12, 2023. The detailed search strategy is available on request via https://richtlijnendatabase.nl/. The systematic literature search resulted in 1583 hits. Studies were selected based on the following inclusion criteria: unpublished and published RCTs that investigated the effect of prophylactic incisional intra-operative wound irrigation on SSI rates in any type of surgery, using antiseptic, antibiotic, or saline solutions, compared to each other or to no irrigation. Other solutions investigated in the literature (e.g., castile soap by Bhandari et al)4 were not included because they did not fit into either an antiseptic or an antibiotic profile. Furthermore, studies investigating intra-cavity lavage (i.e. abdominal, peritoneal or mediastinal) or surgical lavage of any other kind were excluded. 146 studies were initially selected based on title and abstract screening. After reading the full text, 105 studies were excluded (see the table with reasons for exclusion in Reasons for exclusion after full text review ) and 41 studies were included.
Results
Forty-one studies were included in the systematic review and 37 RCTs in the network meta-analysis of the literature. Important study characteristics and results and quality assessments are summarized in the evidence tables and risk of bias tables under the 'evidence tabellen' tab and 'Study characteristics' under the 'Samenvatting literatuur' tab.
Referenties
- Aftab R, Dodhia VH, Jeanes C, Wade RG. Bacterial sensitivity to chlorhexidine and povidone-iodine antiseptics over time: a systematic review and meta-analysis of human-derived data. Sci Rep. Jan 7 2023;13(1):347. doi:10.1038/s41598-022-26658-1
- Akhavan-Sigari R, Abdolhoseinpour H. Operative site irrigation with povidone-iodine solution in spinal surgery for surgical site infection prevention: Can it be used safety? Anaesth Pain Intensi. Jul-Sep 2020;24(3):314-319. doi:10.35975/apic.v24i3.1282
- Al-Abdulla MOKK, A.M.; Al-Katrani, H.A.S. Topical Application of Povidone Iodine to Minimize Post Appendectomy Wound Infection. Indian Journal of Forensic Medicine & Toxicology. 2021;15(4):1743-1747.
- Al-Ramahi M, Bata M, Sumreen I, Amr M. Saline irrigation and wound infection in abdominal gynecologic surgery. Int J Gynaecol Obstet. Jul 2006;94(1):33-6.
- Aslan Çetin B, Aydogan Mathyk B, Barut S, Koroglu N, Zindar Y, Konal M, Atis Aydin A. The impact of subcutaneous irrigation on wound complications after cesarean sections: A prospective randomised study. Eur J Obstet Gynecol Reprod Biol. Aug 2018;227:67-70. doi:10.1016/j.ejogrb.2018.06.006
- Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. May 2017;96(1):1-15. doi:10.1016/j.jhin.2017.03.004
- Barakat NA, Rasmy SA, Hosny AE-DMS, Kashef MT. Effect of povidone-iodine and propanol-based mecetronium ethyl sulphate on antimicrobial resistance and virulence in Staphylococcus aureus. Antimicrobial Resistance & Infection Control. 2022/11/11 2022;11(1):139. doi:10.1186/s13756-022-01178-9
- Barreto R, Barrois B, Lambert J, Malhotra-Kumar S, Santos-Fernandes V, Monstrey S. Addressing the challenges in antisepsis: focus on povidone iodine. Int J Antimicrob Agents. Sep 2020;56(3):106064. doi:10.1016/j.ijantimicag.2020.106064
- Bhargava PK, N.M.A. Wound infection after metronidazole infiltration. Tropical Doctor. 2006;36:37-38.
- Brignardello-Petersen R, Bonner A, Alexander PE, et al. Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol. Jan 2018;93:36-44. doi:10.1016/j.jclinepi.2017.10.005
- Brignardello-Petersen R, Guyatt GH, Mustafa RA, Chu DK, Hultcrantz M, Schunemann HJ, Tomlinson G. GRADE guidelines 33: Addressing imprecision in a network meta-analysis. J Clin Epidemiol. Nov 2021;139:49-56. doi:10.1016/j.jclinepi.2021.07.011
- Brignardello-Petersen R, Mustafa RA, Siemieniuk RAC, et al. GRADE approach to rate the certainty from a network meta-analysis: addressing incoherence. J Clin Epidemiol. Apr 2019;108:77-85. doi:10.1016/j.jclinepi.2018.11.025
- Brignardello-Petersen R, Tomlinson G, Florez I, et al. Grading of recommendations assessment, development, and evaluation concept article 5: addressing intransitivity in a network meta-analysis. J Clin Epidemiol. Aug 2023;160:151-159. doi:10.1016/j.jclinepi.2023.06.010
- Cervantes-Sanchez CR, Gutierrez-Vega R, Vazquez-Carpizo JA, Clark P, Athie-Gutierrez C. Syringe pressure irrigation of subdermic tissue after appendectomy to decrease the incidence of postoperative wound infection. World J Surg. Jan 2000;24(1):38-41; discussion 41-2. doi:10.1007/s002689910008
- Chang FY, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. Can povidone-iodine solution be used safely in a spinal surgery? Eur Spine J. Jun 2006;15(6):1005-14. doi:10.1007/s00586-005-0975-6
- Cheng MTC, M.C.; Wang, S.T.; Yu, W.K.; Liu, C.L.; Chen, T.H. Efficacy of Dilute Betadine Solution Irrigation in the Prevention of Postoperative Infection of Spinal Surgery. SPINE. 2005;30(15):1689-1693.
- Cohen LL, Schwend RM, Flynn JM, et al. Why Irrigate for the Same Contamination Rate: Wound Contamination in Pediatric Spinal Surgery Using Betadine Versus Saline. J Pediatr Orthop. Nov/Dec 2020;40(10):e994-e998. doi:10.1097/BPO.0000000000001620
- De Luna V, Mancini F, De Maio F, Bernardi G, Ippolito E, Caterini R. Intraoperative Disinfection by Pulse Irrigation with Povidone-Iodine Solution in Spine Surgery. Adv Orthop. 2017;2017:7218918. doi:10.1155/2017/7218918
- Efthimiou O, Rücker G, Schwarzer G, Higgins JPT, Egger M, Salanti G. Network meta-analysis of rare events using the Mantel-Haenszel method. Statistics in Medicine. 2019;38(16):2992-3012. doi:https://doi.org/10.1002/sim.8158
- Emile SH, Elfallal AH, Abdel-Razik MA, El-Said M, Elshobaky A. A randomized controlled trial on irrigation of open appendectomy wound with gentamicin- saline solution versus saline solution for prevention of surgical site infection. Int J Surg. Sep 2020;81:140-146. doi:10.1016/j.ijsu.2020.07.057
- Etaati ZR, M.; Rajaee, M.; Askari, A.; Hosseini, S. Cefazoline or Normal Saline Irrigation Doesn’t Reduce Surgical Site Infections After Cesarean. International Electronic Journal of Medicine (IEJM). 2012;1(2):6-11.
- Fei J, Gu J. Comparison of Lavage Techniques for Preventing Incision Infection Following Posterior Lumbar Interbody Fusion. Med Sci Monit. Jun 20 2017;23:3010-3018. doi:10.12659/msm.901868
- Garner JS. CDC guideline for prevention of surgical wound infections, 1985. Supersedes guideline for prevention of surgical wound infections published in 1982. (Originally published in November 1985). Revised. Infect Control. Mar 1986;7(3):193-200. doi:10.1017/s0195941700064080
- Gillespie BM, Harbeck E, Rattray M, et al. Worldwide incidence of surgical site infections in general surgical patients: A systematic review and meta-analysis of 488,594 patients. Int J Surg. Nov 2021;95doi:ARTN 106136
- Gomaa EA, Abou-Gamrah AA, Eltalbanty EMM, Kamel OI. The effect of subcutaneous saline irrigation on wound complication after cesarean section: a randomized controlled trial. Voprosy ginekologii, akušerstva i perinatologii. 2022;21(2):25-32. doi:10.20953/1726-1678-2022-2-25-32
- Gül DK. The role of saline irrigation of subcutaneous tissue in preventing surgical site complications during cesarean section: A prospective randomized controlled trial. Journal of Surgery and Medicine. 2021;5(1):8-11. doi:10.28982/josam.842145
- Güngördük K, Asicioglu O, Celikkol O, Ark C, Tekirdag AI. Does saline irrigation reduce the wound infection in caesarean delivery? J Obstet Gynaecol. 2010;30(7):662-6. doi:10.3109/01443615.2010.494206
- Haider S, Basit A, Abbasi SH, Shah FH, Kiani YM. Efficacy of irrigation with povidone iodine solution before skin closure to reduce surgical site infections in clean elective surgeries. Rawal Medical Journal. Jul-Sep 2018;43(3):467-470.
- Inojie MO, Okwunodulu O, Ndubuisi CA, Campbell FC, Ohaegbulam SC. Prevention of Surgical Site Infection Following Open Spine Surgery: The Efficacy of Intraoperative Wound Irrigation with Normal Saline Containing Gentamicin Versus Dilute Povidone-Iodine. World Neurosurgery. May 2023;173:E1-E10. doi:10.1016/j.wneu.2022.12.134
- Investigators F, Bhandari M, Jeray KJ, et al. A Trial of Wound Irrigation in the Initial Management of Open Fracture Wounds. N Engl J Med. Dec 31 2015;373(27):2629-41.
- Iqbal MJ, M.; Qureshi, A.; Iqbal, S. Effect of povidone-iodine irrigation on post appendectomy wound Infection: randomized control trial. J Postgrad Med Inst. 2015;29(3):160-4.
- Karuserci OK, Sucu S, Ozcan HC, Tepe NB, Ugur MG, Guneyligil T, Balat O. Topical Rifampicin versus Povidone-Iodine for the Prevention of Incisional Surgical Site Infections Following Benign Gynecologic Surgery: A Prospective, Randomized, Controlled Trial. New Microbiologica. Oct 2019;42(4):205-209.
- Karuserci OK, Sucu S. Subcutaneous irrigation with rifampicin vs. povidone-iodine for the prevention of incisional surgical site infections following caesarean section: a prospective, randomised, controlled trial. J Obstet Gynaecol. Jul 4 2022;42(5):951-956. doi:10.1080/01443615.2021.1964453
- Karuserci OKB, O. Subcutaneous rifampicin versus povidone-iodine for the prevention of incisional surgical site infections following gynecologic oncology surgery - a prospective, randomized, controlled trial. Ginekol Pol. 2020;91(9):513-518. doi:10.5603/GP.a2020.0134
- Kokavec MF, M. Efficacy of Antiseptics in the Prevention of Post-Operative lnfections of the Proximal Femur, Hip and Pelvis Regions in Orthopedic Pediatric Patients. Analysis of the First Results. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca. 2008;75:105-109.
- Köşüş AK, N.; Güler, A.; Çapar, M. Rifamycin SV Application to Subcutanous Tissue for Prevention of Post-Cesarean Surgical Site Infection. European Journal of General Medicine. 2010;7(3):269-276.
- Laxminarayan R, Matsoso P, Pant S, Brower C, Rottingen JA, Klugman K, Davies S. Access to effective antimicrobials: a worldwide challenge. Lancet. Jan 9 2016;387(10014):168-75. doi:10.1016/S0140-6736(15)00474-2
- Maemoto R, Noda H, Ichida K, et al. Aqueous Povidone-Iodine Versus Normal Saline For Intraoperative Wound Irrigation on The Incidence of Surgical Site Infection in Clean-Contaminated Wounds After Gastroenterological Surgery: A Single-Institute, Prospective, Blinded-Endpoint, Randomized Controlled Trial. Annals of Surgery. May 2023;277(5):727-733. doi:10.1097/Sla.0000000000005786
- Maghsoudipour N, Mohammadi A, Nazari H, Nazari H, Ziaei N, Amiri SM. The effect of 3 % hydrogen peroxide irrigation on postoperative complications of rhinoplasty: A double-blinded, placebo-controlled Randomized Clinical Trial. J Craniomaxillofac Surg. Sep 2022;50(9):681-685. doi:10.1016/j.jcms.2022.06.012
- Mahomed K, Ibiebele I, Buchanan J, Betadine Study G. The Betadine trial - antiseptic wound irrigation prior to skin closure at caesarean section to prevent surgical site infection: A randomised controlled trial. Aust N Z J Obstet Gynaecol. Jun 2016;56(3):301-6. doi:10.1111/ajo.12437
- Mirsharifi SRERSHJ, S.; Bateni, H. The effect of antibiotic irrigation of surgical Incisions in prevention of Surgical Site Infection. Tehran University Medical Journal 2008;65(11):71-75.
- Mueller TCK, V.; Dimpel, R.; Blankenstein, C.; Egert-Schwender, S.; Strudthoff, J.; Lock, J.F.; Wiegering, A.; Hadian, A.; Lang, H.; Albertsmeier, M.; Neuberger, M.; Von Ehrlich-Treuenstätt, V.; Mihaljevic, A.L.; Knebel, P.; Pianka, F.; Braumann, C.; Uhl, W.; Bouchard, R.; Petrova, E.; Bork, U.; Distler, M.; Tachezy, M.; Izbicki, J.R.; Reissfelder, C.; Herrle, F.; Vay, C.; Knoefel, W.T.; Buia, A.; Hanisch, E.; Friess, H.; Reim, D. on behalf of the IOWISI Study Group. Intraoperative wound irrigation for the prevention of surgical site infection after laparotomy: the multicenter, double-blind, randomized controlled IOWISI trial (DRKS00012251) of the Study Centre of the German Surgical Society (SDGC CHIR-Net). only preprint2023.
- Neeff HP, Anna MS, Holzner PA, Wolff-Vorbeck G, Hopt UT, Makowiec F. Effect of Polyhexanide on the Incidence of Surgical Site Infections After Colorectal Surgery. Gastroenterology. Apr 2016;150(4):S1244-S1244. doi:Doi 10.1016/S0016-5085(16)34202-0
- Nguyen L, Afshari A, Green J, Joseph J, Yao J, Perdikis G, Higdon KK. Post-Mastectomy Surgical Pocket Irrigation With Triple Antibiotic Solution vs Chlorhexidine Gluconate: A Randomized Controlled Trial Assessing Surgical Site Infections in Immediate Tissue Expander Breast Reconstruction. Aesthet Surg J. Oct 15 2021;41(11):NP1521-NP1528. doi:10.1093/asj/sjab290
- Okunlola AI, Adeolu AA, Malomo AO, Okunlola CK, Shokunbi MT. Intra-operative wound irrigation with ceftriaxone does not reduce surgical site infection in clean neurosurgical procedures. Br J Neurosurg. Dec 2021;35(6):766-769. doi:10.1080/02688697.2020.1812518
- Oller I, Ruiz-Tovar J, Cansado P, Zubiaga L, Calpena R. Effect of Lavage with Gentamicin vs. Clindamycin vs. Physiologic Saline on Drainage Discharge of the Axillary Surgical Bed after Lymph Node Dissection. Surg Infect (Larchmt). Dec 2015;16(6):781-4. doi:10.1089/sur.2015.020
- Papadakis M. Wound irrigation for preventing surgical site infections. World J Methodol. Jul 20 2021;11(4):222-227. doi:10.5662/wjm.v11.i4.222
- Platt AJ, Mohan D, Baguley P. The effect of body mass index and wound irrigation on outcome after bilateral breast reduction. Ann Plast Surg. Dec 2003;51(6):552-5. doi:10.1097/01.sap.0000095656.18023.6b
- Puhan MA, Schunemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. Sep 24 2014;349:g5630. doi:10.1136/bmj.g5630
- Ruiz-Tovar J, Cansado P, Perez-Soler M, et al. Effect of gentamicin lavage of the axillary surgical bed after lymph node dissection on drainage discharge volume. Breast. Oct 2013;22(5):874-8. doi:10.1016/j.breast.2013.03.008
- Shah A, Sasoli NA, Sami F. Compare the Incidence of Surgical Site Infection after Appendectomy Wound Irrigation with Normal Saline and Imipenem Solutions. Pakistan Journal of Medical and Health Sciences. 2021;15(8):2184-2186. doi:10.53350/pjmhs211582184
- Song F, Glenny AM. Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomized controlled trials. Br J Surg. Sep 1998;85(9):1232-41. doi:10.1046/j.1365-2168.1998.00883.x
- Strobel RM, Leonhardt M, Krochmann A, et al. Reduction of Postoperative Wound Infections by Antiseptica (RECIPE)?: A Randomized Controlled Trial. Ann Surg. Jul 2020;272(1):55-64. doi:10.1097/SLA.0000000000003645
- Takesue Y, Takahashi Y, Ichiki K, Nakajima K, Tsuchida T, Uchino M, Ikeuchi H. Application of an electrolyzed strongly acidic aqueous solution before wound closure in colorectal surgery. Dis Colon Rectum. Jul 2011;54(7):826-32. doi:10.1007/DCR.0b013e318211b83a
- Teillant A, Gandra S, Barter D, Morgan DJ, Laxminarayan R. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: a literature review and modelling study. Lancet Infect Dis. Dec 2015;15(12):1429-37. doi:10.1016/S1473-3099(15)00270-4
- Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane Database of Systematic Reviews. Int J Epidemiol. Jun 2012;41(3):818-27. doi:10.1093/ije/dys041
- Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P t. Apr 2015;40(4):277-83.
- Vinay HGKR, G.; Arudhra, P.; Udayeeteja, B. Comparison of the Efficacy of Povidone-Iodine and Normal Saline Wash in Preventing Surgical Site Infections in Laparotomy Wounds-Randomized Controlled Trial. Surgery: Current Research. 2019;08(02)doi:10.4172/2161-1076.1000319
- Zeb AK, M.S.; Iqbal, A.; Khan, A.; Ali, I.; Ahmad, M. Compare the Frequency of Surgical Site Infections Following Irrigation of Appendectomy Wounds with Sterile Saline Solution Vs Imipenem Solution. 2023;17(2):617-619. doi:10.53350/pjmhs2023172617
- Zeng L, Brignardello-Petersen R, Hultcrantz M, et al. GRADE Guidance 34: update on rating imprecision using a minimally contextualized approach. J Clin Epidemiol. Oct 2022;150:216-224. doi:10.1016/j.jclinepi.2022.07.014
- Zeng L, Brignardello-Petersen R, Hultcrantz M, et al. GRADE guidelines 32: GRADE offers guidance on choosing targets of GRADE certainty of evidence ratings. J Clin Epidemiol. Sep 2021;137:163-175. doi:10.1016/j.jclinepi.2021.03.026
- Zhao LY, Zhang WH, Liu K, Chen XL, Yang K, Chen XZ, Hu JK. Comparing the efficacy of povidone-iodine and normal saline in incisional wound irrigation to prevent superficial surgical site infection: a randomized clinical trial in gastric surgery. J Hosp Infect. Jan 2023;131:99-106. doi:10.1016/j.jhin.2022.10.005
Evidence tabellen
GRADE assessment
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology was used to evaluate the the certainty of the evidence using a minimally contextualized approach for direct, indirect and the complete network meta-analysis evidence sequentially.
Minimally important benefit, -harm, or trivial to no effect was chosen as the target estimate based on the point estimate in relation to the minimally important difference. Considering the inherently different trade-offs between saline, antiseptic and antibiotic irrigation with respect to concerns on resistance and other adverse effects we defined different minimally important differences (MID) for these interventions. In line, the precedent set by the long standing practice to reserve surgical antibiotic prophylaxis for clean-contaminated procedures (unless special considerations such as the use of implant material apply), we defined the MID as 3.5% for the routine use of antibiotic irrigation based on the upper limit of the incidence of SSI in clean procedures at the time (5%) and the RR of SSI after the use of surgical antibiotic prophylaxis in common clean-contaminated procedures (0.35). The MID for other interventions was defined as 2% based on the default for appreciable benefit and harm of 25% and the SSI incidence of 8% without irrigation in the presented data.
Since all included studies are randomised controlled trials, the rating for the GRADE starts high for all direct comparisons. Starting GRADE for the indirect evidence was based on the lowest of the two most dominant first order direct comparisons contributing to the indirect evidence. Starting GRADE for the network meta-analysis evidence was based on the highest certainty of evidence of the contributing direct and indirect evidence or whichever of the two was available.
Each comparison can be downgraded due to one of the following reasons:
- Risk of bias
Of the 41 studies included in the network meta-analysis, four had an overall “High risk of bias”. Due to the network meta-analysis, this may have an effect on all the network estimates of all comparisons. We performed a (network) sensitivity meta-analysis excluding studies with high risk of bias. The results were comparable with the overall analysis, and downgrading for risk of bias was not needed. - Inconsistency
Low, moderate, and high inconsistency were characterized using the first and third quantiles of the empirical distribution of non-pharmacological interventions on subjective outcomes. For the direct evidence, -1 downgrade for inconsistency was necessary for the comparison antibiotic versus antiseptic (I2 = 50.6%, τ2 = 1.12). Coherence was only applied to the network meta-analysis evidence. For the assessment of coherence both the point estimates, confidence intervals and outcomes from the Separate Indirect from Direct Design Evidence node splitting (Appendix 5) analysis were interpreted in context.
Indirectness
Transitivity was only applied to indirect evidence. Due to the broad inclusion criteria and consequential clinical heterogeneity some intransitivity was anticipated. We evaluated transitivity by comparing the SSI incidence in the common control group between the two contributing direct comparisons and considered relative differences larger than 25% sufficient concern for downgrading. - Imprecision
Imprecision was only applied to the final evaluation of the evidence. Imprecision was evaluated taking the minimally important differences into account and assessing the optimal information size in case of large effects by calculating the ratio between the lowest and highest boundary of the confidence interval with a threshold for downgrading of 2.5. - Publication bias
The comparison-adjusted funnel plot showed in Appendix 8 shows no sign of small-study effects.
Network evidence
For all comparisons, both direct and indirect evidence are available. Therefore, we used the highest of the two certainty ratings as the certainty rating for the NMA estimate. The certainty of the network estimate can be upgraded if precision is greater than direct or indirect estimates.
|
Comparison |
Direct evidence |
Indirect evidence |
Network meta-analysis |
||||
|
Relative Risk (95%CI) |
Certainty of evidence |
Relative Risk (95%CI) |
Certainty of evidence |
Relative Risk (95%CI) |
Certainty of evidence |
Target |
|
|
Antibiotic vs antiseptic |
1.07 (0.51 – 2.24) |
ÅOOO very low |
0.64 (0.37 – 1.10) |
ÅÅOO low |
0.77 (0.50 – 1.19) |
ÅOOO very low |
Trivial to no effect |
|
Antibiotic vs saline |
0.57 (0.37 – 0.90) |
ÅÅÅO moderate |
0.59 (0.20 - 1.75) |
ÅOOO very low |
0.56 (0.37 – 0.83) |
ÅÅÅO moderate |
Minimally important benefit |
|
Antibiotic vs no irrigation |
0.19 (0.06 – 0.59) |
ÅÅOO low |
0.55 (0.34 - 0.90) |
ÅOOO very low |
0.46 (0.29 - 0.73) |
ÅÅOO |
Minimally important benefit |
|
Antiseptic vs saline |
0.67 (0.51 – 0.88) |
ÅÅÅÅ high |
1.00 (0.61 – 1.65) |
ÅOOO very low |
0.72 (0.57 – 0.93) |
ÅÅÅÅ high |
Minimally important benefit |
|
Antiseptic vs no irrigation |
0.77 (0.52 – 1.13) |
ÅÅÅO moderate |
0.40 (0.24 – 0.66) |
ÅÅOO low |
0.60 (0.44 – 0.81) |
ÅÅÅÅ high |
Minimally important benefit |
|
Saline vs no irrigation |
0.75 (0.54 – 1.04) |
ÅÅÅO moderate |
1.10 (0.59 – 2.08) |
ÅOOO very low |
0.83 (0.63 – 1.09) |
ÅÅÅO moderate |
Trivial to no effect |
|
Comparison |
Reasons for downgrading |
||
|
Direct evidence |
Indirect evidence |
Network meta-analysis |
|
|
Antibiotic vs antiseptic |
-1 inconsistency -3 imprecision |
-1 imprecision |
-2 imprecision |
|
Antibiotic vs saline |
-1 imprecision |
-3 imprecision -1 intransivity |
-1 imprecision |
|
Antibiotic vs no irrigation |
-2 imprecision |
-1 intransivity |
-1 incoherence |
|
Antiseptic vs saline |
no downgrade |
-3 imprecision
|
no downgrade |
|
Antiseptic vs no irrigation |
-1 imprecision |
-1 intransivity
|
no downgrade |
|
Saline vs no irrigation |
-1 imprecision |
-1 intransitivity -3 imprecision |
-1 imprecision |
GRADE conclusions surgical site infections (SSI)
Antibiotic vs antiseptic
|
Very low GRADE |
Antibiotics solutions may have little to no effect on SSI when compared with antiseptic solutions in surgical patients but the evidence is very uncertain. |
Antibiotic vs saline
|
Moderate GRADE |
Antibiotic solutions likely reduce SSI when compared with saline in surgical patients. |
Antibiotic vs no irrigation
|
Low GRADE |
Antibiotic solutions may result in a reduction of SSI when compared with no irrigation in surgical patients. |
Antiseptic vs saline
|
High GRADE |
Antiseptic solutions result in a reduction of SSI when compared with saline in surgical patients. |
Antiseptic vs no irrigation
|
High |
Antiseptic solutions result in a reduction of SSI when compared with no irrigation in surgical patients. |
Saline vs no irrigation
|
Moderate GRADE |
Saline solutions likely result in little to no difference in SSI when compared with saline in surgical patients. |
Figures and Tables
Figure 1: Forest plot
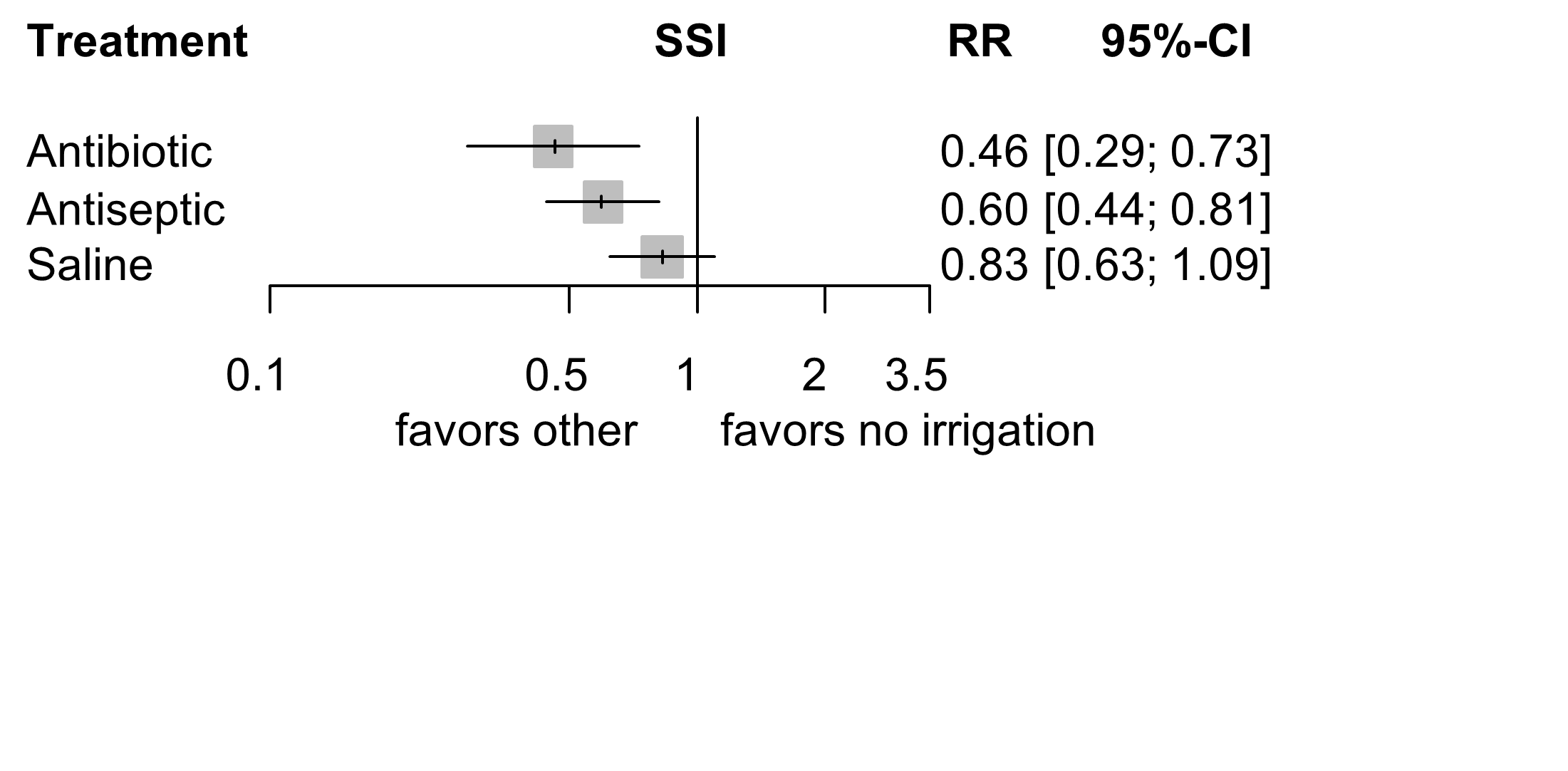
The forest plot shows the efficacy of different wound irrigation solutions in the prevention of surgical site infections (SSI) compared to no irrigation. Data are relative risk (RR) with corresponding 95% confidence interval (CI).
Table 1: League table
|
Antibiotic |
1.07 [0.51; 2.24] |
0.57 [0.37; 0.90] |
0.19 [0.06; 0.59] |
|
0.77 [0.50; 1.19] |
Antiseptic |
0.67 [0.51; 0.88] |
0.77 [0.52; 1.13] |
|
0.56 [0.37; 0.83] |
0.72 [0.57; 0.93] |
Saline |
0.75 [0.54; 1.04] |
|
0.46 [0.29; 0.73] |
0.60 [0.44; 0.81] |
0.83 [0.63; 1.09] |
No irrigation |
The league table is a square matrix showing all pairwise comparisons in the network meta-analysis. In the lower triangle of the league table the network relative risks (RR) with corresponding 95% confidence intervals (CI) are shown. The upper triangle shows the relative risks of only the direct comparisons (comparable with a regular pairwise meta-analysis).
For instance, the first column (in the lower triangle) shows the network RR with corresponding 95% CI of antibiotic compared with the other irrigation solutions. The last column (upper triangle) shows the direct RR with corresponding 95% CI of no irrigation compared with the other irrigation solutions.
Table 2: GRADE assessment
|
Comparison |
Direct evidence |
Indirect evidence |
Network meta-analysis |
||||
|
Relative Risk (95%CI) |
Certainty of evidence |
Relative Risk (95%CI) |
Certainty of evidence |
Relative Risk (95%CI) |
Certainty of evidence |
Target |
|
|
Antibiotic vs antiseptic |
1.07 (0.51 – 2.24) |
ÅOOO very low |
0.64 (0.37 – 1.10) |
ÅÅOO low |
0.77 (0.50 – 1.19) |
ÅOOO very low |
Trivial to no effect |
|
Antibiotic vs saline |
0.57 (0.37 – 0.90) |
ÅÅÅO moderate |
0.59 (0.20 - 1.75) |
ÅOOO very low |
0.56 (0.37 – 0.83) |
ÅÅÅO moderate |
Minimally important benefit |
|
Antibiotic vs no irrigation |
0.19 (0.06 – 0.59) |
ÅÅOO low |
0.55 (0.34 - 0.90) |
ÅOOO very low |
0.46 (0.29 - 0.73) |
ÅÅOO |
Minimally important benefit |
|
Antiseptic vs saline |
0.67 (0.51 – 0.88) |
ÅÅÅÅ high |
1.00 (0.61 – 1.65) |
ÅOOO very low |
0.72 (0.57 – 0.93) |
ÅÅÅÅ high |
Minimally important benefit |
|
Antiseptic vs no irrigation |
0.77 (0.52 – 1.13) |
ÅÅÅO moderate |
0.40 (0.24 – 0.66) |
ÅÅOO low |
0.60 (0.44 – 0.81) |
ÅÅÅÅ high |
Minimally important benefit |
|
Saline vs no irrigation |
0.75 (0.54 – 1.04) |
ÅÅÅO moderate |
1.10 (0.59 – 2.08) |
ÅOOO very low |
0.83 (0.63 – 1.09) |
ÅÅÅO moderate |
Trivial to no effect |
Network evidence
For all comparisons, both direct and indirect evidence are available. Therefore, we used the highest of the two certainty ratings as the certainty rating for the NMA estimate. The certainty of the network estimate can be upgraded if precision is greater than direct or indirect estimates.
GRADE = Grading of Recommendations Assessment, Development and Evaluation
Elaborate risk of bias assessment



Reasons for exclusion after full text review
|
|
Study |
Reason for exclusion |
|
1 |
Abdelrahman 20201 |
No data available |
|
2 |
Actrn 20202 |
Intra-cavity lavage |
|
3 |
Actrn 20123 |
Outcome, comparison or setting not of interest |
|
4 |
Akhavan-Sigari 20194 |
Conference abstract of included study (Akhavan-Sigari 2020)5 |
|
5 |
Aneja 20226 |
Study protocol |
|
6 |
Arslan 20207 |
No randomisation |
|
7 |
Baker 19948 |
Before the year 2000 |
|
8 |
Bhandari 20159 |
Outcome, comparison or setting not of interest |
|
9 |
Bourgeois 198510 |
Before the year 2000 |
|
10 |
Calkins 201911 |
Same data as Calkins 202012 |
|
11 |
Calkins 202012 |
Outcome, comparison or setting not of interest |
|
12 |
Conover 198413 |
Before the year 2000 |
|
13 |
Ctri 202314 |
Study protocol |
|
14 |
Ctri 202215 |
Study registration: no data available |
|
15 |
Ctri 202116 |
Study registration: no data available |
|
16 |
Ctri 202117 |
Study registration: intra-cavity lavage |
|
17 |
Ctri 201218 |
Study registration: no data available |
|
18 |
De Jong 198219 |
Before the year 2000 |
|
19 |
Dineen 201520 |
No randomisation |
|
20 |
Donnenfeld 198621 |
Before the year 2000 |
|
21 |
Drks 202222 |
Intra-cavity lavage |
|
22 |
Drks 201423 |
No randomisation |
|
23 |
Drks 201324 |
Study registration: no data available |
|
24 |
Elliott 198625 |
Before the year 2000 |
|
25 |
Englund 201926 |
No randomisation |
|
26 |
Euctr 201727 |
Study protocol of included study (Mueller 2023)28 |
|
27 |
Freischlag 198429 |
Before the year 2000 |
|
28 |
Greig 198730 |
Before the year 2000 |
|
29 |
Hargrove 200631 |
Outcome, comparison or setting not of interest |
|
30 |
Harrigill 200332 |
Intra-cavity lavage |
|
31 |
Irct20140503017537N, 201933 |
Study protocol |
|
32 |
Irct20200126046261N, 202034 |
Study protocol |
|
33 |
Isrctn 200535 |
Intra-cavity lavage |
|
34 |
Karuserci 202136 |
Same data as included study (Karuserci 2022)37 |
|
35 |
Kellum 198538 |
Before the year 2000 |
|
36 |
Ko 199239 |
Before the year 2000 |
|
37 |
Lavery 198640 |
Before the year 2000 |
|
38 |
Levin 198341 |
Before the year 2000 |
|
39 |
Lindsey 198242 |
Before the year 2000 |
|
40 |
Liu 201743 |
Intra-cavity lavage |
|
41 |
Lord 198344 |
Before the year 2000 |
|
42 |
Lord 197745 |
Before the year 2000 |
|
43 |
Maatman 201946 |
Intra-cavity lavage |
|
44 |
Maemoto 202147 |
Study protocol of included study (Maemoto 2023)48 |
|
45 |
Magann 199349 |
Before the year 2000 |
|
46 |
Mahomed 201650 |
Conference abstract of included study (Mahomed 2016)51 |
|
47 |
Marti 197952 |
Before the year 2000 |
|
48 |
Mashbari 201853 |
Intra-cavity lavage |
|
49 |
Mathelier 199254 |
Before the year 2000 |
|
50 |
Mohd 201055 |
Outcome, comparison or setting not of interest |
|
51 |
Moradi 201956 |
Intra-cavity lavage |
|
52 |
Mueller 201757 |
Study protocol of included study (Mueller 2023)28 |
|
53 |
Nct 202258 |
Study protocol |
|
54 |
Nct 202259 |
Study protocol |
|
55 |
Nct 202260 |
Study protocol |
|
56 |
Nct 202061 |
Study protocol |
|
57 |
Nct 202062 |
Study protocol of included study (Emile 2020)63 |
|
58 |
Nct 201964 |
Study protocol of included study (Strobel 2020)65 |
|
59 |
Nct 201866 |
Study protocol |
|
60 |
Nct 201867 |
Study protocol of included study (Emile 2020)63 |
|
61 |
Nct 201768 |
Intra-cavity lavage |
|
62 |
Nct 201669 |
Intra-cavity lavage |
|
63 |
Nct 201570 |
Same data as included study (Nguyen 2021)71 |
|
64 |
Nct 201572 |
Study protocol of included study (Cohen 2020)73 |
|
65 |
Nct 201474 |
Outcome, comparison or setting not of interest |
|
66 |
Nct 201275 |
No data available |
|
67 |
Nct 201276 |
Study protocol of included study (Etaati 2012)77 |
|
68 |
Nct 201178 |
Intra-cavity lavage |
|
69 |
Nct 200879 |
Study protocol of included study (Bhandari 2015)9 |
|
70 |
Nikfarjam 201480 |
Outcome, comparison or setting not of interest |
|
71 |
Oestreicher 198981 |
Before the year 2000 |
|
72 |
Patellugari 202082 |
Outcome, comparison or setting not of interest |
|
73 |
Pitt 198083 |
Before the year 2000 |
|
74 |
Pitt 198284 |
Before the year 2000 |
|
75 |
Pollock 197885 |
Before the year 2000 |
|
76 |
Quiroga-Garza 201786 |
Outcome, comparison or setting not of interest |
|
77 |
Rambo 197287 |
Before the year 2000 |
|
78 |
Rogers 198388 |
Before the year 2000 |
|
79 |
Ruiz-Tovar 201689 |
Intra-cavity lavage |
|
80 |
Ruiz-Tovar 201190 |
Intra-cavity lavage |
|
81 |
Ruiz-Tovar 201291 |
Intra-cavity lavage |
|
82 |
Ruiz-Tovar 201692 |
Same data as Ruiz-Tovar 201689 |
|
83 |
Salamat 202293 |
Outcome, comparison or setting not of interest |
|
84 |
Schottel 201694 |
Outcome, comparison or setting not of interest |
|
85 |
Silverman 198695 |
Before the year 2000 |
|
86 |
Sindelar 198596 |
Before the year 2000 |
|
87 |
Sindelar 197997 |
Before the year 2000 |
|
88 |
Sindelar 197798 |
Before the year 2000 |
|
89 |
Sood 198599 |
Before the year 2000 |
|
90 |
Tanaka 2015100 |
Intra-cavity lavage |
|
91 |
Tanphiphat 1978101 |
Before the year 2000 |
|
92 |
Tctr 2021102 |
Study protocol |
|
93 |
Temizkan 2016103 |
Intra-cavity lavage |
|
94 |
Terzi 2015104 |
Conference abstract of Arslan 20207 |
|
95 |
Tighe 1982105 |
Before the year 2000 |
|
96 |
Umin 2019106 |
Study protocol of included study (Maeomoto 2023)48 |
|
97 |
Umin 2012107 |
Intra-cavity lavage |
|
98 |
Umin 2011108 |
Intra-cavity lavage |
|
99 |
Vinay 2020109 |
Conference abstract of included study (Vinay 2019)110 |
|
100 |
Viney 2012111 |
Intra-cavity lavage |
|
101 |
Weiss 2013112 |
Outcome, comparison or setting not of interest |
|
102 |
Wu 1992113 |
Before the year 2000 |
|
103 |
Wu 1991114 |
Before the year 2000 |
|
104 |
Yang 2021115 |
Intra-cavity lavage |
|
105 |
Yazdi 2014116 |
Outcome, comparison or setting not of interest |
|
1 Abdelrahman, A. H. N., Samy, M. M., Shawky, M. E. A. & Azmy, G. A. Subcutaneous tissue irrigation with povidone iodine in decreasing the rate of surgical site infection following cesarean section: (randomized control trial). Qjm 113, i165-i166, doi:doi:https://dx.doi.org/10.1093/qjmed/hcaa056.020 (2020). 2 Actrn. Does Peritoneal Lavage Influence the Rate of Complications in Paediatric Laparoscopic Appendicectomy? A Prospective Multisite Randomised Controlled Trial. https://trialsearch.who.int/Trial2.aspx?TrialID=ACTRN12620000017921, doi:doi: (2020). 3 Actrn. Randomised controlled trial of pressure Irrigation of major surgical wounds. https://trialsearch.who.int/Trial2.aspx?TrialID=ACTRN12612000170820, doi:doi: (2012). 4 Akhavan-Sigari, R. & Vahedi, P. Intraoperative Irrigation with Povidone-Iodine Solution in Spine Surgery; Is it really safe? European Spine Journal 28, 2752, doi:doi:https://dx.doi.org/10.1007/s00586-019-06170-3 (2019). 5 Akhavan-Sigari, R. & Abdolhoseinpour, H. Operative site irrigation with povidone-iodine solution in spinal surgery for surgical site infection prevention: Can it be used safety? Anaesth Pain Intensi 24, 314-319, doi:10.35975/apic.v24i3.1282 (2020). 6 Aneja, A. et al. Does prophylactic local tobramycin injection lower open fracture infection rates? OTA International 5, E210, doi:doi:https://dx.doi.org/10.1097/OI9.0000000000000210 (2022). 7 Arslan, N. C., Degirmenci, A. K., Ozdenkaya, Y. & Terzi, C. Wound Irrigation with Chlorhexidine Gluconate Reduces Surgical Site Infection in Pilonidal Disease: Single-Blind Prospective Study. Surg Infect (Larchmt) 21, 143-149, doi:10.1089/sur.2019.053 (2020). 8 Baker, D. M. et al. Taurolidine peritoneal lavage as prophylaxis against infection after elective colorectal surgery. British Journal of Surgery 81, 1054-1056, doi:doi:https://dx.doi.org/10.1002/bjs.1800810743 (1994). 9 Bhandari, M. et al. A Trial of Wound Irrigation in the Initial Management of Open Fracture Wounds. New England journal of medicine 373, 2629‐2641, doi:doi:10.1056/NEJMoa1508502 (2015). 10 Bourgeois, F. J., Pinkerton, J. A., Andersen, W. & Thiagarajah, S. Antibiotic irrigation prophylaxis in the high-risk cesarean section patient. American Journal of Obstetrics and Gynecology 153, 197-201, doi:doi: (1985). 11 Calkins Tyler, E. et al. Dilute Betadine Lavage Reduces the Risk of Acute Postoperative Infection in Aseptic Revision Total Knee or Hip Arthroplasty: a Randomized Controlled Trial. American academy of orthopaedic surgeons, doi:doi: (2019). 12 Calkins, T. E. et al. Dilute Betadine Lavage Reduces the Risk of Acute Postoperative Periprosthetic Joint Infection in Aseptic Revision Total Knee and Hip Arthroplasty: A Randomized Controlled Trial. Journal of Arthroplasty 35, 538-543.e531, doi:doi:https://dx.doi.org/10.1016/j.arth.2019.09.011 (2020). 13 Conover, W. B. & Moore, T. R. Comparison of irrigation and intravenous antibiotic prophylaxis at cesarean section. Obstetrics and gynecology 63, 787‐791, doi:doi: (1984). 14 Ctri. Comparision of effectiveness of 3 antiseptics(1% povidone iodine , 0.9% saline, 0.04% polyhexanide ) in preventing surgical site infections when applied as a preventive measure before suturing the skin. https://trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2023/03/050211, doi:doi: (2023). 15 Ctri. Subcutaneous Saline irrigation during Caesarean section to reduce Superficial stitchline infections. https://trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2022/09/045576, doi:doi: (2022). 16 Ctri. SURGICAL SITE INFECTION FOLLOWING WOUND IRRIGATION WITH POVIDONE-IODINE VS NORMAL SALINE. https://trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2021/12/038632, doi:doi: (2021). 17 Ctri. Effect of antibiotics mixed peritoneal lavage on preventing postoperative surgical site infections in patients undergoing elective hepatectomies. https://trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2021/03/032430, doi:doi: (2021). 18 Ctri. A research to study the effects of normal saline wound irrigation on surgical wounds. https://trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2012/12/003197, doi:doi: (2012). 19 de Jong, T. E., Vierhout, R. J. & van Vroonhoven, T. J. Povidone-iodine irrigation of the subcutaneous tissue to prevent surgical wound infections. Surgery, gynecology & obstetrics 155, 221‐224, doi:doi: (1982). 20 Dineen, S. P. et al. Feasibility of subcutaneous gentamicin and pressurized irrigation as adjuvant strategies to reduce surgical site infection in colorectal surgery: results of a pilot study. American surgeon 81, 573‐579, doi:doi: (2015). 21 Donnenfeld, A. E., Otis, C. & Weiner, S. Antibiotic prophylaxis in cesarean section. Comparison of intrauterine lavage and intravenous administration. Journal of reproductive medicine 31, 15‐18, doi:doi: (1986). 22 Drks. Peritoneal antiseptic irrigation to prevent surgical site infection after laparotomy for hepatobiliary or gastrointestinal surgery. https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00028037, doi:doi: (2022). 23 Drks. POLihexanid for prevention of Infection in Surgery. https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00006004, doi:doi: (2014). 24 Drks. Effect of Polyhexanid (Lavanid) on the incidence of surgical side infections in colorectal surgery. https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00002698, doi:doi: (2013). 25 Elliott, J. P. & Flaherty, J. F. Comparison of lavage or intravenous antibiotics at cesarean section. Obstetrics and gynecology 67, 29‐32, doi:doi: (1986). 26 Englund, K. & Heidari, N. Is There a Role for the Use of Dilute Povidone-Iodine (Betadine) Irrigation or Other Antiseptic Irrigation Solutions During Total Ankle Arthroplasty (TAA) or Other Foot and Ankle Procedures? Foot and Ankle International 40, 14S-15S, doi:doi:https://dx.doi.org/10.1177/1071100719859329 (2019). 27 Euctr, D. E. Intraoperative wound irrigation to prevent surgical site infection after laparotomy. https://trialsearch.who.int/Trial2.aspx?TrialID=EUCTR2017-000152-26-DE, doi:doi: (2017). 28 Mueller, T. C. K., V.; Dimpel, R.; Blankenstein, C.; Egert-Schwender, S.; Strudthoff, J.; Lock, J.F.; Wiegering, A.; Hadian, A.; Lang, H.; Albertsmeier, M.; Neuberger, M.; Von Ehrlich-Treuenstätt, V.; Mihaljevic, A.L.; Knebel, P.; Pianka, F.; Braumann, C.; Uhl, W.; Bouchard, R.; Petrova, E.; Bork, U.; Distler, M.; Tachezy, M.; Izbicki, J.R.; Reissfelder, C.; Herrle, F.; Vay, C.; Knoefel, W.T.; Buia, A.; Hanisch, E.; Friess, H.; Reim, D. on behalf of the IOWISI Study Group. (only preprint, 2023). 29 Freischlag, J., McGrattan, M. & Busuttil, R. W. Topical versus systemic cephalosporin administration in elective biliary operations. Surgery 96, 686‐693, doi:doi: (1984). 30 Greig, J. et al. Wound sepsis after colorectal surgery: the effect of cefotetan lavage. Chemioterapia 6, 595-596, doi:doi: (1987). 31 Hargrove, R. et al. Does pulse lavage reduce hip hemiarthroplasty infection rates? Journal of hospital infection 62, 446‐449, doi:doi:10.1016/j.jhin.2005.07.012 (2006). 32 Harrigill, K. M., Miller, H. S. & Haynes, D. E. The effect of intraabdominal irrigation at cesarean delivery on maternal morbidity: A randomized trial. Obstetrics and Gynecology 101, 80-85, doi:doi:https://dx.doi.org/10.1016/S0029-7844%2802%2902466-3 (2003). 33 Irct20140503017537N. The effects of hydrogen peroxide irrigation on postoperative complications of rhinoplasty. https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20140503017537N6, doi:doi: (2019). 34 Irct20200126046261N. The effect of Gentamicin at cesarean section infection. https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20200126046261N1, doi:doi: (2020). 35 Isrctn. Intraabdominal irrigation at caesarean delivery and infectious morbidity: randomised controlled trial (RCT). https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN64436929, doi:doi: (2005). 36 Komurcu Karuserci, O. & Sucu, S. Subcutaneous irrigation with rifampicin vs. povidone-iodine for the prevention of incisional surgical site infections following caesarean section: a prospective, randomised, controlled trial. Journal of obstetrics and gynaecology, doi:doi: (2021). 37 Komurcu Karuserci, O. & Sucu, S. Subcutaneous irrigation with rifampicin vs. povidone-iodine for the prevention of incisional surgical site infections following caesarean section: a prospective, randomised, controlled trial. Journal of Obstetrics and Gynaecology 42, 951-956, doi:doi:https://dx.doi.org/10.1080/01443615.2021.1964453 (2022). 38 Kellum, R. B., Roberts, W. E., Harris, J. B., Khansur, N. & Morrison, J. C. Effect of intrauterine antibiotic lavage after cesarean birth on postoperative morbidity. Journal of reproductive medicine 30, 527‐529, doi:doi: (1985). 39 Ko, W., Lazenby, W. D., Zelano, J. A., Isom, O. W. & Krieger, K. H. Effects of shaving methods and intraoperative irrigation on suppurative mediastinitis after bypass operations. Annals of thoracic surgery 53, 301‐305, doi:doi:10.1016/0003-4975(92)91337-9 (1992). 40 Lavery, J. P. et al. Mezlocillin prophylaxis against infection after cesarean section: a comparison of techniques. Southern medical journal 79, 1248‐1251, doi:doi:10.1097/00007611-198610000-00013 (1986). 41 Levin, D. K., Gorchels, C. & Andersen, R. Reduction of post-cesarean section infectious morbidity by means of antibiotic irrigation. Am J Obstet Gynecol 147, 273-277, doi:doi:10.1016/0002-9378(83)91110-9 (1983). 42 Lindsey, D., Nava, C. & Marti, M. Effectiveness of penicillin irrigation in control of infection in sutured lacerations. Journal of trauma 22, 186‐189, doi:doi:10.1097/00005373-198203000-00002 (1982). 43 Liu, J. et al. A contrast study of Dermacyn on enterocoely irrigate to control intraoperative infection. Minerva chirurgica 72, 121‐124, doi:doi:10.23736/S0026-4733.16.07192-3 (2017). 44 Lord, J. W., LaRaja, R. D., Daliana, M. & Gordon, M. T. Prophylactic antibiotic wound irrigation in gastric, biliary, and colonic surgery. American journal of surgery 145, 209‐212, doi:doi:10.1016/0002-9610(83)90064-8 (1983). 45 Lord, J. W., Rossi, G. & Daliana, M. Intraoperative antibiotic wound lavage: an attempt to eliminate postoperative infection in arterial and clean general surgical procedures. Annals of surgery 185, 634‐641, doi:doi:10.1097/00000658-197706000-00004 (1977). 46 Maatman, T. K. et al. Antibiotic irrigation during pancreatoduodenectomy to prevent infection and pancreatic fistula: A randomized controlled clinical trial. Surgery (United States) 166, 469-475, doi:doi:https://dx.doi.org/10.1016/j.surg.2019.05.053 (2019). 47 Maemoto, R. et al. Superiority trial comparing intraoperative wound irrigation with aqueous 10% povidone–iodine to saline for the purpose of reducing surgical site infection after elective gastrointestinal surgery: study protocol for a randomised controlled trial. BMJ open 11, doi:doi:10.1136/bmjopen-2021-051374 (2021). 48 Maemoto, R. et al. Aqueous Povidone-Iodine Versus Normal Saline For Intraoperative Wound Irrigation on The Incidence of Surgical Site Infection in Clean-Contaminated Wounds After Gastroenterological Surgery: A Single-Institute, Prospective, Blinded-Endpoint, Randomized Controlled Trial. Annals of Surgery 277, 727-733, doi:10.1097/Sla.0000000000005786 (2023). 49 Magann, E. F. et al. Preoperative skin preparation and intraoperative pelvic irrigation: impact on post-cesarean endometritis and wound infection. Obstetrics and gynecology 81, 922‐925, doi:doi: (1993). 50 Mahomed, K., Ibiebele, I. & Buchanan, J. Povidone-Iodine wound irrigation prior to skin closure at caesarean section to prevent surgical site infection: A randomised controlled trial. BJOG: An International Journal of Obstetrics and Gynaecology 123, 146-147, doi:doi:https://dx.doi.org/10.1111/1471-0528.14106 (2016). 51 Mahomed, K., Ibiebele, I. & Buchanan, J. The Betadine trial - antiseptic wound irrigation prior to skin closure at caesarean section to prevent surgical site infection: A randomised controlled trial. Australian & New Zealand Journal of Obstetrics & Gynaecology 56, 301-306, doi:doi:10.1111/ajo.12437 (2016). 52 Marti, M. C. & Moser, G. Prevention of parietal septic complications by irrigation of the surgical wound. Helvetica chirurgica acta 45, 739‐742, doi:doi: (1979). 53 Mashbari, H. et al. A randomized controlled trial on intra-abdominal irrigation during emergency trauma laparotomy; Time for yet another paradigm shift. Bulletin of Emergency and Trauma 6, 100-107, doi:doi:https://dx.doi.org/10.29252/beat-060203 (2018). 54 Mathelier, A. C. A comparison of postoperative morbidity following prophylactic antibiotic administration by combined irrigation and intravenous route or by intravenous route alone during cesarean section. Journal of perinatal medicine 20, 177‐182, doi:doi:10.1515/jpme.1992.20.3.177 (1992). 55 Mohd, A. R., Ghani, M. K., Awang, R. R., Su Min, J. O. & Dimon, M. Z. Dermacyn irrigation in reducing infection of a median sternotomy wound. Heart surgery forum 13, E228‐232, doi:doi:10.1532/HSF98.20091162 (2010). 56 Moradi, M., Alemrajabi, M., Negahi, A., Vaseghi, H. & Arminfard, A. Gentamicin-clindamycin lavage on post-operational pain and infection in laparoscopic colectomy surgery. Colorectal disease 21, 17‐, doi:doi: (2019). 57 Mueller, T. C. et al. Intraoperative wound irrigation to prevent surgical site infection after laparotomy (IOWISI): Study protocol for a randomized controlled trial. Trials 18, doi:doi:https://dx.doi.org/10.1186/s13063-017-2154-6 (2017). 58 Nct. Efficacy of Diluted Betadine vs Antibiotic Installation Before Surgical Wound Closure in Prevention of Post Cardiac Surgery Wound Infection. https://clinicaltrials.gov/show/NCT05276687, doi:doi: (2022). 59 Nct. Randomized Controlled Trial Comparing Irrisept Versus Normal Saline for Wound Irrigation After Posterior Spine Surgery. https://clinicaltrials.gov/show/NCT05408923, doi:doi: (2022). 60 Nct. Rate of Total Joint Infection 90-day After Surgery Following Irrigation With Next Science No-Rinse Solution vs SOC Alone. https://clinicaltrials.gov/show/NCT05519007, doi:doi: (2022). 61 Nct. Clinical Evaluation of Adults Undergoing Elective Surgery Utilizing Intraoperative Incisional Wound Irrigation. https://clinicaltrials.gov/show/NCT04548661, doi:doi: (2020). 62 Nct. A Randomized Controlled Trial on Wound Irrigation in Open Appendectomy. https://clinicaltrials.gov/show/NCT04332809, doi:doi: (2020). 63 Emile, S. H., Elfallal, A. H., Abdel-Razik, M. A., El-Said, M. & Elshobaky, A. A randomized controlled trial on irrigation of open appendectomy wound with gentamicin- saline solution versus saline solution for prevention of surgical site infection. International Journal of Surgery 81, 140-146, doi:doi:https://dx.doi.org/10.1016/j.ijsu.2020.07.057 (2020). 64 Nct. Reduction of Postoperative Wound Infections by Antiseptica? https://clinicaltrials.gov/show/NCT04055233, doi:doi: (2019). 65 Strobel, R. M. et al. Reduction of Postoperative Wound Infections by Antiseptica (RECIPE)?: A Randomized Controlled Trial. Annals of surgery 272, 55-64, doi:doi:https://dx.doi.org/10.1097/SLA.0000000000003645 (2020). 66 Nct. Subcutaneous Tissue Irrigation With Povidone Iodine in Decreasing the Rate of Surgical Site Infection Following Cesarean Section. https://clinicaltrials.gov/show/NCT03549702, doi:doi: (2018). 67 Nct. Role of Wound Irrigation With Saline-gentamicin in Prevention of Wound Infection After Appendectomy. https://clinicaltrials.gov/show/NCT03773224, doi:doi: (2018). 68 Nct. The Effect of Intraabdominal Saline Irrigation in Abdominal Hysterectomies. https://clinicaltrials.gov/show/NCT03085732, doi:doi: (2017). 69 Nct. Betadine Irrigation in Cesarean Section. https://clinicaltrials.gov/show/NCT02865993, doi:doi: (2016). 70 Nct. Surgical Site Infection With 0.05% Chlorhexidine (CHG) Compared to Triple Antibiotic Irrigation. https://clinicaltrials.gov/show/NCT02395614, doi:doi: (2015). 71 Nguyen, L. et al. Post-Mastectomy Surgical Pocket Irrigation with Triple Antibiotic Solution vs Chlorhexidine Gluconate: A Randomized Controlled Trial Assessing Surgical Site Infections in Immediate Tissue Expander Breast Reconstruction. Aesthetic Surgery Journal 41, NP1521-NP1528, doi:doi:https://dx.doi.org/10.1093/asj/sjab290 (2021). 72 Nct. Bacterial Contamination: iodine vs Saline Irrigation in Pediatric Spine Surgery. https://clinicaltrials.gov/show/NCT02527512, doi:doi: (2015). 73 Cohen, L. L. et al. Why Irrigate for the Same Contamination Rate: wound Contamination in Pediatric Spinal Surgery Using Betadine Versus Saline. Journal of pediatric orthopedics 40, e994‐e998, doi:doi:10.1097/BPO.0000000000001620 (2020). 74 Nct. IrrSept vs. Standard of Care in Prevention of Surgical Site Infections. https://clinicaltrials.gov/show/NCT02255487, doi:doi: (2014). 75 Nct. The Use of Diluted Povidone Iodine Irrigation in Spine Surgery. https://clinicaltrials.gov/show/NCT01577524, doi:doi: (2012). 76 Nct. Effect of Cefazolin and Normal Saline Irrigation on Surgical Site Infections (SSIs). https://clinicaltrials.gov/show/NCT01566734, doi:doi: (2012). 77 Etaati, Z. R., M.; Rajaee, M.; Askari, A.; Hosseini, S. Cefazoline or Normal Saline Irrigation Doesn’t Reduce Surgical Site Infections After Cesarean. International Electronic Journal of Medicine (IEJM) 1, 6-11 (2012). 78 Nct. Effect of Peritoneal Lavage With Clindamycin-gentamicin Solution on Postoperative Colorectal Cancer Infection in Elective Surgery. https://clinicaltrials.gov/show/NCT01378832, doi:doi: (2011). 79 Nct. Fluid Lavage of Open Wounds. https://clinicaltrials.gov/show/NCT00788398, doi:doi: (2008). 80 Nikfarjam, M. et al. Pressurized pulse irrigation with saline reduces surgical-site infections following major hepatobiliary and pancreatic surgery: randomized controlled trial. World journal of surgery 38, 447-455, doi:doi:https://dx.doi.org/10.1007/s00268-013-2309-x (2014). 81 Oestreicher, M. & Tschantz, P. Prevention of infection at the operative site: irrigation with iodine derivatives, or NaCl. A prospective and randomized study in general surgery. Helvetica chirurgica acta 56, 133‐137, doi:doi: (1989). 82 Patellugari, B. T. R. et al. A prospective randomized controlled study of gentamycin irrigation in reducing the postoperative infections following upper tract endoscopy. Indian journal of urology 36, S52‐, doi:doi: (2020). 83 Pitt, H. A. et al. Prophylactic antibiotics in vascular surgery. Topical, systemic, or both? Ann Surg 192, 356-364, doi:10.1097/00000658-198009000-00011 (1980). 84 Pitt, H. A., Postier, R. G., Gadacz, T. R. & Cameron, J. L. The role of topical antibiotics in "high-risk" biliary surgery. Surgery 91, 518‐524, doi:doi: (1982). 85 Pollock, A. V., Froome, K. & Evans, M. The bacteriology of primary wound sepsis in potentially contaminated abdominal operations: the effect of irrigation, povidone-iodine and cephaloridine on the sepsis rate assessed in a clinical trial. British journal of surgery 65, 76‐80, doi:doi:10.1002/bjs.1800650204 (1978). 86 Quiroga-Garza, A. et al. A Prospective, Randomized, Controlled Clinical Trial to Assess Use of 2% Lidocaine Irrigation to Prevent Abdominal Surgical Site Infection. Ostomy/wound management 63, 12‐21, doi:doi: (2017). 87 Rambo, W. M. Irrigation of the peritoneal cavity with cephalothin. American journal of surgery 123, 192‐195, doi:doi:10.1016/0002-9610(72)90332-7 (1972). 88 Rogers, D. M., Blouin, G. S. & O'Leary, J. P. Povidone-iodine wound irrigation and wound sepsis. Surgery, gynecology & obstetrics 157, 426‐430, doi:doi: (1983). 89 Ruiz-Tovar, J., Llavero, C., Muñoz, J. L., Zubiaga, L. & Diez, M. Effect of Peritoneal Lavage with Clindamycin-Gentamicin Solution on Post-Operative Pain and Analytic Acute-Phase Reactants after Laparoscopic Sleeve Gastrectomy. Surg Infect (Larchmt) 17, 357-362, doi:doi:10.1089/sur.2015.196 (2016). 90 Ruiz-Tovar, J. et al. Evaluation of the effect of intabdominal irrigation with normal saline and a with a gentamicin-clindamicin solutionon the appearance of postoperative intrabdominal abscess and wound infection after elective surgery for colorectal cancer. Surgical Infections 12, A15, doi:doi:https://dx.doi.org/10.1089/sur.2011.9918 (2011). 91 Ruiz-Tovar, J. et al. Effect of peritoneal lavage with clindamycin-gentamicin solution on infections after elective colorectal cancer surgery. Journal of the American College of Surgeons 214, 202-207, doi:doi:https://dx.doi.org/10.1016/j.jamcollsurg.2011.10.014 (2012). 92 Ruiz-Tovar, J. et al. Effect of Peritoneal Lavage with Clindamycin-Gentamicin Solution during Elective Colorectal Cancer Surgery on the Oncologic Outcome. Surgical Infections 17, 65-70, doi:doi:10.1089/sur.2015.064 (2016). 93 Salamat, N., Khawaja, M. A. & Amir, W. Comparison of the Outcome of Gentamycin Lavage Versus Normal Saline Lavage for Axillary Dissection in Modified Radical Mastectomy. Pakistan journal of medical and health sciences 16, 159‐160, doi:doi:10.53350/pjmhs22169159 (2022). 94 Schottel, P. Wound irrigation pressure did not affect reoperation rate after open fracture repair, but normal saline solution was better than castile soap. Journal of bone and joint surgery - american volume 98, 871‐, doi:doi:10.2106/JBJS.16.00210 (2016). 95 Silverman, S. H., Ambrose, N. S. & Youngs, D. J. The effect of peritoneal lavage with tetracycline solution of postoperative infection. A prospective, randomized, clinical trial. Diseases of the Colon and Rectum 29, 165-169, doi:doi:http://dx.doi.org/10.1007/BF02555014 (1986). 96 Sindelar, W. F., Brower, S. T., Merkel, A. B. & Takesue, E. I. Randomised trial of intraperitoneal irrigation with low molecular weight povidone-iodine solution to reduce intra-abdominal infectious complications. Journal of hospital infection 6, 103‐114, doi:doi:10.1016/s0195-6701(85)80054-2 (1985). 97 Sindelar, W. F. & Mason, G. R. Irrigation of subcutaneous tissue with povidone-iodine solution for prevention of surgical wound infections. Surgery, gynecology & obstetrics 148, 227‐231, doi:doi: (1979). 98 Sindelar, W. F. & Mason, G. R. Efficacy of povidone-iodine irrigation in prevention of surgical wound infections. Surgical forum 28, 48‐51, doi:doi: (1977). 99 Sood, S., Kapur, B. M., Gupta, A. & Shriniwas, n. Role of intra-operative wound lavage in post-operative wound infection. Indian journal of medical research 81, 92‐95, doi:doi: (1985). 100 Tanaka, K. et al. Randomized clinical trial of peritoneal lavage for preventing surgical site infection in elective liver surgery. Journal of Hepato-Biliary-Pancreatic Sciences 22, 446-453, doi:doi:https://dx.doi.org/10.1002/jhbp.222 (2015). 101 Tanphiphat, C. et al. Wound infection in emergency appendicectomy: a prospective trial with tropical ampicillin and antiseptic solution irrigation. British journal of surgery 65, 89‐91, doi:doi:10.1002/bjs.1800650206 (1978). 102 Tctr. A randomized controlled trial comparing intro-operative wound irrigation with normal saline versus aqueous chlorhexidine for surgical site infection prevention. https://trialsearch.who.int/Trial2.aspx?TrialID=TCTR20211027010, doi:doi: (2021). 103 Temizkan, O. et al. The effect of peritoneal cavity saline irrigation at cesarean delivery on maternal morbidity and gastrointestinal system outcomes. Journal of Maternal-Fetal and Neonatal Medicine 29, 651-655, doi:doi:https://dx.doi.org/10.3109/14767058.2015.1015415 (2016). 104 Terzi, C., Arslan, N. C., Egeli, T. & a, A. E. Effect of irrigation with chlorhexidine gluconate on surgical site infections in pilonidal disease. European Surgery - Acta Chirurgica Austriaca 1, S86, doi:doi:https://dx.doi.org/10.1007/s10353-015-0305-0 (2015). 105 Tighe, B. et al. Betadine irrigation following appendicectomy--a randomized prospective trial. Irish medical journal 75, 96, doi:doi: (1982). 106 Umin. Effect of irrigation with aqueous iodophor solution on the incidence of surgical site infection after abdominal wall closure in gastroenterologic surgery: a double-blind, randomized controlled trial in a single center. https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000036889, doi:doi: (2019). 107 Umin. Effect of peritoneal lavege in liver surgery: a randomised trial. https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000007058, doi:doi: (2012). 108 Umin. Effect of peritoneal lavage in elective colorectal surgery: a randomised trial. https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000004967, doi:doi: (2011). 109 Vinay, H. G. & Reddy, R. Comparison of the efficacy of povidone-iodine and normal saline wash in preventing surgical site infections in laparotomy woundsrandomized controlled trial. Gut 69, A27, doi:doi:https://dx.doi.org/10.1136/gutjnl-2020-IDDF.41 (2020). 110 Vinay, H. G. K. R., G.; Arudhra, P.; Udayeeteja, B. Comparison of the Efficacy of Povidone-Iodine and Normal Saline Wash in Preventing Surgical Site Infections in Laparotomy Wounds-Randomized Controlled Trial. Surgery: Current Research 08, doi:10.4172/2161-1076.1000319 (2019). 111 Viney, R., Isaacs, C. & Chelmow, D. Intra-abdominal irrigation at cesarean delivery: A randomized controlled trial. Obstetrics and Gynecology 119, 1106-1111, doi:doi:https://dx.doi.org/10.1097/AOG.0b013e3182460d09 (2012). 112 Weiss, E. A., Oldham, G., Lin, M., Foster, T. & Quinn, J. V. Water is a safe and effective alternative to sterile normal saline for wound irrigation prior to suturing: a prospective, double-blind, randomised, controlled clinical trial. BMJ open 3, doi:doi:10.1136/bmjopen-2012-001504 (2013). 113 Wu, Y. Prevention of post-operative infection by using antibiotics of 217 cases of cesarean section. Zhonghua fu chan ke za zhi 27, 73‐75, 123, doi:doi: (1992). 114 Wu, Y., Zhan, L. & Jing, Y. Prevention of post-operative infection by uterine and intraperitoneal irrigation with ampicillin during cesarean section. International journal of experimental and clinical chemotherapy 4, 132‐136, doi:doi: (1991). 115 Yang, H. K. et al. Extensive peritoneal lavage with saline after curative gastrectomy for gastric cancer (EXPEL): a multicentre randomised controlled trial. The lancet. Gastroenterology & hepatology 6, 120‐127, doi:doi:10.1016/S2468-1253(20)30315-0 (2021). 116 Yazdi, H., Moradi, A. & Herbort, M. The effect of gentamicin in irrigating solutions on articular infection prophylaxis during arthroscopic ACL reconstruction. Archives of Orthopaedic and Trauma Surgery 134, 257-261, doi:doi:https://dx.doi.org/10.1007/s00402-013-1910-7 (2014). |
||
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 17-12-2024
Beoordeeld op geldigheid : 01-12-2024
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodules 2 tot 16 is in 2020 op initiatief van de NVvH een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor preventie van postoperatieve wondinfecties. Daarnaast is in 2022 op initiatief van het Samenwerkingsverband Richtlijnen Infectiepreventie (SRI) een separate multidisciplinaire werkgroep samengesteld voor de herziening van de WIP-richtlijn over postoperatieve wondinfecties: module 17-22. De ontwikkelde modules van beide werkgroepen zijn in deze richtlijn samengevoegd.
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoek financiering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Mevr. prof. dr. M.A. Boermeester |
Chirurg |
* Medisch Ethische Commissie, Amsterdam UMC, locatie AMC * Antibiotica Commissie, Amsterdam UMC |
Persoonlijke financiële belangen Hieronder staan de beroepsmatige relaties met bedrijfsleven vermeld waarbij eventuele financiële belangen via de AMC Research B.V. lopen, dus institutionele en geen persoonlijke gelden zijn: Skillslab instructeur en/of spreker (consultant) voor KCI/3M, Smith&Nephew, Johnson&Johnson, Gore, BD/Bard, TELABio, GDM, Medtronic, Molnlycke.
Persoonlijke relaties Geen.
Extern gefinancierd onderzoek Institutionele grants van KCI/3M, Johnson&Johnson en New Compliance.
Intellectuele belangen en reputatie Ik maak me sterk voor een 100% evidence-based benadering van maken van aanbevelingen, volledig transparant en reproduceerbaar. Dat is mijn enige belang in deze, geen persoonlijk gewin.
Overige belangen Geen.
|
Extra kritische commentaarronde. |
|
Dhr. dr. M.J. van der Laan |
Vaatchirurg |
Vice voorzitter Consortium Kwaliteit van Zorg NFU, onbetaald
|
Persoonlijke financiële belangen Geen.
Persoonlijke relaties Geen.
Extern gefinancierd onderzoek Geen.
Intellectuele belangen en reputatie Geen.
Overige belangen Geen.
|
Geen.
|
|
Dhr. dr. W.C. van der Zwet |
Arts-microbioloog |
Lid Regionaal Coördinatie Team, Limburgs infectiepreventie & ABR Zorgnetwerk (onbetaald) |
||
|
Dhr. dr. D.R. Buis |
Neurochirurg |
Lid Hoofdredactieraad Tijdschrift voor Neurologie & Neurochirurgie - onbetaald |
||
|
Dhr. dr. J.H.M. Goosen |
Orthopaedisch Chirurg |
Inhoudelijke presentaties voor Smith&Nephew en Zimmer Biomet. Deze worden vergoed per uur. |
||
| Dhr. drs. N. Bontekoning |
Arts-onderzoeker |
Geen. |
Persoonlijke financiële belangen Geen.
Persoonlijke relaties Geen.
Extern gefinancierd onderzoek Geen.
Intellectuele belangen en reputatie Geen.
Overige belangen Geen. |
Geen.
|
|
Mw. drs. H. Jalalzadeh |
Arts-onderzoeker |
|||
|
Dhr. dr. N. Wolfhagen |
AIOS chirurgie |
|||
|
Mw. drs. H. Groenen |
Arts-onderzoeker |
|||
|
Dhr. dr. F.F.A. Ijpma |
Traumachirurg |
|||
|
Dhr. dr. P. Segers |
Cardiothoracaal chirurg |
|||
|
Mw. Y.E.M. Dreissen |
AIOS neurochirurgie |
|||
|
Dhr. R.R. Schaad |
Anesthesioloog |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door uitnodigen van de Patiëntenfederatie Nederland voor de invitational conference. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptmodules zijn tevens voor commentaar voorgelegd aan de Patiëntenfederatie Nederland en de eventueel aangeleverde commentaren zijn bekeken en verwerkt. Voor de modules 17-22 was de patiëntfederatie vertegenwoordigd in de werkgroep.
Wkkgz & Kwalitatieve raming van mogelijke substantiële financiële gevolgen
Bij de richtlijn is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling zijn richtlijnmodules op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Uit de kwalitatieve raming blijkt dat er waarschijnlijk geen substantiële financiële gevolgen zijn.
Voor module 8 (Negatieve druktherapie) geldt dat uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (5.000 - 40.000 patiënten). Tevens volgt uit de toetsing dat het geen nieuwe manier van zorgverlening of andere organisatie van zorgverlening betreft. Er worden daarom geen substantiële financiële gevolgen verwacht.
Voor de overige modules en aanbevelingen geldt dat uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (>40.000 patiënten). Tevens volgt uit de toetsing dat het overgrote deel (±90%) van de zorgaanbieders en zorgverleners al aan de norm voldoet en het geen nieuwe manier van zorgverlening of andere organisatie van zorgverlening betreft. Ook wordt geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners verwacht of een wijziging in het opleidingsniveau van zorgpersoneel. Er worden daarom geen substantiële financiële gevolgen verwacht.
Methode ontwikkeling
Evidence based
Implementatie
Zie voor de implementatie het implementatieplan in het tabblad 'Bijlagen'.
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroepen de knelpunten in de zorg voor patiënten die chirurgie ondergaan. Tevens zijn er knelpunten aangedragen door middel van een invitational conference. De verslagen hiervan zijn opgenomen onder aanverwante producten.
Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Adaptatie
Een aantal modules van deze richtlijn betreft een adaptatie van modules van de World Health Organization (WHO)-richtlijn ‘Global guidelines for the prevention of surgical site infection’ (WHO, 2018), te weten:
- Module Normothermie
- Module Immunosuppressive middelen
- Module Glykemische controle
- Module Antimicrobiële afdichtingsmiddelen
- Module Wondbeschermers bij laparotomie
- Module Preoperatief douchen
- Module Preoperatief verwijderen van haar
- Module Chirurgische handschoenen: Vervangen en type handschoenen
- Module Afdekmaterialen en operatiejassen
Methode
- Uitgangsvragen zijn opgesteld in overeenstemming met de standaardprocedures van het Kennisinstituut van de Federatie Medisch Specialisten.
- De inleiding van iedere module betreft een korte uiteenzetting van het knelpunt, waarbij eventuele onduidelijkheid en praktijkvariatie voor de Nederlandse setting wordt beschreven.
- Het literatuuronderzoek is overgenomen uit de WHO-richtlijn. Afhankelijk van de beoordeling van de actualiteit van de richtlijn is een update van het literatuuronderzoek uitgevoerd.
- De samenvatting van de literatuur is overgenomen van de WHO-richtlijn, waarbij door de werkgroep onderscheid is gemaakt tussen ‘cruciale’ en ‘belangrijke’ uitkomsten. Daarnaast zijn door de werkgroep grenzen voor klinische besluitvorming gedefinieerd in overeenstemming met de standaardprocedures van het Kennisinstituut van de Federatie Medisch Specialisten, en is de interpretatie van de bevindingen primair gebaseerd op klinische relevantie van het gevonden effect, niet op statistische significantie. In de meta-analyses zijn naast odds-ratio’s ook relatief risico’s en risicoverschillen gerapporteerd.
- De beoordeling van de mate van bewijskracht is overgnomen van de WHO-richtlijn, waarbij de beoordeling is gecontroleerd op consistentie met de standaardprocedures van het Kennisinstituut van de Federatie Medisch Specialisten (GRADE-methode; http://www.gradeworkinggroup.org/). Eventueel door de WHO gerapporteerde bewijskracht voor observationele studies is niet overgenomen indien ook gerandomiseerde gecontroleerde studies beschikbaar waren.
- De conclusies van de literatuuranalyse zijn geformuleerd in overeenstemming met de standaardprocedures van het Kennisinstituut van de Federatie Medisch Specialisten.
- In de overwegingen heeft de werkgroep voor iedere aanbeveling het bewijs waarop de aanbeveling is gebaseerd en de aanvaardbaarheid en toepasbaarheid van de aanbeveling voor de Nederlandse klinische praktijk beoordeeld. Op basis van deze beoordeling is door de werkgroep besloten welke aanbevelingen ongewijzigd zijn overgenomen, welke aanbevelingen niet zijn overgenomen, en welke aanbevelingen (mits in overeenstemming met het bewijs) zijn aangepast naar de Nederlandse context. ‘De novo’ aanbevelingen zijn gedaan in situaties waarin de werkgroep van mening was dat een aanbeveling nodig was, maar deze niet als zodanig in de WHO-richtlijn was opgenomen. Voor elke aanbeveling is vermeld hoe deze tot stand is gekomen, te weten: ‘WHO’, ‘aangepast van WHO’ of ‘de novo’.
Voor een verdere toelichting op de procedure van adapteren wordt verwezen naar de Bijlage Adapteren.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
World Health Organization. Global guidelines for the prevention of surgical site infection,
second edition. Geneva: World Health Organization; 2018. (https://www.who.int/publications/i/item/9789241550475, accessed 12 June 2023).
Zoekverantwoording
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H,
Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
World Health Organization. Global guidelines for the prevention of surgical site infection,
second edition. Geneva: World Health Organization; 2018. (https://www.who.int/publications/i/item/9789241550475, accessed 12 June 2023).
