Gastro-intestinale chirurgie
Uitgangsvraag
Wat zijn de effecten van gastro-intestinale chirurgie bij kinderen met downsyndroom?
Aanbeveling
Sterke aanbeveling voor:
Zorg in het preoperatieve traject voor een zo optimaal mogelijke pre-operatieve conditie.
Wees alert op postoperatieve complicaties, gezien het verhoogde risico hierop bij kinderen met downsyndroom.
Bespreek dit risico ook met ouders, met onder andere aandacht voor enterocolitis, voedingsproblemen, obstipatie en fecale incontinentie, met het doel deze problemen vroegtijdig te signaleren en behandelen.
Overwegingen
Aangeboren gastro-intestinale afwijkingen komen vaker voor bij downsyndroom (3-13%) in vergelijking met de algemene bevolking (15 per 10.000 geboortes) en zijn geassocieerd met aanzienlijke morbiditeit en mortaliteit. Volgens Europese prevalentiecijfers is de prevalentie in de algemene bevolking tussen 2005 en 2022 niet wezenlijk veranderd. De meest voorkomende afwijkingen zijn duodenum atresie/stenose/web (1-5%), anus atresie/stenose (1-4%), ziekte van Hirschsprung (1-3%), oesophagus atresie/tracheo-oesophageale fistel (0,3-0,8%) en pylorusstenose (0,3%). Chirurgische interventie is geïndiceerd en vaak geassocieerd met verschillende postchirurgische complicaties, zoals voedingsproblemen, obstipatie, enterocolitis. Aangezien deze complicaties belangrijke consequenties hebben voor de morbiditeit en mortaliteit bij kinderen met downsyndroom is het van belang om deze zorgvuldig in kaart te brengen om de gevolgen van gastro-intestinale aandoeningen en chirurgie beter te begrijpen en de alertheid van medici te verhogen.
Hoewel in deze module literatuuronderzoek breed werd ingezet konden alleen studies met cruciale uitkomstmaten geïncludeerd worden na chirurgische correctie van twee congenitale gastro-intestinale afwijkingen, namelijk duodenumobstructie en ziekte van Hirschsprung. Hieronder volgen de bevindingen, belangrijkste overwegingen en aanbevelingen.
Balans tussen gewenste en ongewenste effecten
Enterocolitis
Uit de gepoolde resultaten van acht studies blijkt dat downsyndroom is geassocieerd met een hoger risico op enterocolitis in kinderen die een operatieve ingreep ondergaan vanwege HD en dat het effect klinisch relevant is.
Mortaliteit
Kinderen met HD
Vier studies rapporteerden de uitkomst mortaliteit. Downsyndroom is geassocieerd met een hoger risico op mortaliteit in kinderen die een operatieve ingreep ondergaan vanwege HD, en het gevonden effect is klinisch relevant.
Kinderen met congenitale duodenumobstructie
Downsyndroom is geassocieerd met een hoger risico op mortaliteit in kinderen die een operatieve ingreep ondergaan vanwege congenitale duodenumobstructie, volgens de resultaten van drie studies. Het effect is klinisch relevant.
Toxisch megacolon
Er werd geen bewijs gevonden voor de uitkomst toxisch megacolon.
Overige complicaties in de buikholte
Kinderen met HD
Eén studie rapporteerde de uitkomst overige complicaties in de buikholte in kinderen die een operatieve ingreep ondergaan vanwege HD. Downsyndroom is geassocieerd met een hoger risico op overige complicaties in de buikholte, het effect is klinisch relevant.
Kinderen met congenitale duodenumobstructie
Eén studie rapporteerde de uitkomst overige complicaties in de buikholte in kinderen die een operatieve ingreep ondergaan vanwege congenitale duodenumobstructie. Downsyndroom is geassocieerd met een lager risico op overige complicaties in de buikholte, het effect is klinisch relevant.
Constipatie
Vijf studies rapporteerden de uitkomst constipatie. Downsyndroom is geassocieerd met een hoger risico op constipatie in kinderen die een operatieve ingreep ondergaan vanwege HD, en het effect is klinisch relevant.
Incontinentie en soiling
Uit de gepoolde resultaten van vier studies blijkt dat downsyndroom geassocieerd is met een hoger risico op incontinentie en soiling in kinderen die een operatieve ingreep ondergaan vanwege HD. Het effect is voor beide uitkomsten klinisch relevant.
Voedingsproblemen
Eén studie in kinderen met congenitale duodenumobstructie toonde aan dat downsyndroom is geassocieerd met een lager risico op voedingsproblemen in kinderen die een operatieve ingreep ondergaan vanwege congenitale duodenumobstructie. Het effect is klinisch relevant.
In bestaande internationale richtlijnen (Marilyn 2022, Roche 2015) worden deze complicaties niet besproken en aldus geen adviezen gegeven voor eventuele pre- en peri-operatieve maatregelen om het risico op complicaties te verkleinen of voor de postoperatieve follow-up.
Ten aanzien van mortaliteit heeft de werkgroep in de geïncludeerde studies specifiek naar de gerapporteerde oorzaken gekeken. In veruit de meeste gevallen was de oorzaak van overlijden niet gerelateerd aan de chirurgische interventie maar aan andere oorzaken, zoals congenitale hartafwijkingen, aspiratiepneumonie, longhypoplasie, necrotiserende enterocolitis en werd 1 intra-operatief overlijden vermeld bij het intercurrent voorkomen van tracheo-oesophageale fistel.
Een aantal van de cruciale uitkomstmaten betreffen ziektebeelden die vaker voorkomen bij downsyndroom, ook wanneer geen chirurgische ingreep heeft plaatsgevonden, zoals obstipatie (19-25%, incontinentie (kinderen met downsyndroom zijn doorgaans op een latere leeftijd zindelijk voor urine en ontlasting (6-7 jaar) in vergelijking met de algemene bevolking (gemiddeld 3 jaar)) en voedingsproblemen (18-30% en volgens AAP richtlijn zelfs 31-80%) (Bermudez 2019, Lagan 2020, Ravel 2020). De informatie betreffende deze uitkomstmaten is op basis van de verrichte literatuurstudie in deze module slechts gerelateerd aan één van beide congenitale gastro-intestinale afwijkingen waarvan studies geïncludeerd konden worden en niet aan beide.
De gerapporteerde complicaties in de geïncludeerde studies traden zowel binnen enkele dagen post-operatief als >30 dagen tot wel 3 en 6 jaar postoperatief op.
Hoewel obstipatie als postoperatieve complicatie na chirurgische interventie vanwege de ziekte van Hirschsprung vaker (44%) lijkt voor te komen dan in zijn algemeenheid bij downsyndroom, is het heel goed mogelijk dat de pre-operatieve conditie van de darmen van langer bestaande obstipatie tgv de ziekte van Hirschsprung bijdraagt aan de postoperatieve conditie. De kans is groot dat de chirurgische interventie in dat geval niet heeft geleid tot obstipatie en obstipatie in dat geval niet beschouwd kan worden als postoperatieve complicatie. Datzelfde geldt voor incontinentieklachten en voedingsproblemen. Bij voedingsproblemen valt op dat dit opvallend weinig voorkwam als postoperatieve complicatie terwijl dit in het algemeen bij downsyndroom veelvuldig voorkomt.
Kwaliteit van bewijs
1. Kinderen die een operatieve ingreep ondergaan vanwege HD
De overall kwaliteit van bewijs is zeer laag. Dit betekent dat we zeer onzeker zijn over het gevonden geschatte effect van de cruciale uitkomstmaten.
Er is afgewaardeerd vanwege:
Zeer ernstige risk of bias: methodologische beperkingen (twee niveaus). Inclusie- en exclusiecriteria werden niet altijd duidelijk beschreven, in sommige studies werden niet alle belangrijke variabelen van de nulmeting beschreven, en de uitval was hoog in enkele studies en werd niet voldoende beschreven. Ook werd er niet altijd een standaarddefinitie van de uitkomst gebruikt en werd er niet gecorrigeerd voor relevante confounders.
(Zeer) ernstige imprecisie: onnauwkeurigheid, omdat het betrouwbaarheidsinterval de grens/beide grenzen van klinische relevantie overschrijdt of extreem breed is.
2. Kinderen die een operatieve ingreep ondergaan vanwege congenitale duodenumobstructie
De overall kwaliteit van bewijs is zeer laag. Dit betekent dat we zeer onzeker zijn over het gevonden geschatte effect van de cruciale uitkomstmaten.
Er is afgewaardeerd vanwege:
Zeer ernstige risk of Bias (twee niveaus): methodologische beperkingen. Inclusie- en exclusiecriteria werden niet altijd duidelijk beschreven, en de uitval was hoog in enkele studies en werd niet voldoende beschreven. Ook werd er niet gecorrigeerd voor relevante confounders.
Waarden en voorkeuren van patiënten (en eventueel hun naasten/verzorgers)
Bespreek in het pre-operatieve traject met ouders/verzorgers het belang van een zo optimaal mogelijke conditie pre-operatief. De afwegingen t.a.v. de timing van de chirurgische ingreep zijn vaak complexer bij downsyndroom als er sprake is van comorbiditeit(en) maar ook vanwege het vermoedelijk verhoogde risico op postoperatieve complicaties.
Veel ouders vinden het belangrijk om de overwegingen van een arts te horen, ook al zijn die complex.
Ouders willen ook graag weten waar ze op moeten letten in het kader van postoperatieve complicaties. Veel ouders hebben behoefte om uitgelegd te krijgen wat na een operatie normaal is en wanneer ze contact met de arts moeten opnemen. Goede informatie over de route (wanneer direct bellen, wanneer bellen tijdens ‘kantooruren’, wanneer bellen met huisarts, etc.) met bijbehorende telefoonnummers is belangrijk.
Wanneer de situatie acuut is, en ouders minder uitgelegd krijgen, is het belangrijk dat ouders wel opgevangen worden en erkend wordt dat ze gevoelens van angst en machteloosheid ervaren.
Gewenste effecten
Hoewel de overall kwaliteit van bewijs zeer laag is voor alle cruciale uitkomstmaten, zijn de gevonden effecten van de cruciale uitkomstmaten klinisch relevant. Voor alle cruciale uitkomstmaten wordt een vergelijkbare trend gezien ten nadele van downsyndroom, behalve voor toxisch megacolon waarbij in het geheel geen bewijs kon worden gevonden. Deze trend is dat het risico op complicaties na gastro-intestinale chirurgie bij kinderen met downsyndroom groter is dan bij kinderen zonder downsyndroom. Dat komt overeen met de ervaring van de werkgroep. Voor de klinische praktijk betekent dit extra alertheid tijdens de follow-up na een gastro-intestinale chirurgische ingrepen bij kinderen met downsyndroom op mogelijke complicaties. Op deze manier kan indien geïndiceerd tijdig behandeling plaatsvinden.
In het algemeen geldt bij alle chirurgische ingrepen dat in het pre-operatieve traject gestreefd wordt naar een zo optimaal mogelijke lichamelijke conditie en wordt de ingreep, indien de klinische conditie van de patiënt dit toelaat, uitgesteld naar de meest wenselijke leeftijd om het risico op peri-operatieve complicaties te minimaliseren. Bij downsyndroom zijn deze pre-operatieve afwegingen meer complex omdat vaker sprake is van comorbiditeiten (met name cardiaal), maar ook vanwege de mogelijke trend dat postoperatieve complicaties (na gastro-intestinale chirurgie) vaker voorkomen, zoals hierboven beschreven. Voor een optimale pre-operatieve conditie is een goede voedingstoestand van belang naast optimale behandeling van eventuele comorbiditeiten. Hiervoor wordt in sommige studies aangeraden om in het pre-operatieve traject te screenen op oa cardiale aandoeningen en tevens tijdens laparotomie grondig op zoek te gaan naar eventuele bijkomende gastro-intestinale malformaties (Singh 2004).
Aanvullende adviezen ten aanzien van bijvoorbeeld (de keuze van) antibioticumprofylaxe of het al dan niet geven van probiotica vallen buiten bestek van deze module.
Kostenaspecten
De bevindingen danwel gevonden trend in deze module lever(-en)(-t) geen extra kosten op ten opzichte van de bestaande situatie. Het gaat om kennis die kan worden meegenomen in het pre-, post- en mogelijk ook peri-operatieve traject. De verwachting is dat dankzij deze kennis de kans op (een ernstiger beloop bij) postoperatieve complicaties eerder zal afnemen dan zal toenemen met als gevolg een reductie van de kosten. Het is ook mogelijk dat er geen wezenlijke verandering optreedt t.o.v. de bestaande situatie en de kosten vergelijkbaar zullen zijn. Een toename van kosten zou kunnen optreden wanneer deze kennis leidt tot vaker en langduriger behandelen van postoperatieve complicaties. Aangezien tijdig signaleren en behandelen doorgaans leidt tot minder intensief en langdurig behandelen is dit laatste onwaarschijnlijk.
Gelijkheid ((health) equity/equitable)
Verbetering van kennis t.a.v. de complexiteit van pre-operatieve afwegingen bij downsyndroom maakt de kans groter op een gunstiger peri- en postoperatieve beloop. Alertheid op het optreden van eventuele postoperatieve complicaties maakt tijdige aanpassingen en zo nodig behandeling mogelijk en daarmee het risico op een ongunstiger beloop bij downsyndroom kleiner. Beide aspecten leiden tot een (mogelijke) toename van gezondheidsgelijkheid van kinderen met downsyndroom t.o.v. kinderen zonder downsyndroom.
Aanvaardbaarheid:
Ethische aanvaardbaarheid
Aangezien de bevindingen danwel gevonden trend in deze module niet leiden tot een nieuwe interventie of aanpassing van een bestaande interventie is dit aspect niet van toepassing. De bevindingen in deze module leiden eerder tot meer zorgvuldigheid bij het nemen van pre-, post- en mogelijk ook peri-operatieve beslissingen en daarbij zijn geen ethische bezwaren te verwachten.
Duurzaamheid
De bevindingen danwel gevonden trend in deze module leid(-en)(-t) niet tot wezenlijke veranderingen van het bestaande beleid en daardoor spelen duurzaamheidsaspecten geen rol. Meer zorgvuldigheid bij het nemen van pre-, post- en peri-operatieve beslissingen en tijdige aanpassingen danwel behandeling bij postoperatieve complicaties leidt doorgaans tot efficiënter gebruik van beschikbare middelen, maar kan in het laatste geval mogelijk leiden tot een toename in gebruik van geneesmiddelen, zoals laxantia. Aangezien tijdig signaleren en behandelen doorgaans leidt tot minder intensief en langdurig behandelen is dit laatste onwaarschijnlijk.
Haalbaarheid
De bevindingen danwel gevonden trend in deze module leid(-en)(-t) verhogen zorgvuldigheid en alertheid tijdens het pre-, post- en peri-operatieve traject. Binnen de werkgroep bestaat geen twijfel over de haalbaarheid hiervan.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
De gevonden trend dat het risico op postoperatieve complicaties verhoogd is bij gastro-intestinale chirurgie bij kinderen met downsyndroom is acht de werkgroep van belang om mee te nemen ter bevordering van de zorgvuldigheid en alertheid in het pre-, post- en mogelijk ook peri-operatieve traject. De overall kwaliteit van bewijs is echter zeer laag, maar de gevonden effecten van de cruciale uitkomstmaten zijn klinisch relevant en laten een vergelijkbare trend zien.
Onderbouwing
Achtergrond
Congenital gastrointestinal malformations are more common in children with Down syndrome (DS) (prevalence 3-13%) than in children without Down syndrome (prevalence 15 per 10.000 live and still births) and are associated with serious morbidity and mortality (Bermudez 2019, Lagan 2020, Marilyn 2022). According to the European Prevalence charts and tables the overall prevalence of congenital gastrointestinal malformations is rather stable in the period 2005-2022. The most common disorders include esophageal atresia/tracheoesophageal fistula (0.3-0.8%), pyloric stenosis (0.3%), duodenal stenosis/web/atresia (1-5%), Hirschsprung’s Disease (HD) (1-3%), and anal stenosis/atresia (1-4%) (Ravel 2020). These conditions are surgically treated and are associated with several (post-surgical) complications, including feeding problems, obstipation, and enterocolitis. Because of the severe impact on the children’s health, it is important to map the risk of post-surgical complications, in order to better understand the consequences of gastrointestinal disorders and surgery in children with Down syndrome and improve awareness for clinicians.
Conclusies / Summary of Findings
1. Children who have undergone a gastrointestinal surgery for HD
Table 9. Summary of Findings – Down Syndrome versus no Down Syndrome with outcomes enterocolitis, mortality, toxic megacolon, other abdominal complications, constipation, incontinence, soiling, and feeding difficulties
Population: Children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
Intervention: Down Syndrome
Comparator: No Down Syndrome
|
Outcome Timeframe |
Study results and measurements |
Absolute effect estimates |
Certainty of the evidence (Quality of evidence) |
Summary |
|
|
No Down Syndrome |
Down Syndrome |
||||
|
Enterocolitis (critical)
|
Relative risk: 1.42 (95% CI 1.01 to 1.99) Based on data from 1230 participants in 8 studies
|
25 per 100 |
34 per 100 |
Very low Due to very serious risk of bias, due to serious imprecision1 |
The evidence is very uncertain about the risk of enterocolitis in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
(Hackam, 2003; Morabito, 2006; Travassos, 2011; Pini Prato, 2019; Kwendakwema, 2016; Le-Nguyen, 2019; Surana, 1994; Sakurai, 2020) |
|
Difference: 5 more per 100 (95% CI 9 fewer to 18 more) |
|||||
|
Mortality (critical)
|
Relative risk: 9.68 (95% CI 3.06 to 30.6) Based on data from 765 participants in 4 studies
|
2 per 100 |
11 per 100 |
Very low Due to very serious risk of bias, due to serious imprecision2 |
The evidence is very uncertain about the risk of mortality in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
(Hackam, 2003; Morabito, 2006; Travassos, 2011; Pini Prato, 2019) |
|
Difference: 9 more per 100 (95% CI 3 fewer to 21 more) |
|||||
|
Toxic megacolon (critical) |
- |
-
|
No GRADE |
No evidence was found regarding the risk of toxic megacolon in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery |
|
|
Other abdominal complications* (important) |
Relative risk: 1.90 (95% CI 0.61 to 5.89) Based on data from 114 participants in 1 study
|
21 Per 100
|
40 per 100 |
Very low Due to very serious imprecision3 |
The evidence is very uncertain about the risk of other abdominal complications in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
(Balela, 2023) |
|
Difference: 25 more per 100 (95% CI 14.0 more to 36.0 more) |
|||||
|
Constipation (important) |
Relative risk: 1.44 (95% CI 1.13 to 1.82) Based on data from 683 participants in 4 studies
|
26 per 100 |
44 per 100 |
Very low Due to very serious risk of bias, due to serious imprecision4 |
The evidence is very uncertain about the risk of constipation in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
(Hackam, 2003; Travassos, 2011; Menezes, 2005; Pini Prato, 2019) |
|
Difference: 15 more per 100 (95% CI 4 more to 26 more)
|
|||||
|
Incontinence (important)
|
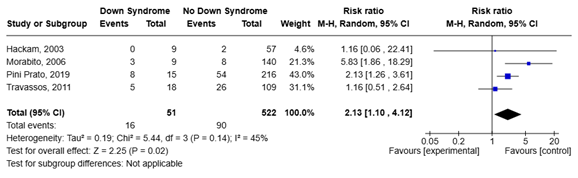
Relative risk: 2.13 (95% CI 1.1 to 4.12) Based on data from 573 participants in 4 studies
|
17 per 100 |
31 per 100 |
Very low Due to very serious risk of bias, due to serious imprecision5 |
The evidence is very uncertain about the risk of incontinence in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
(Hackam, 2003; Morabito, 2006; Travassos, 2011; Pini Prato, 2019) |
|
Difference: 12 more per 100 (95% CI 7 fewer to 31 more) |
|||||
|
Soiling (important)
|
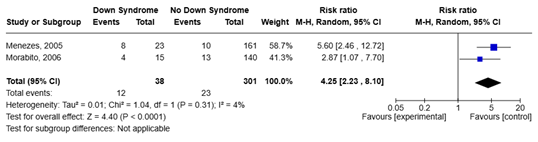
Relative risk: 4.25 (95% CI 2.23 to 8.10) Based on data from 339 participants in 2 studies
|
8 per 100 |
32 per 100 |
Very low Due to very serious risk of bias, due to serious imprecision6 |
The evidence is very uncertain about the risk of soiling in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery
(Morabito, 2006; Menezes, 2005) |
|
Difference: 24 more per 100 (95% CI 9 more to 39 more)
|
|||||
|
Feeding difficulties (important) |
- |
-
|
No GRADE |
No evidence was found regarding the risk of feeding difficulties in children with Down Syndrome when compared to children without Down Syndrome in children with Hirschsprung’s disease who have undergone a gastrointestinal surgery |
|
- Risk of Bias: very serious (-2 levels). Inclusion criteria and exclusion criteria were not always clearly defined, demographic information was missing for some studies, loss to follow-up was not always clearly reported, the outcome was not always clearly and consistently defined, and confounders were not taken into account. Imprecision: serious (-1 level). Confidence interval crosses one border of clinical significance;
- Risk of Bias: very serious (-2 levels). Inclusion criteria and exclusion criteria were not always clearly described, demographic information was not always reported, loss to follow-up was not always clearly reported, and confounders were not assessed. Imprecision: serious (-1 level). The confidence interval is very wide;
- Imprecision: very serious (-2 levels). The confidence interval crosses overlaps both borders of clinical significance.
- Risk of Bias: very serious (-2 levels). Inclusion criteria and exclusion criteria were not always clearly described, loss to follow-up was not always clearly reported, outcome measures were not always clearly defined, and no confounders were assessed. Imprecision: serious (-1 level). The confidence interval crosses one border of clinical significance;
- Risk of Bias: very serious (-2 levels). Inclusion criteria and exclusion criteria were not always clearly described, loss to follow-up was not always clearly reported, outcome measures were not always clearly defined, and no confounders were assessed. Imprecision: serious (-1 level). Confidence interval crosses one border of clinical significance;
- Risk of Bias: very serious (-2 levels). Inclusion criteria and exclusion criteria were not clearly described, loss to follow-up was not clearly reported, outcome measures were not always clearly defined, and no confounders were assessed. Imprecision: serious (-1 level). The confidence interval is very wide;
* Balela (2023) defined other abdominal complications as postoperative persistent obstructive symptoms: abdominal distension, bloating, borborygmi, vomiting, or severe constipation following pull-through
2. Children who have undergone a gastrointestinal surgery for congenital duodenal obstruction
Table 10. Summary of Findings – Down Syndrome versus no Down Syndrome with outcomes mortality, enterocolitis, toxic megacolon, other abdominal complications, feeding difficulties, constipation, incontinence, and soiling
Population: Children with congenital duodenal obstruction who have undergone a gastrointestinal surgery
Intervention: Down Syndrome
Comparator: No Down Syndrome
|
Outcome Timeframe |
Study results and measurements |
Absolute effect estimates |
Certainty of the evidence (Quality of evidence) |
Summary |
|
|
No Down Syndrome |
Down Syndrome |
||||
|
Mortality (critical) |
Relative risk: 3.05 (95% CI 1.85 to 5.01) Based on data from 381 participants in 3 studies
|
26 per 100 |
8 per 100 |
Very low Due to very serious risk of bias1 |
The evidence is very uncertain about the risk of mortality in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
Difference: 16 more per 100 (95% CI 9 more to 24 more) |
|||||
|
Enterocolitis (critical)
|
- |
-
|
No GRADE |
No evidence was found regarding the risk of enterocolitis in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
|
Toxic megacolon (critical)
|
- |
-
|
No GRADE |
No evidence was found regarding the risk of toxic megacolon in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
|
Other abdominal complications (important)
|
Relative risk: 0.69 (95% CI 0.14 to 3.30) Based on data from 76 participants in 1 study
|
7 per 100 |
10 per 100 |
Very low Due to very serious risk of bias, due to very serious imprecision2 |
The evidence is very uncertain about the risk of other abdominal complications in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
Difference: 3 less per 100 (95% CI 16 less to 10 more) |
|||||
|
Feeding difficulties (important)
|
Relative risk: 0.71 (95% CI 0.03 to 16.81) Based on data from 64 participants in 1 study Follow up 1 year |
2 per 100 |
0 per 100 |
Very low Due to very serious risk of bias3 |
The evidence is very uncertain about the risk of feeding difficulties in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery
|
|
Difference: 2 fewer per 100 (95% CI 11 fewer to 6 more)
|
|||||
|
Constipation (important)
|
- |
-
|
No GRADE |
No evidence was found regarding the risk of constipation in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
|
Incontinence (important)
|
- |
-
|
No GRADE |
No evidence was found regarding the risk of incontinence in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
|
Soiling (important)
|
- |
-
|
No GRADE |
No evidence was found regarding the risk of soiling in children with Down Syndrome when compared to children without Down Syndrome in children with congenital duodenal obstruction who have undergone a gastrointestinal surgery |
|
- Risk of Bias: very serious (-2 levels). Inclusion criteria and exclusion criteria were not always clearly described, loss to follow-up was not always clearly reported, and confounders were not always assessed;
- Risk of Bias: very serious (-2 levels). Complications were not clearly (pre-)defined, and no confounders were assessed. Imprecision: very serious (-2 levels). Confidence interval crosses both borders of clinical significance
- Risk of Bias: very serious (-2 levels). Loss to follow-up was not clearly reported, and no confounders were assessed.
Samenvatting literatuur
Description of studies
A total of 13 studies were included in the analysis of the literature. Important study characteristics and results are summarized in table 2. The assessment of the risk of bias is summarized in the risk of bias tables.
Hackam (2003) conducted an observational study in children with Hirschsprung’s disease (HD) undergoing surgery between 1 January 1995 and 31 December 2000. Children with a diagnosis of HD were included in this study. Exclusion criteria were having undergone surgery for HD at another institution or before the study period and having total colonic disease.
Morabito (2006) conducted an observational study in children with HD undergoing surgery between January 1990 and December 2006. Patients with confirmed Down syndrome and total colonic aganglionosis were included in this study. No exclusion criteria were defined.
Travassos (2011) conducted an observational study in children with HD undergoing surgery between March 1987 and August 2008. No further inclusion criteria and exclusion criteria were defined.
Menezes (2005) conducted an observational study in children with HD undergoing surgery between 1975 and 2003. No further inclusion criteria and exclusion criteria were defined.
Pini Prato (2019) conducted an observational study in children with HD undergoing surgery between January 1994 and December 2017. Inclusion criteria were HD diagnosis confirmed by an expert pathologist based on histochemistry on rectal suction biopsy or on histochemistry and histology on resected specimen, and Down syndrome confirmed at postnatal karyotype. Exclusion criteria were lack of data regarding extent of aganglionosis, surgery and/or outcome measures, and patients who are not being regularly followed up in the dedicated outpatient clinic.
Niramis (2010) conducted an observational study in children undergoing surgery for congenital intrinsic duodenal obstruction (CIDO) between 1997 and 2006. Additionally, they divided the groups of children with and without DS in children with and without congenital heart disease (CHD). No further inclusion criteria and exclusion criteria were defined.
Bethell (2020) conducted an observational study in children undergoing surgery for congenital duodenal obstruction (CDO) between 1 March 2016 and 1 March 2017. Inclusion criteria were live born cases of congenital occlusion or narrowing of the duodenum associated with atresia, stenosis, duodenal web, or annular pancreas, presenting prior to a post-conceptual age of 44 completed weeks, having undergone operative repair, and having a diagnosis of Down Syndrome or no other detected chromosomal abnormality. Exclusion criteria were cases of duodenal occlusion or narrowing caused by congenital bands associated with malrotation, intestinal volvulus, duplication cyst, or malignancy without an intrinsic duodenal abnormality.
Balela (2023) conducted an observational study in children with HD undergoing surgery between January 2017 and January 2022. Inclusion criteria were a diagnosis of HD, age <18 years, and undergoing a pull-through surgery at. Exclusion criteria were deceased patients and incomplete medical records.
Kwendakwema (2016) conducted an observational study in children with HD undergoing surgery between 2000 and 2015. A diagnosis of HD was the only inclusion criterion. Exclusion criteria were chromosomal anomalies other than trisomy 21 and patients with missing data.
Le-Nguyen (2019) conducted an observational study in children with HD undergoing surgery between January 1990 and December 2017. Exclusion criteria were children with early deaths owing to severe and complex malformations (mostly cardiac), patients with incomplete information about enterocolitis, and patients with missing data.
Surena (1994) conducted an observational study in children with HD undergoing surgery between 1975 and 1992. No further inclusion and exclusion criteria were defined.
Sakurai (2020) conducted an observational study in children with HD undergoing surgery between 2004 and 2018. Exclusion criteria were having undergone surgery in other hospitals, children on parenteral nutrition without radical surgery due to severe extensive aganglionosis, and children who underwent radical surgery at over one year of age.
Singh (2004) conducted an observational study in children with congenital duodenal obstruction who were diagnosed between January 1991 and April 2002 and underwent surgery. Exclusion criteria were patients with extrinsic duodenal obstruction caused by peritoneal bands or annular pancreas.
Table 2. Characteristics of included studies
*For further details, see risk of bias table in the appendix
1N estimated based on percentages provided
2Only provided for total study population or other subgroups as specified
Results
1. Enterocolitis
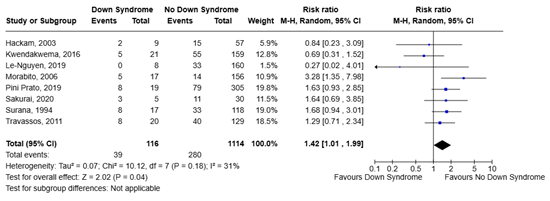
Eight studies reported the outcome enterocolitis, all in children with HD. The results are presented in Table 3. A pooled RR of 1.42 (95% CI 1.01 to 1.99) was calculated, meaning that Down syndrome is associated with a higher risk of postoperative enterocolitis, when compared to no Down syndrome. This is considered a clinically relevant difference between the two groups. The results are also shown in Figure 1.
Table 3. Postoperative enterocolitis in children with HD: DS versus no DS
|
Author, year |
Proportion of children with postoperative enterocolitis |
Relative risk (95% CI) |
|
|
Children with DS |
Children without DS |
||
|
Hackam, 2003 |
2/9 (22%) |
15/57 (26%) |
0.84 (0.23 to 3.09) |
|
Morabito, 2006 |
5/17 (29%) |
14/156 (9%) |
3.28 (1.35 to 7.98) |
|
Travassos, 2011 |
8/20 (40%) |
40/129 (31%) |
1.29 (0.71 to 2.34) |
|
Pini Prato, 2019 |
8/19 (42%) |
79/305 (26%) |
1.63 (0.93 to 2.85) |
|
Kwendakwema, 2016 |
5/21 (24%) |
55/159 (35%) |
0.69 (0.31 to 1.52) |
|
Le-Nguyen, 2019 |
0/8 (0%) |
33/160 (21%) |
0.27 (0.02 to 4.01) |
|
Surana, 1994 |
8/17 (47%) |
33/118 (28%) |
1.68 (0.94 to 3.01) |
|
Sakurai, 2020 |
3/5 (60%) |
11/30 (37%) |
1.64 (0.69 to 3.85) |
|
All studies pooled |
39/116 (34%) |
280/1114 (25%) |
1.42 (1.01 to 1.99)1 |
1The difference between the groups is clinically relevant
Figure 1. Forest plot of postoperative enterocolitis in children with HD: DS versus no DS
2. Mortality
Seven studies reported the outcome mortality, four in children with HD, and three in children with congenital duodenal obstruction. Cause of death was not always reported, but was often not directly related to surgery.
2.1. Children who have undergone a gastrointestinal surgery for HD
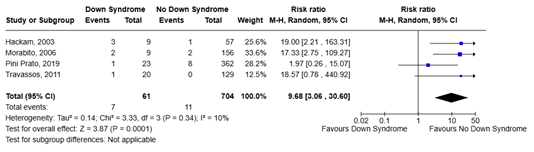
The results are presented in Table 4. A pooled RR of 9.68 (95% CI 3.06 to 30.60) was calculated, meaning that DS is associated with a higher risk of mortality, when compared to no DS. This is a clinically relevant difference between the two groups. The results are also shown in Figure 2.
Table 4. Mortality in children with HD: DS versus no DS
|
Author, year |
Proportion of children that died during follow-up |
Relative risk (95% CI) |
|
|
Children with DS |
Children without DS |
||
|
Hackam, 2003 |
3/9 (33%) |
1/57 (2%) |
19.00 (2.21 to 163.31) |
|
Morabito, 2006 |
2/9 (22%) |
2/156 (1%) |
17.33 (2.75 to 109.27) |
|
Travassos, 2011 |
1/20 (5%) |
0/129 (0%) |
18.57 (0.78 to 440.92) |
|
Pini Prato, 2019 |
1/23 (4%) |
8/362 (2%) |
1.97 (0.26 to 15.07) |
|
All studies pooled |
7/61 (11%) |
11/704 (2%) |
9.68 (3.06 to 30.60)1 |
1The difference between the groups is clinically relevant
Figure 2. Forest plot of mortality in children with HD: DS versus no DS
2.2 Children who have undergone a gastrointestinal surgery for congenital duodenal obstruction
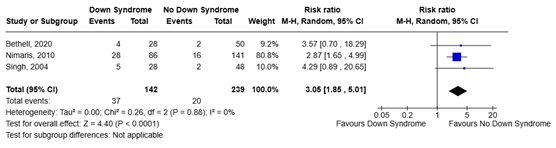
Niramis (2010), Bethell (2020), and Singh (2004) examined mortality in children with congenital duodenal obstruction. The results are presented in Table 5. A pooled RR of 3.05 (95% CI 1.85 to 5.01) was calculated, meaning that DS is associated with a higher risk of mortality, when compared to no DS. This is a clinically relevant difference between the two groups. The results are also shown in Figure 3.
Table 5. Mortality in children with congenital duodenal obstruction: DS versus no DS
|
Author, year |
Proportion of children that died during follow-up |
Relative risk (95% CI) |
|
|
Children with DS |
Children without DS |
||
|
Niramis, 2010 |
28/86 (31%) |
16/141 (11%) |
2.87 (1.65 to 4.99) |
|
Bethell, 2020 |
4/28 (15%) |
2/50 (4%) |
3.57 (0.70 to 18.29) |
|
Singh, 2004 |
5/28 (18%) |
2/48 (4%) |
4.29 (0.89 to 20.65) |
|
Both studies pooled |
37/142 (26%) |
20/239 (8%) |
3.05 (1.85 to 5.01)1 |
1The difference between the groups is clinically relevant
Figure 3. Forest plot of mortality in children with congenital duodenal obstruction: DS versus no DS
Subgroup of children with congenital heart disease (CHD)
Niramis (2010) additionally examined mortality in a subgroup of children with CHD. 18 of 49 children (37%) of children with DS died during follow-up, compared to 11 of 25 children (44%) without DS, RR = 0.83 (95% CI 0.47 to 1.49). This is not a clinically relevant difference between the groups.
Subgroup of children without congenital heart disease (CHD)
Niramis (2010) also evaluated mortality in a subgroup of children without CHD. 10 of 37 children (27%) with DS died during follow-up, compared to 5 of 116 children (4%) without DS, RR = 6.27 (95% CI 2.29 to 17.18). This is a clinically relevant difference between the groups.
3. Toxic megacolon
No evidence was found for the outcome toxic megacolon.
4. Other abdominal complications
Two studies reported the outcome other abdominal complications. Balela (2023) assessed persistent obstructive symptoms in children with HD, and Singh (2004) evaluated complications in children with congenital duodenal obstruction.
4.1 Children who have undergone a gastrointestinal surgery for HD
Balela (2023) reported that 2 of 5 children (40%) in the DS group experienced persistent obstructive symptoms, compared to 23 of 109 children (21%) in the no DS group, RR = 1.90 (95% CI 0.61 to 5.89) and OR = 2.49 (95% CI 0.39 to 15.81). After adjusting for type of surgery, sex, age at surgery, aganglionosis type, and global developmental delay, OR = 2.63 (95% CI 0.38 to 18.08). This is a clinically relevant difference.
4.2 Children who have undergone a gastrointestinal surgery for congenital duodenal obstruction
Singh (2004) reported that 2 of 28 children (7%) in the DS group experienced complications, compared to 5 of 48 children (10%) in the no DS group, RR = 0.69 (95% CI 0.14 to 3.30). This is considered a clinically relevant difference between the groups.
5. Constipation
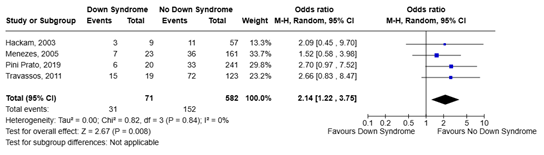
Five studies reported the outcome constipation, all in children with HD. The results are presented in Table 6. A pooled RR of 1.44 (95% CI 1.13 to 1.82) was calculated, meaning that DS is associated with a higher risk of constipation, when compared to no DS. This is a clinically relevant difference between the two groups. The results are also shown in Figure 4.
Table 6. Constipation in children with HD: DS versus no DS
|
Author, year |
Proportion of children with constipation |
Relative risk (95% CI) |
|
|
Children with DS |
Children without DS |
||
|
Hackam, 2003 |
3/9 (33%) |
11/57 (19%) |
1.73 (0.60 to 5.01) |
|
Travassos, 2011 |
15/19 (79%) |
72/123 (59%) |
1.35 (1.02 to 1.78) |
|
Menezes, 2005 |
7/23 (30%) |
36/161 (22%) |
1.36 (0.69 to 2.69) |
|
Pini Prato, 2019 |
6/20 (30%) |
33/241 (14%) |
2.19 (1.04 to 4.60) |
|
All studies pooled |
31/71 (44%) |
152/582 (26%) |
1.44 (1.13 to 1.82)1 |
1The difference between the groups is clinically relevant
Figure 4. Forest plot of constipation in children with HD: DS versus no DS
6. Incontinence and soiling
Incontinence
Four studies reported the outcome incontinence, all in children with HD. The results are presented in Table 7. A pooled RR of 2.13 (95% CI 1.10 to 4.12) was calculated, meaning that DS is associated with a higher risk of incontinence, when compared to no DS. This is a clinically relevant difference between the two groups. The results are also shown in Figure 5.
Table 7. Incontinence in children with HD: DS versus no DS
|
Author, year |
Proportion of children with incontinence
|
Relative risk (95% CI) |
|
|
Children with DS |
Children without DS |
||
|
Hackam, 2003 |
0/9 (0%) |
2/57 (4%) |
1.16 (0.06 to 22.41) |
|
Morabito, 2006 |
3/9 (33%) |
8/140 (6%) |
5.83 (1.86 to 18.29) |
|
Travassos, 2011 |
5/18 (28%) |
26/109 (24%) |
1.16 (0.51 to 2.64) |
|
Pini Prato, 2019 |
8/15 (53%) |
54/216 (14%) |
2.13 (1.26 to 3.61) |
|
All studies pooled |
16/51 (31%) |
90/522 (17%) |
2.13 (1.10 to 4.12)1 |
1The difference between the groups is clinically relevant
Figure 5. Forest plot of incontinence in children with HD: DS versus no DS
Soiling
Two studies reported the outcome soiling, both in children with HD. The results are presented in Table 8. A pooled RR of 4.25 (95% CI 2.23 to 8.10) was calculated, meaning that DS is associated with a higher risk of incontinence, when compared to no DS. This is a clinically relevant difference between the two groups. The results are also shown in Figure 6.
Table 8. Soiling in children with HD: DS versus no DS
|
Author, year |
Proportion of children for whom soiling occurred |
Relative risk (95% CI) |
|
|
Children with DS |
Children without DS |
||
|
Morabito, 2006 |
4/15 (27%) |
13/140 (9%) |
2.87 (1.07 to 7.70) |
|
Menezes, 2005 |
8/23 (35%) |
10/161 (6%) |
5.60 (2.46 to 12.72) |
|
Both studies pooled |
12/38 (32%) |
23/301 (8%) |
4.25 (2.23 to 8.10)1 |
1The difference between the groups is clinically relevant
Figure 6. Forest plot of soiling in children with HD: DS versus no DS
7. Feeding difficulties
Having achieved full enteral feeds
One study in children with congenital duodenal obstruction reported the outcome feeding difficulties. Bethell (2020) reported that 0 of 20 children (0%) in the DS group had not achieved full enteral feeds 1 year post-surgery, compared to 1 of 44 children (2%) in the no DS group, RR = 0.71 (95% CI 0.03 to 16.81). This is a clinically relevant difference between the groups.
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question(s):
What is the risk of complications in children with DS undergoing a gastrointestinal surgery?
Table 1. PICO
|
Patients |
Children who have undergone a gastrointestinal surgery |
|
Intervention |
Down syndrome |
|
Control |
No Down syndrome |
|
Outcomes |
Enterocolitis, mortality, toxic megacolon, constipation, incontinence and soiling, feeding difficulties, other abdominal complications (all outcomes occurring postoperative, during a follow-up period >30 days) |
|
Other selection criteria |
Study design: systematic reviews and meta-analyses, randomized controlled trials (RCTs), comparative observational studies |
Relevant outcome measures
The guideline panel considered enterocolitis, mortality and toxic megacolon as critical outcome measures for decision making; and constipation, incontinence and soiling, feeding difficulties, and other abdominal complications as important outcome measures for decision making.
The guideline panel defined a difference of 25% (0.8 ≥ RR ≥ 1.25) as minimal clinically (patient) relevant difference.
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms until 8 May 2024. The detailed search strategy is listed under the tab ‘Literature search strategy’. The systematic literature search resulted in 453 hits. Studies were selected based on the following criteria: fitting PICO, published in 1990 or later, systematic reviews and or meta-analyses, RCTs, comparative observational studies. 23 studies were initially selected based on title and abstract screening. After reading the full text, 13 studies were excluded (see the table of excluded studies), and 10 studies were included. Three studies included in the review of Zhang (2023) were additionally included (Le-Nguyen, 2019; Sakurai, 2020; Surena, 1994).
Referenties
- Balela N, Fauzi AR, Nugroho N, Dwihantoro A, Gunadi. Prognostic factors for persistent obstructive symptoms in patients with Hirschsprung disease following pull-through. PLoS One. 2023 Sep 8;18(9):e0290430. doi: 10.1371/journal.pone.0290430. PMID: 37682877; PMCID: PMC10490837.
- Bermudez BEBV, de Oliveira CM, de Lima Cat MN, Magdalena NIR, Celli A. Gastrointestinal disorders in Down syndrome. Am J Med Genet A. 2019 Aug;179(8):1426-1431. doi: 10.1002/ajmg.a.61258. Epub 2019 Jun 10. PMID: 31183986
- Bethell GS, Long AM, Knight M, Hall NJ; BAPS-CASS. The impact of trisomy 21 on epidemiology, management, and outcomes of congenital duodenal obstruction: a population-based study. Pediatr Surg Int. 2020 Apr;36(4):477-483. doi: 10.1007/s00383-020-04628-w. Epub 2020 Feb 29. PMID: 32114651; PMCID: PMC7069923.
- Hackam DJ, Reblock K, Barksdale EM, Redlinger R, Lynch J, Gaines BA. The influence of Down's syndrome on the management and outcome of children with Hirschsprung's disease. J Pediatr Surg. 2003 Jun;38(6):946-9. doi: 10.1016/s0022-3468(03)00129-5. PMID: 12778399.
- Kwendakwema N, Al-Dulaimi R, Presson AP, Zobell S, Stevens AM, Bucher BT, Barnhart DC, Rollins MD. Enterocolitis and bowel function in children with Hirschsprung disease and trisomy 21. J Pediatr Surg. 2016 Dec;51(12):2001-2004. doi: 10.1016/j.jpedsurg.2016.09.026. Epub 2016 Sep 15. PMID: 27670962.
- Lagan N, Huggard D, Mc Grane F, Leahy TR, Franklin O, Roche E, Webb D, O' Marcaigh A, Cox D, El-Khuffash A, Greally P, Balfe J, Molloy EJ. Multiorgan involvement and management in children with Down syndrome. Acta Paediatr. 2020 Jun;109(6):1096-1111. doi: 10.1111/apa.15153. Epub 2020 Jan 24. PMID: 31899550.
- Le-Nguyen A, Righini-Grunder F, Piché N, Faure C, Aspirot A. Factors influencing the incidence of Hirschsprung associated enterocolitis (HAEC). J Pediatr Surg. 2019 May;54(5):959-963. doi: 10.1016/j.jpedsurg.2019.01.026. Epub 2019 Jan 31. PMID: 30808539.
- Marilyn J. Bull, Tracy Trotter, Stephanie L. Santoro, Celanie Christensen, Randall W. Grout, THE COUNCIL ON GENETICS; Health Supervision for Children and Adolescents With Down Syndrome. Pediatrics. 2022. 149 (5): e2022057010. 10.1542/peds.2022-057010
- Menezes M, Puri P. Long-term clinical outcome in patients with Hirschsprung's disease and associated Down's syndrome. J Pediatr Surg. 2005 May;40(5):810-2. doi: 10.1016/j.jpedsurg.2005.01.048. PMID: 15937820.
- Morabito A, Lall A, Gull S, Mohee A, Bianchi A. The impact of Down's syndrome on the immediate and long-term outcomes of children with Hirschsprung's disease. Pediatr Surg Int. 2006 Feb;22(2):179-81. doi: 10.1007/s00383-005-1617-0. Epub 2005 Dec 14. PMID: 16362310.
- Niramis R, Anuntkosol M, Tongsin A, Mahatharadol V. Influence of Down's syndrome on management and outcome of patients with congenital intrinsic duodenal obstruction. J Pediatr Surg. 2010 Jul;45(7):1467-72. doi: 10.1016/j.jpedsurg.2010.02.049. PMID: 20638526.
- Pini Prato A, Arnoldi R, Sgrò A, Felici E, Racca F, Nozza P, Mariani N, Mosconi M, Mazzola C, Mattioli G. Hirschsprung disease and Down syndrome: From the reappraisal of risk factors to the impact of surgery. J Pediatr Surg. 2019. 54(9):1838-1842. doi: 10.1016/j.jpedsurg.2019.01.053. Epub 2019 Feb 12. PMID: 30814038.
- Ravel A, Mircher C, Rebillat AS, Cieuta-Walti C, Megarbane A. Feeding problems and gastrointestinal diseases in Down syndrome. Arch Pediatr. 2020 Jan;27(1):53-60. doi: 10.1016/j.arcped.2019.11.008. Epub 2019 Nov 26. PMID: 31784293
- Roche E, Hoey H, Murphy J. Medical Management of Children & Adolescents with Down Syndrome in Ireland. Url: https://downsyndrome.ie/wp-content/uploads/2018/03/Medical-Management-Guidelines-for-Children-and-Adolescents-with-Down-Syndrome-with-updates-2009-and-2015.pdf. 2015. Last accessed November 8, 2024.
- Sakurai T, Tanaka H, Endo N. Predictive factors for the development of postoperative Hirschsprung-associated enterocolitis in children operated during infancy. Pediatr Surg Int. 2021 Feb;37(2):275-280. doi: 10.1007/s00383-020-04784-z. Epub 2020 Nov 27. PMID: 33245447.
- Singh MV, Richards C, Bowen JC. Does Down syndrome affect the outcome of congenital duodenal obstruction? Pediatr Surg Int. 2004 Aug;20(8):586-9. doi: 10.1007/s00383-004-1236-1. Epub 2004 Aug 12. PMID: 15309469.
- Surana R, Quinn F, Puri P. Evaluation of risk factors in the development of enterocolitis complicating Hirschsprung’s disease. Pediatric surgery international. 1994. 1994;9(4):234–6.
- Travassos D, van Herwaarden-Lindeboom M, van der Zee DC. Hirschsprung's disease in children with Down syndrome: a comparative study. Eur J Pediatr Surg. 2011 Aug;21(4):220-3. doi: 10.1055/s-0031-1271735. Epub 2011 Feb 24. PMID: 21351043.
Evidence tabellen
Risk of Bias table
Table of quality assessment – prognostic factor (PF) studies
Based on: QUIPSA (Haydn, 2006; Haydn 2013)
|
Study reference
(first author, year of publication) |
Study participation
Study sample represents the population of interest on key characteristics?
Definitely yes Probably yes Probably no Definitely no No information |
Study Attrition
Loss to follow-up not associated with key characteristics (i.e., the study data adequately represent the sample)?
Definitely yes Probably yes Probably no Definitely no No information |
Prognostic factor measurement3
Was the PF of interest defined and adequately measured?
Definitely yes Probably yes Probably no Definitely no No information |
Outcome measurement
Was the outcome of interest defined and adequately measured?
Probably yes Probably no Definitely no No information |
Study confounding
Important potential confounders are appropriately accounted for?
Definitely yes Probably yes Probably no Definitely no No information |
Statistical Analysis and Reporting
Statistical analysis appropriate for the design of the study?
Probably yes Probably no Definitely no No information |
Overall judgement
High risk of bias Moderate risk of bias Low risk of bias |
|
Hackam, 2003 |
Conclusion:
Probably no
Reason:
Inclusion and exclusion criteria are not clearly defined in the methods section. It is only described in the results section which patients were excluded
|
Conclusion:
Definitely yes
Reason:
No loss to follow-up |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients |
Conclusion:
Definitely no
Reason:
It is not clear how incontinence and constipation are defined. |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH
|
|
Morabito, 2006 |
Conclusion:
Probably no
Reason:
Overall clear, but no exclusion criteria were defined, it is not clear if there were any |
Conclusion:
Definitely yes
Reason:
No loss to follow-up was reported |
Conclusion:
Definitely yes
Reason:
Assessment of Down Syndrome by chromosomal assessment |
Conclusion:
Definitely yes
Reason:
Outcome measures were clearly defined |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH |
|
Travassos, 2011 |
Conclusion:
Probably no
Reason:
It is not clear if there were any exclusion criteria, as this was not mentioned
|
Conclusion:
Probably yes
Reason:
Limited loss to follow-up, but reasons for missing outcome data not always clearly described |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Definitely yes
Reason:
Outcome measures were clearly defined |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH |
|
Menezes, 2005 |
Conclusion:
Probably no
Reason:
It is not clear if there were any exclusion criteria, as this was not mentioned
|
Conclusion:
Definitely no
Reason:
Large number of loss to follow-up, no comparison with those children who completed the study |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Probably no
Reason:
Soiling and incontinence were not defined. Measurement method was accurate |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH |
|
Pini Prato, 2019 |
Conclusion:
Probably yes
Reason:
Inclusion and exclusion criteria were clearly defined, but some baseline characteristics, such as age, were not reported |
Conclusion:
Definitely no
Reason:
Large number of loss to follow-up, no comparison with those children who completed the study |
Conclusion:
Definitely yes
Reason:
Assessment of Down Syndrome is clearly described |
Conclusion:
Definitely yes
Reason:
Outcome measures were clearly defined |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH |
|
Nimaris, 2010 |
Conclusion:
Probably no
Reason:
Recruitment and baseline characteristics are clearly described, but it is not clear if there are specific inclusion and exclusion criteria |
Conclusion:
Definitely yes
Reason:
Limited number of loss to follow-up |
Conclusion:
Definitely yes
Reason:
Assessment of Down Syndrome by chromosomal assessment and CHD was checked using patient records |
Conclusion:
Definitely no
Reason:
complications are not defined |
Conclusion:
Probably no
Reason:
Subgroup analyses based on CHD are performed, but no other confounders are considered |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH |
|
Bethell, 2020 |
Conclusion:
Definitely yes
Reason:
Study sample is clearly described |
Conclusion:
Definitely no
Reason:
large number of loss to follow-up, no comparison between participants who completed the study and those lost to follow-up |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely yes
Reason:
Outcome measures were clearly defined |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH
|
|
Balela, 2023 |
Conclusion:
Definitely yes
Reason:
Study sample is clearly described |
Conclusion:
Definitely yes
Reason:
No loss to follow-up |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely yes
Reason:
Outcome measure was clearly defined |
Conclusion:
Definitely yes
Reason:
Confounder-adjusted analyses were conducted |
Conclusion:
Definitely yes
Reason:
Multivariate logistic regression analysis was conducted |
LOW |
|
Kwendakwema, 2016 |
Conclusion:
Definitely yes
Reason: Study sample is clearly described |
Conclusion:
Definitely yes
Reason:
No loss to follow-up |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely no
Reason:
No standard definition of the outcome was used |
Definitely no
Reason:
no stratification or adjustment for confounders |
Definitely no
Reason:
No multivariate analyses are conducted |
HIGH |
|
Le-Nguyen, 2019 |
Conclusion:
Definitely yes
Reason:
Study sample is clearly described
|
Conclusion:
Probably yes
Reason:
Number of loss to follow-up was limited |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely no
Reason:
No standard definition of the outcome was used |
Conclusion:
Probably no
Reason:
Confounders are listed and included in univariate analysis. However, association between Down Syndrome and enterocolitis was not evaluated in a multivariate model |
Conclusion:
Definitely no
Reason:
No multivariate analyses are conducted for the association between Down Syndrome and enterocolitis |
HIGH |
|
Surana, 1994 |
Conclusion:
Definitely no
Reason:
inclusion and exclusion criteria were not clearly described, and basic descriptives, such as age of the study population, were not provided |
Conclusion:
Probably yes
Reason:
no loss to follow-up described |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely yes
Reason:
Enterocolitis was clearly defined and the same definition was used for all patients |
Conclusion:
Definitely no
Reason:
two potential confounders were reported, but no stratification or adjustments in the analyses were done |
Conclusion:
Definitely no
Reason:
No multivariate analyses are conducted for the association between Down Syndrome and enterocolitis |
HIGH |
|
Sakurai, 2020 |
Conclusion:
Probably yes
Reason:
exclusion criteria were clearly defined, it is not entirely clear if there were additional inclusion criteria |
Conclusion:
Definitely yes
Reason:
no loss to follow-up |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely yes
Reason:
Enterocolitis was clearly defined and the same definition was used for all patients |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses are conducted for the association between Down Syndrome and enterocolitis |
HIGH |
|
Singh, 2004 |
Conclusion:
Reason:
exclusion criteria were clearly defined, it is not entirely clear if there were additional inclusion criteria
|
Conclusion:
Definitely yes
Reason:
No loss to follow-up (postoperative) |
Conclusion:
Probably yes
Reason:
Assessment of Down Syndrome is not described, but it is likely that it was done in the same manner in all patients. |
Conclusion:
Definitely no
Reason:
Complications were not predefined |
Conclusion:
Definitely no
Reason:
no stratification or adjustment for confounders |
Conclusion:
Definitely no
Reason:
No multivariate analyses were conducted |
HIGH |
Table of excluded studies
|
Reference |
Reason for exclusion |
|
Sutthatarn P, Lapidus-Krol E, Smith C, Halaweish I, Rialon K, Ralls MW, Rentea RM, Madonna MB, Haddock C, Rocca AM, Gosain A, Frischer J, Piper H, Goldstein AM, Saadai P, Durham MM, Dickie B, Jafri M, Langer JC. Hirschsprung-associated inflammatory bowel disease: A multicenter study from the APSA Hirschsprung disease interest group. J Pediatr Surg. 2023 May;58(5):856-861. doi: 10.1016/j.jpedsurg.2023.01.018. Epub 2023 Jan 24. PMID: 36801072.
|
No comparison between patients with DS and patients without DS |
|
Dingemans AJM, Reck-Burneo CA, Fuchs M, Sanchez AV, Lane VA, Hoover E, Maloof T, Weaver L, Levitt MA, Wood RJ. Urinary Outcomes in Patients with Down's Syndrome and Hirschsprung's Disease. Eur J Pediatr Surg. 2019 Aug;29(4):378-383. doi: 10.1055/s-0038-1660509. Epub 2018 Jun 17. PMID: 29909603. |
Also includes patients who did not undergo surgery, and results are not presented separately |
|
Davidson JR, Kyrklund K, Eaton S, Pakarinen MP, Thompson D, Blackburn SC, Cross K, De Coppi P, Curry J. Outcomes in Hirschsprung's disease with coexisting learning disability. Eur J Pediatr. 2021 Dec;180(12):3499-3507. doi: 10.1007/s00431-021-04129-5. Epub 2021 Jun 11. PMID: 34115168; PMCID: PMC8589745. |
Wrong comparison |
|
Knaus ME, Pendola G, Srinivas S, Wood RJ, Halaweish I. Social Determinants of Health and Hirschsprung-associated Enterocolitis. J Pediatr Surg. 2023 Aug;58(8):1458-1462. doi: 10.1016/j.jpedsurg.2022.09.039. Epub 2022 Sep 30. PMID: 36371352. |
Outcome occurred before exposure in 33% of outcomes |
|
Menezes M, Puri P. Long-term outcome of patients with enterocolitis complicating Hirschsprung's disease. Pediatr Surg Int. 2006 Apr;22(4):316-8. doi: 10.1007/s00383-006-1639-2. Epub 2006 Feb 4. PMID: 16463033. |
Outcome occurred before exposure in an unknown proportion of outcomes |
|
Menezes M, Corbally M, Puri P. Long-term results of bowel function after treatment for Hirschsprung's disease: a 29-year review. Pediatr Surg Int. 2006 Dec;22(12):987-90. doi: 10.1007/s00383-006-1783-8. PMID: 17006709. |
Same study population and outcomes as the included study of Menezes (2005), but loss to follow-up and outcomes more clearly described in Menezes (2005) |
|
Zhang X, Sun D, Xu Q, Liu H, Li Y, Wang D, Wang J, Zhang Q, Hou P, Mu W, Jia C, Li A. Risk factors for Hirschsprung disease-associated enterocolitis: a systematic review and meta-analysis. Int J Surg. 2023 Aug 1;109(8):2509-2524. doi: 10.1097/JS9.0000000000000473. PMID: 37288551; PMCID: PMC10442125. |
Only the studies fitting the PICO were extracted from the review. This led to the inclusion of three new studies (Le-Nguyen, 2019; Surana, 1994; Sakurai, 2020) |
|
Miranda, Marcelo E., et al. "Congenital Duodenal Obstruction: The Impact of Down's Syndrome in Neonatal Morbidity. A Two-Center Survey." Current Pediatric Reviews 4.1 (2008): 15-18. |
Also includes patients who did not undergo surgery, and results are not presented separately |
|
Cairo SB, Zeinali LI, Berkelhamer SK, Harmon CM, Rao SO, Rothstein DH. Down Syndrome and Postoperative Complications in Children Undergoing Intestinal Operations. J Pediatr Surg. 2019 Sep;54(9):1832-1837. doi: 10.1016/j.jpedsurg.2018.11.013. Epub 2018 Dec 13. PMID: 30611525. |
Only short-term outcomes are reported |
|
Bartz-Kurycki MA, Anderson KT, Austin MT, Kao LS, Tsao K, Lally KP, Kawaguchi AL. Increased complications in pediatric surgery are associated with comorbidities and not with Down syndrome itself. J Surg Res. 2018 Oct;230:125-130. doi: 10.1016/j.jss.2018.04.010. Epub 2018 May 25. PMID: 30100027. |
Only short-term outcomes are reported |
|
Saberi RA, Gilna GP, Slavin BV, Huerta CT, Ramsey WA, O'Neil CF Jr, Perez EA, Sola JE, Thorson CM. Hirschsprung disease in Down syndrome: An opportunity for improvement. J Pediatr Surg. 2022 Jun;57(6):1040-1044. doi: 10.1016/j.jpedsurg.2022.01.065. Epub 2022 Feb 13. PMID: 35279286. |
Most results censored for Down Syndrome group |
|
Vinycomb T, Browning A, Jones MLM, Hutson JM, King SK, Teague WJ. Quality of life outcomes in children born with duodenal atresia. J Pediatr Surg. 2020 Oct;55(10):2111-2114. doi: 10.1016/j.jpedsurg.2019.11.017. Epub 2019 Dec 28. PMID: 31955988. |
Wrong outcomes |
|
Friedmacher F, Puri P. Hirschsprung's disease associated with Down syndrome: a meta-analysis of incidence, functional outcomes and mortality. Pediatr Surg Int. 2013 Sep;29(9):937-46. doi: 10.1007/s00383-013-3361-1. PMID: 23943251. |
Results from individual studies were sometimes incorrectly reported in this review. Therefore, the individual studies fitting the PICO were included. |
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 17-07-2025
Beoordeeld op geldigheid : 17-04-2025
Voor meer details over de gebruikte richtlijnmethodologie verwijzen wij u naar de Werkwijze. Relevante informatie voor de ontwikkeling/herziening van deze richtlijnmodule is hieronder weergegeven.
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS).
De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2021 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor kinderen met downsyndroom.
Werkgroep
- Dr. H.B.M. (Helma) van Gameren-Oosterom, kinderarts, werkzaam in het Groene Hart Ziekenhuis te Gouda, NVK, voorzitter vanaf 11-12-2023
- R. (Regina) Lamberts, directeur, werkzaam bij Stichting Downsyndroom te Meppel
- H. (Hester) van Wieringen, kinderarts erfelijke en aangeboren aandoeningen, werkzaam in het St. Antonius Ziekenhuis te Utrecht, NVK
- A.M. (Anne-Marie) van Wermeskerken, kinderarts, werkzaam in het Flevoziekenhuis te Almere, NVK
- Dr. E.A. (Eveline) Schell-Feith, kinderarts, werkzaam in het Alrijne Ziekenhuis te Leiderdorp, NVK
- D.A.C.M. (Yvonne) Snepvangers, kinderarts, werkzaam bij Rivas Zorggroep (Beatrixziekenhuis) te Gorinchem, NVK
- Dr. P. (Pit) Vermeltfoort, oogarts, werkzaam in het Elkerliek ziekenhuis te Helmond, NOG
- K.M. (Kirsten) Vogelaar-Burghout, dermatoloog, werkzaam in het Zaans Medisch Centrum te Zaandam, NVDV
- K.C. (Käthe Christel) Noz, dermatoloog, werkzaam in het Adrz te Goes, NVDV
- Dr. C.D.L. (Christine) van Gogh, KNO-arts, werkzaam in Amsterdam UMC te Amsterdam, NVKNO
- Dr. M.E. (Michel) Weijerman, kinderarts, werkzaam in het Alrijne Ziekenhuis te Leiderdorp, NVK (voorzitter tot 11-12-2023)
Klankbordgroep
- L.C. (Lianne) Krab, arts Verstandelijk Gehandicapten, werkzaam bij Hartekamp Groep te Heemstede, NVAVG
- T.F.H. (Tom) Scheers, kinder- en jeugdpsychiater, werkzaam bij GGZ Drenthe te Assen, NVvP
- M.C. (Marianne) Kasius, kinder- en jeugdpsychiater, werkzaam bij Youz (Parnassia Groep), NVvP
- Dr. C. (Christine) de Weger, orthoptist, werkzaam in het RadboudUMC te Nijmegen, NVvO
- Prof. Dr. E. (Esther) de Vries, coördinator Data Science, werkzaam in het Jeroen Bosch Ziekenhuis te Den Bosch, NVK
- F. (Frank) Visscher, kinderneuroloog, werkzaam in Het Van Weel-Bethesda Ziekenhuis te Dirksland, NVN
- J.M. (Rien) Nijman, kinderuroloog, NVU
- E.H. (Erica) Gerkes, kindergeneticus, werkzaam in het UMCG te Groningen, VKGN
- Dr. M. (Mirjam) van Eck, kinderfysiotherapeut, werkzaam in het Amsterdam UMC te Amsterdam, NVFK/KNGF
- S.M. (Sonja) Kalf, tandarts gehandicaptenzorg, werkzaam bij Stichting Bijzondere Tandheelkunde te Amsterdam, KNMT
- H. (Heleen) Eijlders, arts maatschappij en gezondheid, werkzaam bij Ons Tweede Thuis te Amstelveen, AJN
- M. (Marjolein) Coppens, directeur/eigenaar, werkzaam bij ProNect te Ophemert, NVLF
- T.M.C. (Trea) Harperink-Oude Nijhuis, diëtist verstandelijke gehandicaptenzorg, werkzaam bij de Twentse Zorgcentra te Enschede, NVD/DVG
Met ondersteuning van
- Dr. T. (Tim) Christen, adviseur, Kennisinstituut van de Federatie Medisch Specialisten
- Dr. R. (Renee) Bolijn, adviseur, Kennisinstituut van de Federatie Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van (kern)werkgroepleden en klankbordgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Betrokkenen |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Werkgroep |
||||
|
Gameren-Oosterom, van* |
Kinderarts, Groene Hart Ziekenhuis te Gouda. Betaald. |
Geen |
Geen |
Geen |
|
Gogh, van |
KNO-arts Amsterdam UMC |
Geen |
Geen |
Geen |
|
Lamberts |
directeur Stichting Downsyndroom |
Geen |
Geen |
Geen |
|
Noz |
Dermatoloog, 0,8 fte AMS Binnen deze functie mag ik 8 uur per week werkzaamheden verrichten als externe promovendus bij Tranzo (Tilburg University) met als onderwerp "huidafwijkingen bij Downsyndroom) |
Geen |
Ik heb een volwassen dochter met Downsyndroom. Van 2004-2012 zat ik in het bestuur van de Stichting Downsyndroom (SDS) en ik geef sinds jaren op verzoek onbezoldigd advies op vragen van de SDS, kinderartsen en artsen-VG. Voorheen was ik lid van de Domeingroep Kinderdermatologie van de NVDV. Met betrekking deze tot deze richtlijn zal ik een lid en de voorzitter van de Domeingroep ook op de hoogte houden. Door mee te werken aan deze richtlijn verwacht ik geen wezenlijke verandering van mijn reputatie op dit gebied. |
Geen |
|
Schell-Feith |
kinderarts Alrijne ziekenhuis |
Geen |
Geen |
Geen |
|
Snepvangers |
Kinderarts bij Rivas Zorggroep (Beatrixziekenhuis), volledige functie van kinderarts, betaald |
Geen |
Geen |
Geen |
|
Vermeltfoort |
Oogarts in Elkerliek ziekenhuis te Helmond |
Geen |
Takeda TAK-935-3001 en 3002 : Skyline and Skyway (LGS) study |
|
|
Vogelaar-Burghout |
Dermatoloog Zaans medisch centrum (0.75 FTE Dermatoloog VogelBloem (0.2 FTE) |
Lid domeingroep kinderdermatologie |
Meer expertise op het gebied van kinderen met Downsyndroom na medewerking aan deze richtlijn verwacht ik. Maar dat zal de zorg alleen maar ten goede komen. |
|
|
Weijerman |
Directeur, Stichting Artsen voor Kinderen |
Geen |
Geen |
Geen |
|
Wermeskerken, van |
Kinderarts, Flevo Ziekenhuis, Almere |
Geen
|
Ik ben als kinderarts betrokken bij de down poli in Almere |
Geen |
|
Wieringen, van |
kinderarts erfelijke en aangeboren aandoeningen, St. Antonius Ziekenhuis |
Geen |
Geen |
Geen |
|
Klankbordgroep |
||||
|
Coppens |
Directeur/eigenaar ProNect, werkend in opdrachten als wetenschappelijk onderzoeker, docent postacademische opleidingen, hoofdredacteur landelijk vakblad |
Geen |
Geen |
Geen |
|
Eck, van |
Kinderfysiotherapeut in het Amsterdam UMC |
Lid van Commissie Onderzoek en Ontwikkeling van de NVFK: (vacatievergoeding) Docent bij cursus loopproblemen bij kinderen van het NPI: betaald Gastdocent op Hogeschool Utrecht Master Kinderfysiotherapie: betaald Deskundige bij cyberpoli downsyndroom: onbetaald |
Geen |
Geen |
|
Eijlders |
Arts maatschappij en gezondheid. teamarts KDC;s bij Ons tweede Thuis betaald |
voorzitter cie. Zorg voor Zeldzaam AJN: onbetaald |
geen Ons Tweede Thuis is een instelling voor verstandelijk gehandicapten waaronder cliënten met Downsyndroom. Maar de financiering van het bedrijf en mij persoonlijk is onafhankelijk van de richtlijn. Vanuit de cie. Zorg voor Zeldzaam van de AJN ben ik afgevaardigd vanwege mijn expertise binnen de doelgroep kinderen met verstandelijke beperking, waaronder Down. De andere kant is dat de deelname aan de klankbordgroep dit beeld kan bevestigen. |
Geen |
|
Gerkes |
Klinisch geneticus in loondienst academisch ziekenhuis UMCG |
Geen |
Geen |
Geen |
|
Harperink-Oude Nijhuis |
Diëtist VG (in loondienst; 24 uur) De Twentse Zorgcentra Enschede |
Geen |
WUR Nut van voedingssupplementen bij kinderen met Down (2020-2021) Lid DVG (Diëtisten in de zorg voor mensen met een verstandelijke beperking) Lid NVD (Nederlandse vereniging van Diëtisten) |
Geen |
|
Kalf |
tandarts-gehandicaptenzorg bij Stichting Bijzondere Tandheelkunde, Amsterdam, loondienstverband 0,4. |
voorzitter Federatie Tandheelkundige Weenschappelijke Verenigingen FTWV onbetaald. |
Geen |
Geen |
|
Kasius |
PG YOUZ: Profielopleider K&J Psychiatrie, stageopleider Arts Verstandelijk Gehandicapten |
Geen |
Commissielid Kajak ( Academische werkplaat LVB) Onderzoek en Onderwijs |
Geen |
|
Krab |
Arts VG, VG Poli Hartekamp Groep te Heemstede/Velserbroek, loondienst. 0,2 FTE specifiek aan zorg voor mensen met genetische syndromen, binnen de Syndroompoli Hartekampgroep (o.a. voor cliënten met DS) en als lid en arts VG van de transitiepoli van het ENCORE-GRI expertise centrum Erasmus MC – Sophia Kinderziekenhuis – Hartekamp Groep. |
Lid Stuurgroep Richtlijn Ontwikkeling (SRO) van NVAVG t/m mei 2024. Onbetaald. |
Geen |
Geen |
|
Nijman |
Kinderuroloog n.p. |
|
|
|
|
Scheers |
Namens de Nederlandse Vereniging voor Psychiatrie. Werkgever GGZ Drenthe te Assen |
consulent voor CCE, betaald |
Geen, behalve vergroten eigen kennis t.b.v. mijn werk. |
Geen |
|
Visscher |
Federatie Medisch Specialisten |
Neuroloog en kinderneuroloog in ziekenhuis Van Weel Bethesda, Dirklandarts GGZ Eleos |
Geen |
Geen |
|
Vries, de |
Coördinator Data Science (voormalig kinderarts) bij Jeroen Bosch Academie Wetenschap van het Jeroen Bosch Ziekenhuis & Bijzonder Hoogleraar bij Tranzo, TSB, Tilburg University. |
Lid Raad van Toezicht bij Het Laar (ouderenorganisatie in Tilburg) |
unPAD studie (financier: Takeda: primary unclassified antibody deficiency (heeft niet te maken met Downsyndroom) |
Geen |
|
Weger, de |
orthoptist en klinisch epidemioloog / onderzoeker Dondersinstituut /Radbouduniversiteit Nijmegen |
werkzaam bij Bartimeus |
Ik ben gepromoveerd op onderzoek naar de effecten van een bifocale bril bij kinderen met Downsyndroom |
Nee |
* Voorzitter
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door een afgevaardigde van Stichting Downsyndroom in de werkgroep. De conceptrichtlijn wordt tevens voor commentaar voorgelegd aan deze stichting en de eventuele aangeleverde commentaren worden bekeken en verwerkt.
Wkkgz & Kwalitatieve raming van mogelijke substantiële financiële gevolgen
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijn is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling zijn richtlijnmodules op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Uit de kwalitatieve raming blijkt dat er waarschijnlijk geen substantiële financiële gevolgen zijn, zie onderstaande tabel.
|
Module |
Uitkomst raming |
Toelichting |
|
|
Geen financiële gevolgen |
Module beschrijft zorg die voor het overgrote deel reeds aan deze aanbeveling voldoet. |
Zoekverantwoording
Literature search strategy
Embase.com
|
No. |
Query |
Results |
|
#1 |
'down syndrome'/exp OR 'trisomy 21'/exp OR ((down* NEAR/2 syndrome*):ti,ab,kw) OR downsyndrome*:ti,ab,kw OR (((trisomy OR chromosome) NEAR/1 21):ti,ab,kw) OR mongolism*:ti,ab,kw OR ((translocat* NEAR/2 21):ti,ab,kw) |
57322 |
|
#2 |
'gastrointestinal surgery'/exp OR 'abdominal surgery'/de OR ((('alimentary canal*' OR 'alimentary tract*' OR antireflux OR anus OR anal OR anorect* OR cecal OR caecal OR cecum OR caecum OR colon* OR colorect* OR digestive OR duoden* OR esophag* OR gastro* OR ileoanal OR ileorect* OR ileocec* OR ileosec* OR ileum OR ileal OR intestin* OR mesorect* OR oesophag* OR 'pull through' OR pullthrough OR pylorus* OR rectum OR rectal OR rectosigmoid OR 'small bowel' OR stomach OR tracheal OR tracheo*) NEAR/4 (surg* OR operat* OR procedure* OR resect* OR repair* OR anastomos*)):ti,ab,kw) OR (('hirschsprung disease'/exp OR hirschsprung*:ti,ab,kw OR megacolon*:ti,ab,kw OR aganglion*:ti,ab,kw) AND ('postoperative period'/de OR 'postoperative care'/de OR 'postoperative complication'/de OR surg*:ti,ab,kw OR postsurg*:ti,ab,kw OR operat*:ti,ab,kw OR postoperat*:ti,ab,kw)) OR ('digestive system disease'/exp AND 'postoperative complication'/exp) OR ampullectom*:ti,ab,kw OR anastomos*:ti,ab,kw OR anoplast*:ti,ab,kw OR appendectom*:ti,ab,kw OR appendicectom*:ti,ab,kw OR cecectom*:ti,ab,kw OR caecectom*:ti,ab,kw OR coecectom*:ti,ab,kw OR colectom*:ti,ab,kw OR cecostom*:ti,ab,kw OR colostom*:ti,ab,kw OR duodenectom*:ti,ab,kw OR enterostom*:ti,ab,kw OR esophagectom*:ti,ab,kw OR esophagoplast*:ti,ab,kw OR esophagostom*:ti,ab,kw OR fundoplicat*:ti,ab,kw OR gastrectom*:ti,ab,kw OR gastroduodenostom*:ti,ab,kw OR gastroenterostom*:ti,ab,kw OR gastrojejunostom*:ti,ab,kw OR gastropex*:ti,ab,kw OR gastroplast*:ti,ab,kw OR gastrotom*:ti,ab,kw OR gastrostom*:ti,ab,kw OR hemicolectom*:ti,ab,kw OR hemorrhoidectom*:ti,ab,kw OR ileectom*:ti,ab,kw OR ileocecectom*:ti,ab,kw OR ileocaecectom*:ti,ab,kw OR ileocolectom*:ti,ab,kw OR ileostom*:ti,ab,kw OR jejunoileostom*:ti,ab,kw OR jejunostom*:ti,ab,kw OR polypectom*:ti,ab,kw OR portoenterostom*:ti,ab,kw OR proctectom*:ti,ab,kw OR proctocolectom*:ti,ab,kw OR proctopexy:ti,ab,kw OR sigmoidectom*:ti,ab,kw |
899113 |
|
#3 |
#1 AND #2 NOT ('conference abstract'/it OR 'editorial'/it OR 'letter'/it OR 'note'/it) NOT (('animal'/exp OR 'animal experiment'/exp OR 'animal model'/exp OR 'nonhuman'/exp) NOT 'human'/exp) AND [1990-2024]/py |
771 |
|
#4 |
'meta analysis'/exp OR 'meta analysis (topic)'/exp OR metaanaly*:ti,ab OR 'meta analy*':ti,ab OR metanaly*:ti,ab OR 'systematic review'/de OR 'cochrane database of systematic reviews'/jt OR prisma:ti,ab OR prospero:ti,ab OR (((systemati* OR scoping OR umbrella OR 'structured literature') NEAR/3 (review* OR overview*)):ti,ab) OR ((systemic* NEAR/1 review*):ti,ab) OR (((systemati* OR literature OR database* OR 'data base*') NEAR/10 search*):ti,ab) OR (((structured OR comprehensive* OR systemic*) NEAR/3 search*):ti,ab) OR (((literature NEAR/3 review*):ti,ab) AND (search*:ti,ab OR database*:ti,ab OR 'data base*':ti,ab)) OR (('data extraction':ti,ab OR 'data source*':ti,ab) AND 'study selection':ti,ab) OR ('search strategy':ti,ab AND 'selection criteria':ti,ab) OR ('data source*':ti,ab AND 'data synthesis':ti,ab) OR medline:ab OR pubmed:ab OR embase:ab OR cochrane:ab OR (((critical OR rapid) NEAR/2 (review* OR overview* OR synthes*)):ti) OR ((((critical* OR rapid*) NEAR/3 (review* OR overview* OR synthes*)):ab) AND (search*:ab OR database*:ab OR 'data base*':ab)) OR metasynthes*:ti,ab OR 'meta synthes*':ti,ab |
1025597 |
|
#5 |
'clinical trial'/exp OR 'randomization'/exp OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'crossover procedure'/exp OR 'placebo'/exp OR 'prospective study'/exp OR rct:ab,ti OR random*:ab,ti OR 'single blind':ab,ti OR 'randomised controlled trial':ab,ti OR 'randomized controlled trial'/exp OR placebo*:ab,ti |
4024922 |
|
#6 |
'major clinical study'/de OR 'clinical study'/de OR 'case control study'/de OR 'family study'/de OR 'longitudinal study'/de OR 'retrospective study'/de OR 'prospective study'/de OR 'comparative study'/de OR 'cohort analysis'/de OR ((cohort NEAR/1 (study OR studies)):ab,ti) OR (('case control' NEAR/1 (study OR studies)):ab,ti) OR (('follow up' NEAR/1 (study OR studies)):ab,ti) OR (observational NEAR/1 (study OR studies)) OR ((epidemiologic NEAR/1 (study OR studies)):ab,ti) OR (('cross sectional' NEAR/1 (study OR studies)):ab,ti) |
8206230 |
|
#7 |
'case control study'/de OR 'comparative study'/exp OR 'control group'/de OR 'controlled study'/de OR 'controlled clinical trial'/de OR 'crossover procedure'/de OR 'double blind procedure'/de OR 'phase 2 clinical trial'/de OR 'phase 3 clinical trial'/de OR 'phase 4 clinical trial'/de OR 'pretest posttest design'/de OR 'pretest posttest control group design'/de OR 'quasi experimental study'/de OR 'single blind procedure'/de OR 'triple blind procedure'/de OR (((control OR controlled) NEAR/6 trial):ti,ab,kw) OR (((control OR controlled) NEAR/6 (study OR studies)):ti,ab,kw) OR (((control OR controlled) NEAR/1 active):ti,ab,kw) OR 'open label*':ti,ab,kw OR (((double OR two OR three OR multi OR trial) NEAR/1 (arm OR arms)):ti,ab,kw) OR ((allocat* NEAR/10 (arm OR arms)):ti,ab,kw) OR placebo*:ti,ab,kw OR 'sham-control*':ti,ab,kw OR (((single OR double OR triple OR assessor) NEAR/1 (blind* OR masked)):ti,ab,kw) OR nonrandom*:ti,ab,kw OR 'non-random*':ti,ab,kw OR 'quasi-experiment*':ti,ab,kw OR crossover:ti,ab,kw OR 'cross over':ti,ab,kw OR 'parallel group*':ti,ab,kw OR 'factorial trial':ti,ab,kw OR ((phase NEAR/5 (study OR trial)):ti,ab,kw) OR ((case* NEAR/6 (matched OR control*)):ti,ab,kw) OR ((match* NEAR/6 (pair OR pairs OR cohort* OR control* OR group* OR healthy OR age OR sex OR gender OR patient* OR subject* OR participant*)):ti,ab,kw) OR ((propensity NEAR/6 (scor* OR match*)):ti,ab,kw) OR versus:ti OR vs:ti OR compar*:ti OR ((compar* NEAR/1 study):ti,ab,kw) OR (('major clinical study'/de OR 'clinical study'/de OR 'cohort analysis'/de OR 'observational study'/de OR 'cross-sectional study'/de OR 'multicenter study'/de OR 'correlational study'/de OR 'follow up'/de OR cohort*:ti,ab,kw OR 'follow up':ti,ab,kw OR followup:ti,ab,kw OR longitudinal*:ti,ab,kw OR prospective*:ti,ab,kw OR retrospective*:ti,ab,kw OR observational*:ti,ab,kw OR 'cross sectional*':ti,ab,kw OR cross?ectional*:ti,ab,kw OR multicent*:ti,ab,kw OR 'multi-cent*':ti,ab,kw OR consecutive*:ti,ab,kw) AND (group:ti,ab,kw OR groups:ti,ab,kw OR subgroup*:ti,ab,kw OR versus:ti,ab,kw OR vs:ti,ab,kw OR compar*:ti,ab,kw OR 'odds ratio*':ab OR 'relative odds':ab OR 'risk ratio*':ab OR 'relative risk*':ab OR 'rate ratio':ab OR aor:ab OR arr:ab OR rrr:ab OR ((('or' OR 'rr') NEAR/6 ci):ab))) |
15049948 |
|
#8 |
#3 AND #4 - SR |
24 |
|
#9 |
#3 AND #5 NOT #8 - RCT |
44 |
|
#10 |
#3 AND (#6 OR #7) NOT (#8 OR #9) - observationeel |
338 |
|
#11 |
#8 OR #9 OR #10 |
406 |
Ovid/Medline
|
# |
Searches |
Results |
|
1 |
exp Down Syndrome/ or (down* adj2 syndrome*).ti,ab,kf. or downsyndrome*.ti,ab,kf. or ((trisomy or chromosome) adj1 "21").ti,ab,kf. or mongolism*.ti,ab,kf. or (translocat* adj2 "21").ti,ab,kf. |
38767 |
|
2 |
exp Digestive System Surgical Procedures/ or (('alimentary canal*' or 'alimentary tract*' or antireflux or anus or anal or anorect* or cecal or caecal or cecum or caecum or colon* or colorect* or digestive or duoden* or esophag* or gastro* or ileoanal or ileorect* or ileocec* or ileosec* or ileum or ileal or intestin* or mesorect* or oesophag* or 'pull through' or pullthrough or pylorus* or rectum or rectal or rectosigmoid or 'small bowel' or stomach or tracheal or tracheo*) adj4 (surg* or operat* or procedure* or resect* or repair* or anastomos*)).ti,ab,kf. or ((Hirschsprung Disease/ or Hirschsprung*.ti,ab,kf. or megacolon*.ti,ab,kf. or aganglion*.ti,ab,kf.) and (Postoperative Period/ or exp Postoperative Care/ or Postoperative Complications/ or surg*.ti,ab,kf. or postsurg*.ti,ab,kf. or operat*.ti,ab,kf. or postoperat*.ti,ab,kf.)) or (exp Digestive System Diseases/ and exp Postoperative Complications/) or (ampullectom* or anastomos* or anoplast* or appendectom* or appendicectom* or cecectom* or caecectom* or coecectom* or colectom* or cecostom* or colostom* or duodenectom* or enterostom* or esophagectom* or esophagoplast* or esophagostom* or fundoplicat* or gastrectom* or gastroduodenostom* or gastroenterostom* or gastrojejunostom* or gastropex* or gastroplast* or gastrostom* or gastrotom* or gastrostom* or hemicolectom* or hemorrhoidectom* or ileectom* or ileocecectom* or ileocaecectom* or ileocolectom* or ileostom* or jejunoileostom* or jejunostom* or polypectom* or polypectom* or portoenterostom* or proctectom* or proctocolectom* or proctopexy or sigmoidectom*).ti,ab,kf. |
664748 |
|
3 |
(1 and 2) not (comment/ or editorial/ or letter/) not ((exp animals/ or exp models, animal/) not humans/) |
399 |
|
4 |
limit 3 to yr="1990 -Current" |
348 |
|
5 |
meta-analysis/ or meta-analysis as topic/ or (metaanaly* or meta-analy* or metanaly*).ti,ab,kf. or systematic review/ or cochrane.jw. or (prisma or prospero).ti,ab,kf. or ((systemati* or scoping or umbrella or "structured literature") adj3 (review* or overview*)).ti,ab,kf. or (systemic* adj1 review*).ti,ab,kf. or ((systemati* or literature or database* or data-base*) adj10 search*).ti,ab,kf. or ((structured or comprehensive* or systemic*) adj3 search*).ti,ab,kf. or ((literature adj3 review*) and (search* or database* or data-base*)).ti,ab,kf. or (("data extraction" or "data source*") and "study selection").ti,ab,kf. or ("search strategy" and "selection criteria").ti,ab,kf. or ("data source*" and "data synthesis").ti,ab,kf. or (medline or pubmed or embase or cochrane).ab. or ((critical or rapid) adj2 (review* or overview* or synthes*)).ti. or (((critical* or rapid*) adj3 (review* or overview* or synthes*)) and (search* or database* or data-base*)).ab. or (metasynthes* or meta-synthes*).ti,ab,kf. |
744647 |
|
6 |
exp clinical trial/ or randomized controlled trial/ or exp clinical trials as topic/ or randomized controlled trials as topic/ or Random Allocation/ or Double-Blind Method/ or Single-Blind Method/ or (clinical trial, phase i or clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or multicenter study or clinical trial).pt. or random*.ti,ab. or (clinic* adj trial*).tw. or ((singl* or doubl* or treb* or tripl*) adj (blind$3 or mask$3)).tw. or Placebos/ or placebo*.tw. |
2723144 |
|
7 |
Epidemiologic studies/ or case control studies/ or exp cohort studies/ or Controlled Before-After Studies/ or Case control.tw. or cohort.tw. or Cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or Longitudinal.tw. or Retrospective*.tw. or prospective*.tw. or consecutive*.tw. or Cross sectional.tw. or Cross-sectional studies/ or historically controlled study/ or interrupted time series analysis/ [Onder exp cohort studies vallen ook longitudinale, prospectieve en retrospectieve studies] |
4720363 |
|
8 |
Case-control Studies/ or clinical trial, phase ii/ or clinical trial, phase iii/ or clinical trial, phase iv/ or comparative study/ or control groups/ or controlled before-after studies/ or controlled clinical trial/ or double-blind method/ or historically controlled study/ or matched-pair analysis/ or single-blind method/ or (((control or controlled) adj6 (study or studies or trial)) or (compar* adj (study or studies)) or ((control or controlled) adj1 active) or "open label*" or ((double or two or three or multi or trial) adj (arm or arms)) or (allocat* adj10 (arm or arms)) or placebo* or "sham-control*" or ((single or double or triple or assessor) adj1 (blind* or masked)) or nonrandom* or "non-random*" or "quasi-experiment*" or "parallel group*" or "factorial trial" or "pretest posttest" or (phase adj5 (study or trial)) or (case* adj6 (matched or control*)) or (match* adj6 (pair or pairs or cohort* or control* or group* or healthy or age or sex or gender or patient* or subject* or participant*)) or (propensity adj6 (scor* or match*))).ti,ab,kf. or (confounding adj6 adjust*).ti,ab. or (versus or vs or compar*).ti. or ((exp cohort studies/ or epidemiologic studies/ or multicenter study/ or observational study/ or seroepidemiologic studies/ or (cohort* or 'follow up' or followup or longitudinal* or prospective* or retrospective* or observational* or multicent* or 'multi-cent*' or consecutive*).ti,ab,kf.) and ((group or groups or subgroup* or versus or vs or compar*).ti,ab,kf. or ('odds ratio*' or 'relative odds' or 'risk ratio*' or 'relative risk*' or aor or arr or rrr).ab. or (("OR" or "RR") adj6 CI).ab.)) |
5684953 |
|
9 |
4 and 5 - SR |
6 |
|
10 |
(4 and 6) not 9 - RCT |
14 |
|
11 |
(4 and (7 or 8)) not (9 or 10) - observationeel |
181 |
|
12 |
9 or 10 or 11 |
201 |