Muziek tijdens het intraoperatieve proces
Uitgangsvraag
Wat is de toegevoegde waarde van muziek tijdens het intraoperatieve proces voor patiënten die een invasieve operatie onder anesthesiologische begeleiding ondergaan?
Aanbeveling
De werkgroep kan geen aanbeveling doen voor het luisteren naar intraoperatieve muziek.
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Er is voor de literatuursamenvatting gebruik gemaakt van drie systematische reviews waarin de effecten van perioperatieve muziek op angst en/of pijn (Kühlmann, 2018), op de fysiologische stressrespons (Fu, 2019), en op het gebruik van medicatie en opnameduur (Fu, 2020) zijn beschreven. Een aanvullende zoektocht naar recente studies leverde zeven relevante RCT’s op het gebied van intraoperatieve muziek op, dit betrof in alle gevallen opgenomen muziek.
De meta-analyse van Kühlmann (2018) op basis van 10 RCT’s liet geen klinisch relevant effect zien voor pijn (SMD<0,2). Een meta-analyse van vier recente RCT’s liet ook geen klinisch relevant effect zien ten gunste van muziek (het verschil tussen de groepen was minder dan 1,2 punten op de VAS 0-10). De bewijskracht voor de uitkomstmaat pijn was zeer laag.
Voor angst lieten zowel de meta-analyse van Kühlmann (2018) op basis van 10 RCT’s als onze meta-analyse van vier recente RCT’s een klinisch relevant verschil (SMD>0,2) zien ten gunste van muziek, er was sprake van enige variatie in het effect tussen de studies. De bewijskracht was zeer laag.
Wat betreft medicatie liet de meta-analyse van Fu (2020) zien dat muziek voor, tijdens en/of na de operatie tot een klinisch relevant verschil in gebruik van opioïden, propofol en midazolam leidde, ten gunste van muziek (SMD>0,2). Het effect van alleen intraoperatieve muziek is niet duidelijk doordat hier geen subgroepanalyse naar werd gedaan. Vier recente RCT’s lieten slechts kleine verschillen in gebruik van medicatie zien, het is niet aannemelijk dat deze verschillen klinisch relevant zijn. De bewijskracht voor de uitkomst medicatie was zeer laag.
Voor drie van de belangrijke uitkomsten –stress, patiënttevredenheid en opnameduur – werden resultaten gerapporteerd. De meta-analyse van Fu (2019) liet zien dat er aan het eind van de operatie geen klinisch relevant verschil was in cortisolniveau (SMD<0,2), terwijl er postoperatief wel een klein klinisch relevant verschil werd gevonden (SMD>0,2). Er was echter wel sprake van variatie in het effect tussen de studies. Het effect van alleen intraoperatieve muziek is niet duidelijk doordat hier geen subgroepanalyse naar werd gedaan. Voor patiënttevredenheid werd in twee van de drie RCT’s een klinisch relevant verschil gerapporteerd (een verschil >10% tussen de groepen). Deze studies gebruikten een vragenlijst met een continue schaal, waarbij de resultaten gedichotomiseerd gepresenteerd werden (wel/niet tevreden), deze wijze van rapporteren is mogelijk niet gevalideerd. Voor opnameduur lieten zowel de meta-analyse van Fu (2020) (SMD<0,2) (geen subgroepanalyse voor intraoperatieve muziek) als een recente trial (verschil tussen de groepen < 0,5 dag) geen klinisch relevant verschil zien. De bewijskracht van deze belangrijke uitkomsten was zeer laag. Voor delier en slaapkwaliteit werden geen resultaten gerapporteerd.
Bewijskracht
De bewijskracht voor de cruciale en belangrijke uitkomsten was in alle gevallen zeer laag. Er werd onder andere afgewaardeerd vanwege het risico op bias (onder andere het onvolledig rapporteren van de methodologie en onvolledige blindering), indirectheid (omdat de populatie niet geheel overeenkwam met onze criteria, of omdat de uitkomstmaat cortisol werd gebruikt), heterogeniteit, het kleine aantal geïncludeerde patiënten en/of publicatiebias.
Het grootste punt van kritiek op deze studies is de heterogeniteit van de studies, de kleine populaties die onderzocht zijn en de matige kwaliteit van enkele studies, wat het lastig maakt om algehele, sterke aanbevelingen te doen. De hoge mate van heterogeniteit die in vrijwel alle onderzoeken wordt gevonden kan worden verklaard door de verschillende populaties, ingrepen en muziekinterventies die zijn onderzocht. Hoewel heterogeniteit in klinisch onderzoek over het algemeen niet gewenst is, kan het in dit geval ook worden vertaald naar een brede toepassing voor deze eenvoudige interventie.
Op basis van de gerapporteerde resultaten kan in algemene zin geconcludeerd worden dat muziek mogelijk een positieve uitwerking zou kunnen hebben op de patiënt tijdens het intraoperatieve proces aangaande angst. Daarnaast zijn er geen aanwijzingen dat het aanbieden van muziek nadelige effecten heeft op patiënten, wat strookt met het geneeskundige grondbeginsel ‘primair niet schaden’.
Waarden en voorkeuren van patiënten (en eventueel hun verzorgers)
Het belangrijkste doel van luisteren naar muziek rondom de operatie is de verbetering van het zorgproces voor de patiënt die wordt geopereerd, zodat de ervaring met de zorg verbetert en het herstel bespoedigd wordt. Manieren om dit te meten zijn bijvoorbeeld het reduceren van angst en/of pijn, de hoeveelheid medicatie die wordt gebruikt (analgetica of sedativa) of parameters van de stressreactie van het lichaam (zoals fysiologische parameters (hartslag, bloeddruk) of cortisol) rond een operatie. Het optimaliseren van slaapkwaliteit is een voorbeeld van een uitkomst die helpt in een voorspoedig herstel.
Op de preoperatieve polikliniek, of in de preoperatieve informatiefolder, kan de patiënt worden gewezen op de mogelijkheden van het luisteren naar muziek en kan de patiënt geïnformeerd worden hoe het luisteren naar muziek praktisch gezien in zijn werk gaat. De toepassing van muziek in het ziekenhuis vereist beperkte kennis en vaardigheden. Een klein deel van de patiënten, voornamelijk de oudere patiënt, zal hulp nodig hebben bij het gebruik van de muziekapparatuur. Ten aanzien van de soort muziek wordt de voorkeursmuziek van de patiënt aangehouden. Dit kunnen voor de patiënt specifieke muziekstukken zijn, maar er kan ook op basis van genre worden gekozen. Het meest praktische is dat patiënten zelf het volume van de muziek instellen, eventueel kan een volumebegrenzer helpen. Belangrijk is om het volume niet te luid in te stellen, mede vanwege de tijdelijke paralyse van de musculus stapedius bij het in werking treden van algehele anesthesie. Overigens is er ook een groep van patiënten die niet van muziek houdt en hier perioperatief dan ook geen behoefte aan zal hebben. Vanzelfsprekend blijft dit dan achterwege.
Kosten (middelenbeslag)
Er zijn tot op heden geen kosteneffectiviteitsstudies uitgevoerd naar het toepassen van muziek tijdens het perioperatieve proces. Gezien het werkingsmechanisme van muziek zou de kosteneffectiviteit kunnen voortkomen uit de vermindering van angst en pijn rondom de operatie. Hierdoor zou het gebruik van anxiolytica en analgetica kunnen afnemen. Een afname van angst en pijn kan ook leiden tot verkorte opnameduur, en daarmee een daling in complicaties en het risico op delier (voornamelijk maar niet uitsluitend bij de oudere patiëntenpopulatie). De grootte van dit effect, en de eventuele kostenbesparing die hiermee gepaard gaat, zal berekend moeten worden in kosteneffectiviteitsstudies.
Qua mogelijke uitgaven kan er worden gedacht aan eenmalige kosten van aanschaf van apparatuur om muziek af te spelen of op te beluisteren, eventuele abonnementskosten voor online streamingdiensten om muziek af te spelen (met name voor patiënten die dit zelf niet mee hebben), en indien nodig werktijd van zorgprofessionals om te ondersteunen in het afspelen van de muziek. De ervaring uit diverse RCT’s en implementatietrajecten is dat de meeste patiënten hun eigen muziekdrager met hoofdtelefoon of oortelefoon (‘oortjes’) meenemen met eigen muziek. Veel ziekenhuizen hebben al tablets met een hoofd- of oortelefoon in huis.
Aanvaardbaarheid, haalbaarheid en implementatie
In het kader van de procesevaluatie zijn er een aantal verschillende implementatiestudies uitgevoerd naar (perioperatieve) muziekinterventies, waaronder ook een Nederlandse pilot implementatiestudie. De resultaten van deze studie zijn nog niet gepubliceerd, wel is het studieprotocol beschikbaar (Kakar, 2021). Het gaat om een studie uitgevoerd in een Nederlands ziekenhuis waarbij gestreefd werd tenminste 100 patiënten te includeren die een operatie ondergingen wegens een chronische darmontsteking (IBD) of colorectaal carcinoom. De eerste resultaten van deze studie laten zien dat 75% van de patiënten met een op-maat-gemaakte strategie de muziek aangeboden kreeg door zorgprofessionals op verschillende levels (polikliniek, verpleegafdeling). 72% van de patiënten die muziek aangeboden kreeg heeft hier gebruik van gemaakt. Er werden weinig potentiële bezwaren geregistreerd ten aanzien van de muziekinterventie, wel werd benadrukt dat het belangrijk is de voorkeursmuziek van de patiënt te gebruiken.
In de praktijk zal de voornaamste belasting die de intraoperatieve interventie met zich meebrengt liggen bij de anesthesiemedewerker. Het is daarom met name van belang om de anesthesiemedewerkers te informeren over de aanbeveling betreffende perioperatieve muziek en vaardigheden in het ondersteunen bij het luisteren naar muziek te trainen. Deze training kan gekoppeld worden aan bestaande bij- en nascholingsprogramma’s.
Uit de studie bleek verder dat 28% van de patiënten geen behoefte had aan de interventie. Hierbij is niet verder gevraagd naar de reden, mogelijk zouden ze beter geïnformeerd kunnen worden ten aanzien van de voordelen van het luisteren naar muziek, hoewel het luisteren naar muziek in de perioperatieve setting anders is dan op de polikliniek. Morele en ethische bezwaren zijn niet van toepassing bij deze interventie.
In de pilot implementatie studie werd een inschatting gemaakt van de mate van belasting voor zorgverleners. De voornaamste belasting werd ingeschat op tijd en impact op werkzaamheden van verpleegkundigen die de patiënt in de apparatuur voorzien, en de totale belasting werd laag ingeschat. Zie voor toepassing Figuur 1 (Kühlmann, 2019).
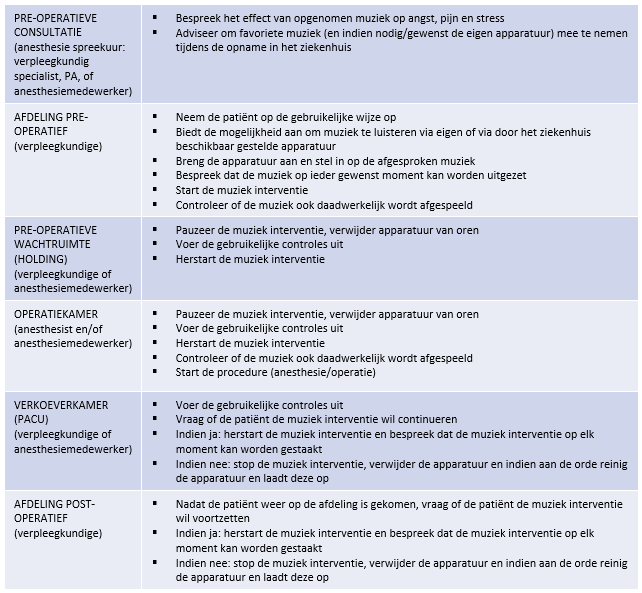
Figuur 1: Werkwijze voor het aanbieden van het luisteren naar muziek tijdens het perioperatieve proces
Deze richtlijnmodule heeft alleen betrekking op patiënten die klinisch worden geopereerd. Het luisteren naar muziek kan worden gestart op de verpleegafdeling en de patiënt kan met de muziekapparatuur en gekozen muziek naar de holding worden vervoerd. Muziek kan vervolgens gedurende de gehele operatie worden aangeboden. In de studies die geïncludeerd zijn in de literatuursamenvatting voor intraoperatieve muziek hebben patiënten doorgaans gedurende de hele operatie naar muziek geluisterd. Het is niet duidelijk wat de optimale duur is voor het aanbieden van muziek, maar om toch een handvat te kunnen geven is ervoor gekozen om aan te houden wat in de geïncludeerde studies het vaakst is gebruikt. Op bepaalde momenten zal de muziek onderbroken moeten worden, om goede communicatie met patiënt en zorgverleners toe te staan, bijvoorbeeld tijdens overdrachten en veiligheidsprocedures (time-out procedure etc.).
Rationale van de aanbeveling: weging van argumenten voor en tegen intraoperatieve muziek
Gezien de zeer lage bewijskracht kan de werkgroep op basis van het beschikbare bewijs geen aanbeveling doen voor het aanbieden van intraoperatieve muziek. Ook op basis van de overige overwegingen slaat de balans niet duidelijk uit in het voordeel van het aanbieden van muziek, aangezien hieraan ook kosten zijn verbonden in de vorm van mogelijke aanschaf en onderhoud van apparatuur, en tijd van het zorgpersoneel om het luisteren naar muziek met de patiënt te bespreken en de patiënt zonodig te ondersteunen bij het luisteren naar muziek. Mocht een patiënt aangeven naar muziek te willen luisteren dan kan besproken worden of en hoe dit gefaciliteerd kan worden.
Onderbouwing
Achtergrond
Veel patiënten die een operatie moeten ondergaan in het ziekenhuis krijgen te maken met angst, stress en pijn. Niet alleen leidt dit tot vervelende ervaringen voor de patiënt, ook kunnen deze factoren het herstel van patiënten na een operatie nadelig beïnvloeden. Het ervaren van angst en stress vóór een operatie kan leiden tot een toename van pijn na de operatie. Luisteren naar muziek rondom het gehele perioperatieve proces (zowel pre-, intra- of post-, alsook een combinatie) kan mogelijk leiden tot een significante vermindering van angst en pijn bij de patiënt. Het luisteren naar muziek activeert het limbische systeem in de hersenen, waardoor er verschillende hormonen zoals serotonine en endogene opioïden vrijkomen, wat leidt tot een vermindering van angst en pijn. Neurofysiologisch onderzoek en fMRI scans laten een verbeterde voortgeleiding van impulsen zien in de hersenen onder invloed van muziek. Ook neemt de activiteit van de sympathicus af waardoor fysiologische symptomen van stress verminderen (denk aan een rustigere hartslag, lagere bloeddruk). Muziek is breed toegankelijk en goedkoop, is duurzaam, mogelijk kostenbesparend en komt daarmee mogelijk het welzijn van de patiënt ten goede.
Deze richtlijn bestaat uit vier verschillende modules. In elke aparte module wordt besproken of preoperatieve, dan wel intraoperatieve, dan wel postoperatieve, dan wel perioperatieve muziek bij volwassen patiënten die geopereerd worden in het ziekenhuis, leidt tot positieve uitkomsten voor de patiënt. Goed is te weten dat deze richtlijn gaat over het luisteren naar opgenomen muziek en niet over muziektherapie. Bij muziektherapie wordt muziek aangeboden door een muziektherapeut, waarbij de werkwijze afgestemd wordt op de individuele patiënt. Het is hierbij niet mogelijk om het effect van de muziek alleen te evalueren, omdat er mogelijk ook een effect is van de interactie tussen de muziektherapeut en de patiënt. Tot slot, de richtlijn gaat ook niet over live muziek aangezien over deze vorm van het aanbieden van muziek vrijwel geen literatuur beschikbaar is.
Deze module betreft intraoperatieve muziek.
Conclusies / Summary of Findings
None of the included studies reported on the effect of live music, therefore no conclusions can be drawn about the effect of live music on the selected outcomes.
Pain (crucial outcome)
|
Very low GRADE |
The evidence is very uncertain about the effect of recorded music in the intraoperative setting on pain when compared with no music in patients undergoing invasive surgery.
Sources: (Kühlmann, 2018; Kurdi, 2018; Tran, 2020; Kavakli, 2019; Gökçek, 2020; Kahloul, 2017) |
Anxiety (crucial outcome)
|
Very low GRADE |
The evidence is very uncertain about the effect of recorded music in the intraoperative setting on anxiety when compared with no music in patients undergoing invasive surgery.
Sources: (Kühlmann, 2018; Choubsaz, 2018; Kurdi, 2018; Kukreja, 2020; Kavakli 2019) |
Medication use (analgesics and hypnotics) (crucial outcome)
|
Very low GRADE |
The evidence is very uncertain about the effect of recorded music in the intraoperative setting on medication use (analgesics and hypnotics) when compared with no music in patients undergoing invasive surgery.
Sources: (Fu, 2020; Kurdi, 2018; Tran, 2020; Kavakli 2019; Kukreja, 2020) |
Stress (important outcome)
|
Very low GRADE |
The evidence is very uncertain about the effect of recorded music in the intraoperative setting on cortisol levels when compared with no music in patients undergoing invasive surgery.
Sources: (Fu, 2019) |
Patient satisfaction (important outcome)
|
Very low GRADE |
The evidence is very uncertain about the effect of recorded music in the intraoperative setting on patient satisfaction when compared with no music in patients undergoing invasive surgery.
Sources: (Kavakli, 2019; Gökçek, 2020; Kahloul, 2017) |
Length of stay (important outcome)
|
Very low GRADE |
The evidence is very uncertain about the effect of recorded music in the intraoperative setting on length of stay when compared with no music in patients undergoing invasive surgery.
Sources: (Fu, 2020; Kavakli, 2019) |
Delirium, sleep disturbance/sleep quality
|
- GRADE |
No evidence (systematic reviews or RCTs) was found regarding the effect of intraoperative music on delirium and sleep disturbance/sleep quality when compared with no music in patients undergoing invasive surgery. |
Samenvatting literatuur
Description of studies
The three systematic reviews and meta-analyses included studies evaluating the effectiveness of intraoperative music on anxiety and/or pain (Kühlmann, 2018), the physiological stress response (Fu, 2019), medication requirement, and hospital length of stay (Fu, 2020). The seven recent RCTs (Choubsaz, 2018; Kurdi, 2018; Kukreja, 2020; Tran, 2020; Kavakli, 2019; Gökçek, 2020; Kahloul, 2017) assessed the effects of intraoperative music on pain, anxiety, medication use, patient satisfaction, and length of stay.
Kühlmann (2018) included RCTs investigating the effect of music interventions on anxiety and pain during invasive surgery. Studies were included in the meta-analysis only if they included measures of dispersion of a particular outcome. For anxiety, 16 RCTs reported on music interventions in the intraoperative setting and 10 of these RCTs were included in the meta-analysis. For pain, 14 RCTs reported on music interventions in the intraoperative setting and 10 of these RCTs were included in the meta-analysis (see Table 2.3).
In total, this review included 21 RCTs evaluating the effectiveness of music on anxiety and/or pain in the intraoperative setting, 6 under general and 15 under regional anesthesia (in two of these studies regional anesthesia and sedation were used). Studies reporting on music in the intraoperative setting were conducted in North America (n=8), Asia (n=9), and Europe (n=4). Patients in these studies underwent a wide variety of invasive types of surgery, some outside the scope of this guideline, such as catheter placement. All studies used recorded music, not necessarily through headphones. The duration of the intervention was often not reported. Different music genres were used, the research team often selected classical, relaxing and/or slow music, while in some studies patients chose their favorite music genre. Patients in the control group received no intervention, standard care (in one study with verbal distraction), headphones with a blank CD or no music, or ambient operating room sounds.
Fu (2019) included RCTs investigating the effect of preoperative, intraoperative and/or postoperative music on the stress response to surgery. Studies were excluded from the meta-analysis if the presented data were not suitable, if the stress response biomarkers differed significantly between the music and control group at baseline preoperatively, or if no preoperative baseline and only postoperative stress levels were presented. Eighteen RCTs were included, of which six RCTs compared the effect of a music intervention in the intraoperative setting on the physiological stress response, as compared with no music (see Table 3.4).
Of these six RCTs, two used general anesthesia, three used regional anesthesia, and one used local anesthesia. Studies were performed in North America (n=1), Asia (n=3), and Europe (n=2). Patients underwent a variety of invasive types of surgery. One study included patients undergoing port catheter placement under local anesthesia which is outside the scope of this guideline. Patients in the intervention group listened to different genres of recorded music, including jazz, classical and new age music, usually for the duration of the procedure. Patients in the control group received standard care or headphones without music.
Fu (2020) included RCTs that evaluated the effect of preoperative, intraoperative and/or postoperative music on medication requirement or length of stay. Out of 55 included RCTs, 13 RCTs reported the effect of music in the intraoperative setting on medication. Three out of these 13 RCTs also reported hospital or PACU length of stay (see Table 3.5).
Of these 13 RCTs, eight used general anesthesia (one with spinal or epidural), three used regional anesthesia, one used epidural, spinal and local anesthesia, and one used propofol patient-controlled sedation with local infiltration. Studies were performed in North America (n=4), Asia (n=4), and Europe (n=5) and included patients undergoing a diverse range of surgical procedures. Patients in the intervention group listened to different genres of recorded music, including jazz, classical and new age music, usually for the duration of the procedure. Patients in the control group received standard care, (occlusive) headphones without music, headphones with operation noise, or white music.
Out of the seven recent RCTs evaluating the effect of intraoperative music, five included patients undergoing surgery under regional anesthesia (Choubsaz, 2018; Kurdi, 2018; Kukreja, 2020; Tran, 2020; Kavakli, 2019) and two included patients undergoing surgery under general anesthesia (Gökçek, 2020; Kahloul, 2017) (see Table 3.6). Studies were performed in North America (n=2), Asia (n=4), and Africa (n=1). Surgery under regional anesthesia included an elective or emergency caesarean section, total knee arthroplasty (TKA), or carotid endarterectomy. Surgery under general anesthesia included septorhinoplasty and abdominal surgery. Patients listened to various music genres, including soothing, sedative, classical, rock or popular music, usually for the duration of surgery. Patients in the control groups received standard care, no intervention, noise reducing ear plugs or headphones, or headphones with OR noise.
Results
Pain
The review by Kühlmann (2018) included 13 RCTs that evaluated the effect of intraoperative music on pain. A meta-analysis of ten of these RCTs showed that the pooled standardized mean difference was -0.18 (95% CI -0.36 to 0.00); p=0.050, I2=44.
Five out of seven recent RCTs assessed pain (Kurdi, 2018; Tran, 2020; Kavakli, 2019; Gökçek, 2020; and Kahloul, 2017). Tran (2020) used an NRS and reported medians and IQRs, the other four studies used a VAS and reported means and SDs. These four studies were included in a meta-analysis. Three of these studies used a VAS with a range 0 to 10, the study of Kahloul (2017) used a VAS with a range 0 to 100 which was transformed to a range 0 to 10. The first postoperative pain measurement (1 hour postoperatively, postoperative in the PACU, postoperative during recovery or on waking) was selected. The pooled mean difference in pain scores between the groups was -0.42 (95%CI -1.08 to 0.24; p=0.21).
Figure 2.1 Forest plot of pain in the music and control groups (intraoperative setting)
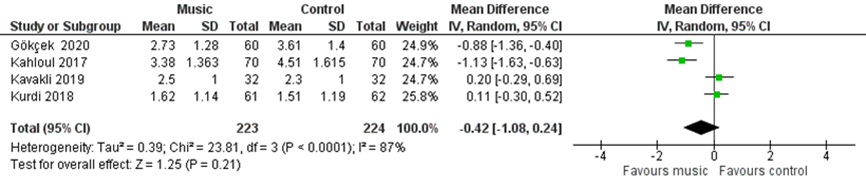
The study of Tran (2020) reported average pain scores over a 24-hour time period, median pain scores on the NRS were 1.6 (IQR 0.79 to 3.5) in the intervention group and 2.4 (IQR 0.72 to 4.5) in the control group (p=0.47). Kurdi (2018) also assessed pain 6 and 24 hours postoperatively. Six hours postoperatively, mean pain scores were 3.22 (SD 1.26) in the intervention group and 4.41 (SD 3.68) in the control group (p=0.042). Twenty-four hours postoperatively, mean pain scores were 0.93 (SD 0.83) in the intervention group and 2.41 (SD 1.28) in the control group (p=0.025). Kavakli (2019) also assessed pain intraoperatively using a VAS, mean scores were 2.4 (SD 0.8) in the intervention group and 2.5 (SD 1) in the control group (p=0.586).
Anxiety
The review by Kühlmann (2018) included 13 studies that evaluated the effect of intraoperative music on anxiety. A meta-analysis of ten of these RCTs showed that the pooled standardized mean difference was -0.57 (95% CI -1.06 to -0.09); p=0.020, I2=92.
Four recent RCTs, all involving surgery under regional anesthesia, assessed anxiety (Choubsaz, 2018; Kurdi, 2018; Kukreja, 2020; Kavakli, 2019). Kurdi (2018) used a VAS, the other three studies used the State-Trait Anxiety Inventory (STAI). Anxiety was assessed intraoperatively and postoperatively (not defined or 1,6, and 24 hours postoperatively).
A meta-analysis of postoperative anxiety scores was performed and because different scales were used to assess anxiety, a standardized mean difference was computed. The two control arms from Choubsaz (2018) were combined into one control arm. The pooled standardized mean difference was -0.82 (95% CI -1.58 to -0.06); p=0.03, I2=90%. To facilitate interpretation of the effect size, the standardized mean difference was back-transformed, demonstrating that STAI state anxiety scores (range 20 to 80) were -9.7 lower for patients in the music group as compared with the control group.
Figure 2.2 Forest plot of anxiety in the music and control groups (intraoperative setting)
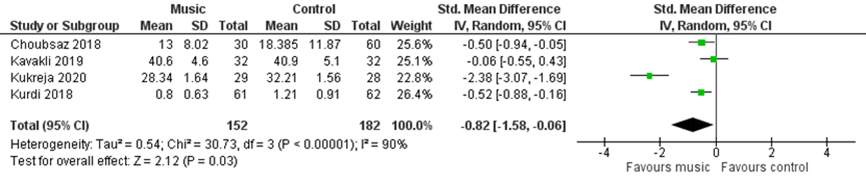
Kurdi (2018) also assessed anxiety 6 and 24 hours postoperatively. Six hours postoperatively, mean anxiety scores were 2.16 (SD 1.26) in the intervention group and 3.59 (SD 1.42) in the control group (p=0.012). Twenty-four hours postoperatively, mean pain scores were 0.62 (SD 0.82) in the intervention group and 1.83 (SD 0.91) in the control group (p=0.015). Kavakli (2019) also assessed anxiety repeatedly during surgery using two questions from the STAI ‘are you calm? ’ and ‘are you relaxed?’. These questions have been shown to be correlated with the full STAI questionnaire. Median scores for the question ‘are you calm?’ were 2 (IQR 2 to 3.75) in the intervention group and 4 (IQR 3 to 4) in the control group (p=0.0001). For the question ‘are you relaxed?’, median scores were 2 (IQR 2 to 4) in the intervention group and 4 (IQR 3 to 4) in the control group (p=0.0001). Kavakli (2019) also assessed anxiety immediately after the end of surgery using an NRS, mean scores were 5.5 (SD 1.9) in the intervention group and 3.4 (SD 1.3) in the control group (p=0.001).
Medication use (analgesics and hypnotics)
The review by Fu (2020) included 13 RCTs that evaluated the effect of intraoperative music on analgesics and/or hypnotics. For analgesics, results included the effect of intraoperative music on postoperative opioid requirement (n=6), intraoperative opioid requirement (n=1), and intraoperative fentanyl requirement (n=2). For hypnotics, results included the effect of intraoperative music on intraoperative propofol requirement (n=5), intraoperative end-tidal isoflurane (n=1) and intraoperative end-tidal sevoflurane (n=1).
A meta-analysis was performed for the effect of preoperative, intraoperative, and/or postoperative music on postoperative opioid requirement, propofol, and midazolam. Results should be interpreted with caution because no subgroup analysis was performed for music in the intraoperative setting alone.
For postoperative opioid requirement, a meta-analysis of 20 RCTs (including six RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of -0.31 (95% CI -0.45 to -0.16); p<0.001, I2=44.3. The forest plot provided in the review demonstrated inconsistency, with several studies showing a lower postoperative opioid requirement in the music group, but also a number of studies showing no difference between the groups, and a few studies showing a lower postoperative opioid requirement in the control group.
For propofol, a meta-analysis of nine RCTs (including three RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of -0.72 (95% CI -1.01 to -0.43); p=0.00001, I2=61.1.
For midazolam, a meta-analysis of three RCTs (including one RCT using music in the intraoperative setting) showed a pooled standardized mean difference of -1.07 (95% CI -1.70 to -0.44); p<0.001, I2=73.1.
Four recent RCTs, all involving surgery under regional anesthesia, evaluated the effect of intraoperative music on analgesics (Kurdi, 2018; Tran, 2020; Kavakli, 2019) and/or hypnotics (Kukreja, 2020; Tran, 2020).
For analgesics, Kurdi (2018) showed that the mean time required for first rescue analgesic was 133.7 minutes (SD 99.78) in the intervention group and 136.58 minutes (SD 68.88) in the control group (p=0.031). Tran (2020) showed that 24-h opioid consumption was on average 20.8 MME (SD 18.8) in the intervention group, while the median 24-h opioid consumption was 18.3 (IQR 7.5 to 43.1) in the control group (p=0.58). Kavakli (2019) showed that the volume of supplemental lidocaine 1% (mL) was 1.4 (SD 2.5) in the intervention group and 1.8 (SD 2.8) in the control group (p=0.552). In addition, patients in the intervention group received a mean dose of 9.3 μg (SD 26.7) intraoperative fentanyl, compared with 7.8 μg (SD 22.3) in the control group (p=0.801). The time to first analgesic requirement in the PACU was 107 minutes (SD 22) in the intervention group and 116 minutes (SD 28) in the control group (p=0.175). Mean postoperative tramadol consumption was 17.1 mg (SD 31.3) in the intervention group and 19.5 (SD 33.4) in the control group.
For hypnotics, Kukreja (2020) showed that the mean propofol dose was 0.06 mg/min/kg (SD 0.004) in the intervention group and 0.05 mg/min/kg (SD 0.004) in the control group (p=0.264). In the study of Tran (2020), mean propofol usage was 3.5 μg/kg/min (SD 8.9) in the intervention group and 5.1 μg/kg/min (SD 8.7) in the control group (p=0.10).
Stress
The review by Fu (2019) included six RCTs that evaluated the effect of intraoperative music on the physiological stress response. A meta-analysis was performed for the effect of preoperative, intraoperative, and/or postoperative music on cortisol levels. Results should be interpreted with caution because no subgroup analysis was performed for music in the intraoperative setting alone.
A meta-analysis of five RCTs reporting cortisol levels at the end of surgery (including three RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of –0.14 (95% CI -0.57 to 0.28); p=0.50, I2=60.15.
A meta-analysis of six RCTs reporting cortisol levels postoperatively (including three RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of –0.30 (95% CI -0.53 to -0.07); p=0.01, I2=0.
None of the recent RCTs reported on the effect of intraoperative music on stress.
Patient satisfaction
None of the systematic reviews reported on the effect of intraoperative music on patient satisfaction.
Three recent RCTs reported patient satisfaction, one RCT involved surgery under regional anesthesia (Kavakli, 2019) and two RCTs involved surgery under general anesthesia (Gökçek, 2020; Kahloul, 2017). In the study of Kavakli (2019), patients who had undergone carotid endarterectomy reported a median satisfaction score of 3 (IQR 3 to 4), in both the intervention and control groups. Gökçek (2020) reported satisfaction rates of 73.3% in the intervention group and 36.3% in the control group (p<0.001). Kahloul (2017) showed satisfaction rates of 81.4% in the intervention group and 51.4% in the control group (p<0.0001). In both of these RCTs (Gökçek, 2020; Kahloul, 2017) patient satisfaction was assessed using the EVAN-G questionnaire, which is designed to provide a score ranging from 0 (worst possible level of satisfaction) to 100 (best possible level of satisfaction), and it is unclear how these scores were transformed into satisfaction rates.
Length of stay
The review by Fu (2020) included three RCTs that evaluated the effect of intraoperative music on PACU or hospital length of stay. A meta-analysis was performed for the effect of preoperative, intraoperative, and/or postoperative music on length of stay. Results should be interpreted with caution because no subgroup analysis was performed for music in the intraoperative setting alone.
A meta-analysis of nine RCTs (including two RCTs using music in the intraoperative setting, both reporting on PACU length of stay) showed a pooled standardized mean difference of –0.18 (95% CI -0.43 to 0.067); p=0.15, I2=56.0.
Kavakli (2019) reported that mean length of stay in the PACU was 139 minutes (SD 20) in the intervention group, compared with 149 minutes (SD 23) in the control group (p=0.112). Total length of hospital stay was 2.8 days (SD 0.7) in the intervention group and 3 (SD 0.8) in the control group (p=0.269).
Delirium, sleep disturbance/sleep quality
None of the three systematic reviews or seven recent RCTs reported on these outcomes of music in the intraoperative setting.
Level of evidence of the literature
All evidence was derived from randomized controlled trials, therefore, the level of evidence for all outcomes started at ‘high quality’.
The level of evidence regarding the outcome measure pain was downgraded by three levels because of study limitations (-1; risk of bias because randomization procedure was inadequate, lack of blinding, and incomplete reporting of study methodology); conflicting results (-1; inconsistency); and applicability (-1; bias due to indirectness because many of the RCTs in the review by Kühlmann that reported on pain involved procedures outside of the scope of this guideline).
The level of evidence regarding the outcome measure anxiety was downgraded by three levels because of study limitations (-1; risk of bias for lack of blinding, loss to follow-up, and incomplete reporting of study methodology); applicability (-1; bias due to indirectness because many of the RCTs in the review by Kühlmann that reported on anxiety involved procedures outside of the scope of this guideline); imprecision (-1; the confidence intervals of both meta-analyses include the option that there is no clinically relevant effect);
and publication bias (-1; the funnel plot in the review by Kühlmann 2018 raised the possibility of publication bias).
The level of evidence regarding the outcome measure medication use (analgesics/hypnotics) was downgraded by three levels because of study limitations (-1; risk of bias for lack of blinding, potentially selective outcome reporting, and incomplete reporting of study methodology); inconsistency (-1; for heterogeneity); applicability (-1; bias due to indirectness because of different timing of the music intervention); and publication bias (-1 as the funnel plot in the review by Fu 2020 raised the possibility of publication bias).
The level of evidence regarding the outcome measure stress was downgraded by three levels because of study limitations (-1; risk of bias because of lack of blinding and incomplete reporting of study methodology); conflicting results (-1; inconsistency); and applicability (-1 ; bias due to indirectness of the outcome cortisol).
The level of evidence regarding the outcome measure patient satisfaction was downgraded by three levels because of study limitations (-2; risk of bias because of inadequate randomization procedure or lack of reporting of randomization and allocation procedure, lack of blinding, unclear reporting of patient satisfaction data); and imprecision (-1 for low number of included patients).
The level of evidence regarding the outcome measure length of stay was downgraded by three levels because of study limitations (-1; risk of bias because of lack of blinding and incomplete reporting of study methodology); conflicting results (-1; inconsistency); and imprecision (-1 for low number of included patients).
The level of evidence regarding the outcome measures delirium and sleep disturbance/sleep quality could not be assessed because none of the included studies reported these outcomes.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question: ‘What are the effects of music in the intraoperative setting on patients undergoing invasive surgery with anaesthesia care when compared to no music?’
P: patients undergoing invasive surgery with anaesthesia care (general anaesthesia, regional anaesthesia, or both);
I: intraoperative music through headphones;
C: no music (no active intervention);
O: pain, anxiety, medication use (analgesics and hypnotics), stress, delirium, sleep disturbance/sleep quality, patient satisfaction, length of stay.
Relevant outcome measures
The guideline development group, although aware that there are many different goals which are aspired in music interventions, considered pain, anxiety and medication use (analgesics and hypnotics) as critical outcome measures for decision making; and stress, delirium, sleep disturbance/sleep quality, patient satisfaction and length of stay as important outcome measures for decision making.
A priori, the working group did not define the outcome measures listed above but used the definitions used in the studies. Outcomes had to be assessed using validated instruments. The outcome stress could be assessed using patient reported outcomes or cortisol levels.
- Pain: The working group defined 12 mm on a Visual Analogue Scale as a minimal clinically (patient) important difference.
- Anxiety: The working group defined 12 mm on a Visual Analogue Scale as a minimal clinically (patient) important difference.
- Stress: the working group defined a difference equal to 0.5 standard deviation between the groups as a minimal clinically (patient) important difference.
- Delirium: The working group defined 1 point on the DOS (Delirium Observatie Screening) as a minimal clinically (patient) important difference.
- Patient satisfaction: the working group defined a difference of 10% as a minimal clinically (patient) important difference.
- Length of stay: The working group defined 0.5 days as a minimal clinically (patient) important difference.
If studies reported a standardized mean difference, a difference >0.2 between the groups was considered as a minimal clinically (patient) important difference (Cohen, 1988).
Search and select (Methods)
Three systematic reviews were suggested by members of the guideline working group. This included a systematic review and meta-analysis by Kühlmann (2018) about the effect of perioperative music interventions on anxiety and pain in surgery, a systematic review and meta-analysis by Fu (2019) about the effect of perioperative music on the physiological stress response to surgery, and a systematic review and meta-analysis by Fu (2020) about the effect of perioperative music on medication requirement and hospital length of stay. The working group decided to use these reviews as a starting point and perform an update of the search to identify recent publications. Although the searches by Fu were conducted more recently (2019), the search conducted by Kühlmann (2018) on 20 October 2016 was more sensitive as it was not limited to studies reporting on specific outcomes (stress response, medication, length of stay).
The databases Embase (through Embase.com), Medline (through OVID), and PsycInfo (through OVID) were searched with relevant search terms from 1 January 2016 until 23 November 2020 for the question regarding the effects of perioperative music on patients undergoing invasive surgery with anaesthesia care. The search was limited to systematic reviews and randomized controlled trials. The detailed search strategy is depicted under the tab Methods. The systematic literature search resulted in 472 hits.
Studies were selected based on the following criteria:
(1) systematic review or randomized controlled trial;
(2) full-text English language publication;
(3) adult patients;
(4) invasive surgery with general anaesthesia, regional anaesthesia or both;
(5) music intervention having melody, harmony and rhythm;
(6) patients listened to intraoperative music through headphones;
(7) the intervention should only involve listening to music and no active participation such as patients making music or singing along;
(8) outcomes were assessed using a validated method.
180 studies were initially selected based on title and abstract screening. After reading the full text, 173 studies were excluded (see the table with reasons for exclusion under the tab Methods) and 7 randomized controlled trials were included.
Results
The three systematic reviews by Kühlmann (2018), Fu (2019) and Fu (2020) (including 92, 18, and 55 RCTs) are summarized in the evidence tables. This guideline consists of four parts, based on the timing of the music intervention (preoperative/ intraoperative/ postoperative/ multiple times). Studies included in the three reviews are presented in the relevant part of the guideline, for example 21/92 RCTs included in the review by Kühlmann (2018) evaluated an intraoperative music intervention. These 21 studies are summarized in Table 3.3. The quality assessment of the systematic reviews is summarized in Table 3.8.
The update of the search identified seven RCTs that were published from 2016 and were not included in the reviews by Kühlmann (2018), Fu (2019) or Fu (2020). Important study characteristics and results are summarized in the evidence tables. and the assessment of the risk of bias for the RCTs is summarized in the risk of bias tables (Table 3.7).
Referenties
- Fu VX, Oomens P, Sneiders D, van den Berg SAA, Feelders RA, Wijnhoven BPL, Jeekel J. The Effect of Perioperative Music on the Stress Response to Surgery: A Meta-analysis. J Surg Res. 2019 Dec;244:444-455. doi: 10.1016/j.jss.2019.06.052. Epub 2019 Jul 18. PMID: 31326711.
- Fu VX, Oomens P, Klimek M, Verhofstad MHJ, Jeekel J. The Effect of Perioperative Music on Medication Requirement and Hospital Length of Stay: A Meta-analysis. Ann Surg. 2020 Dec;272(6):961-972. doi: 10.1097/SLA.0000000000003506. PMID: 31356272; PMCID: PMC7668322.
- Kühlmann AYR, de Rooij A, Kroese LF, van Dijk M, Hunink MGM, Jeekel J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br J Surg. 2018 Jun;105(7):773-783. doi: 10.1002/bjs.10853. Epub 2018 Apr 17. PMID: 29665028; PMCID: PMC6175460.
- Choubsaz M, Rezavand N, Bayat A, Farhadi K, Amirifard N. Comparison between the effect of ear plug and music in reducing anxiety in patients undergoing elective cesarean section under spinal anesthesia. Kuwait Med J. 2018; 50(1): 37-42.
- Gökçek E, Kaydu A. The effects of music therapy in patients undergoing septorhinoplasty surgery under general anesthesia. Braz J Otorhinolaryngol. 2020 Jul-Aug;86(4):419-426. doi: 10.1016/j.bjorl.2019.01.008. Epub 2019 Mar 5. PMID: 31523022.
- Kahloul M, Mhamdi S, Nakhli MS, Sfeyhi AN, Azzaza M, Chaouch A, Naija W. Effects of music therapy under general anesthesia in patients undergoing abdominal surgery. Libyan J Med. 2017 Dec;12(1):1260886. doi: 10.1080/19932820.2017.1260886. PMID: 28452603; PMCID: PMC5328375.
- Kavakli AS, Kavrut Ozturk N, Yavuzel Adas H, Kudsioglu ST, Ayoglu RU, Özmen S, Sagdic K, Yapici N. The effects of music on anxiety and pain in patients during carotid endarterectomy under regional anesthesia: A randomized controlled trial. Complement Ther Med. 2019 Jun;44:94-101. doi: 10.1016/j.ctim.2019.04.005. Epub 2019 Apr 5. PMID: 31126582.
- Kukreja P, Talbott K, MacBeth L, Ghanem E, Sturdivant AB, Woods A, Potter WA, Kalagara H. Effects of Music Therapy During Total Knee Arthroplasty Under Spinal Anesthesia: A Prospective Randomized Controlled Study. Cureus. 2020 Mar 24;12(3):e7396. doi: 10.7759/cureus.7396. PMID: 32337122; PMCID: PMC7179990.
- Kurdi MS, Gasti V. Intraoperative Meditation Music as an Adjunct to Subarachnoid Block for the Improvement of Postoperative Outcomes Following Cesarean Section: A Randomized Placebo-controlled Comparative Study. Anesth Essays Res. 2018 Jul-Sep;12(3):618-624. doi: 10.4103/aer.AER_114_18. PMID: 30283165; PMCID: PMC6157226.
- Tran BW, Nowrouz MY, Dhillon SK, Xie KK, Breslin KM, Golladay GJ. The Impact of Music and Noise-Cancellation on Sedation Requirements During Total Knee Replacement: A Randomized Controlled Trial. Geriatr Orthop Surg Rehabil. 2020 Mar 4;11:2151459320910844. doi: 10.1177/2151459320910844. PMID: 32181048; PMCID: PMC7057404.
- Cohen, J. 1988. Statistical Power Analysis for the Behavioral Sciences, 2nd Edition.
Routledge. - Kakar E, Ista E, Klimek M, Jeekel J. Implementation of music in the perioperative standard care of colorectal surgery: study protocol of the IMPROVE Study. BMJ Open. 2021 Oct 28;11(10):e051878. doi: 10.1136/bmjopen-2021-051878. PMID: 34711596; PMCID: PMC8557300.
- Kühlmann AYR (2019). The Sound of Medicine – Evidence-based music interventions in healthcare practice (ISBN 978-94-6375-451-4 Dissertatie, Erasmus Universiteit Rotterdam). https://www.publicatie-online.nl/publicaties/rosalie-kuhlmann/
Evidence tabellen
Table 3.1 Evidence table for systematic review of RCTs on the effects of music in the intraoperative setting on anxiety and/or pain
|
Study reference |
Study characteristics |
Patient characteristics |
Type of surgery |
Type of anaesthesia |
Intervention
|
Comparison / control |
Anxiety scale and results |
Pain scale and results |
Comments |
|
Kühlmann (2018)
|
Systematic review and meta-analysis of RCTs
Literature search up to 20 October 2016. 92 RCTs were included in the review and 81 in the meta-analysis.
Anxiety 16 RCTs used music in the intraoperative setting and 10 of these RCTs were included in the meta-analysis.
A: Alam, 2016, USA B: Kongsawatvorakul, 2016, Thailand C: Hudson, 2015, UK D: Bae, 2014, South Korea E: Jimenez-Jimenez, 2013, Spain F: Zengin, 2013, Turkey G: Guerrero, 2012, USA H: Wu, 2012, USA I: Kim, 2011, South Korea J: Kang, 2008, South Korea K: Reza, 2007, Iran L: Chang, 2005, Taiwan M: Pongraweewan, 2005, Thailand N: Koch, 1998, USA O: Cruise, 1997, Canada P: Steelman, 1990, USA
Pain 14 RCTs used music in the intraoperative setting and 10 of these RCTs were included in the meta-analysis
A: Alam, 2016, USA B: Kongsawatvorakul, 2016, Thailand C: Hudson, 2015, UK F: Zengin, 2013, Turkey G: Guerrero, 2012, USA I: Kim, 2011, South Korea J: Kang, 2008, South Korea K: Reza, 2007, Iran N: Koch, 1998, USA Q: Şen, 2009, Turkey R: Simcock, 2008, USA S: Szmuk, 2008, USA T: Nilsson, 2003a, Sweden U: Nilsson, 2001, Sweden
Source of funding: This work was funded by Stichting Coolsingel (Rotterdam, The Netherlands) and Stichting Swart-van Essen (Rotterdam, The Netherlands). The funders of the study had no role in the study design, data collection, data analysis, manuscript preparation and publication decision.
Conflicts of interest: M.G.M.H. was supported by ZonMw, the European Institute for Biomedical Imaging Research, European Society of Radiology and Cambridge University Press outside of the submitted work. The authors declare no other conflict of interest.
|
Inclusion criteria SR: -full-text article of an RCT; -investigating effects of music interventions on anxiety and/or pain; -mean age of participants at least 18 years; -written in English; -invasive surgical procedures, either open or laparoscopic, such as abdominal surgery or total knee surgery; -use of general anaesthesia, regional anaesthesia or both; - use of any recorded or live music intervention having melody, harmony and rhythm; - intervention offered by a researcher or a music therapist; - intervention performed in a hospital or outpatient clinic.
Exclusion criteria SR: -studies involving non-invasive procedures such as endoscopy; -studies using quasi- or pseudo-randomization; -nature sounds were considered only when they were used in addition to music;
Important patient characteristics
N, total and per group (music versus no music) A: 105, 54/51 B: 73, 36/37 C: 160, 84/76 D: 80, 40/40 E: 40, 20/20 F: 100, 50/50 G: 101, 54/47 H: 26, 13/13 I: 219, 106/113 J: 40, 20/20 K: 100, 50/50 L: 64, 32/32 M: 44, 22/22 N: 43, 21/22 O: 62, 32/30 P: 43, 21/22 Q: 60, 30/30 R: 30, 15/15 S: 40, 20/20 T: 100, 51/49 U: 58, 30/28
Mean age ± SD or range A: 63.3 B: 42.9 ± 10.8 C: 54.4 ± 12.6 D: 39.2 ± 1.8 E: 43.9 ± 9.0 F: 50.0 ± 15.0 G: 25.1 ± 6.8 H: 25.1 I: (-) J: 68.5 ± 7.2 K: 26.0 ± 5.2 L: 31.3 ± 4.4 M: 43.9 ± 20.8 N: 53.5 ± 13.6 O: 69.6 ± 2.4 P: 23-76 Q: 22.5 ± 3.1 R: 67.3 ± 9.1 S: 52.0 ± 16.0 T: 54.0 ± 13.4 U: 50.5 ± 8.2
Sex (% men) A: 59.5% B: 0% C: 22.5% D: 52.5% E: 30% F: 52% G: 0% H: 0% I: 55.7% J: 10% K: 0% L: 0% M: 57% N: 62% O: 32.5% P: - Q: 100% R: 60% S: 50% T: 69% U: 0% |
A: cutaneous carcinoma face surgery B: large loop excision C: varicose veins D: orthopedic E: elective varicose vein F: catheter placement G: first trimester surgical abortion H: surgical abortion I: surgical third molar extraction J: total knee arthroplasty K: Caesarean section L: Caesarean section M: orthopedic N: lithropsy renal calculi O: cataract P: orthopedic Q: urological R: total knee arthroplasty S: laparoscopic T: varicose vein and inguinal hernia U: hysterectomy
|
A: regional B: regional C: regional D: regional E: regional F: regional G: regional H: regional I: regional J: regional, sedation K: general L: regional M: regional N: regional O: regional, sedation P: regional Q: general R: general S: general T: general U: general
|
Live/recorded music All 16 studies used recorded music
Music genre (duration in minutes) A: standard soothing and nature sounds (30) B: standard slow-rhythm classical (-) C: selection classical, easy listening, pop or online library (-) D: selection CD classical, pop, religious, Korean pop, relaxation (80) E: Henry Gorecki Symphony no. 3 (-) F: standard slow instrument Turkish classical (-) G: Spanish (44%), hip-hop (23%), pop( 11%), rock rap classical jazz easy listening reggae (22%) (-) H: different genres (-) I: self-chosen classical, pop, folk, hymns, Korean style country, own favorites (25) J: folk, popular or classical (98) K: Spanish guitar music (-) L: western classical, new age or Chinese religion (88) M: standard, not specified (-) N: self-brought CD or suitable alternative (-) (43) O: relaxing classical and soothing nature sounds (-) P: classical, new age, instrument, easy listening/ popular, country (-) Q: self-chosen (-) R: selection not specified (-) S: selection of different styles (-) T: soft, slow, flowing, rhythmic instrumental new-age synthesizer (43) U: relaxing music with wave sounds (-)
|
A: headphone no music B: standard care C: treatment as usual D: no treatment E: standard care F: unclear G: routine pain control without headphone H: nothing I: no music J: ambient OR noise K: blank CD with headphones L: routine care M: no adjunct techniques N: no headphone, ambient OR noise O: operating room noise P: routine care, verbal distraction Q: earphones no music R: headphone with white noise S: headphone no music T: blank CD U: operating room sounds
|
Scale A: STAI short version B: STAI C: STAI D: STAI, VAS E: STAI, VAS F: STAI G: STAI H: VRS I: Carah's Dental Anxiety Scale J: VAS K: VAS L: VAS M: VAS N: STAI O: STAI, VAS P: STAI
Results meta-analysis pooled standardized mean difference: -0.57 (95% CI -1.06 to -0.09); p=0.020, I2=92
|
Scale A: VAS B: VAS C: NRS F: VAS G: VAS I: VAS 0-5 J: VAS K: VAS N: VAS Q: VAS R: VAS S: VAS T: NRS U: VAS
Results meta-analysis pooled standardized mean difference: -0.18 (95% CI -0.36 to 0.00); p=0.050, I2=44 |
Authors’ conclusion This meta-analysis found a statistically significant decrease in both anxiety and pain in adults receiving music interventions pre-, intra-, and/or postoperatively.
Selection criteria This review excluded seven studies that generated randomization sequences inadequately
Risk of bias Overall, risk of bias in the included studies was moderate to high. Many studies did not adequately address methodological considerations (randomization techniques and power) and risk of bias, and were therefore scored as having an unclear risk.
Heterogeneity The overall level of heterogeneity was high (I2=92% for anxiety and I2=44% for pain). There was a wide variety of surgical procedures, a variety in control conditions, and diverse methods of anesthesia.
Publication bias The funnel plot for anxiety raises the possibility of publication bias. Previous publications of mainly favourable results might affect the conclusion of this review. |
Abbreviations: STAI: State-Trait Anxiety Inventory; VAS: Visual Analog Scale; VRS: Verbal Rating Scale; NRS: Numerical Rating Scale
Table 3.2 Evidence table for systematic review of RCTs on the effects of music in the intraoperative setting on stress
|
Study reference |
Study characteristics |
Patient characteristics |
Type of surgery |
Type of anaesthesia |
Intervention
|
Comparison / control |
Cortisol outcome measures and results |
Comments |
|
Fu (2019)
|
Systematic review and meta-analysis of RCTs
Literature search up to 5 February 2019. 18 RCTs were included in the review and 8 in the meta-analysis.
Cortisol 6 RCTs used music in the intraoperative setting
A: Hepp, 2018, Germany B: Liang, 2017, China C: Migneault, 2004, Canada* D: Nilsson, 2005, Sweden* E: Tabrizi, 2012, Iran* F: Zengin, 2013, Turkey*
Source of funding: No external funding was received for this study.
Conflicts of interest: The authors declared no conflicts of interest.
|
Inclusion criteria SR: -randomized controlled trials (RCTs) investigating the effect of recorded music pre-, intra-, and/or postoperatively; -adult surgical patients aged ≥18 y; -stress response to surgery assessed by measuring stress response biomarker levels; - full text, peer-reviewed published papers in the English language.
Exclusion criteria SR: -music intervention did not contain the elements melody, harmony and rhythm; -use of multiple, concomitant interventions; -live music with a musical therapist; -intervention consisted solely of nature sounds.
Important patient characteristics
N, total and per group (music versus control) A: 254, 154/150 B: 60, 30/30 C: 30, 15/15 D: 50, 25/25 E: 90, 30/30/30 F: 100, 50/50
Mean age ± SD or range (music versus control) A: 33.5 ± 5.4, range 18-47 / 33.7 ± 5.4, range 21-44 B: range 65-75 C: 52.2 ± 9.1 / 46.3 ± 12.1 D: 55 ± 14.7 / 57 ± 11.6 E: 23.83 ± 6.2, range 18-45 F: 49 ± 15.58 / 50.74 ± 14.01
Sex (% men) (music versus control) A: 0% / 0% B: - C: 0% / 0% D: 96% / 96% E: 100% / 100% F: 56% / 48%
|
A: Primary caesarean Section B: not specified C: Abdominal hysterectomy or (hystero)salpingooophorectomy D: Open hernia repair (Lichtenstein) E: Urological or abdominal surgery F: port catheter placement
|
A: regional B: spinal C: general D: general E: spinal F: local
|
Live/recorded music All 6 studies used recorded music
Type of music (minutes) A: Choice of 60 tracks of jazz, lounge, classical, meditation music (procedure duration) B: Choice of hypnotic music list (procedure duration) C: Choice of jazz, classical, new-age, popular piano music (procedure duration) D: Soft, relaxing, new age synthesizer melodies (procedure duration) E: Choice of relaxing Bach pieces (procedure duration) F: “Acemişiran” (Turkish classical music) (procedure duration)
Research team selected
|
A: standard care B: standard care C: headphones without music D: standard care E: headphones without music (control group 1) and standard care control group 2) F: standard care
|
Outcome measures A: salivary cortisol B: salivary cortisol C: plasma cortisol D: serum cortisol E: serum cortisol F: serum cortisol
Results meta-analysis A meta-analysis of five RCTs reporting cortisol levels at the end of surgery (including three RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of –0.14 (95% CI -0.57 to 0.28); p=0.50, I2=60.15.
A meta-analysis of six RCTs reporting cortisol levels postoperatively (including three RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of –0.30 (95% CI -0.53 to -0.07); p=0.01, I2=0
|
Authors’ conclusion Perioperative music can attenuate the physiological and neuroendocrine stress response to surgery. As none of the included studies assessed postoperative complications or patient outcome, the clinical implications are not yet totally clear.
Intervention Music delivery was achieved in a majority of the studies through headphones (11 studies, 61%) or a music pillow (three studies, 17%)
Outcomes Only data on cortisol were extracted from this review, because this outcome has the strongest association with patient experienced stress
Risk of bias Several studies provided insufficient details to assess all quality domains. Risk of performance bias was high, as it is difficult to achieve adequate blinding to the music intervention. Most included studies in the meta-analysis had a relatively small number of patients
Heterogeneity The patients, surgical procedures, and anesthesia method used and perioperative care offered differed substantially
Publication bias Publication bias was not assessed, as less than 10 studies were included in the meta-analysis |
* study included in meta-analysis
Table 3.3 Evidence table for systematic review of RCTs on the effects of music in the intraoperative setting on medication and length of stay
|
Study reference |
Study characteristics |
Patient characteristics |
Type of surgery |
Type of anaesthesia
|
Intervention
|
Comparison / control
|
Outcome measure(s) and results medication |
Outcome measure(s) and results length of stay |
Comments |
|
Fu (2020)
|
Systematic review and meta-analysis of RCTs
Literature search up to 7 January 2019. 55 RCTs were included in the review and 33 in the meta-analysis.
Medication 13 RCTs used music solely in the intraoperative setting
A: Ayoub, 2005, USA* B: Bansal, 2010, India* C: Kliempt, 1999, UK D: Koch, 1998, USA* E: Migneault, 2004, Canada* F: Nielsen, 2018, Sweden* G: Nilsson, 2001, Sweden* H: Nilsson, 2003b, Sweden* I: Nilsson, 2005, Sweden* J: Reza, 2007, Iran* K: Şen, 2009a, Turkey* L: Szmuk, 2008, USA M: Zhang, 2005, China*
Length of stay 3 RCTs used music solely in the intraoperative setting
A: Ayoub, 2005, USA D: Koch, 1998, USA G: Nilsson, 2001, Sweden
Source of funding: No external funding was received for this study.
Conflicts of interest: The authors declared no conflicts of interest.
|
Inclusion criteria SR: -available, peer-reviewed, full-text articles of randomized controlled trials in the English language; -adult patients 18 years old; -undergoing an inhospital or outpatient invasive, surgical procedure; -investigating the use of recorded music pre-, intra-, and/or postoperatively with either medication requirement, hospital length of stay or direct medical costs as outcome measures.
Exclusion criteria SR: -studies investigating solely nature sounds; -studies investigating live music with a music therapist; -studies investigating music with an additional, concomitant intervention were excluded, except if this additional intervention was used in both the intervention and control group.
Important patient characteristics
N, total and per group (music versus control) A: 59, 31/28 B: 100, 50/50 C: 51, 25/26 D: 34, 19/15 E: 30, 15/15 F: 102, 58/44 G: 58, 30/28 H: 100, 51/49 I: 50, 25/25 J: 100, 50/50 K: 60, 30/30 L: 40, 20/20 M: 110, 55/55
Mean age ± SD or range (music versus control) A: 55 ± 12 / 57 ± 10 B: 34 ± 16.6 / 32 ± 17.8 C: range 24-75 / range 21-75 D: 54 ± 15 / 53 ± 12 E: 52.2 ± 9.1 / 46.3 ± 12.1 F: 59 ± 17 / 56 ± 18 G: 51 ± 8.1 / 50 ± 8.2 H: 54.0 ± 13.4 I: 55 ± 14.7 / 57 ± 11.6 J: 26.0 ± 5.2 K: 22.5 ± 3.1 L: 52.0 ± 16.0 M: 41 ± 5 / 41 ± 3
Sex (% men) (music versus control) A: 90% / 84% B: 76% / 68% C: 36% / 35% D: 85% / 87% E: 0% / 0% F: 48% / 41% G: 0% / 0% H: 50% I: 96% / 96% J: 0% K: 100% L: 50% M: 0% / 0% |
A: Urological procedures B: Abdominal, urological, or lower extremity surgery C: diverse range of surgical procedures D: Outpatient urological procedures E: Gynaecological surgery F: Unspecified orthopedic, urological, gynaecological and general surgery G: Elective abdominal hysterectomy H: Daycare surgery: varicose veins, open inguinal hernia repair I: Open hernia repair (Lichtenstein) J: Elective caesarean section K: Local urological procedures L: Laparoscopic hernia or cholecystectomy M: Total abdominal hysterectomy
|
A: regional B: spinal C: general D: Spinal E: General F: Epidural, spinal and local G: general H: General I: General J: General K: Propofol PCS with local infiltration L: General M: General with spinal or epidural
|
Live/recorded music All 13 studies used recorded music
Music genre (duration) A: own favorite music (procedure duration) B: choice of folk, classical, religious, soothing music (-) C: classical music Adagio Karajan (procedure duration) D: own favorite music (procedure duration) E: choice of jazz, classical, popular new-age or piano music (procedure duration) F: Musicure (procedure duration) G: relaxing, calming music with sea waves sound (procedure duration) H: soft instrumental new-age synthesizer music (procedure duration) I: soft, new-age synthesizer (procedure duration) J: soft, instrumental, Spanish style guitar music (procedure duration) K: own favorite music (procedure duration) L: choice of pop-rock, classical or Israeli music (procedure duration) M: own favorite music (procedure duration)
|
A: headphones with operation noise recording B: occlusive headphones C: headphones without music D: standard care E: headphones without music F: standard care G: headphones with operation noise recording H: headphones without music I: headphones without music J: white music K: earphones without music L: headphones without music M: headphones without music
|
Outcome measures A: intraoperative propofol requirement B: intraoperative midazolam requirement C: Intraoperative opioid requirement D: Intraoperative propofol Requirement E: Intraoperative end-tidal Isoflurane and Intraoperative fentanyl requirement and postoperative opioid requirement F: Intraoperative fentanyl requirement and intraoperative propofol requirement G: postoperative opioid requirement H: postoperative opioid requirement I: postoperative opioid requirement J: postoperative opioid requirement K: Intraoperative propofol requirement L: intraoperative end-tidal sevoflurane and postoperative opioid requirement M: intraoperative propofol requirement Results meta-analysis For postoperative opioid requirement, a meta-analysis of 20 RCTs (including six RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of -0.31 (95% CI -0.45 to -0.16); p<0.001, I2=44.3
For propofol, a meta-analysis of nine RCTs (including three RCTs using music in the intraoperative setting) showed a pooled standardized mean difference of -0.72 (95% CI -1.01 to -0.43); p=0.00001, I2=61.1
For midazolam, a meta-analysis of three RCTs (including one RCT using music in the intraoperative setting) showed a pooled standardized mean difference of -1.07 (95% CI -1.70 to -0.44); p<0.001, I2=73.1
|
Outcome measures A: PACU length of stay D: PACU length of stay G: hospital length of stay
Results meta-analysis A meta-analysis of nine RCTs (including two RCTs using music in the intraoperative setting, both reporting on PACU length of stay) showed a pooled standardized mean difference of –0.18 (95% CI -0.43 to 0.067); p=0.15, I2=56.0
|
Authors’ conclusion Perioperative music can reduce postoperative opioid and intraoperative sedative medication requirement. Therefore, perioperative music may potentially improve patient outcome and reduce medical costs, as a higher opioid dosage is associated with an increased risk of adverse events and chronic opioid use. No effect of perioperative music on length of stay was demonstrated.
Intervention In a majority of studies, music delivery was achieved using a music player and headphones (41 studies, 75%). Other reported music delivery methods were a music pillow (3 studies, 5.5%), CD-player (3 studies, 5.5%), personal stereo (1 study, 1.8%), an integrated music system in the patient room (1 study, 1.8%), or not specified (6 studies, 11%).
Outcomes Only postoperative opioids were assessed, as other analgesic medications were often not reported. Some included studies did report that perioperative music also reduced nonopioid analgesic requirement postoperatively.
Risk of bias A potentially high risk of selection bias was present in several studies, and several studies provided insufficient details to assess selection bias. A moderate to high risk of performance bias was present, as blinding of patients for the music intervention is only possible when the intervention is performed solely intraoperatively during general anesthesia.
Heterogeneity The included studies contained different surgical patients, surgical procedures, and follow-up duration of the outcome assessment. This was reflected in the moderate to high level of heterogeneity observed.
Publication bias A funnel plot to investigate publication bias of studies assessing the effect of perioperative music on postoperative opioid requirement showed a near funnel-shaped plot, lacking a small number of studies in the lower-left corner which could be indicative of studies with relatively small samples sizes and small effect sizes being potentially absent |
Table 3.4 Evidence table of recent RCTs on the effects of music in the intraoperative setting
Study reference |
Study population |
Type of surgery |
Type of anaesthesia
General perioperative pain protocol |
Intervention (I)
|
Comparison / control (C)
|
Outcome measures and effect size |
Comments |
|
Choubsaz (2018)
Iran |
Inclusion criteria: -ASA (American Society for Anesthesiology) classes I and II pregnant women who were candidates for elective cesarean section for delivery
Exclusion criteria: -history of psychological problems -history of psychotropic drug use -hearing problems -dissatisfaction about participation in the study
N at baseline and analysis: I: 30 C1: 30 C2: 30
Important prognostic factors:
Mean age ± SD I: 27.1 ± 4.94 C1: 30.17 ± 8.11 C2: 26.6 ± 5.59
Sex: I: 0% M / C1: 0% M / C2: 0% M
There were a number of baseline differences: -education (% Diploma to bachelor’s degree I: 73% / C1: 93% / C2: 80%) -parity (first pregnancy I: 60%, C1: 50% / C2: 83%). Regarding parity, the differences between music and control group (p = 0.135) and music and ear plug group (p = 0.326) were not significant. -pre-test anxiety (I: 21.83 ± 11.9 / C1: 22.63 ± 12.13 / C2: 24.4 ± 11.89). |
Elective Caesarean section |
Regional anesthesia / spinal anesthesia with a standard dose of bupivacaine 0.5% was performed
No information given about pain protocol
|
Sedative musical piece of the Iranian Music Therapy Association through headphones
Recorded music
Selected by research team
Intraoperatively for the duration of surgery |
Control group 1: ear plug with a noise reduction rating of 30 dB for the duration of surgery
Control group 2: Routine medical care |
Timing of measurements: before and after surgery
Anxiety (STAI (20-80)) mean ± SD
Before surgery: I: 21.83 ± 11.9 C1: 22.63 ± 12.13 C2: 24.4 ± 11.89
After surgery: I: 13 ± 8.02 C1: 20.17 ± 10.38 C2: 16.6 ± 8.14
Although the result of one-way ANOVA showed no significant difference between the scores in the three groups, the result of post-test score showed that anxiety scores after surgery were lower in the music group compared with the ear plug group (p=0.007).
|
No information given about the duration of the Caesarean section.
|
|
Kurdi (2018)
India |
Inclusion criteria: -women aged over 18 years -posted for emergency caesarean section delivery -ASA physical status classes 1E and 2E - willing to participate and signed an informed consent form
Exclusion criteria: -hearing defects or any ear abnormalities -psychiatric disorders
N total at baseline / analysis: I: 63 / 61 C: 63 / 62
Important prognostic factors:
Mean age ± SD I: 25.4 ± 3.3 C: 24.5 ± 2.7
Sex: I: 0% M C: 0% M
Groups comparable at baseline
|
Emergency Caesarean section |
Regional (spinal)
Postoperatively, whenever patient requested for analgesia or when VAS score for pain was >3 (whichever was first), intramuscular diclofenac 75 mg was injected
|
Soothing meditation music through headphones covering the whole ear
Recorded music
Selected by research team
Intraoperatively for the duration of surgery
|
Headphones covering the whole ear |
Mean time required for first rescue analgesic (minutes) mean ± SD I: 133.7 ± 99.78 C: 136.58 ± 68.88 p=0.031
1 hour post-operatively
Pain (VAS; 0-10) mean ± SD I: 1.62 ± 1.14 C: 1.51 ± 1.19 p=0.05
Anxiety (VAS; 0-10) mean ± SD I: 0.8 ± 0.63 C: 1.21 ± 0.91 p=0.031
6 hours post-operatively
Pain (VAS; 0-10) mean ± SD I: 3.22 ± 1.26 C: 4.41 ± 3.68 p=0.042
Anxiety (VAS; 0-10) mean ± SD I: 2.16 ± 1.26 C: 3.59 ± 1.42 p=0.012
24 hours post-operatively
Pain (VAS; 0-10) mean ± SD I: 0.93 ± 0.83 C: 2.41 ± 1.28 p=0.025
Anxiety (VAS; 0-10) mean ± SD I: 0.62 ± 0.82 C: 1.83 ± 0.91 p=0.015 |
This study also evaluated the effect of another intervention, binaural beat meditation music, but this intervention did not meet the criteria for ‘music’.
|
|
Kukreja (2020)
USA |
Inclusion criteria: -patients greater than 18 years of age -American Society of Anesthesiologists (ASA) Class I, II, or III -undergoing total knee Arthroplasty under spinal anesthesia
Exclusion criteria: -any contraindications for spinal anesthesia
N at baseline / analysis: Intervention: 38 / 29 Control: 43 / 28
Important prognostic factors:
Mean age ± SD I: 65.14 ± 1.82 C: 61.68 ± 2.27
Sex: I: 31% M C: 36% M
Length of surgery was comparable between groups. However, subjects in the music group had a statistically significant lower average STAI-State baseline (pre-operative) score as compared to the control group (music group: 31.00 ± 1.44; control group: 38.04 ± 2.35); p=0.013) |
Total knee arthroplasty |
Regional (spinal anesthesia)
Preoperatively, all patients in both groups received continuous adductor canal block for postoperative analgesia. All patients received 1 mg of midazolam and 50 mcg of fentanyl as sedatives for performing the nerve block.Intraoperatively, all patients were given a standardized dose of 1 mg midazolam and 50 mcg fentanyl, as well as started on a propofol infusion. |
Blues, classical, country, gospel, jazz, classical, rhythm and blues, rock, or soundtrack through headphones
Recorded music
Patient selected a genre
Intraoperatively for the duration of spinal anesthesia |
No music, no headphones |
Postoperative
Anxiety (STAI-State (20-80)) mean ± SD I: 28.34 ± 1.64 C: 32.21 ± 1.56 p=0.094 (mean score in the music group was already lower at baseline, change from pre-post was not significant)
Anxiety (STAI-Trait (20-80)) mean ± SD I: 28.14 ± 1.00 p=0.011 (mean score in the music group was already lower at baseline, change from pre-post was not significant)
Propofol dose per kilogram per surgical minute C: 0.06 p=0.264
|
|
|
Tran (2020)
USA |
Inclusion criteria: -patients aged at least 18 years -scheduled to undergo primary total knee arthroplasty by a single orthopedic surgeon -eligibility for spinal anesthesia -mental capacity to consent and follow study instructions
Exclusion criteria: -members of regulated vulnerable populations (ie, prisoners, parturients) -contraindications to spinal anesthesia -morbid obesity -specific allergies (propofol, midazolam, and morphine) -preoperative daily morphine equivalent greater than 60 mg -impaired hearing
N at baseline / analysis: Intervention: 19 / 16 Control: 17 / 16
Important prognostic factors:
Mean age ± SD I: mean 67 ± 8 C: median 62 (IQR 59 to 72)
Sex: I: 56% M C: 25% M
BMI, ASA classification, anesthesia time, and surgical duration were not statistically different between groups
Groups comparable at baseline |
Primary total knee arthroplasty |
Regional (spinal-epidural)
All patients received premedication with acetaminophen, celecoxib, gabapentin, and scopolamine.
After the surgical procedure, the study participants received acetaminophen, celecoxib, and gabapentin at scheduled intervals per standard protocol.
|
Variety of music genres through noise-cancelling wireless headphones
Recorded music
Patient selected genre
Intraoperatively for the duration of surgery (I: mean 119 minutes ± 26 / C: 103±25.6)
|
Noise-cancelling, wireless headphones |
Intraoperative
Propofol usage (mg/kg/min) mean ± SD I: 3.5 ± 8.9 C: 5.1 ± 8.7 P value: 0.10
Postoperative
Median pain scores (NRS (0-10)) taken immediately after surgery and every 4 hours afterward over a 24-hour time period I: 1.6 (IQR 0.79 to 3.5) C: 2.4 (IQR 0.72 to 4.5) P=0.47
Mean/median opioid consumption over 24-hour time period starting immediately after surgery (MME) I: mean 20.8 (SD 18.8) C: median 18.3 (IQR 7.5 to 43.1) P=0.58
|
This study was likely to be underpowered since the authors assumed a large reduction in sedation usage (≥50%) for the power calculation
|
|
Kavakli (2019)
Turkey |
Inclusion criteria:
Exclusion criteria: -contraindications for the cervical plexus block (local infection, coagulation disorders) -hypersensitivity to the local anaesthetics -refusal of regional anaesthesia
N at baseline / analysis: I: 35 / 32 C: 35 / 32
Important prognostic factors:
Mean age ± SD I: 68.5 ± 8.4 / C: 66.5 ± 9.7
Sex: I: 69% M / C: 69% M
Duration of surgery, Carotid clamping time were not statistically different between groups
Groups comparable at baseline
|
Carotid endarterectomy
|
Regional
(Combined (deep and superficial) cervical plexus blocks were performed as regional anaesthetic technique)
When intraoperative VAS was > 3, a 0.4 mg/kg bolus of supplemental 1% lidocaine was administered to the surgical area by the surgeon. If pain persisted despite a 2 mg/kg dose of lidocaine, then supplemental intravenous (IV) analgesia of 0.5μg/kg of fentanyl up to a maximum dose of 200μg was given.
When the postoperative VAS scores exceeded 3/10, 1 mg/kg dose of IV tramadol was administered. |
Turkish folk music, Turkish classical music, Turkish popular music or Turkish art music through headphones
Recorded music
Patient selected one of four genres
Intraoperatively for the duration of surgery (I: mean 67 ± 15 / C: 76 ± 32)
|
Operation room noise through headphones
|
Intraoperative: Volume of supplemental lidocaine 1% (mL) C: 1.8 ± 2.8 p=0.552
Patients requiring lidocaine 1% n (%) I: 8 (25%) C: 10 (31.2%) p=0.578
Intraoperative fentanyl used (μg) I: 9.3 ± 26.7 C: 7.8 ± 22.3
Intraoperative response to question of “are you relaxed” (question STAI-S (1-4)) median (IQR) C: 4 (3–4) MD -0.8 (95%CI -1 to -0.6; p=0.0001)
Intraoperative response to question of “are you calm” (question STAI) median (IQR) C: 4 (3–4) MD -0.7 (95%CI -0.9 to -0.5; p=0.0001)
Intraoperative anxiety (NRS (0-10)) immediately after surgery mean ± SD I: 5.5 ± 1.9 C: 3.4 ± 1.3 MD 2.0 (95% CI 1.1 to 2.8; p=0.001)
Intraoperative pain (VAS (0-10)) I: 2.4 ± 0.8 C: 2.5 ± 1
Postoperative: Time of first analgesic requirement in PACU (min) I: 107 ± 22 C: 116 ± 28
Postoperative tramadol consumption (mg) mean ± SD I: 17.1 ± 31.3 C: 19.5 ± 33.4
Postoperative state anxiety (STAI-S (20-80)) mean ± SD unknown at what time
Postoperative pain (VAS (0-10)) in the PACU mean ± SD C: 2.3 ± 1
Patient satisfaction score postoperatively (Likert scale (1-5)) median (IQR)
Length of stay in PACU (minutes) mean ± SD I: 139 ± 20 C: 149 ± 23 p=0.112
Hospital stay (days) mean ± SD I: 2.8 ± 0.7 C: 3 ± 0.8 p=0.269 |
|
|
Gökçek (2020)
Turkey |
Inclusion criteria: -undergoing septorhinoplasty under general anesthesia -aged 18-70 years
Exclusion criteria: - patients who had emergency surgery -patients with hearing problems -patients unable to cooperate (due to dementia, mental retardation, et cetera) -patients with drug or alcohol abuse history -patients who did not want to participate in the study
N at baseline / analysis: Music group: 60 / 60 Control: 60 / 60
Important prognostic factors:
Mean age ± SD I: 31.93 ± 8.67 C: 31.56 ± 8.05
Sex: I: 48% M C: 45% M
There was no statistically significant difference between groups in terms of demographic characteristics (age, BMI, gender, ASA). The duration of surgery and anesthesia of the groups were similar. |
septorhinoplasty |
general anesthesia
Thirty minutes before surgery, all patients were premedicated with 0.03 mg/kg intramuscular midazolam (Dormicum, Roche). During the anesthesia induction, 2.5 mg/kg IV propofol (Pofol ), 1g/kg fentanyl (Fentanyl , Janssen) bolus IV, and 1 mg/kg IV arithmetic (Aritmal , Adeka) were applied. Muscle relaxation was achieved with 0.6 mg/kg rocuronium (Esmeron , 10 m/mL, Organon). After endotracheal intu bation, 2% sevoflurane (Sevorane , Abbot) was injected with 40% oxygen rate in anesthesia maintenance. In addition to inhalation anesthesia, IV infusion of remifentanil (Ultiva, Glaxo Welcome) was applied at 0.05---10g/kg/min. The remifentanil dose was increased or decreased when an increase or decrease of more than 20% of the baseline systolic arterial pressure was observed. An additional muscle relaxant was administered depending on the duration of the operation and follow-up of the neuromuscular blockade. When the heart rate dropped below 50 beats/min, 0.5 mg atropine was injected; when mean arterial pressure (MAP) dropped below 60 mg, 10 mg of ephedrine was injected.
Patients with severe postoperative pain (VAS ≥ 5) were medicated with 0.5 mg/kg Petidin HCL (Aldolan) (4 patients of the music group versus 9 of the control group) |
Relaxing Indigenous and foreign music (pop, arebesk, jazz, alaturka, classical, ethnic, MMP-3078) through headphones enclosing the ears
Recorded music
Mostly patient selected from list; the anesthesiologist chose classical music for 2 patients who did not show a particular preference
Intraoperatively for the duration of surgery (I: mean 139.75 minutes ± 9.75 / C: 141.03 minutes ± 10.8)
|
no music / no headphones |
Postoperative pain during recovery (VAS (0-10)) mean ± SD I: 2.73 ± 1.28 C: 3.61 ± 1.40 p<0.001
Patient satisfaction (EVAN-G scale (0-100)) I: 44 (73.3%) C: 22 (36.6%) p<0.001
|
|
|
Kahloul (2017)
Tunisia |
Inclusion criteria: -all patients scheduled for abdominal surgery -aged more than 18 years -agreed to participate
Exclusion criteria: -urgent surgery cognitive or psychiatric disorders -hearing-impairing diseases -chronic treatment with analgesics
N at baseline / analysis: I: 70 / 70 C: 70 / 70
Important prognostic factors:
Mean age ± SD: I: 51.7 ± 13.58 C: 51.2 ± 12.5
Sex: I: not reported C: not reported
The comparison between the two groups regarding demographic characteristics (BMI) and surgical interventions did not find statistically significant differences
|
Abdominal surgery |
General anesthesia
Anesthesia induction was carried out by Fentanyl at the dose of 3 µ/ kg, propofol titration, and eventually cisatracurium at a dose of 0.15 mg/kg if a tracheal intubation was considered. Anesthesia was maintained by isoflurane in a mixture of 50% oxygen and 50% air. Fentanyl and cisatracurium were reinjected depending on intervention duration and neuromuscular blockade monitoring
Pain protocol: Anticipation of analgesia was made by 1 g of paracetamol and 20 mg of nefopam infusion 30 minutes before the end of the surgical procedure. |
Different types of music, including Tunisian music, Eastern and Western music
Recorded music
Mostly patient selected from list; the anesthesiologist chose classical music for 4 patients who did not show a particular preference
Intraoperatively for the duration of surgery (I: mean 79.1 minutes ± 43.6 / C: 82.6 minutes ± 36.6)
|
Headphones |
Postoperative pain on waking (VAS (0-100)) I: 33.8 ± 13.63 C: 45.1 ± 16.15 P<0.001
Patient satisfaction 24 hours after surgery (EVAN-G): I: 81.42% C: 51.42% P<0.001
|
|
Abbreviations: STAI: State-Trait Anxiety Inventory; VAS: Visual Analog Scale; NRS: numerical rating scale; MME: morphine milligram equivalents; EVAN-G: Evaluation du Vecu de l'Anesthesie Generale
Table 3.5 Risk of bias table for recent RCTs on the effects of music in the intraoperative setting
Research question: ‘What are the effects of music (recorded or live) in the intraoperative setting on patients undergoing invasive surgery with anaesthesia care when compared to no music?’
|
Study reference
(first author, publication year) |
Was the allocation sequence adequately generated? a
Definitely yes Probably yes Probably no Definitely no |
Was the allocation adequately concealed?b
Definitely yes Probably yes Probably no Definitely no |
Blinding: Was knowledge of the allocated interventions adequately prevented?c
Were patients blinded?
Were healthcare providers blinded?
Were data collectors blinded?
Were outcome assessors blinded?
Were data analysts blinded? Definitely yes Probably yes Probably no Definitely no |
Was loss to follow-up (missing outcome data) infrequent?d
Definitely yes Probably yes Probably no Definitely no |
Are reports of the study free of selective outcome reporting?e
Definitely yes Probably yes Probably no Definitely no |
Was the study apparently free of other problems that could put it at a risk of bias?f
Definitely yes Probably yes Probably no Definitely no |
Overall risk of bias If applicable/necessary, per outcome measureg
LOW Some concerns HIGH
|
|
Choubsaz (2018) |
Probably no;
Reason: no information provided about sequence generation |
Probably no;
Reason: no information provided about allocation concealment |
Definitely no;
Reason: patients were not blinded |
Definitely yes;
Reason: no missing outcome data |
Probably no;
Reason: all outcomes described in the Methods section are reported but no trial registration or protocol was available |
Probably no;
Reason: baseline differences regarding education, parity, and anxiety scores
|
HIGH (anxiety)
|
|
Kurdi (2018) |
Definitely yes;
Reason: Randomization was done by means of picking up chits by the patient marked as M, B, and C kept in a box. There were a total of 189 chits in the box, with equal number of M, B and C chits (63 each) |
Probably yes;
Reason: Randomization was done by means of picking up chits by the patient marked as M, B, and C kept in a box. There were a total of 189 chits in the box, with equal number of M, B and C chits (63 each) |
Definitely no;
Reason: patients were not blinded |
Definitely yes;
Reason: loss to follow-up infrequent and comparable between groups (I: 3% / C: 2%) |
Probably yes;
Reason: all outcomes described in the Methods section are reported but no trial registration or protocol was available |
Probably no;
Reason: no ITT analysis (but loss to follow-up was infrequent) |
Some concerns (analgesics, pain, anxiety) |
|
Kukreja (2020) |
Definitely yes;
Reason: computer-generated random numbers |
Probably no;
Reason: no information provided about allocation concealment |
Definitely no;
Reason: patients were not blinded. Probably others also not blinded (not reported) |
Definitely no;
Reason: 9 patients in the music group (24%) and 15 patients in the control group (35%) were lost to follow-up |
Probably no;
Reason: all outcomes described in the Methods section are reported but the trial registration did not include anxiety or propofol dose |
Definitely no;
Reason: no ITT analysis, very limited information about study arms. |
HIGH |
|
Tran (2020) |
Definitely yes;
Reason: Simple randomization for 2 study arms was prepared through Research Randomizer (randomizer.org). |
Probably yes;
Reason: Treatment allocations were documented and distributed using a sealed envelope system |
Definitely no;
Reason: patients were not blinded |
Probably no;
Reason: 3/19 patients (16%) in the intervention group and 1/17 (6%) in the control group withdrew |
Definitely no;
Reason: patient satisfaction is not reported, opioid consumption was not mentioned in the trial registration |
Definitely no;
Reason: no ITT analysis and this study was likely to be underpowered since the authors assumed a large reduction in sedation usage (≥50%) for the power calculation |
HIGH (propofol usage, pain scores, opioid consumption) |
|
Kavakli (2019) |
Definitely yes;
Reason: simple, non-stratified randomization scheme generated by software available online |
Probably yes;
Reason: Group allocation was concealed within numbered, sealed, opaque envelope |
Definitely no;
Reason: patients were not blinded |
Probably yes;
Reason: only three patients (9%) were lost to follow-up in each group
|
Probably no;
Reason: all outcomes described in the Methods section are reported but the trial registration did not include medication outcomes, length of stay, and patient satisfaction scores |
Probably yes; |
Some concerns (pain, anxiety, length of stay, analgesic requirement, patient satisfaction)
|
|
Gökçek (2020) |
Probably no;
Reason: Randomization procedure not described |
Probably no;
Reason: Randomization procedure not described |
Definitely no;
Reason: patients and healthcare providers were not blinded (patients in the control group did not wear headphones) |
Definitely yes;
Reason: no missing outcome data |
Probably yes;
Reason: all outcomes described in the Methods section are reported but no trial registration or protocol was available
|
Probably yes;
|
HIGH (pain, patient satisfaction)
|
|
Kahloul (2017) |
Definitely no;
Reason: the patients operated on during even days were included in the intervention group while the patients operated during odd days were included in the control group |
Probably no;
Reason: allocation concealment not described. |
Probably yes;
Reason: double blinded but no details provided |
Probably no;
Reason: no information about proportion of missing outcomes |
Probably no;
Reason: Outcomes of interest are reported incompletely (no raw data available) |
Probably yes;
|
HIGH (pain, patient satisfaction)
|
Table 3.6 Quality assessment for systematic reviews of RCTs and observational studies
Based on AMSTAR checklist (Shea, 2007; BMC Methodol 7: 10; doi:10.1186/1471-2288-7-10) and PRISMA checklist (Moher, 2009; PLoS Med 6: e1000097; doi:10.1371/journal.pmed1000097)
|
Study
First author, year |
Appropriate and clearly focused question?1
Yes/no/unclear |
Comprehensive and systematic literature search?2
Yes/no/unclear |
Description of included and excluded studies?3
Yes/no/unclear |
Description of relevant characteristics of included studies?4
Yes/no/unclear |
Appropriate adjustment for potential confounders in observational studies?5
Yes/no/unclear/not applicable |
Assessment of scientific quality of included studies?6
Yes/no/unclear |
Enough similarities between studies to make combining them reasonable?7
Yes/no/unclear |
Potential risk of publication bias taken into account?8
Yes/no/unclear |
Potential conflicts of interest reported?9
Yes/no/unclear |
|
Kühlmann, 2018 |
Yes |
Yes |
Yes |
Yes |
Not applicable |
Yes |
Yes |
Yes |
No (reported for review but not for included studies) |
|
Fu, 2019 |
Yes |
Yes |
Yes |
Yes |
Not applicable |
Yes |
Yes |
Yes (publication bias could not be assessed because there were fewer than 10 studies included in the meta-analysis) |
No (reported for review but not for included studies) |
|
Fu, 2020 |
Yes |
Yes |
Yes |
Yes |
Not applicable |
Yes |
Yes |
Yes |
No (reported for review but not for included studies) |
- Research question (PICO) and inclusion criteria should be appropriate and predefined.
- Search period and strategy should be described; at least Medline searched; for pharmacological questions at least Medline + EMBASE searched.
- Potentially relevant studies that are excluded at final selection (after reading the full text) should be referenced with reasons.
- Characteristics of individual studies relevant to research question (PICO), including potential confounders, should be reported.
- Results should be adequately controlled for potential confounders by multivariate analysis (not applicable for RCTs).
- Quality of individual studies should be assessed using a quality scoring tool or checklist (Jadad score, Newcastle-Ottawa scale, risk of bias table et cetera)
- Clinical and statistical heterogeneity should be assessed; clinical: enough similarities in patient characteristics, intervention and definition of outcome measure to allow pooling? For pooled data: assessment of statistical heterogeneity using appropriate statistical tests (for example Chi-square, I2)?
- An assessment of publication bias should include a combination of graphical aids (for example funnel plot, other available tests) and/or statistical tests (for example Egger regression test, Hedges-Olken). Note: If no test values or funnel plot included score “no”. Score “yes” if mentions that publication bias could not be assessed because there were fewer than 10 included studies.
- Sources of support (including commercial co-authorship) should be reported in both the systematic review and the included studies. Note: To get a “yes,” source of funding or support must be indicated for the systematic review AND for each of the included studies.
Table of excluded studies
|
Author and year |
Reason for exclusion |
|
Akbas 2016 |
Wrong population: shockwave lithotripsy, no invasive surgery |
|
Alam 2016 |
Wrong population: local anesthetic |
|
Ames 2017 |
RCT included in the review by Kühlmann (2018) |
|
Amini 2018 |
Wrong intervention: nature sounds |
|
Amiri 2017 |
Wrong intervention: nature sounds |
|
Arango-Gutierrez 2019 |
Wrong language: Spanish |
|
Aris 2019 |
Wrong intervention: music in the postoperative setting |
|
Ashok 2018 |
Wrong publication type: study protocol |
|
Ashok 2019 |
Wrong intervention: music in the postoperative setting |
|
Bakl 2018 |
Wrong population: children |
|
Bashiri 2018 |
Wrong population: endoscopy/colonoscopy, no invasive surgery |
|
Belloeil 2020 |
Wrong population: local anaesthesia |
|
Bennett 2020 |
Wrong population: image-guided breast biopsy, no invasive surgery |
|
Billar 2020 |
Wrong publication type: study protocol |
|
Boustani 2018 |
Wrong intervention: LASIK eye surgery |
|
Browne 2020 |
Wrong intervention: shockwave lithotripsy, no invasive surgery |
|
Buehler 2017 |
Wrong population: children |
|
Cakmak 2017 |
Wrong intervention: shockwave lithotripsy, no invasive surgery |
|
Carter 2018 |
Wrong study type: implementation study |
|
Celebi 2020 |
Wrong intervention: colonoscopy, no invasive surgery |
|
Cetinkaya 2019 |
Wrong outcomes: no crucial outcomes reported |
|
Çetinkaya 2019 |
Wrong outcomes: nausea and vomiting |
|
Chai 2020 |
Wrong population: emergency department, not surgery |
|
Chantawong 2017 |
Wrong population: loop electrosurgical excision procedure, no invasive surgery |
|
Cheung 2018 |
Wrong population: no invasive surgery |
|
Cheung 2019 |
Wrong population: transvaginal ultrasound guided oocyte retrieval: no invasive surgery |
|
Chiodo 2019 |
Wrong outcomes: no crucial outcomes reported |
|
Cho 2016 |
Wrong population: transrectal ultrasound-guided prostate biopsies: no invasive surgery |
|
Choi 2018 |
Wrong population: topical anesthesia for cataract surgery, no invasive surgery |
|
Cift 2020 |
Wrong population: shockwave lithotripsy, no invasive surgery |
|
Cimen 2020 |
Wrong population: local anesthesia |
|
Cotoia 2018 |
Wrong intervention: music in the preoperative setting |
|
Denney 2018 |
Wrong intervention: music in the perioperative setting |
|
De Silva 2016 |
Wrong population: colonoscopy, no invasive surgery |
|
Di Nasso 2016 |
Wrong population: endodontic treatment (root canal therapy): no invasive surgery |
|
Diri 2019 |
Wrong population: urodynamic study, no invasive surgery |
|
Drzymalski 2017 |
Wrong population: no surgery |
|
Drzymalski 2020 |
Wrong intervention: no headphones |
|
Ebrahimi 2020 |
Wrong population: invasive coronary angiography, no invasive surgery |
|
El-Khoury 2020 |
Wrong population: shockwave lithotripsy: no invasive surgery |
|
Eren 2018 |
Wrong intervention: no headphones |
|
Ertug 2017 |
Wrong intervention: nature sounds |
|
Farzaneh 2019 |
Wrong intervention: nature sounds |
|
Faught 2016 |
Wrong publication type |
|
Ferraz 2020 |
Wrong outcome: pain related to wound care after surgery for diaphyseal tibial fractures |
|
Franzoi 2016 |
Wrong population: children |
|
Gallagher 2018 |
Wrong intervention: patients actively participated in music therapy |
|
Gasenzer 2017 |
Wrong outcome |
|
Gelatti 2020 |
Wrong comparison: effect of ‘live music’ compared with ‘recorded music’, rather than ‘music’ and ‘no music’ |
|
Gezginci 2018 |
Wrong population: cystoscopy: no invasive surgery |
|
Gezginci 2018 |
Wrong population: shockwave lithotripsy: no invasive surgery |
|
Glickman-Simon 2016 |
Wrong publication type: comment |
|
Gogoularadja 2020 |
Wrong intervention: music in the perioperative setting |
|
Goli 2018 |
Wrong intervention: music in the preoperative setting |
|
Gómez-Urquiza 2016 |
Wrong intervention: combination of music and photographic display |
|
Graff 2019 |
Wrong comparison: midazolam given in control group |
|
Gulnahar 2020 |
Wrong intervention: dental implant surgery, not invasive surgery |
|
Haack 2017 |
Wrong timing of intervention: some patients were re-admitted because of complications therefore music was not always provided immediately after surgery |
|
Hamidi 2017 |
Wrong population: office-based Percutaneous Nephrostomy Tube Placement |
|
Hanprasertpong 2016 |
Wrong population: second trimester genetic amniocentesis: no invasive surgery |
|
Harada 2017 |
Wrong outcome |
|
Hepp 2018 |
Wrong intervention: music via loudspeakers |
|
Hetland 2017 |
Wrong population: mechanical ventilation weaning: not necessarily related to surgery |
|
Hilal 2018 |
Wrong population: colposcopy, no invasive surgery |
|
Hill 2020 |
Wrong intervention: combination of music and a natural landscape image |
|
Jacq 2018 |
Wrong population: bed bathing of mechanically ventilated patients: no surgery |
|
Jeppesen 2016 |
Wrong population: bronchoscopy, no invasive surgery |
|
Kallush 2018 |
Wrong intervention: music therapy, long-term intervention, rather than a one-off intervention |
|
Karalar 2016 |
Wrong population: shockwave lithotripsy: no invasive surgery |
|
Kavak Akelma 2020 |
Wrong intervention: music in the preoperative setting |
|
Keilani 2017 |
Wrong study type: not an RCT or SR |
|
Khan 2020 |
Wrong comparison: no control group without music |
|
Kim 2020 |
Wrong comparison: results for two control groups (passive listening to music and no music) are reported together |
|
Ko 2017 |
Wrong population: colonoscopy, no invasive surgery |
|
Ko 2019 |
Wrong population: colonoscopy, no invasive surgery |
|
Kongsawatvorakul 2016 |
Wrong population: local anesthesia' for large loop excision of transformation zone, no invasive surgery |
|
Kupeli 2020 |
Wrong population: third molar surgery, no invasive surgery |
|
Kyavar 2016 |
Wrong outcome: pain following a painful procedure in intubated patients after coronary artery bypass graft surgery |
|
Kyrillos 2017 |
Wrong population: effect of music on professionals |
|
Labrague 2016 |
Wrong study design: not an RCT |
|
Laframboise-Otto 2020 |
Wrong intervention: music in the postoperative setting |
|
Lee 2017 |
Wrong intervention: music in the postoperative setting |
|
Leonard 2019 |
Wrong timing of intervention: effect of music during rehabilitation after surgery. |
|
Li 2020 |
Wrong population: image-guided musculoskeletal corticosteroid injections |
|
Lin 2020 |
Wrong intervention: music therapy for a duration of six months after surgery |
|
Low 2020 |
Wrong intervention: long-term intervention (vocal music therapy ) for chronic pain |
|
Luis 2019 |
Wrong intervention: patients actively participated in music therapy |
|
Mackintosh 2018 |
Wrong population: therapeutic pleural procedures (e.g. therapeutic pleural aspiration, intercostal chest tube insertion and tunnelled pleural catheter) --> local anaesthetic used |
|
McClurkin 2016 |
RCT included in the review by Kühlmann (2018) |
|
Messika 2016 |
Wrong publication type: study protocol |
|
Mietzsch 2020 |
Wrong population: effect of music on professionals |
|
Miladinia 2017 |
RCT included in the review by Kühlmann (2018) |
|
Mondanaro 2017 |
Wrong intervention: patients actively participated in music therapy |
|
Muddana 2020 |
Wrong population: topical anesthesia |
|
Najafi Ghezeljeh 2017 |
Wrong population: music for burn patients before wound care |
|
Najafi Ghezeljeh 2018 |
Wrong population: music for burn patients before wound care |
|
Ölçücü 2020 |
Wrong population: cystoscopy and ureteral stent removal, no invasive surgery |
|
Oomens 2020 |
Wrong population: effect of music on professionals |
|
Orak 2020 |
Wrong population: oocyte pick-up, no invasive surgery |
|
Ordaz Jurado 2017 |
Wrong population: shockwave lithotripsy, no invasive surgery |
|
Ortega 2019 |
Wrong population: local anesthesia for nasal bone fracture reduction |
|
Özdemir 2019 |
Wrong population: bone marrow aspiration and biopsy, no invasive surgery |
|
Packiam 2018 |
Wrong population: transrectal prostate biopsy: no invasive surgery |
|
Padam 2017 |
Wrong population: endoscopy, no invasive surgery |
|
Parodi 2020 |
Wrong intervention: binaural beats |
|
Proceedings of the 2017 RAMI Section of Ophthalmology Meeting 2018 |
Wrong publication type |
|
Rahmati 2018 |
Wrong intervention: music in the preoperative setting |
|
Roshani 2019 |
Wrong intervention: binaural beats |
|
Sanchez-Jauregui 2019 |
Wrong population: biopsy, no invasive surgery |
|
Scerrati 2020 |
Wrong population: musicians who underwent surgery |
|
Sfaniakis 2017 |
Wrong intervention: music in the postoperative setting |
|
Shabandokht-Zarmi 2017 |
Wrong population: fistula puncture-related pain, no invasive surgery |
|
Shakir 2017 |
Wrong population: effect of music on professionals |
|
Soo 2016 |
Wrong population: biopsy, no invasive surgery |
|
Sorensen 2020 |
Wrong population: local anesthesia |
|
Spagnuolo 2020 |
Wrong population: endoscopy, no invasive surgery |
|
Uğras 2018 |
Wrong intervention: music in the preoperative setting |
|
Wiwatwongwana 2016 |
Wrong population: topical anesthesia |
|
Wren 2016 |
Wrong publication type: not peer reviewed |
|
Wu 2017 |
Wrong intervention: no headphones |
|
Yamasaki 2016 |
Wrong population: effect of music on professionals |
|
Yamashita 2019 |
Wrong population: extraction of the impacted mandibular third molar, no invasive surgery |
|
Dale 2020 |
SRs including 12 RCTs, most of which were published before 2016. 1 relevant RCT by Sfakianakis (2017) |
|
Fu 2020 |
This SR was already included in the literature analysis |
|
Fu 2019 |
This SR was already included in the literature analysis |
|
Kühlmann 2018 |
This SR was already included in the literature analysis |
|
Abraha 2016 |
Wrong publication type |
|
Grafton-Clarke 2019 |
SR including 6 RCTs, all published before 2016 |
|
Abdelhakim 2019 |
Review about effect of music during colposcopy, no invasive surgery |
|
Ambler 2020 |
Wrong publication type |
|
Amiri 2019 |
SR not including recent studies about the effect of music |
|
Ayling 2020 |
Wrong outcomes |
|
Boyce 2018 |
SR including several RCTs, all published before 2016 |
|
Bradt 2016 |
SR including 20 studies about surgery, all published before 2016 |
|
Bro 2018 |
SR including 5 studies about surgery, all published before 2016 |
|
Chow 2016 |
SR about the effect of music on children |
|
Daniel 2016 |
SR not including recent relevant RCTs |
|
Fan 2020 |
SR not including recent relevant RCTs |
|
Felix 2019 |
Review about wrong intervention: guided imagery |
|
Field 2018 |
Review about postnatal anxiety, not focused on surgery |
|
Garcia-Perdomo 2018 |
Review about the effect of music during cystoscopy |
|
Janssen 2019 |
SR not including recent relevant RCTs |
|
Khan 2018 |
SR not including recent relevant RCTs |
|
Kievisiene 2020 |
SR not including recent relevant RCTs |
|
Cornelis 2019 |
SR not including recent relevant RCTs |
|
Burghardt 2018 |
SR not including recent relevant RCTs |
|
Feast 2020 |
SR not including recent relevant RCTs |
|
Garcia Guerra 2019 |
SR not including recent relevant RCTs |
|
Ghamry 2020 |
Review about the effect of music during hysteroscopy |
|
Gramaglia 2019 |
SR not including recent relevant RCTs |
|
Iyendo 2016 |
SR not including recent relevant RCTs |
|
Lin 2020 |
SR including three relevant RCTs that were found in our search |
|
Sibanda 2019 |
SR including one recent RCT with a focus on post-operative rehabilitation |
|
Wang 2020 |
SR not including recent relevant RCTs |
|
Yu 2020 |
SR not including recent relevant RCTs |
|
Zapata-Copete 2019 |
SR not including recent relevant RCTs |
|
Kyriakides 2018 |
SR about the effect of music during outpatient urology procedures (e.g. biopsy, shockwave lithotripsy, cystoscopy) |
|
Li 2017 |
SR about music for burn patients during treatment procedures |
|
Martin-Saavedra 2018 |
SR not including recent relevant RCTs |
|
Martin-Saavedra 2018 |
SR not including recent relevant RCTs |
|
Meghani 2017 |
SR not including recent relevant RCTs |
|
Song 2018 |
SR about the effect of music during biopsy |
|
van der Wal- Huisman 2018 |
SR not including recent relevant RCTs |
|
Vitale 2020 |
SR about the effect of music during hysteroscopy |
|
Whale 2019 |
SR not including recent relevant RCTs |
|
Lee 2016 |
SR not including recent relevant RCTs |
|
Oomens 2019 |
SR about wrong population: effect of music on professionals |
|
Rastipisheh 2019 |
SR about wrong population: effect of music on professionals |
|
Walker 2018 |
Wrong publication type: review methodology |
|
Williams 2018 |
Wrong publication type: review methodology |
|
Zimpel 2020 |
SR not including recent relevant RCTs |
|
Tam 2016 |
SR about the effect of music during bronchoscopy |
|
Lunde 2019 |
SR not including recent relevant RCTs |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 15-02-2023
Beoordeeld op geldigheid : 27-03-2023
De geldigheid van de richtlijnmodules komt te vervallen indien nieuwe ontwikkelingen aanleiding zijn een herzieningstraject te starten.
NB: Informatie over de autorisatiedatum, autoriserende partij(en), herbevestiging en regiehouder(s) worden ter zijne tijd na autorisatie toegevoegd aan deze alinea.
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Stichting Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodules.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodules is in 2020 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor volwassen patiënten die klinisch geopereerd worden, onder algehele en regionale anesthesie.
Werkgroep
- Prof. dr. E. (Erik) Heineman, chirurg, UMCG, Groningen, NVvH (voorzitter)
- Prof. dr. J. (Hans) Jeekel, chirurg, Erasmus MC, Rotterdam, NVvH
- Dr. E.G.J.M. (Robert) Pierik, chirurg, Isala, Zwolle, NVvH
- Dr. P. (Peter) van Vliet, neuroloog-intensivist, Haaglanden MC, Den Haag, NVIC
- Dr. W.K. (Wim) Lagrand, cardioloog-intensivist, Amsterdam UMC, Amsterdam, NVIC
- Dr. A.Y.R. (Rosalie) Kühlmann, anesthesioloog (in opleiding), Antonius ziekenhuis, Nieuwegein, NVA
- Prof. dr. F.U.S. (Francesco) Mattace Raso, geriater, Erasmus MC, Rotterdam, NVKG
- Drs. H.P.J.M. (Herbert) Habets, verplegingswetenschapper, vakgroep ouderengeneeskunde, Zuyderland Medisch Centrum, Sittard-Geleen, V&VN (Geriatrie & Gerontologie)
- A. (Arieke) Prozée, verpleegkundig specialist, UMCG, Groningen, V&VN
- K. (Klaartje) Spijkers, senior adviseur patiëntbelang, PFNL
- R. (René) van Munster, musicus
Met ondersteuning van
- Dr. J. Buddeke, senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Dr. L.J.M. Oostendorp, adviseur, Kennisinstituut van de Federatie Medisch Specialisten
Met dank aan Anna-Eva Prick (senior wetenschappelijk onderzoeker, Erasmus MC) en Roos Geensen (arts-onderzoeker, Erasmus MC) voor ondersteuning bij de selectie van recent gepubliceerde RCT’s en data extractie uit de geselecteerde RCT’s.
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
De meeste werkgroepleden zijn muziekliefhebbers. Om een goede richtlijn met breed draagvlak te ontwikkelen is het van belang om alle invalshoeken mee te nemen. Daarom is op advies van de belangencommissie een chirurg (dr. Pierik) toegevoegd aan de werkgroep. Daarnaast zijn de modules voorafgaand aan de commentaarfase naar de NVvH en NVA gestuurd voor commentaar.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Heineman (voorzitter) |
Hoogleraar chirurgie met emeritaat (0-aanstelling bij de RUG, Faculteit Geneeskunde en bij de afdeling Chirurgie van het UMCG). |
Voorzitter werkgroep richtlijn Algemene Chirurgie; Werkzaam in het Isala Ziekenhuis te Zwolle als interim in het kader van ondersteuning leiderschap; Begeleiding diverse maatschappen medische specialisten in het kader van interne communicatie uitdagingen - toekomst perspectief ontwikkeling (onder andere via BeBright); Bijdragen leveren aan diverse leergangen op het gebied van leiderschap; Voorzitter Stichting MIMIC (Meaningful Music in Health Care); Moderator in het HMC voor het Pro-RAAK programma (interprofessionele ontwikkeling bij verpleegkundigen en musici); Hoofd- en eindredacteur Leerboek Chirurgie (verschijnt in 2021). |
Persoonlijke relaties: Het advies kan potentieel de muziek praktijk van 'life performing' musici beïnvloeden. In mijn vriendenkring en in de Stichting MIMIC zitten musici. Wat hierbij van belang is om te weten dat de conservatoria in Den Haag en Groningen, waarmee ik een relatie heb, onderwijs modules hebben, die zich richten op onderwijs in 'personalised improvisation in music'. Dus, deze muziek praktijk is al geïnstitutionaliseerd.
Extern gefinancierd onderzoek: Het Pro-Raak programma betreft de interprofessionele ontwikkeling tussen verpleegkundigen en musici. Als zodanig zal de uitkomst van dit project (gefinancierd door de (semi)overheid) en de te ontwikkelen richtlijn geen direct effect hebben op de muziek praktijk in zorginstellingen. Bovendien betreft dit programma live-muziek postoperatief bij kwetsbare ouderen. De richtlijn ontwikkeling betreft alle vormen van muziek gedurende het gehele perioperatieve proces bij alle leeftijdsklassen. |
Geen |
|
Jeekel |
Hoogleraar Erasmus MC Rotterdam |
Geen |
Persoonlijke financiële belangen: Geen financieel voordeel. Het onderzoek wordt niet gefinancierd door industrie of overheid. De fondsen hebben geen enkel belang.
Extern gefinancierd onderzoek: Het onderzoek wordt niet gefinancierd door industrie of overheid De fondsen hebben geen enkel belang.
Intellectuele belangen en reputatie: Kan me niet voorstellen dat de ontwikkeling van een richtlijn enig effect zal hebben op bescherming van positie/reputatie, Boegbeeld functie bij patiënten of beroepsorganisatie is niet aan de orde. |
Geen |
|
Pierik |
Chirurg, Isala Zwolle |
Niet van toepassing |
Niet van toepassing |
Geen |
|
Habets |
Verpleegkundig Consulent, Verplegingswetenschapper, Vakgroep Ouderengeneeskunde, Zuyderland MC, Sittard-Geleen Seniordocent, Faculteit Gezondheidszorg, Zuyd Hogeschool, Heerlen |
Ik ben voorzitter van de Geriatrie Giants (www.geriatricgiants.nl) een non profit organisatie met als doelstelling het organiseren van inspiratie bijeenkomsten ten behoeve van verpleegkundigen en verzorgenden werkzaam in de ouderenzorg in Zuid Limburg (geriatriesalons, congres) |
Geen |
Geen |
|
Mattace Raso |
Hoogleraar Geriatrie EUR, hoofd sector geriatrie Erasmus MC, opleider klinische geriatrie Erasmus MC. |
Geen |
Geen |
Geen |
|
Spijkers |
Senior Adviseur Patiëntbelang |
Niet van toepassing |
Niet van toepassing |
Geen |
|
Van Munster |
Musicus, ik werk als zelfstandig ondernemer. Onder andere werkzaam bij stichting Mimic muziek in Promimic. |
Geen |
Persoonlijke financiële belangen: De richtlijn zou meer werk kunnen genereren voor mij als musicus |
Actie: wordt niet betrokken bij de besluitvorming rondom live muziek |
|
Prozée |
Verpleegkundig specialist chirurgische oncologie UMC Groningen |
Niet van toepassing |
Niet van toepassing |
Geen |
|
Van Vliet |
intensivist, Haaglanden Medisch Centrum |
Docent CTG (IC practitioner opleidingen) – betaald Toegevoegd september 2022: Docent IC verpleegkundige opleiding LUMC |
Toegevoegd september 2022: bestuurslid MuzIC |
Geen |
|
Lagrand |
Intensivist, Amsterdam UMC
|
Overige commissies: echografie commissie NVIC |
Extern gefinancierd onderzoek: Nu niet van toepassing. Mogelijk in de toekomst: deelname aan onderzoek waarde muziek bij behandeling van patiënten op de IC. |
Geen |
|
Kühlmann |
AIOS Anesthesiologie St. Antoniusziekenhuis, Nieuwegein --> 1.0 FTE Momenteel gedetacheerd in Jeroen Boschziekenhuis, Den Bosch |
Geen |
Intellectuele belangen en reputatie: 2014-2018 promotieonderzoek verricht naar de toepassing van muziekinterventies in de gezondheidszorg, zoals perioperatieve muziekinterventies, muziekinterventies bij hypertensie, effect van muziekinterventies in fundamenteel onderzoek. In september 2019 gepromoveerd op dit onderzoek. |
Geen |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door het uitnodigen van de Patiëntenfederatie om deel te nemen in de werkgroep en deel te nemen aan de schriftelijke knelpuntenanalyse. Het verslag hiervan (zie aanverwante producten) is besproken in de werkgroep. De verkregen input is meegenomen bij het opstellen van de uitgangsvragen, de keuze voor de uitkomstmaten en bij het opstellen van de overwegingen. De conceptrichtlijn is tevens voor commentaar voorgelegd aan Patiëntenfederatie Nederland.
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerden de werkgroep de knelpunten met betrekking tot het aanbieden van muziek aan volwassen patiënten die klinisch geopereerd worden, onder algehele en regionale anesthesie. Tevens zijn er knelpunten aangedragen door de NVKG en NVZ via een schriftelijke knelpuntenanalyse. Een verslag hiervan is opgenomen onder aanverwante producten. Op basis van de uitkomsten van de knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur en de beoordeling van de risk-of-bias van de individuele studies is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello, 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE-methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodules worden aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren zullen worden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren worden de conceptrichtlijnmodules aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule wordt aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd. De NVAM is in een later stadium betrokken, namens de voorzitter Remko ter Riet zijn een aantal aanvullingen gedaan waarna de NVAM de modules in juni 2023 heeft geautoriseerd
WKKGZ
|
Module |
Uitkomst kwalitatieve raming |
Toelichting |
|
Module ‘Muziek tijdens het preoperatieve proces’ |
geen substantiële financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (>40.000 patiënten), volgt ook uit de toetsing dat het geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners betreft en het geen wijziging in het opleidingsniveau van zorgpersoneel betreft. Er worden daarom geen substantiële financiële gevolgen verwacht
|
|
Module ‘Muziek tijdens het intraoperatieve proces’ |
geen substantiële financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (>40.000 patiënten), volgt ook uit de toetsing dat het geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners betreft en het geen wijziging in het opleidingsniveau van zorgpersoneel betreft. Er worden daarom geen substantiële financiële gevolgen verwacht
|
|
Module ‘Muziek tijdens het postoperatieve proces’ |
geen substantiële financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (>40.000 patiënten), volgt ook uit de toetsing dat het geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners betreft en het geen wijziging in het opleidingsniveau van zorgpersoneel betreft. Er worden daarom geen substantiële financiële gevolgen verwacht
|
|
Module ‘Muziek tijdens het perioperatieve proces’ |
geen substantiële financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn (>40.000 patiënten), volgt ook uit de toetsing dat het geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners betreft en het geen wijziging in het opleidingsniveau van zorgpersoneel betreft. Er worden daarom geen substantiële financiële gevolgen verwacht
|
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Jaeschke R, Vist GE, Williams JW Jr, Kunz R, Craig J, Montori VM, Bossuyt P, Guyatt GH; GRADE Working Group. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ. 2008 May 17;336(7653):1106-10. doi: 10.1136/bmj.39500.677199.AE. Erratum in: BMJ. 2008 May 24;336(7654). doi: 10.1136/bmj.a139.
Schünemann, A Holger J (corrected to Schünemann, Holger J). PubMed PMID: 18483053; PubMed Central PMCID: PMC2386626.
Wessels M, Hielkema L, van der Weijden T. How to identify existing literature on patients' knowledge, views, and values: the development of a validated search filter. J Med Libr Assoc. 2016 Oct;104(4):320-324. PubMed PMID: 27822157; PubMed Central PMCID: PMC5079497.
Zoekverantwoording
Zoekverantwoording
Algemene informatie
|
Richtlijn: Muziek tijdens het peri-operatief proces |
|
|
Uitgangsvraag: Wat is de effectiviteit van muziek (opgenomen of live) op de patiënt bij het pre/per/post operatief proces? |
|
|
Database(s): Ovid/Medline, Embase, PsychInfo |
Datum: 23-11-2020 |
|
Periode: 2016-heden |
Talen: Engels, Nederlands |
|
Literatuurspecialist: Miriam van der Maten |
|
|
BMI zoekblokken: voor verschillende opdrachten wordt (deels) gebruik gemaakt van de zoekblokken van BMI-Online https://blocks.bmi-online.nl/ Bij gebruikmaking van een volledig zoekblok zal naar de betreffende link op de website worden verwezen. |
|
|
Toelichting en opmerkingen:
|
|
|
Te gebruiken voor richtlijnen tekst: In de databases Embase (Embase.com), Medline (OVID), PsychInfo (OVID) is op 23-11-2020 met relevante zoektermen gezocht naar systematische reviews en randomized controlled trials over de effectiviteit van muziek op de patiënt bij het pre-, per- en postoperatief proces?. De literatuurzoekactie leverde 472 unieke treffers op. |
|
Zoekopbrengst
|
|
Embase |
OVID/MEDLINE |
PsychInfo |
Ontdubbeld |
|
SRs |
125 |
79 |
31 |
152 |
|
RCT |
256 |
186 |
35 |
320 |
|
Totaal |
381 |
265 |
66 |
472 |
Zoekstrategie
Embase
|
No. |
Query |
Results |
|
#8 |
#6 OR #7 |
381 |
|
#7 |
#3 AND #5 NOT #6 = RCT |
256 |
|
#6 |
#3 AND #4 = SR |
125 |
|
#5 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
3163976 |
|
#4 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
683622 |
|
#3 |
#1 AND #2 AND ((english)/lim OR (dutch)/lim) AND (2016-2020)/py NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) |
848 |
|
#2 |
'music'/de OR 'music therapy'/de OR music:ti,ab,kw OR musical:ti,ab,kw OR musicotherap*:ti,ab,kw |
32245 |
|
#1 |
'surgery'/exp OR 'obstetric operation'/exp OR 'postoperative complication'/exp OR 'anesthesiological procedure'/exp OR 'perioperative nursing'/de OR 'postanesthesia nursing'/de OR 'operating room'/de OR 'recovery room'/de OR 'operating room personnel'/de OR surger*:ti,ab,kw OR surgic*:ti,ab,kw OR peroperat*:ti,ab,kw OR perioperat*:ti,ab,kw OR preoperat*:ti,ab,kw OR postoperat*:ti,ab,kw OR operati*:ti,ab,kw OR interoperat*:ti,ab,kw OR intraoperat*:ti,ab,kw OR anesthe*:ti,ab,kw OR anaesthe*:ti,ab,kw OR perianesthe*:ti,ab,kw OR peranesthe*:ti,ab,kw OR perianaesthe*:ti,ab,kw OR peranaesthe*:ti,ab,kw OR preanasthe*:ti,ab,kw OR preanaesthe*:ti,ab,kw OR postanasthe*:ti,ab,kw OR postanaesthe*:ti,ab,kw OR surgery:lnk OR 'surgeon'/exp OR surgeon*:ti,ab,kw |
7425789 |
Ovid/Medline
|
# |
Searches |
Results |
|
9 |
7 or 8 |
265 |
|
8 |
(4 and 6) not 7 = RCT |
186 |
|
7 |
4 and 5 = SR |
79 |
|
6 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2228666 |
|
5 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
486188 |
|
4 |
limit 3 to (english language and yr="2016 -Current") |
655 |
|
3 |
1 and 2 |
2325 |
|
2 |
music/ or "music therapy"/ or (music or musical or musicotherap*).ti,ab,kf. |
26210 |
|
1 |
exp "Surgical Procedures, Operative"/ or exp "postoperative complications"/ or "Anesthesiology"/ or "perioperative nursing"/ or "Operating Rooms"/ or "recovery room"/ or (surger* or surgic* or peroperat* or perioperat* or preoperat* or postoperat* or operati* or interoperat* or intraoperat* or anesthe* or anaesthe* or perianesthe* or peranesthe* or perianaesthe* or peranaesthe* or preanasthe* or preanaesthe* or postanasthe* or postanaesthe*).ti,ab,kf. or surgery.xs. or exp surgeons/ or surgeon*.ti,ab,kf. or exp anesthesia/ |
5001579 |
PsychInfo
|
# |
Searches |
Results |
|
9 |
7 or 8 |
66 |
|
8 |
(4 and 6) not 7 = RCT |
35 |
|
7 |
4 and 5 = SR |
31 |
|
6 |
exp clinical trial/ or randomized controlled trial/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
250319 |
|
5 |
((literature review or systematic review or meta analysis).md. or "literature review"/ or meta analysis/ or (((meta adj2 analy*) or metaanaly* or (synthes* adj2 (literature* or research* or studies or data)) or (pooled and analys*) or ((data adj1 pool*) and studies) or ((hand or manual or database* or computer*) adj1 search*) or (electronic adj1 (database* or data base or data bases))).ti,ab,id. or (bibliograph* or relevant journals or ((review* or overview*) adj9 (systematic* or methodologic* or quantitativ* or research* or literature* or studies or trial* or effective*))).ab.)) not (((retrospective* or record* or case* or patient*) adj1 review*) or ((patient* or review*) adj1 chart*)).ti,ab,id. |
326508 |
|
4 |
limit 3 to yr="2016 -Current" |
284 |
|
3 |
1 and 2 |
1280 |
|
2 |
music/ or "music therapy"/ or (music or musical or musicotherap*).ti,ab. |
37779 |
|
1 |
exp "Surgery"/ or "Surgical Patients"/ or exp "Postsurgical Complications"/ or exp "Surgical Complications"/ or "Anesthesiology"/ or (surger* or surgic* or peroperat* or perioperat* or preoperat* or postoperat* or operati* or interoperat* or intraoperat* or anesthe* or anaesthe* or perianesthe* or peranesthe* or perianaesthe* or peranaesthe* or preanasthe* or preanaesthe* or postanasthe* or postanaesthe*).ti,ab. or exp surgeons/ or surgeon*.ti,ab. or exp anesthesia/ |
216466 |
