Katheterablatie
Uitgangsvraag
Wanneer wordt katheterablatie voor ritme-regulatie bij patiënten met atriumfibrilleren gekozen?
Deze uitgangsvraag bevat de volgende deelvragen:
- Welke aanvullende ablatiestrategie wordt gekozen wanneer de pulmonaal venen al geïsoleerd zijn na een eerdere ablatie en dit onvoldoende effect heeft op het atriumfibrilleren?
- Wanneer dient katheterablatie te worden overwogen na het falen van medicamenteuze ritme-regulatie therapie?
Aanbeveling
Betere uitkomsten na ablatie:
Behandel modificeerbare risicofactoren (overgewicht, hypertensie en OSA) en adviseer het vermijden van uitlokkende factoren, voor en na katheterablatie om uitkomsten van ablatie te verbeteren (Zie ook Supplementary Box 2).
Ablatie indien geneesmiddelen niet voldoende effectief zijn of bijwerkingen geven:
- Indien ritme-regulatie met een antiaritmicum (klasse I of III) onvoldoende effect op de klachten van atriumfibrilleren heeft, bespreek met patiënt om een katheterablatie te verrichten zowel bij paroxysmaal als persistent atriumfibrilleren.
- Overweeg dit ook als alleen een bètablokker niet effectief is.
Ablatie als eerste behandeling:
- Overweeg als eerste behandeling een katheterablatie bij paroxysmaal of persistent atriumfibrilleren, als alternatief voor antiaritmica.
- Overweeg bij LV-dysfunctie als gevolg van tachycardie-geïnduceerd hartfalen een katheterablatie, ongeacht symptomen.
- Overweeg katheterablatie bij patiënten met hartfalen bij verminderde EF om hospitalisatie en mortaliteit te verminderen.
- Overweeg katheterablatie bij patiënten met atriumfibrilleren en bradycardieën, om pacemakerimplantatie te voorkomen.
Ablatietechnieken:
- Isoleer de pulmonaal venen bij alle ablatieprocedures.
- Overweeg ook ablatie van de cavotricuspidale isthmus indien de patiënt ook typische atriumflutters heeft laten zien.
- Overweeg additionele ablatiestrategieën naast isolatie van de pulmonaal venen, hoewel de effectiviteit hiervan niet vaststaat.
Overweeg opnieuw een katheterablatie na recidiverend atriumfibrilleren.
Overwegingen
AF catheter ablation is a well-established treatment for the prevention of AF recurrences (Calkins, 2018; Arbelo, 2012; Arbelo, 2014; Arbelo, 2017). When performed by appropriately trained operators, AF catheter ablation is a safe and superior alternative to AADs for maintenance of sinus rhythm and symptom improvement (Nyong, 2016; Jais, 2008; Oral, 2006; Mont, 2014; Forleo, 2009; Wilber, 2010; Wazni, 2005; Morillo, 2014; Cosedis Nielsen, 2012; Blomstrom-Lundqvist, 2019; Mark, 2019; Krittayaphong, 2003; Stabile, 2006; Pappone, 2006; Calkins, 2009; Packer, 2013; Ganesan, 2013; Di Biase, 2016; Kuck, 2016; Sohara, 2016; Hakalahti, 2015; Nielsen, 2017; Chen, 2018; Packer, 2019; Noseworthy, 2019). It is advised to discuss the efficacy and complication rates of AF catheter ablation and AADs with the patient once rhythm control as long-term management has been selected.
Indications
In the following section, indications for AF catheter ablation are presented for paroxysmal and persistent AF in patients with and without risk factors for post-ablation AF recurrence. Differentiation of persistent and long-standing persistent AF was omitted because the latter only expresses the duration of persistent AF above an arbitrary and artificial cut-off at 12 months’ duration. The significance of such a cut-off as a single measure has never been substantially proven.
A number of risk factors for AF recurrence after AF ablation have been identified, including LA size, AF duration, patient age, renal dysfunction, and substrate visualization by means of MRI (Teh, 2012; D’Ascenzo, 2013; Berruezo, 2007; Nedios, 2015; Njoku, 2018; Costa, 2015; Marrouche, 2014). Recent systematic reviews on prediction models for AF recurrence after catheter ablation showed the potential benefits of risk predictions, but a more robust evaluation of such models is desirable (Deng, 2017; Kosich, 2019). The model variables can be measured before ablation; therefore, models could be used pre-procedurally to predict the likelihood of recurrence (Kornej, 2015; Kornej, 2017; Kornej, 2018; Kosiuuk, 2015; Mujovic, 2017; Mesquita, 2018; Winkle, 2016; Canpolat, 2013; Wojcik, 2013). However, no single score has been presently identified as consistently superior to others. Thus, at present, for an improved and more balanced indication for ablation in patients with persistent AF and risk factors for recurrence, the most intensely evaluated risk predictors (including duration of AF) should be considered and adjusted to the individual patient’s situation including their preferences. Notably, patients must also be explicitly informed about the importance of treating modifiable risk factors to reduce risk of recurrent AF (Berruezo, 2007; Pathak, 2014; Trines, 2019; Wong, 2015; Wokhlu, 2010; Arya, 2010; Santoro, 2015; Letsas, 2009; Jongnarangsin, 2008; Patel, 2010; Matiello, 2010; Chilukuri, 2010; Ng, 2011; Naruse, 2013; Li, 2014; Kawakami, 2016; Congrete, 2018; Deng, 2018).
The indications for AF catheter ablation are summarized in Figure 1. AF catheter ablation is effective in maintaining sinus rhythm in patients with paroxysmal and persistent AF Nyong, 2016; Jais, 2008; Oral, 2006; Mont, 2014; Forleo, 2009; Wilber, 2010; Wazni, 2005; Morillo, 2014; Cosedis Nielsen, 2012; Krittayaphong, 2003; Stabile, 2006; Pappone, 2006; Calkins, 2009; Packer, 2013; Ganesan, 2013; Di Biase, 2016; Kuck, 2016; Sohara, 2016; Hakalahti, 2015; Nielsen, 2017; Chen, 2018). The main clinical benefit of AF catheter ablation is the reduction of arrhythmia-related symptoms (Blomstrom-Lundqvist, 2019; Mark, 2019; Arbelo, 2014; Arbelo, 2017; Pappone, 2006; Packer, 2019; Wokhlu, 2010; Reddy, 2015). This has been confirmed in a recent RCT showing that the improvement in QoL was significantly higher in the ablation versus medical therapy group, as was the associated reduction in AF burden (Blomstrom-Lundqvist, 2019). Symptom improvement has also been confirmed in the recent large CABANA (Catheter ABlation versus ANtiarrhythmic Drug Therapy for Atrial Fibrillation) RCT (Mark, 2019), but the trial showed that the strategy of AF catheter ablation did not significantly reduce the primary composite outcome of death, disabling stroke, serious bleeding, or cardiac arrest compared with medical therapy (Packer, 2019). As no RCT has yet demonstrated a significant reduction in all-cause mortality, stroke, or major bleeding with AF catheter ablation in the ’general’ AF population, the indications for the procedure have not been broadened beyond symptom relief (Packer, 2019), and AF catheter ablation is generally not indicated in asymptomatic patients. Further important evidence regarding the impact of ablation on major cardiovascular events is expected from the EAST trial (Kirchhof, 2013).
Figure 1 Indications for catheter ablation of symptomatic AF
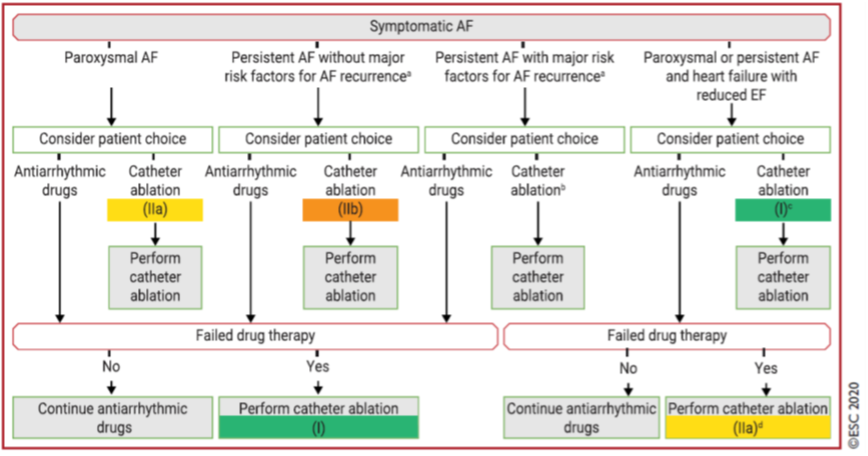
The arrows from AAD to ablation indicate failed drug therapy. AAD = antiarrhythmic drug; AF = atrial fibrillation; EF = ejection fraction; LA = left atrial. aSignificantly enlarged LA volume, advanced age, long AF duration, renal dysfunction, and other cardiovascular risk factors. bIn rare individual circumstances, catheter ablation may be carefully considered as first-line therapy. cRecommended to reverse LV dysfunction when tachycardiomyopathy is highly probably. dTo improve survival and reduce hospitalization. Adapted from Hindricks (2020)
In selected patients with HF and reduced LVEF, two RCTs have shown a reduction in all-cause mortality and hospitalizations with AF catheter ablation (Di Biase, 2016; Marrouche, 2018), although combined mortality and HF hospitalization was a primary endpoint only in the CASTLE-AF (Catheter Ablation versus Standard conventional Treatment in patients with Left ventricular dysfunction and Atrial Fibrillation) trial (Marrouche, 2018). The generalizability of the trial has recently been evaluated in a large HF patient population (Noseworthy, 2020). This analysis showed that only a small number of patients met the trial inclusion criteria (< 10%) and patients who met the CASTLE-AF inclusion criteria had a significant benefit from treatment as demonstrated in the trial (Noseworthy, 2020). The smaller AMICA (Atrial Fibrillation Management in Congestive Heart Failure With Ablation) RCT, which included patients with more advanced HFrEF, did not show benefits gained by AF catheter ablation at 1-year follow-up (Kuck, 2019), whereas a recent CABANA subgroup analysis supported the benefits of AF catheter ablation in patients with HFrEF, showing a significant reduction in the study primary endpoint (death, stroke, bleeding, cardiac arrest) and reduced mortality in the ablation group (Packer, 2019a; Packer, 2019b). Overall, AF catheter ablation in patients with HFrEF results in higher rates of preserved sinus rhythm and greater improvement in LVEF, exercise performance, and QoL compared with AAD and rate control (Di Biase, 2016; Marrouche, 2018; Khan, 2008; MacDonald, 2011; Jones, 2013; Hunter, 2014; Al Halabi, 2015; Prabhu, 2017; Elgendy, 2018; Briceno, 2018; Ma, 2018; Kheiri, 2018; Khan, 2018). Accordingly, ablation should be considered in patients with HFrEF who have been selected for rhythm control treatment to improve QoL and LV function, and to reduce HF hospitalization and, potentially, mortality.
When AF-mediated tachycardia-induced cardiomyopathy (i.e., ventricular dysfunction secondary to rapid and/or asynchronous/irregular myocardial contraction, partially or completely reversed after treatment of the causative arrhythmia) is highly suspected, AF catheter ablation is recommended to restore LV function (Martin, 2017; Raymond-Pagquin, 2018; Brembilla-Perrot, 2016; Dagres, 2011; Prabhu, 2018).
Ablation is recommended, in general, as a second-line therapy after failure (or intolerance) of class I or class III AADs. This recommendation is based on the results of multiple RCTs showing superiority of AF catheter ablation versus AADs regarding freedom from recurrent arrhythmia or improvement in symptoms, exercise capacity, and QoL after medication failure (Jais, 2008; Oral, 2006; Mont, 2014; Forleo, 2009; Wilber, 2010; Blomstrom-Lundqvist, 2019; Mark, 2019; Krittayaphong, 2003; Stabile, 2006; Pappone, 2006; Di Biase, 2016; Sohara, 2016; Hakalahti, 2015; Nielsen, 2017; Chen, 2018; Packer, 2019a). Clinical trials considering AF catheter ablation before any AAD suggest that AF catheter ablation is more effective in maintaining sinus rhythm, with comparable complication rates in experienced centres (Wazni, 2005; Morillo, 2014; Cosedis Nielsen, 2012; Hakalahti, 2015). The 5-year follow-up in the MANTRA-PAF (Medical Antiarrhythmic Treatment or Radiofrequency Ablation in Paroxysmal Atrial Fibrillation) trial showed a significantly lower AF burden in the ablation arm that did not, however, translate into improved QoL compared with AAD treatment (Nielsen, 2017), whereas the CAPTAF (Catheter Ablation compared with Pharmacological Therapy for Atrial Fibrillation) study showed that, in AF patients mostly naive to class I and III AADs, the greater improvement in QoL in the ablation arm was directly associated with greater reduction in AF burden compared with the AAD arm (Blomstrom-Lundqvist, 2019). Based on these studies and patient preferences, AF catheter ablation should be considered before a trial of AAD in patients with paroxysmal AF episodes (class IIa), or may be considered in patients with persistent AF without risk factors for recurrence (class IIb).
Techniques and technologies
The cornerstone of AF catheter ablation is the complete isolation of pulmonary veins by linear lesions around their antrum, either using point-by-point radiofrequency ablation or single-shot ablation devices (Jais, 2008; Mont, 2014; Wilber, 2010; Pappone, 2006; Calkins, 2009; Packer, 2013; Kuck, 2016 Sohara, 2016; Reddy, 2015; Tamborero, 2009; Natale, 2014; McLellan, 2015; Verma, 2015; Luik, 2015; Dukkipati, 2015; Kuck, 2016; Nery, 2016; Bassiouny, 2016; Hindricks, 2018). Unfortunately, persistent pulmonary vein electrical isolation is difficult to achieve (pulmonary vein reconnection rates of > 70% are reported (Kuck, 2016; Nanthakumar, 2004; Verma, 2005; Ouyang, 2005; Cheema, 2007; Pratola, 2008; Rajappan, 2008; Bansch, 2013; Nakamura, 2013; Neuzil, 2013; Jiang, 2014; Kim, 2017), but could be significantly lower with the newer generation of catheters (Bordignon, 2015; Ullah, 2016; Phlips, 2018)).
Particularly in persistent and long-standing persistent AF, more extensive ablation has been advocated. This may include linear lesions in the atria, isolation of the LAA or of the superior vena cava, ablation of complex fractionated electrograms, rotors, non-pulmonary foci, or ganglionated plexi, fibrosis-guided voltage and/or MRI-mapping, or ablation of high dominant frequency sites (Shad, 2003; Nademanee, 2004; Haissaguerre, 2005a; Haissaguerre, 2005b; Jais, 2006; Atienza, 2009; Stavrakis, 2015; Di Biase, 2016; Gianni, 2016; Santangeli, 2016). However, additional benefit versus pulmonary vein isolation (PVI) alone, justifying its use during the first procedure, is yet to be confirmed (Tamborero, 2009; Verma, 2015; Katritsis, 2013; Arbelo, 2014; Da Costa, 2015; Wong, 2015; Vogler, 2015; Faustino, 2015; Scott, 2016; Driessen, 2016; Qin, 2016; Hu, 2016; Wynn, 2016; Zhang, 2016; Fink, 2017; Kim, 2017; Kircher, 2018; Ammar-Busch, 2017; Blandino, 2017; Yang, 2017; Yu, 2017; Wang, 2018). A RCT-based data suggest improved outcome with targeting extrapulmonary (particularly the LAA) foci and selective ablation of low-voltage areas as adjunct to PVI (Di Biase, 2016; Kircher, 2018). In patients with documented cavotricuspid isthmus (CTI)-dependent flutter undergoing AF catheter ablation, right isthmus ablation may be considered (Perez, 2009; Natale, 2000; Wazni, 2003; Shah, 2007). In case of non-CTI-dependent atrial tachycardia, the ablation technique depends on the underlying mechanism and tachycardia focus or circuit (Calkins, 2018; Hakalahti, 2015).
Several RCTs and observational studies have compared point-by-point radiofrequency and cryoballoon ablation, mostly in the first procedure for paroxysmal AF (Kuck, 2016; Luik, 2015; Neumann, 2011; Herrera Siklody, 2011; Herrera Siklody, 2012; Pokushalov, 2013; Schmidt, 2014; Perez-Castellano, 2014; Hunter, 2015; Squara, 2015; Straube, 2016; Schmidt, 2016; Boveda, 2016; Kuck, 2016; Buist, 2018; Gunawardene, 2018; Mortsell, 2019; Akkaya, 2018; Murray, 2018; Chen, 2017; Buiatti, 2017; Cardoso, 2016; Kabunga, 2916). They reported broadly similar arrhythmia-free survival and overall complications with either technique, with slightly shorter procedure duration but longer fluoroscopy time with cryoballoon ablation (Kuck, 2016; Luik, 2015; Neumann, 2011; Herrera Siklody, 2011; Herrera Siklody, 2012; Pokushalov, 2013; Schmidt, 2014; Perez-Castellano, 2014; Hunter, 2015; Squara, 2015; Straube, 2016; Schmidt, 2016; Boveda, 2016; Kuck, 2016; Buist, 2018; Gunawardene, 2018; Mortsell, 2019; Akkaya, 2018; Murray, 2018; Chen, 2017; Buiatti, 2017; Cardoso, 2016; Kabunga, 2016). However, some studies showed reduced hospitalization and lower complication rates with cryoballoon ablation (Kuck, 2016; Bollmann, 2018; Ueberham, 2018). The choice of energy source may depend on centre availability, operator preference/experience, and patient preference. Alternative catheter designs and energy sources have been developed in an attempt to simplify the ablation procedure and improve outcomes (Sohara, 2016; Kabunga, 2016; Hummel, 2014; Boersma, 2016; Nagashima, 2018; Ucer, 2018), but further evidence is required before changing current recommendations.
Complications
Prospective, registry-based data show that approximately 4 to 14% of patients undergoing AF catheter ablation experience complications, 2 to 3% of which are potentially life-threatening (Arbelo, 2012; Arbelo, 2014; Arbelo, 2017; De Greef, 2018; Steinbeck, 2018; Fink, 2019; Szegedi, 2019). In the recent CABANA-trial, mostly including experienced high-volume centres, complications occurred in the lower range of these rates (Packer, 2019). Complications occur mostly within the first 24 h after the procedure, but some may appear 1 to 2 months after ablation (Calkins, 2018; Arbelo, 2012; Arbelo, 2014; Arbelo, 2017) (Table 1 and supplementary table 10). Periprocedural death is rare (< 0.2%) and usually related to cardiac tamponade (Arbelo, 2014; Arbelo, 2017; Cappato, 2010; Lee, 2011; Deshmukh, 2013; Tripathi, 2018; Voskoboinik, 2018).
Table 1 Procedure-related complications in catheter ablation and thoracoscopic ablation of AF
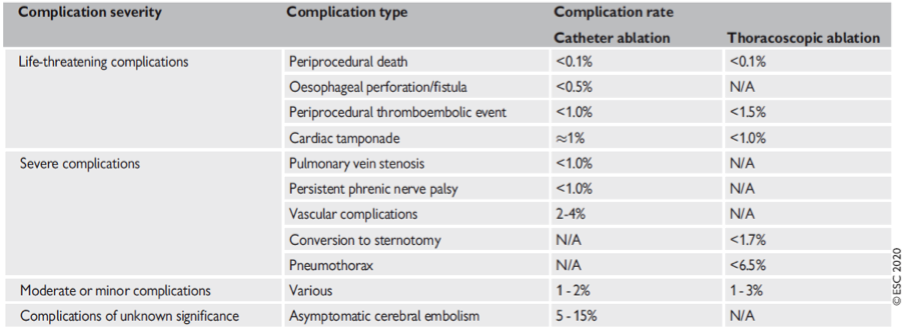
NA = not available
Adapted from Hindricks (2020)
AF catheter ablation outcome and impact of modifiable risk factors
Multiple RCTs have compared AADs with AF catheter ablation using different technologies/ energy sources, either as ‘first-line’ therapy or after AAD failure, showing superiority of AF catheter ablation in arrhythmia-free survival (Nyong, 2016; Jais, 2008; Oral, 2006; Mont, 2014; Forleo, 2009; Wilber, 2010; Wazni, 2005; Morillo, 2014; Cosedis Nielsen, 2012; Krittayaphong, 2003; Stabile, 2006; Pappone, 2006; Calkins, 2009; Packer, 2013; Ganesan, 2013; Di Biase, 2016; Kuck, 2016; Sohara, 2016; Hakalahti, 2015; Nielsen, 2017; Chen, 2018). However, many patients require several procedures and late recurrences are not infrequent (Gaita, 2018; Wokhlu, 2010; Shah, 2008; Sawhney, 2009; Ouyang, 2010; Bertaglia, 2010; Weerasooriya, 2011; Medi, 2011; Schreiber, 2015; Scherr, 2015; Bertaglia, 2017).
Key outcomes include QoL, HF, stroke, and mortality (Shi, 2015; Siontis, 2016; Kim, 2016; Di Biase, 2016; Skelly, 2015; Zheng, 2015). Compared with AADs, AF catheter ablation was associated with significant and sustained improvement in QoL scores in several RCTs and meta-analyses (Calkins, 2018; Jais, 2008; Wilber, 2010; Wazni, 2005; Morillo, 2014; Cosedis Nielsen, 2012; Blomstrom-Lundqvist, 2019; Mark, 2019; Shi, 2015; Siontis, 2016; Kim, 2016; Reynolds, 2010; Walfridsson, 2015). To date, there is no RCT sufficiently large to properly evaluate a reduction in stroke by catheter ablation.
Several factors, including AF type and duration (Jais, 2008; Oral, 2006; Mont, 2014; Wilber, 2010; Pappone, 2006; Packer, 2013; Kuck, 2016; Sohara, 2016; Reddy; 2015; Verma, 2015; Dukkipati, 2015; De Greef, 2018), and the presence of comorbidities such as hypertension (Berruezo, 2007; Wokhlu, 2010; Arya, 2010; Santoro, 2015), obesity (Wong, 2015; Wokhlu, 2010; Jongnarangsin, 2008; Chilukuri, 2010; Shah, 2008; Wong, 2011; Kang, 2012; Mahajan, 2015; Winkle, 2017; De Maat, 2018; Glover, 2019), metabolic syndrome (Chang, 2009; Tang, 2009; Mohanty, 2012), and sleep apnoea (Jongnarangsin, 2008; Patel, 2010; Matiello, 2010; Ng, 2011; Naruse, 2013; Li, 2014; Kawakami, 2016; Congrete, 2018; Deng, 2018) may influence the outcome of catheter ablation (Figure 2 and supplementary box 2). Prospective cohort studies suggest that aggressive control of modifiable risk factors may improve arrhythmia-free survival after catheter ablation (Pathak, 2014).
Figure 2 Risk factors for AF contributing to the development of an abnormal substrate translating into poorer outcomes with rhythm control strategies
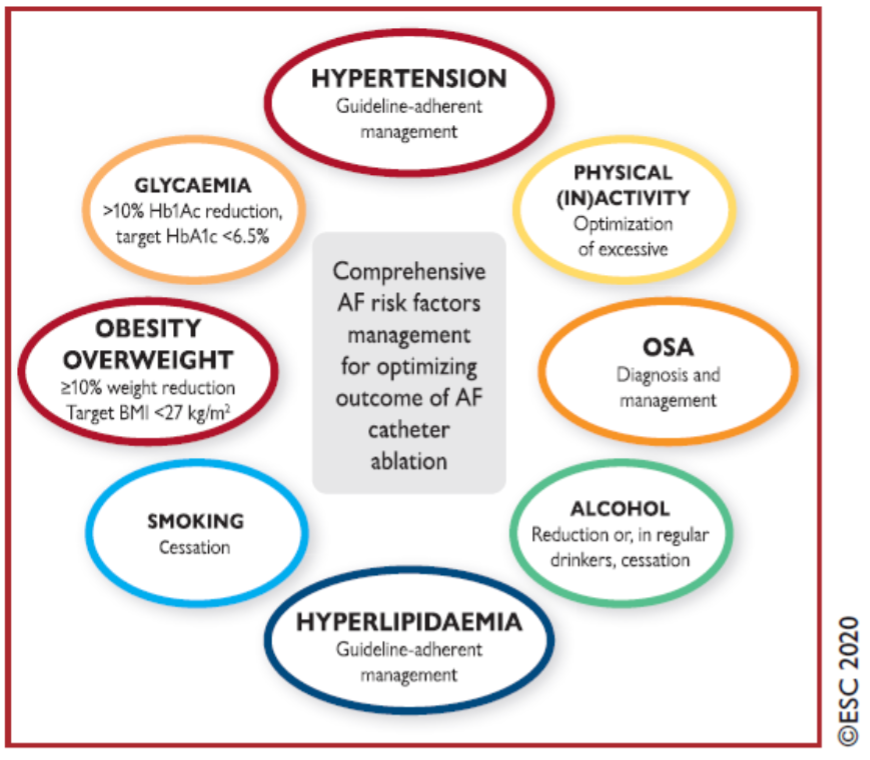
AF = atrial fibrillation; BMI = body mass index; CPAP = continuous positive airway pressure; HbA1C = haemoglobin A1c; OSA = obstructive sleep apnoea. Several AF risk factors may contribute to the development of LA substrates and thus affect the outcome of AF catheter ablation, predisposing to a higher recurrence rate. Aggressive control of modifiable risk factors may reduce recurrence rate.
Adapted from Hindricks (2020)
Follow-up after atrial fibrillation ablation
AF catheter ablation is a complex procedure that may be associated with a range of specific post-procedural complications (module 6.3) (Arbelo, 2014; Arbelo, 2017; Cappato, 2010; Lee, 2011; Deshmukh, 2013; Tripathi, 2018; Voskoboinik, 2018). Although mostly rare, potentially catastrophic complications may initially present with non-specific symptoms and signs to which managing physicians should be attuned. Key issues in follow-up are shown in Table 2.
Table 2 Key issues in follow-up after AF catheter ablation
|
Key issues |
|
Recognition and management
|
|
Follow-up monitoring: Useful to assess procedural success and correlate symptom status with rhythm. Recurrences beyond the first month post-ablation are generally predictive of late recurrences, but recurrent symptoms may be due to ectopic beats or other non-sustained arrhythmia; conversely the presence of asymptomatic AF after ablation is well described. Monitoring may be performed with intermittent ECG, Holter, Patch recordings, external or implanted loop recorder, or smart phone monitor (although the latter has not been validated for such use). Patients should be first reviewed at a minimum of 3 months and annually thereafter. |
|
Management of antiarrhythmic medication and treatment of AF recurrences
Clinical practice regarding routine AAD treatment after ablation varies and there is no convincing evidence that such treatment is routinely needed.
|
|
Management of anticoagulation therapy
|
AAD = antiarrhythmic drug; AF = atrial fibrillation; CHA2DS2-VASc = Congestive heart failure, Hypertension, Age >_75 years, Diabetes mellitus, Stroke, Vascular disease, Age 65 to 74 years, Sex category (female); ECG=electrocardiogram; OAC = oral anticoagulant.
Adapted from Hindricks (2020)
Risk assessment for recurrence of atrial fibrillation post catheter ablation
Recurrence of AF after catheter ablation is driven by the complex interaction of various factors. These include increasing AF duration, age, and LA size (The, 2012; D’Ascenzo, 2013; Berruezo, 2007; Njoku, 2018; Costa, 2015), and structural factors such as the abundance of epicardial fat tissue (Nakahara, 2014; Chao, 2013; Masuda, 2015; Sepehri Shamloo, 2019) and the presence of atrial substrate as evident from electrical or morphological markers (Blanche, 2013). A number of risk-prediction scores have been evaluated (for detailed description see supplementary table 11 and Supplementary Box 2).Whereas these scores only moderately predict AF recurrence, one of the strongest predictors is early recurrent AF, indicating the need for further refinement of these scoring systems (Kornej, 2018).
Onderbouwing
Zoeken en selecteren
To answer the clinical question, the ESC-guideline for the diagnosis and management of atrial fibrillation from 2020 (Hindricks, 2020) was used.
Referenties
- Akkaya E, Berkowitsch A, Zaltsberg S, Greiss H, Hamm CW, Sperzel J, Neumann T, Kuniss M. Ice or fire? Comparison of second-generation cryoballoon ablation and radiofrequency ablation in patients with symptomatic persistent atrial fibrillation and an enlarged left atrium. J Cardiovasc Electrophysiol 2018;29:375-384.
- Al Halabi S, Qintar M, Hussein A, Alraies MC, Jones DG, Wong T, MacDonald MR, Petrie MC, Cantillon D, Tarakji KG, Kanj M, Bhargava M, Varma N, Baranowski B, Wilkoff BL, Wazni O, Callahan T, Saliba W, Chung MK. Catheter ablation for atrial fibrillation in heart failure patients: a meta-analysis of randomized controlled trials. JACC Clin Electrophysiol 2015;1:200-209.
- Ammar-Busch S, Bourier F, Reents T, Semmler V, Telishevska M, Kathan S, Hofmann M, Hessling G, Deisenhofer I. Ablation of complex fractionated electrograms with or without ADditional LINEar Lesions for Persistent Atrial Fibrillation (the ADLINE trial). J Cardiovasc Electrophysiol 2017;28:636-641.
- Arbelo E, Brugada J, Blomstrom-Lundqvist C, Laroche C, Kautzner J, Pokushalov E, Raatikainen P, Efremidis M, Hindricks G, Barrera A, Maggioni A, Tavazzi L, Dagres N, on the behalf of the ESC EHRA Atrial Fibrillation Ablation Long-term Registry Investigators. Contemporary management of patients undergoing atrial fibrillation ablation: in-hospital and 1-year follow-up findings from the ESC-EHRA atrial fibrillation ablation long-term registry. Eur Heart J 2017;38:1303-1316.
- Arbelo E, Brugada J, Hindricks G, Maggioni A, Tavazzi L, Vardas P, Anselme F, Inama G, Jais P, Kalarus Z, Kautzner J, Lewalter T, Mairesse G, Perez-Villacastin J, Riahi S, Taborsky M, Theodorakis G, Trines S; Atrial Fibrillation Ablation Pilot Study Investigators. ESC-EURObservational Research Programme: the Atrial Fibrillation Ablation Pilot Study, conducted by the European Heart Rhythm Association. Europace 2012;14:1094-1103.
- Arbelo E, Brugada J, Hindricks G, Maggioni AP, Tavazzi L, Vardas P, Laroche C, Anselme F, Inama G, Jais P, Kalarus Z, Kautzner J, Lewalter T, Mairesse GH, Perez-Villacastin J, Riahi S, Taborsky M, Theodorakis G, Trines SA; Atrial Fibrillation Ablation Pilot Study Investigators. The atrial fibrillation ablation pilot study: a European Survey on Methodology and results of catheter ablation for atrial fibrillation conducted by the European Heart Rhythm Association. Eur Heart J 2014;35:1466-1478.
- Arbelo E, Guiu E, Ramos P, Bisbal F, Borras R, Andreu D, Tolosana JM, Berruezo A, Brugada J, Mont L. Benefit of left atrial roof linear ablation in paroxysmal atrial fibrillation: a prospective, randomized study. J Am Heart Assoc 2014;3:e000877.
- Arya A, Hindricks G, Sommer P, Huo Y, Bollmann A, Gaspar T, Bode K, Husser D, Kottkamp H, Piorkowski C. Long-term results and the predictors of outcome of catheter ablation of atrial fibrillation using steerable sheath catheter navigation after single procedure in 674 patients. Europace 2010;12:173-180.
- Atienza F, Almendral J, Jalife J, Zlochiver S, Ploutz-Snyder R, Torrecilla EG, Arenal A, Kalifa J, Fernandez-Aviles F, Berenfeld O. Real-time dominant frequency mapping and ablation of dominant frequency sites in atrial fibrillation with left-to-right frequency gradients predicts long-term maintenance of sinus rhythm. Heart Rhythm 2009;6:33-40.
- Bansch D, Bittkau J, Schneider R, Schneider C, Wendig I, Akin I, Nienaber CA. Circumferential pulmonary vein isolation: wait or stop early after initial successful pulmonary vein isolation?Europace 2013;15:183-188.
- Bassiouny M, Saliba W, Hussein A, Rickard J, Diab M, Aman W, Dresing T, Tt Callahan, Bhargava M, Martin DO, Shao M, Baranowski B, Tarakji K, Tchou PJ, Hakim A, Kanj M, Lindsay B, Wazni O. Randomized study of persistent atrial fibrillation ablation: ablate in sinus rhythm versus ablate complex-fractionated atrial electrograms in atrial fibrillation. Circ Arrhythm Electrophysiol 2016;9:e003596.
- Berruezo A, Tamborero D, Mont L, Benito B, Tolosana JM, Sitges M, Vidal B, Arriagada G, Mendez F, Matiello M, Molina I, Brugada J. Pre-procedural predictors of atrial fibrillation recurrence after circumferential pulmonary vein ablation. Eur Heart J 2007;28:836-841.
- Bertaglia E, Senatore G, De Michieli L, De Simone A, Amellone C, Ferretto S, La Rocca V, Giuggia M, Corrado D, Zoppo F, Stabile G. Twelve-year follow-up of catheter ablation for atrial fibrillation: a prospective, multicenter, randomized study. Heart Rhythm 2017;14:486-492.
- Bertaglia E, Tondo C, De Simone A, Zoppo F, Mantica M, Turco P, Iuliano A, Forleo G, La Rocca V, Stabile G. Does catheter ablation cure atrial fibrillation? Single-procedure outcome of drug-refractory atrial fibrillation ablation: a 6-year multicentre experience. Europace 2010;12:181-187.
- Blanche C, Tran N, Rigamonti F, Burri H, Zimmermann M. Value of P-wave signal averaging to predict atrial fibrillation recurrences after pulmonary vein isolation. Europace 2013;15:198-204.
- Blandino A, Bianchi F, Grossi S, Biondi-Zoccai G, Conte MR, Gaido L, Gaita F, Scaglione M, Rametta F. Left atrial substrate modification targeting low-voltage areas for catheter ablation of atrial fibrillation: a systematic review and metaanalysis. Pacing Clin Electrophysiol 2017;40:199-212.
- Blomstrom-Lundqvist C, Gizurarson S, Schwieler J, Jensen SM, Bergfeldt L, Kenneback G, Rubulis A, Malmborg H, Raatikainen P, Lonnerholm S, Hoglund N, Mortsell D. Effect of catheter ablation vs antiarrhythmic medication on quality of life in patients with atrial fibrillation: the CAPTAF randomized clinical trial. JAMA 2019;321:1059-1068.
- Boersma LV, van der Voort P, Debruyne P, Dekker L, Simmers T, Rossenbacker T, Balt J, Wijffels M, Degreef Y. Multielectrode pulmonary vein isolation versus single tip wide area catheter ablation for paroxysmal atrial fibrillation: a multinational multicenter randomized clinical trial. Circ Arrhythm Electrophysiol 2016;9:e003151.
- Bollmann A, Ueberham L, Schuler E, Wiedemann M, Reithmann C, Sause A, Tebbenjohanns J, Schade A, Shin DI, Staudt A, Zacharzowsky U, Ulbrich M, Wetzel U, Neuser H, Bode K, Kuhlen R, Hindricks G. Cardiac tamponade in catheter ablation of atrial fibrillation: German-wide analysis of 21 141 procedures in the Helios atrial fibrillation ablation registry (SAFER). Europace 2018;20:1944-1951.
- Bordignon S, Furnkranz A, Perrotta L, Dugo D, Konstantinou A, Nowak B, Schulte-Hahn B, Schmidt B, Chun KR. High rate of durable pulmonary vein isolation after second-generation cryoballoon ablation: analysis of repeat procedures. Europace 2015;17:725-731.
- Boveda S, Providencia R, Defaye P, Pavin D, Cebron JP, Anselme F, Halimi F, Khoueiry Z, Combes N, Combes S, Jacob S, Albenque JP, Sousa P. Outcomes after cryoballoon or radiofrequency ablation for persistent atrial fibrillation: a multicentric propensity-score matched study. J Interv Card Electrophysiol 2016;47:133-142.
- Brembilla-Perrot B, Ferreira JP, Manenti V, Sellal JM, Olivier A, Villemin T, Beurrier D, De Chillou C, Louis P, Brembilla A, Juilliere Y, Girerd N. Predictors and prognostic significance of tachycardiomyopathy: insights from a cohort of 1269 patients undergoing atrial flutter ablation. Eur J Heart Fail 2016;18:394-401.
- Briceno DF, Markman TM, Lupercio F, Romero J, Liang JJ, Villablanca PA, Birati EY, Garcia FC, Di Biase L, Natale A, Marchlinski FE, Santangeli P. Catheter ablation versus conventional treatment of atrial fibrillation in patients with heart failure with reduced ejection fraction: a systematic review and meta-analysis of randomized controlled trials. J Interv Card Electrophysiol 2018;53:19-29.
- Buiatti A, von Olshausen G, Barthel P, Schneider S, Luik A, Kaess B, Laugwitz KL, Hoppmann P. Cryoballoon versus radiofrequency ablation for paroxysmal atrial fibrillation: an updated meta-analysis of randomized and observational studies. Europace 2017;19:378-384.
- Buist TJ, Adiyaman A, Smit JJJ, Ramdat Misier AR, Elvan A. Arrhythmia-free survival and pulmonary vein reconnection patterns after second-generation cryoballoon and contact-force radiofrequency pulmonary vein isolation. Clin Res Cardiol 2018;107:498-506.
- C, Mansour MC, Melby DP, Packer DL, Nakagawa H, Zhang B, Stagg RB, Boo LM, Marchlinski FE. Paroxysmal AF catheter ablation with a contact force sensing catheter: results of the prospective, multicenter SMART-AF trial. J Am Coll Cardiol 2014;64:647-656.
- Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen PS, Chen SA, Chung MK, Nielsen JC, Curtis AB, Davies DW, Day JD, d’Avila A, de Groot N, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao HM, Verma A, Wilber DJ, Yamane T. 2017 HRS/ EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. Europace 2018;20:157-208.
- Calkins H, Reynolds MR, Spector P, Sondhi M, Xu Y, Martin A, Williams CJ, Sledge I. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol 2009;2:349-361.
- Canpolat U, Aytemir K, Yorgun H, Sahiner L, Kaya EB, Oto A. A proposal for a new scoring system in the prediction of catheter ablation outcomes: promising results from the Turkish Cryoablation Registry. Int J Cardiol 2013;169:201-206.
- Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, Klein G, Natale A, Packer D, Skanes A, Ambrogi F, Biganzoli E. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol 2010;3:32-38.
- Cardoso R, Mendirichaga R, Fernandes G, Healy C, Lambrakos LK, Viles-Gonzalez JF, Goldberger JJ, Mitrani RD. Cryoballoon versus radiofrequency catheter ablation in atrial fibrillation: a meta-analysis. J Cardiovasc Electrophysiol 2016;27:1151-1159.
- Chang SL, Tuan TC, Tai CT, Lin YJ, Lo LW, Hu YF, Tsao HM, Chang CJ, Tsai WC, Chen SA. Comparison of outcome in catheter ablation of atrial fibrillation in patients with versus without the metabolic syndrome. Am J Cardiol 2009;103:67-72.
- Chao TF, Hung CL, Tsao HM, Lin YJ, Yun CH, Lai YH, Chang SL, Lo LW, Hu YF, Tuan TC, Chang HY, Kuo JY, Yeh HI, Wu TJ, Hsieh MH, Yu WC, Chen SA. Epicardial adipose tissue thickness and ablation outcome of atrial fibrillation. PLoS One 2013;8:e74926.
- Cheema A, Dong J, Dalal D, Marine JE, Henrikson CA, Spragg D, Cheng A, Nazarian S, Bilchick K, Sinha S, Scherr D, Almasry I, Halperin H, Berger R, Calkins H. Incidence and time course of early recovery of pulmonary vein conduction after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 2007;18:387-391.
- Chen C, Zhou X, Zhu M, Chen S, Chen J, Cai H, Dai J, Xu X, Mao W. Catheter ablation versus medical therapy for patients with persistent atrial fibrillation: a systematic review and meta-analysis of evidence from randomized controlled trials. J Interv Card Electrophysiol 2018;52:9-18.
- Chen CF, Gao XF, Duan X, Chen B, Liu XH, Xu YZ. Comparison of catheter ablation for paroxysmal atrial fibrillation between cryoballoon and radiofrequency: a meta-analysis. J Interv Card Electrophysiol 2017;48:351-366.
- Chilukuri K, Dalal D, Gadrey S, Marine JE, Macpherson E, Henrikson CA, Cheng A, Nazarian S, Sinha S, Spragg D, Berger R, Calkins H. A prospective study evaluating the role of obesity and obstructive sleep apnea for outcomes after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 2010;21:521-525.
- Congrete S, Bintvihok M, Thongprayoon C, Bathini T, Boonpheng B, Sharma K, Chokesuwattanaskul R, Srivali N, Tanawuttiwat T, Cheungpasitporn W. Effect of obstructive sleep apnea and its treatment of atrial fibrillation recurrence after radiofrequency catheter ablation: a meta-analysis. J Evid BasedMed 2018;11:145-151.
- Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, Pehrson S, Englund A, Hartikainen J, Mortensen LS, Hansen PS. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med 2012;367:1587-1595.
- Costa FM, Ferreira AM, Oliveira S, Santos PG, Durazzo A, Carmo P, Santos KR, Cavaco D, Parreira L, Morgado F, Adragao P. Left atrial volume is more important than the type of atrial fibrillation in predicting the long-term success of catheter ablation. Int J Cardiol 2015;184:56-61.
- D’Ascenzo F, Corleto A, Biondi-Zoccai G, Anselmino M, Ferraris F, di Biase L, Natale A, Hunter RJ, Schilling RJ, Miyazaki S, Tada H, Aonuma K, Yenn-Jiang L, Tao H, Ma C, Packer D, Hammill S, Gaita F. Which are the most reliable predictors of recurrence of atrial fibrillation after transcatheter ablation?: a meta-analysis. Int J Cardiol 2013;167:1984-1989.
- Da Costa A, Levallois M, Romeyer-Bouchard C, Bisch L, Gate-Martinet A, Isaaz K. Remote-controlled magnetic pulmonary vein isolation combined with superior vena cava isolation for paroxysmal atrial fibrillation: a prospective randomized study. Arch Cardiovasc Dis 2015;108:163-171.
- Dagres N, Varounis C, Gaspar T, Piorkowski C, Eitel C, Iliodromitis EK, Lekakis JP, Flevari P, Simeonidou E, Rallidis LS, Tsougos E, Hindricks G, Sommer P, Anastasiou-Nana M. Catheter ablation for atrial fibrillation in patients with left ventricular systolic dysfunction. A systematic review and meta-analysis. J Card Fail 2011;17:964-970.
- De Greef Y, Schwagten B, Chierchia GB, de Asmundis C, Stockman D, Buysschaert I. Diagnosis-to-ablation time as a predictor of success: early choice for pulmonary vein isolation and long-term outcome in atrial fibrillation: results from the Middelheim-PVI registry. Europace 2018;20:589-595.
- De Greef Y, Stroker E, Schwagten B, Kupics K, De Cocker J, Chierchia GB, de Asmundis C, Stockman D, Buysschaert I. Complications of pulmonary vein isolation in atrial fibrillation: predictors and comparison between four different ablation techniques: results from the Middelheim PVI-registry. Europace 2018;20:1279-1286.
- De Maat GE, Mulder B, Berretty WL, Al-Jazairi MIH, Tan YES, Wiesfeld ACP, Mariani MA, Van Gelder IC, Rienstra M, Blaauw Y. Obesity is associated with impaired long-term success of pulmonary vein isolation: a plea for risk factor management before ablation. Open Heart 2018;5:e000771.
- Deng F, Raza A, Guo J. Treating obstructive sleep apnea with continuous positive airway pressure reduces risk of recurrent atrial fibrillation after catheter ablation: a meta-analysis. Sleep Med 2018;46:5-11.
- Deng H, Bai Y, Shantsila A, Fauchier L, Potpara TS, Lip GYH. Clinical scores for outcomes of rhythm control or arrhythmia progression in patients with atrial fibrillation: a systematic review. Clin Res Cardiol 2017;106:813-823.
- Deshmukh A, Patel NJ, Pant S, Shah N, Chothani A, Mehta K, Grover P, Singh V, Vallurupalli S, Savani GT, Badheka A, Tuliani T, Dabhadkar K, Dibu G, Reddy YM, Sewani A, Kowalski M, Mitrani R, Paydak H, Viles-Gonzalez JF. In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010: analysis of 93 801 procedures. Circulation 2013;128:2104-2112.
- Di Biase L, Burkhardt JD, Mohanty P, Mohanty S, Sanchez JE, Trivedi C, Gunes M, Gokoglan Y, Gianni C, Horton RP, Themistoclakis S, Gallinghouse GJ, Bailey S, Zagrodzky JD, Hongo RH, Beheiry S, Santangeli P, Casella M, Dello Russo A, Al-Ahmad A, Hranitzky P, Lakkireddy D, Tondo C, Natale A. Left atrial appendage isolation in patients with longstanding persistent af undergoing catheter ablation: BELIEF trial. J Am Coll Cardiol 2016;68:1929-1940.
- Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D, Reddy M, Jais P, Themistoclakis S, Dello Russo A, Casella M, Pelargonio G, Narducci ML, Schweikert R, Neuzil P, Sanchez J, Horton R, Beheiry S, Hongo R, Hao S, Rossillo A, Forleo G, Tondo C, Burkhardt JD, Haissaguerre M, Natale A. Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device: results from the AATAC multicenter randomized trial. Circulation 2016;133:1637-1644.
- Driessen AHG, Berger WR, Krul SPJ, van den Berg NWE, Neefs J, Piersma FR, Chan Pin Yin D, de Jong J, van Boven WP, de Groot JR. Ganglion plexus ablation in advanced atrial fibrillation: the AFACT study. J Am Coll Cardiol 2016;68:1155-1165.
- Dukkipati SR, Cuoco F, Kutinsky I, Aryana A, Bahnson TD, Lakkireddy D, Woollett I, Issa ZF, Natale A, Reddy VY; HeartLight Study Investigators. Pulmonary vein isolation using the visually guided laser balloon: a prospective, multicenter, and randomized comparison to standard radiofrequency ablation. J Am Coll Cardiol 2015;66:1350-1360.
- Elgendy AY, Mahmoud AN, Khan MS, Sheikh MR, Mojadidi MK, Omer M, Elgendy IY, Bavry AA, Ellenbogen KA, Miles WM, McKillop M. Meta-analysis comparing catheter-guided ablation versus conventional medical therapy for patients with atrial fibrillation and heart failure with reduced ejection fraction. Am J Cardiol 2018;122:806-813.
- Faustino M, Pizzi C, Agricola T, Xhyheri B, Costa GM, Flacco ME, Capasso L, Cicolini G, Di Girolamo E, Leonzio L, Manzoli L. Stepwise ablation approach versus pulmonary vein isolation in patients with paroxysmal atrial fibrillation: randomized controlled trial. Heart Rhythm 2015;12:1907-1915.
- Fink T, Metzner A, Willems S, Eckardt L, Ince H, Brachmann J, Spitzer SG, Deneke T, Schmitt C, Hochadel M, Senges J, Rillig A. Procedural success, safety and patients satisfaction after second ablation of atrial fibrillation in the elderly: results from the German ablation registry. Clin Res Cardiol 2019;108:1354-1363.
- Fink T, Schluter M, Heeger CH, Lemes C, Maurer T, Reissmann B, Riedl J, Rottner L, Santoro F, Schmidt B, Wohlmuth P, Mathew S, Sohns C, Ouyang F, Metzner A, Kuck KH. Stand-alone pulmonary vein isolation versus pulmonary vein isolation with additional substrate modification as index ablation procedures in patients with persistent and long-standing persistent atrial fibrillation: the randomized Alster-Lost-AF trial (Ablation at St. Georg Hospital for longstanding persistent atrial fibrillation). Circ Arrhythm Electrophysiol 2017;10.
- Forleo GB, Mantica M, De Luca L, Leo R, Santini L, Panigada S, De Sanctis V, Pappalardo A, Laurenzi F, Avella A, Casella M, Dello Russo A, Romeo F, Pelargonio G, Tondo C. Catheter ablation of atrial fibrillation in patients with diabetes mellitus type 2: results from a randomized study comparing pulmonary vein isolation versus antiarrhythmic drug therapy. J Cardiovasc Electrophysiol 2009;20:22-28.
- Gaita F, Scaglione M, Battaglia A, Matta M, Gallo C, Galata M, Caponi D, Di Donna P, Anselmino M. Very long-term outcome following transcatheter ablation of atrial fibrillation. Are results maintained after 10 years of followup? Europace 2018;20:443-450.
- Ganesan AN, Shipp NJ, Brooks AG, Kuklik P, Lau DH, Lim HS, Sullivan T, Roberts-Thomson KC, Sanders P. Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc 2013;2:e004549.
- Gianni C, Mohanty S, Di Biase L, Metz T, Trivedi C, Gokoglan Y, Gunes MF, Bai R, Al-Ahmad A, Burkhardt JD, Gallinghouse GJ, Horton RP, Hranitzky PM, Sanchez JE, Halbfass P, Muller P, Schade A, Deneke T, Tomassoni GF, Natale A. Acute and early outcomes of focal impulse and rotor modulation (FIRM)-guided rotors-only ablation in patients with nonparoxysmal atrial fibrillation. Heart Rhythm 2016;13:830-835.
- Glover BM, Hong KL, Dagres N, Arbelo E, Laroche C, Riahi S, Bertini M, Mikhaylov EN, Galvin J, Kiliszek M, Pokushalov E, Kautzner J, Calvo N, Blomstrom-Lundqvist C, Brugada J; ESC-EHRA Atrial Fibrillation Ablation Long-Term Registry Investigators. Impact of body mass index on the outcome of catheter ablation of atrial fibrillation. Heart 2019;105:244-250.
- Gunawardene MA, Hoffmann BA, Schaeffer B, Chung DU, Moser J, Akbulak RO, Jularic M, Eickholt C, Nuehrich J, Meyer C, Willems S. Influence of energy source on early atrial fibrillation recurrences: a comparison of cryoballoon versus radiofrequency current energy ablation with the endpoint of unexcitability in pulmonary vein isolation. Europace 2018;20:43-49.
- Haissaguerre M, Hocini M, Sanders P, Sacher F, Rotter M, Takahashi Y, Rostock T, Hsu LF, Bordachar P, Reuter S, Roudaut R, Clementy J, Jais P. Catheter ablation of long-lasting persistent atrial fibrillation: clinical outcome and mechanisms of subsequent arrhythmias. J Cardiovasc Electrophysiol 2005b;16:1138-1147.
- Haissaguerre M, Sanders P, Hocini M, Takahashi Y, Rotter M, Sacher F, Rostock T, Hsu LF, Bordachar P, Reuter S, Roudaut R, Clementy J, Jais P. Catheter ablation of long-lasting persistent atrial fibrillation: critical structures for termination. J Cardiovasc Electrophysiol 2005a;16:1125-1137.
- Hakalahti A, Biancari F, Nielsen JC, Raatikainen MJ. Radiofrequency ablation versus antiarrhythmic drug therapy as first line treatment of symptomatic atrial fibrillation: systematic review and meta-analysis. Europace 2015;17:370-378.
- Herrera Siklody C, Arentz T, Minners J, Jesel L, Stratz C, Valina CM, Weber R, Kalusche D, Toti F, Morel O, Trenk D. Cellular damage, platelet activation, and inflammatory response after pulmonary vein isolation: a randomized study comparing radiofrequency ablation with cryoablation. Heart Rhythm 2012;9:189-196.
- Herrera Siklody C, Deneke T, Hocini M, Lehrmann H, Shin DI, Miyazaki S, Henschke S, Fluegel P, Schiebeling-Romer J, Bansmann PM, Bourdias T, Dousset V, Haissaguerre M, Arentz T. Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. J Am Coll Cardiol 2011;58:681-688.
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS) (published online ahead of print, 2020 Aug 29). Eur Heart J. 2020;ehaa612. doi:10.1093/eurheartj/ehaa612.
- Hindricks G, Sepehri Shamloo A, Lenarczyk R, Kalarus Z, Arya A, Kircher S, Darma A, Dagres N. Catheter ablation of atrial fibrillation: current status, techniques, outcomes and challenges. Kardiol Pol 2018;76:1680-1686.
- Hu X, Jiang J, Ma Y, Tang A. Is there still a role for additional linear ablation in addition to pulmonary vein isolation in patients with paroxysmal atrial fibrillation? An updated meta-analysis of randomized controlled trials. Int J Cardiol 2016;209:266-274.
- Hummel J, Michaud G, Hoyt R, DeLurgio D, Rasekh A, Kusumoto F, Giudici M, Dan D, Tschopp D, Calkins H, Boersma L; TTOP-AF Investigators. Phased RF ablation in persistent atrial fibrillation. Heart Rhythm 2014;11:202-209.
- Hunter RJ, Baker V, Finlay MC, Duncan ER, Lovell MJ, Tayebjee MH, Ullah W, Siddiqui MS, Mc LA, Richmond L, Kirkby C, Ginks MR, Dhinoja M, Sporton S, Earley MJ, Schilling RJ. Point-by-point radiofrequency ablation versus the cryoballoon or a novel combined approach: a randomized trial comparing 3 methods of pulmonary vein isolation for paroxysmal atrial fibrillation (the Cryo Versus RF trial). J Cardiovasc Electrophysiol 2015;26:1307-1314.
- Hunter RJ, Berriman TJ, Diab I, Kamdar R, Richmond L, Baker V, Goromonzi F, Sawhney V, Duncan E, Page SP, Ullah W, Unsworth B, Mayet J, Dhinoja M, Earley MJ, Sporton S, Schilling RJ. A randomized controlled trial of catheter ablation versus medical treatment of atrial fibrillation in heart failure (the CAMTAF trial). Circ Arrhythm Electrophysiol 2014;7:31-38.
- Jais P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, Hocini M, Extramiana F, Sacher F, Bordachar P, Klein G, Weerasooriya R, Clementy J, Haissaguerre M. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation 2008;118:2498-2505.
- Jaïs P, O’Neill MD, Takahashi Y, Jo¨nsson A, Hocini M, Sacher F, Sanders P, Kodali S, Rostock T, Rotter M, Cle´menty J, Haı¨ssaguerre M. Stepwise catheter ablation of chronic atrial fibrillation:importance of discrete anatomic sites for termination. J Cardiovasc Electrophysiol 2006;17:S28-S36.
- Jiang RH, Po SS, Tung R, Liu Q, Sheng X, Zhang ZW, Sun YX, Yu L, Zhang P, Fu GS, Jiang CY. Incidence of pulmonary vein conduction recovery in patients without clinical recurrence after ablation of paroxysmal atrial fibrillation: mechanistic implications. Heart Rhythm 2014;11:969-976.
- Jones DG, Haldar SK, Hussain W, Sharma R, Francis DP, Rahman-Haley SL, McDonagh TA, Underwood SR, Markides V, Wong T. A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure. J Am Coll Cardiol 2013;61:1894-1903.
- Jongnarangsin K, Chugh A, Good E, Mukerji S, Dey S, Crawford T, Sarrazin JF, Kuhne M, Chalfoun N, Wells D, Boonyapisit W, Pelosi F, Jr., Bogun F,Morady F, Oral H. Body mass index, obstructive sleep apnea, and outcomes of catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 2008;19:668-672.
- Kabunga P, Phan K, Ha H, Sy RW. Meta-analysis of contemporary atrial fibrillation ablation strategies: irrigated radiofrequency versus duty-cycled phased radiofrequency versus cryoballoon ablation. JACC Clin Electrophysiol 2016;2:377-390.
- Kang JH, Lee DI, Kim S, Kim MN, Park YM, Ban JE, Choi JI, Lim HE, Park SW, Kim YH. Prediction of long-term outcomes of catheter ablation of persistent atrial fibrillation by parameters of preablation DC cardioversion. J Cardiovasc Electrophysiol 2012;23:1165-1170.
- Katritsis DG, Pokushalov E, Romanov A, Giazitzoglou E, Siontis GC, Po SS, Camm AJ, Ioannidis JP. Autonomic denervation added to pulmonary vein isolation for paroxysmal atrial fibrillation: a randomized clinical trial. J Am Coll Cardiol 2013;62:2318-2325.
- Kawakami H, Nagai T, Fujii A, Uetani T, Nishimura K, Inoue K, Suzuki J, Oka Y, Okura T, Higaki J, Ogimoto A, Ikeda S. Apnea-hypopnea index as a predictor of atrial fibrillation recurrence following initial pulmonary vein isolation: usefulness of type-3 portable monitor for sleep-disordered breathing. J Interv Card Electrophysiol 2016;47:237-244.
- Khan MN, Jais P, Cummings J, Di Biase L, Sanders P, Martin DO, Kautzner J, Hao S, Themistoclakis S, Fanelli R, Potenza D, Massaro R, Wazni O, Schweikert R, Saliba W, Wang P, Al-Ahmad A, Beheiry S, Santarelli P, Starling RC, Dello Russo A, Pelargonio G, Brachmann J, Schibgilla V, Bonso A, Casella M, Raviele A, Haissaguerre M, Natale A; PABA-CHF Investigators. Pulmonary-vein isolation for atrial fibrillation in patients with heart failure. N Engl J Med 2008;359:1778-1785.
- Khan SU, Rahman H, Talluri S, Kaluski E. The clinical benefits and mortality reduction associated with catheter ablation in subjects with atrial fibrillation: a systematic review and meta-analysis. JACC Clin Electrophysiol 2018;4:626-635.
- Kheiri B, Osman M, Abdalla A, Haykal T, Ahmed S, Bachuwa G, Hassan M, Bhatt DL. Catheter ablation of atrial fibrillation with heart failure: an updated meta-analysis of randomized trials. Int J Cardiol 2018;269:170-173.
- Kim TH, Park J, Uhm JS, Joung B, Lee MH, Pak HN. Pulmonary vein reconnection predicts good clinical outcome after second catheter ablation for atrial fibrillation. Europace 2017;19:961-967.
- Kim TH, Uhm JS, Kim JY, Joung B, Lee MH, Pak HN. Does additional electrogram-guided ablation after linear ablation reduce recurrence after catheter ablation for longstanding persistent atrial fibrillation? A prospective randomized study. J Am Heart Assoc 2017;6:e004811.
- Kim YG, Shim J, Choi JI, Kim YH. Radiofrequency catheter ablation improves the quality of life measured with a short form-36 questionnaire in atrial fibrillation patients: a systematic review and meta-analysis. PLoS One 2016;11:e0163755.
- Kircher S, Arya A, Altmann D, Rolf S, Bollmann A, Sommer P, Dagres N, Richter S, Breithardt OA, Dinov B, Husser D, Eitel C, Gaspar T, Piorkowski C, Hindricks G. Individually tailored versus standardized substrate modification during radiofrequency catheter ablation for atrial fibrillation: a randomized study. Europace 2018;20:1766-1775.
- Kirchhof P, Breithardt G, Camm AJ, Crijns HJ, Kuck KH, Vardas P, Wegscheider K. Improving outcomes in patients with atrial fibrillation: rationale and design of the Early treatment of Atrial fibrillation for Stroke prevention Trial. Am Heart J 2013;166:442-448.
- Kornej J, Hindricks G, Arya A, Sommer P, Husser D, Bollmann A. The APPLE score - a novel score for the prediction of rhythm outcomes after repeat catheter ablation of atrial fibrillation. PLoS One 2017;12:e0169933.
- Kornej J, Hindricks G, Shoemaker MB, Husser D, Arya A, Sommer P, Rolf S, Saavedra P, Kanagasundram A, Patrick Whalen S, Montgomery J, Ellis CR, Darbar D, Bollmann A. The APPLE score: a novel and simple score for the prediction of rhythm outcomes after catheter ablation of atrial fibrillation. Clin Res Cardiol 2015;104:871-876.
- Kornej J, Schumacher K, Dinov B, Kosich F, Sommer P, Arya A, Husser D, Bollmann A, Lip GYH, Hindricks G. Prediction of electro-anatomical substrate and arrhythmia recurrences using APPLE, DR-FLASH and MB-LATER scores in patients with atrial fibrillation undergoing catheter ablation. Sci Rep 2018;8:12686.
- Kosich F, Schumacher K, Potpara T, Lip GY, Hindricks G, Kornej J. Clinical scores used for the prediction of negative events in patients undergoing catheter ablation for atrial fibrillation. Clin Cardiol 2019;42:320-329.
- Kosiuk J, Dinov B, Kornej J, Acou WJ, Schonbauer R, Fiedler L, Buchta P, Myrda K, Gasior M, Polonski L, Kircher S, Arya A, Sommer P, Bollmann A, Hindricks G, Rolf S. Prospective, multicenter validation of a clinical risk score for left atrial arrhythmogenic substrate based on voltage analysis: DR-FLASH score. Heart Rhythm 2015;12:2207-2212.
- Krittayaphong R, Raungrattanaamporn O, Bhuripanyo K, Sriratanasathavorn C, Pooranawattanakul S, Punlee K, Kangkagate C. A randomized clinical trial of the efficacy of radiofrequency catheter ablation and amiodarone in the treatment of symptomatic atrial fibrillation. J Med Assoc Thai 2003;86 Suppl 1:S8-16.
- Kuck KH, Brugada J, Furnkranz A, Metzner A, Ouyang F, Chun KR, Elvan A, Arentz T, Bestehorn K, Pocock SJ, Albenque JP, Tondo C; FIRE AND ICE Investigators. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med 2016;374:2235-2245.
- Kuck KH, Furnkranz A, Chun KR, Metzner A, Ouyang F, Schluter M, Elvan A, Lim HW, Kueffer FJ, Arentz T, Albenque JP, Tondo C, Kuhne M, Sticherling C, Brugada J; FIRE AND ICE Investigators. Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur Heart J 2016;37:2858-2865.
- Kuck KH, Hoffmann BA, Ernst S, Wegscheider K, Treszl A, Metzner A, Eckardt L, Lewalter T, Breithardt G, Willems S; Gap-AFAFNET 1 Investigators. Impact of complete versus incomplete circumferential lines around the pulmonary veins during catheter ablation of paroxysmal atrial fibrillation: results from the Gap-Atrial Fibrillation-German Atrial Fibrillation Competence Network 1 trial. Circ Arrhythm Electrophysiol 2016;9:e003337.
- Kuck KH, Merkely B, Zahn R, Arentz T, Seidl K, Schluter M, Tilz RR, Piorkowski C, Geller L, Kleemann T, Hindricks G. Catheter ablation versus best medical therapy in patients with persistent atrial fibrillation and congestive heart failure: the randomized AMICA trial. Circ Arrhythm Electrophysiol 2019;12:e007731.
- Lee G, Sparks PB, Morton JB, Kistler PM, Vohra JK, Medi C, Rosso R, Teh A, Halloran K, Kalman JM. Low risk of major complications associated with pulmonary vein antral isolation for atrial fibrillation: results of 500 consecutive ablation procedures in patients with low prevalence of structural heart disease from a single center. J Cardiovasc Electrophysiol 2011;22:163-168.
- Letsas KP, Weber R, Burkle G, Mihas CC, Minners J, Kalusche D, Arentz T. Preablative predictors of atrial fibrillation recurrence following pulmonary vein isolation: the potential role of inflammation. Europace 2009;11:158-163.
- Li L, Wang ZW, Li J, Ge X, Guo LZ, Wang Y, Guo WH, Jiang CX, Ma CS. Efficacy of catheter ablation of atrial fibrillation in patients with obstructive sleep apnoea with and without continuous positive airway pressure treatment: a meta-analysis of observational studies. Europace 2014;16:1309-1314.
- Luik A, Radzewitz A, Kieser M, Walter M, Bramlage P, Hormann P, Schmidt K, Horn N, Brinkmeier-Theofanopoulou M, Kunzmann K, Riexinger T, Schymik G, Merkel M, Schmitt C. Cryoballoon versus open irrigated radiofrequency ablation in patients with paroxysmal atrial fibrillation: the prospective, randomized, controlled, noninferiority FreezeAF study. Circulation 2015;132:1311-1319.
- Ma Y, Bai F, Qin F, Li Y, Tu T, Sun C, Zhou S, Liu Q. Catheter ablation for treatment of patients with atrial fibrillation and heart failure: a meta-analysis of randomized controlled trials. BMC Cardiovasc Disord 2018;18:165.
- MacDonald MR, Connelly DT, Hawkins NM, Steedman T, Payne J, Shaw M, Denvir M, Bhagra S, Small S, Martin W, McMurray JJ, Petrie MC. Radiofrequency ablation for persistent atrial fibrillation in patients with advanced heart failure and severe left ventricular systolic dysfunction: a randomised controlled trial. Heart 2011;97:740-747.
- Mahajan R, Lau DH, Brooks AG, Shipp NJ, Manavis J, Wood JPM, Finnie JW, Samuel CS, Royce SG, Twomey DJ, Thanigaimani S, Kalman JM, Sanders P. Electrophysiological, electroanatomical, and structural remodeling of the atria as consequences of sustained obesity. J Am Coll Cardiol 2015;66:1-11.
- Mark DB, Anstrom KJ, Sheng S, Piccini JP, Baloch KN, Monahan KH, Daniels MR, Bahnson TD, Poole JE, Rosenberg Y, Lee KL, Packer DL. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 2019;321:1275-1285.
- Mark DB, Anstrom KJ, Sheng S, Piccini JP, Baloch KN, Monahan KH, Daniels MR, Bahnson TD, Poole JE, Rosenberg Y, Lee KL, Packer DL; CABANA Investigators. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 2019.
- Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, Merkely B, Pokushalov E, Sanders P, Proff J, Schunkert H, Christ H, Vogt J, Bansch D; CASTLE-AF Investigators. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 2018;378:417-427.
- Marrouche NF, Wilber D, Hindricks G, Jais P, Akoum N, Marchlinski F, Kholmovski E, Burgon N, Hu N, Mont L, Deneke T, Duytschaever M, Neumann T, Mansour M, Mahnkopf C, Herweg B, Daoud E, Wissner E, Bansmann P, Brachmann J. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA 2014;311:498-506.
- Martin CA, Lambiase PD. Pathophysiology, diagnosis and treatment of tachycardiomyopathy. Heart 2017;103:1543-1552.
- Masuda M, Mizuno H, Enchi Y, Minamiguchi H, Konishi S, Ohtani T, Yamaguchi O, Okuyama Y, Nanto S, Sakata Y. Abundant epicardial adipose tissue surrounding the left atrium predicts early rather than late recurrence of atrial fibrillation after catheter ablation. J Interv Card Electrophysiol 2015;44:31-37.
- Matiello M, Nadal M, Tamborero D, Berruezo A, Montserrat J, Embid C, Rios J, Villacastin J, Brugada J, Mont L. Low efficacy of atrial fibrillation ablation in severe obstructive sleep apnoea patients. Europace 2010;12:1084-1089.
- McLellan AJ, Ling LH, Azzopardi S, Lee GA, Lee G, Kumar S, Wong MC, Walters TE, Lee JM, Looi KL, Halloran K, Stiles MK, Lever NA, Fynn SP, Heck PM, Sanders P, Morton JB, Kalman JM, Kistler PM. A minimal or maximal ablation strategy to achieve pulmonary vein isolation for paroxysmal atrial fibrillation: a prospective multi-centre randomized controlled trial (the Minimax study). Eur Heart J 2015;36:1812-1821.
- Medi C, Sparks PB, Morton JB, Kistler PM, Halloran K, Rosso R, Vohra JK, Kumar S, Kalman JM. Pulmonary vein antral isolation for paroxysmal atrial fibrillation: results from long-term follow-up. J Cardiovasc Electrophysiol 2011;22:137-141.
- Mesquita J, Ferreira AM, Cavaco D, Moscoso Costa F, Carmo P, Marques H, Morgado F, Mendes M, Adragao P. Development and validation of a risk score for predicting atrial fibrillation recurrence after a first catheter ablation procedure - ATLAS score. Europace 2018;20:f428-f435.
- Mohanty S, Mohanty P, Di Biase L, Bai R, Pump A, Santangeli P, Burkhardt D, Gallinghouse JG, Horton R, Sanchez JE, Bailey S, Zagrodzky J, Natale A. Impact of metabolic syndrome on procedural outcomes in patients with atrial fibrillation undergoing catheter ablation. J Am Coll Cardiol 2012;59:1295-1301.
- Mont L, Bisbal F, Hernandez-Madrid A, Perez-Castellano N, Vinolas X, Arenal A, Arribas F, Fernandez-Lozano I, Bodegas A, Cobos A, Matia R, Perez-Villacastin J, Guerra JM, Avila P, Lopez-Gil M, Castro V, Arana JI, Brugada J; SARA investigators. Catheter ablation versus antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study). Eur Heart J 2014;35:501-507.
- Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, Sterns LD, Beresh H, Healey JS, Natale A; RAAFT Investigators. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA 2014;311:692-700.
- Mortsell D, Arbelo E, Dagres N, Brugada J, Laroche C, Trines SA, Malmborg H, Hoglund N, Tavazzi L, Pokushalov E, Stabile G, Blomstrom-Lundqvist C; ESCEHRA Atrial Fibrillation Ablation Long-Term Registry Investigators. Cryoballoon versus radiofrequency ablation for atrial fibrillation: a study of outcome and safety based on the ESC-EHRA atrial fibrillation ablation long-term registry and the Swedish catheter ablation registry. Europace 2019;21:581-589.
- Mujovic N, Marinkovic M, Markovic N, Shantsila A, Lip GY, Potpara TS. Prediction of very late arrhythmia recurrence after radiofrequency catheter ablation of atrial fibrillation: the MB-LATER clinical score. Sci Rep 2017;7:40828.
- Murray MI, Arnold A, Younis M, Varghese S, Zeiher AM. Cryoballoon versus radiofrequency ablation for paroxysmal atrial fibrillation: a meta-analysis of randomized controlled trials. Clin Res Cardiol 2018;107:658-669.
- Nademanee K, McKenzie J, Kosar E, Schwab M, Sunsaneewitayakul B, Vasavakul T, Khunnawat C, Ngarmukos T. A new approach for catheter ablation of atrial fibrillation: mapping of the electrophysiologic substrate. J Am Coll Cardiol 2004;43:2044-2053.
- Nagashima K, Okumura Y, Watanabe I, Nakahara S, Hori Y, Iso K, Watanabe R, Arai M, Wakamatsu Y, Kurokawa S, Mano H, Nakai T, Ohkubo K, Hirayama A. Hot balloon versus cryoballoon ablation for atrial fibrillation: lesion characteristics and middle-term outcomes. Circ Arrhythm Electrophysiol 2018;11:e005861.
- Nakahara S, Hori Y, Kobayashi S, Sakai Y, Taguchi I, Takayanagi K, Nagashima K, Sonoda K, Kogawa R, Sasaki N, Watanabe I, Okumura Y. Epicardial adipose tissue-based defragmentation approach to persistent atrial fibrillation: its impact on complex fractionated electrograms and ablation outcome. Heart Rhythm 2014;11:1343-1351.
- Nakamura K, Naito S, Kaseno K, Tsukada N, Sasaki T, Hayano M, Nishiuchi S, Fuke E, Miki Y, Sakamoto T, Nakamura K, Kumagai K, Kataoka A, Takaoka H, Kobayashi Y, Funabashi N, Oshima S. Optimal observation time after completion of circumferential pulmonary vein isolation for atrial fibrillation to prevent chronic pulmonary vein reconnections. Int J Cardiol 2013;168:5300-5310.
- Nanthakumar K, Plumb VJ, Epstein AE, Veenhuyzen GD, Link D, Kay GN. Resumption of electrical conduction in previously isolated pulmonary veins: rationale for a different strategy?Circulation 2004;109:1226-1229.
- Naruse Y, Tada H, Satoh M, Yanagihara M, Tsuneoka H, Hirata Y, Ito Y, Kuroki K, Machino T, Yamasaki H, Igarashi M, Sekiguchi Y, Sato A, Aonuma K. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm 2013;10:331-337.
- Natale A, Newby KH, Pisano E, Leonelli F, Fanelli R, Potenza D, Beheiry S, Tomassoni G. Prospective randomized comparison of antiarrhythmic therapy versus first-line radiofrequency ablation in patients with atrial flutter. J Am Coll Cardiol 2000;35:1898-1904.
- Natale A, Reddy VY, Monir G, Wilber DJ, Lindsay BD, McElderry HT, Kantipudi
Nedios S, Kosiuk J, Koutalas E, Kornej J, Sommer P, Arya A, Richter S, Rolf S, Husser D, Hindricks G, Bollmann A. Comparison of left atrial dimensions in CT and echocardiography as predictors of long-term success after catheter ablation of atrial fibrillation. J Interv Card Electrophysiol 2015;43:237-244. - Nery PB, Belliveau D, Nair GM, Bernick J, Redpath CJ, Szczotka A, Sadek MM, Green MS, Wells G, Birnie DH. Relationship between pulmonary vein reconnection and atrial fibrillation recurrence: a systematic review and meta-analysis. JACC Clin Electrophysiol 2016;2:474-483.
- Neumann T, Kuniss M, Conradi G, Janin S, Berkowitsch A, Wojcik M, Rixe J, Erkapic D, Zaltsberg S, Rolf A, Bachmann G, Dill T, Hamm CW, Pitschner HF. MEDAFI-Trial (Micro-embolization during ablation of atrial fibrillation): comparison of pulmonary vein isolation using cryoballoon technique versus radiofrequency energy. Europace 2011;13:37-44.
- Neuzil P, Reddy VY, Kautzner J, Petru J, Wichterle D, Shah D, Lambert H, Yulzari A, Wissner E, Kuck KH. Electrical reconnection after pulmonary vein isolation is contingent on contact force during initial treatment: results from the EFFICAS I study. Circ Arrhythm Electrophysiol 2013;6:327-333.
- Ng CY, Liu T, Shehata M, Stevens S, Chugh SS, Wang X. Meta-analysis of obstructive sleep apnea as predictor of atrial fibrillation recurrence after catheter ablation. Am J Cardiol 2011;108:47-51.
- Nielsen JC, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Pehrson SM, Englund A, Hartikainen J, Mortensen LS, Hansen PS; MANTRA-PAF Investigators. Long-term efficacy of catheter ablation as first-line therapy for paroxysmal atrial fibrillation: 5-year outcome in a randomised clinical trial. Heart 2017;103:368-376.
- Njoku A, Kannabhiran M, Arora R, Reddy P, Gopinathannair R, Lakkireddy D, Dominic P. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: a meta-analysis. Europace 2018;20:33-42.
- Noseworthy PA, Gersh BJ, Kent DM, Piccini JP, Packer DL, Shah ND, Yao X. Atrial fibrillation ablation in practice: assessing CABANA generalizability. Eur Heart J 2019;40:1257-1264.
- Noseworthy PA, Van Houten HK, Gersh BJ, Packer DL, Friedman PA, Shah ND, Dunlay SM, Siontis KC, Piccini JP, Yao X. Generalizability of the CASTLEAF trial: catheter ablation for patients with atrial fibrillation and heart failure in routine practice. Heart Rhythm 2020;17:1057-1065.
- Nyong J, Amit G, Adler AJ, Owolabi OO, Perel P, Prieto-Merino D, Lambiase P, Casas JP, Morillo CA. Efficacy and safety of ablation for people with nonparoxysmal atrial fibrillation. Cochrane Database Syst Rev 2016;11:CD012088.
- Oral H, Pappone C, Chugh A, Good E, Bogun F, Pelosi F, Jr., Bates ER, Lehmann MH, Vicedomini G, Augello G, Agricola E, Sala S, Santinelli V, Morady F. Circumferential pulmonary-vein ablation for chronic atrial fibrillation. N Engl J Med 2006;354:934-941.
- Ouyang F, Antz M, Ernst S, Hachiya H, Mavrakis H, Deger FT, Schaumann A, Chun J, Falk P, Hennig D, Liu X, Bansch D, Kuck KH. Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation 2005;111:127-135.
- Ouyang F, Tilz R, Chun J, Schmidt B, Wissner E, Zerm T, Neven K, Kokturk B, Konstantinidou M, Metzner A, Fuernkranz A, Kuck KH. Long-term results of catheter ablation in paroxysmal atrial fibrillation: lessons from a 5-year followup. Circulation 2010;122:2368-2377.
- Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG, Dubuc M, Reddy V, Nelson L, Holcomb RG, Lehmann JW, Ruskin JN; STOP AF Cryoablation Investigators. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J Am Coll Cardiol 2013;61:1713-1723.
- Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE, Noseworthy PA, Rosenberg YD, Jeffries N, Mitchell LB, Flaker GC, Pokushalov E, Romanov A, Bunch TJ, Noelker G, Ardashev A, Revishvili A, Wilber DJ, Cappato R, Kuck KH, Hindricks G, Davies DW, Kowey PR, Naccarelli GV, Reiffel JA, Piccini JP, Silverstein AP, Al-Khalidi HR, Lee KL; CABANA Investigators. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 2019a;321:1261-1274.
- Packer DL, Monahan KH, Al-KhalidiHR, Silverstein AP, Poole JP, Bahnson TD, Mark DB, Lee KL. Ablation of Atrial Fibrillation in Heart Failure Patients: Additional outcomes of the CABANATrial. Heart Rhythm 2019b;16(suppl):S35.
- Pappone C, Augello G, Sala S, Gugliotta F, Vicedomini G, Gulletta S, Paglino G, Mazzone P, Sora N, Greiss I, Santagostino A, LiVolsi L, Pappone N, Radinovic A, Manguso F, Santinelli V. A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation: the APAF Study. J Am Coll Cardiol 2006;48:2340-2347.
- Patel D, Mohanty P, Di Biase L, Shaheen M, Lewis WR, Quan K, Cummings JE, Wang P, Al-Ahmad A, Venkatraman P, Nashawati E, Lakkireddy D, Schweikert R, Horton R, Sanchez J, Gallinghouse J, Hao S, Beheiry S, Cardinal DS, Zagrodzky J, Canby R, Bailey S, Burkhardt JD, Natale A. Safety and efficacy of pulmonary vein antral isolation in patients with obstructive sleep apnea: the impact of continuous positive airway pressure. Circ Arrhythm Electrophysiol 2010;3:445-451.
- Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, Alasady M, Hanley L, Antic NA, McEvoy RD, Kalman JM, Abhayaratna WP, Sanders P. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol 2014;64:2222-2231.
- Perez FJ, Schubert CM, Parvez B, Pathak V, Ellenbogen KA, Wood MA. Longterm outcomes after catheter ablation of cavo-tricuspid isthmus dependent atrial flutter: a meta-analysis. Circ Arrhythm Electrophysiol 2009;2:393-401.
- Perez-Castellano N, Fernandez-Cavazos R, Moreno J, Canadas V, Conde A, Gonzalez-Ferrer JJ, Macaya C, Perez-Villacastin J. The COR trial: a randomized study with continuous rhythm monitoring to compare the efficacy of cryoenergy and radiofrequency for pulmonary vein isolation. Heart Rhythm 2014;11:8-14.
- Phlips T, Taghji P, El Haddad M, Wolf M, Knecht S, Vandekerckhove Y, Tavernier R, Duytschaever M. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace 2018;20:f419-f427.
- Pokushalov E, Romanov A, Artyomenko S, Baranova V, Losik D, Bairamova S, Karaskov A, Mittal S, Steinberg JS. Cryoballoon versus radiofrequency for pulmonary vein re-isolation after a failed initial ablation procedure in patients with paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 2013;24:274-279.
- Prabhu S, Costello BT, Taylor AJ, Gutman SJ, Voskoboinik A, McLellan AJA, Peck KY, Sugumar H, Iles L, Pathik B, Nalliah CJ, Wong GR, Azzopardi SM, Lee G, Mariani J, Kaye DM, Ling LH, Kalman JM, Kistler PM. Regression of diffuse ventricular fibrosis following restoration of sinus rhythm with catheter ablation in patients with atrial fibrillation and systolic dysfunction: a substudy of the CAMERA MRI trial. JACC Clin Electrophysiol 2018;4:999-1007.
- Prabhu S, Taylor AJ, Costello BT, Kaye DM, McLellan AJA, Voskoboinik A, Sugumar H, Lockwood SM, Stokes MB, Pathik B, Nalliah CJ, Wong GR, Azzopardi SM, Gutman SJ, Lee G, Layland J, Mariani JA, Ling LH, Kalman JM, Kistler PM. Catheter ablation versus medical rate control in atrial fibrillation and systolic dysfunction: the CAMERA-MRI study. J Am Coll Cardiol 2017;70:1949-1961.
- Pratola C, Baldo E, Notarstefano P, Toselli T, Ferrari R. Radiofrequency ablation of atrial fibrillation: is the persistence of all intraprocedural targets necessary for long-term maintenance of sinus rhythm?Circulation 2008;117:136-143.
- Qin M, Liu X, Wu SH, Zhang XD. Atrial substrate modification in atrial fibrillation: targeting GP or CFAE? Evidence from meta-analysis of clinical trials. PLoS One 2016;11:e0164989.
- Rajappan K, Kistler PM, Earley MJ, Thomas G, Izquierdo M, Sporton SC, Schilling RJ. Acute and chronic pulmonary vein reconnection after atrial fibrillation ablation: a prospective characterization of anatomical sites. Pacing Clin Electrophysiol 2008;31:1598-1605.
- Raymond-Paquin A, Nattel S, Wakili R, Tadros R. Mechanisms and clinical significance of arrhythmia-induced cardiomyopathy. Can J Cardiol 2018;34:1449-1460.
- Reddy VY, Dukkipati SR, Neuzil P, Natale A, Albenque JP, Kautzner J, Shah D, Michaud G, Wharton M, Harari D, Mahapatra S, Lambert H, Mansour M. Randomized, controlled trial of the safety and effectiveness of a contact forcesensing irrigated catheter for ablation of paroxysmal atrial fibrillation: results of the TactiCath Contact Force Ablation Catheter Study for Atrial Fibrillation (TOCCASTAR) Study. Circulation 2015;132:907-915.
- Reynolds MR, Walczak J, White SA, Cohen DJ, Wilber DJ. Improvements in symptoms and quality of life in patients with paroxysmal atrial fibrillation treated with radiofrequency catheter ablation versus antiarrhythmic drugs. Circ Cardiovasc Qual Outcomes 2010;3:615-623.
- Santangeli P, Zado ES, Hutchinson MD, Riley MP, Lin D, Frankel DS, Supple GE, Garcia FC, Dixit S, Callans DJ, Marchlinski FE. Prevalence and distribution of focal triggers in persistent and long-standing persistent atrial fibrillation. Heart Rhythm 2016;13:374-382.
- Santoro F, Di Biase L, Trivedi C, Burkhardt JD, Paoletti Perini A, Sanchez J, Horton R, Mohanty P, Mohanty S, Bai R, Santangeli P, Lakkireddy D, Reddy M, Elayi CS, Hongo R, Beheiry S, Hao S, Schweikert RA, Viles-Gonzalez J, Fassini G, Casella M, Dello Russo A, Tondo C, Natale A. Impact of uncontrolled hypertension on atrial fibrillation ablation outcome. JACC Clin Electrophysiol 2015;1:164-173.
- Sawhney N, Anousheh R, Chen WC, Narayan S, Feld GK. Five-year outcomes after segmental pulmonary vein isolation for paroxysmal atrial fibrillation. Am J Cardiol 2009;104:366-372.
- Scherr D, Khairy P, Miyazaki S, Aurillac-Lavignolle V, Pascale P, Wilton SB, Ramoul K, Komatsu Y, Roten L, Jadidi A, Linton N, Pedersen M, Daly M, O’Neill M, Knecht S, Weerasooriya R, Rostock T, Manninger M, Cochet H, Shah AJ, Yeim S, Denis A, Derval N, Hocini M, Sacher F, Haissaguerre M, Jais P. Five-year outcome of catheter ablation of persistent atrial fibrillation using termination of atrial fibrillation as a procedural endpoint. Circ Arrhythm Electrophysiol 2015;8:18-24.
- Schmidt M, Dorwarth U, Andresen D, Brachmann J, Kuck K, Kuniss M, Willems S, Deneke T, Tebbenjohanns J, Gerds-Li JH, Spitzer S, Senges J, Hochadel M, Hoffmann E. German ablation registry: cryoballoon versus radiofrequency ablation in paroxysmal atrial fibrillation one-year outcome data. Heart Rhythm 2016;13:836-844.
- Schmidt M, Dorwarth U, Andresen D, Brachmann J, Kuck KH, Kuniss M, Lewalter T, Spitzer S, Willems S, Senges J, Junger C, Hoffmann E. Cryoballoon versus RF ablation in paroxysmal atrial fibrillation: results from the German Ablation Registry. J Cardiovasc Electrophysiol 2014;25:1-7.
- Schreiber D, Rostock T, Frohlich M, Sultan A, Servatius H, Hoffmann BA, Luker J, Berner I, Schaffer B, Wegscheider K, Lezius S, Willems S, Steven D. Five-year follow-up after catheter ablation of persistent atrial fibrillation using the stepwise approach and prognostic factors for success. Circ Arrhythm Electrophysiol 2015;8:308-317.
- Scott PA, Silberbauer J, Murgatroyd FD. The impact of adjunctive complex fractionated atrial electrogram ablation and linear lesions on outcomes in persistent atrial fibrillation: a meta-analysis. Europace 2016;18:359-367.
- Sepehri Shamloo A, Dagres N, Dinov B, Sommer P, Husser-Bollmann D, Bollmann A, Hindricks G, Arya A. Is epicardial fat tissue associated with atrial fibrillation recurrence after ablation? A systematic review and meta-analysis. Int J Cardiol Heart Vasc 2019;22:132-138.
- Shah AN, Mittal S, Sichrovsky TC, Cotiga D, Arshad A, Maleki K, Pierce WJ, Steinberg JS. Long-term outcome following successful pulmonary vein isolation: pattern and prediction of very late recurrence. J Cardiovasc Electrophysiol 2008;19:661-667.
- Shah D, Haissaguerre M, Jais P, Hocini M. Nonpulmonary vein foci: do they exist?Pacing Clin Electrophysiol 2003;26:1631-1635.
- Shah DC, Sunthorn H, Burri H, Gentil-Baron P. Evaluation of an individualized strategy of cavotricuspid isthmus ablation as an adjunct to atrial fibrillation ablation. J Cardiovasc Electrophysiol 2007;18:926-930.
- Shi LZ, Heng R, Liu SM, Leng FY. Effect of catheter ablation versus antiarrhythmic drugs on atrial fibrillation: a meta-analysis of randomized controlled trials. Exp Ther Med 2015;10:816-822.
- Siontis KC, Ioannidis JPA, Katritsis GD, Noseworthy PA, Packer DL, Hummel JD, Jais P, Krittayaphong R, Mont L, Morillo CA, Nielsen JC, Oral H, Pappone C, Santinelli V, Weerasooriya R, Wilber DJ, Gersh BJ, Josephson ME, Katritsis DG. Radiofrequency ablation versus antiarrhythmic drug therapy for atrial fibrillation: meta-analysis of quality of life, morbidity, and mortality. JACC Clin Electrophysiol 2016;2:170-180.
- Skelly A, Hashimoto R, Al-Khatib S, et al. Catheter Ablation for Treatment of Atrial Fibrillation (Internet). Rockville, MD: Agency for Healthcare Research and Quality (US). Available from https://www.ncbi.nlm.nih.gov/books/NBK305763/ (accessed 20 April 2015).
- Sohara H, Ohe T, Okumura K, Naito S, Hirao K, Shoda M, Kobayashi Y, Yamauchi Y, Yamaguchi Y, Kuwahara T, Hirayama H, YeongHwa C, Kusano K, Kaitani K, Banba K, Fujii S, Kumagai K, Yoshida H, Matsushita M, Satake S, Aonuma K. HotBalloon ablation of the pulmonary veins for paroxysmal AF: a multicenter randomized trial in Japan. J Am Coll Cardiol 2016;68:2747-2757.
- Squara F, Zhao A, Marijon E, Latcu DG, Providencia R, Di Giovanni G, Jauvert G, Jourda F, Chierchia GB, De Asmundis C, Ciconte G, Alonso C, Grimard C, Boveda S, Cauchemez B, Saoudi N, Brugada P, Albenque JP, Thomas O. Comparison between radiofrequency with contact force-sensing and secondgeneration cryoballoon for paroxysmal atrial fibrillation catheter ablation: a multicentre European evaluation. Europace 2015;17:718-724.
- Stabile G, Bertaglia E, Senatore G, De Simone A, Zoppo F, Donnici G, Turco P, Pascotto P, Fazzari M, Vitale DF. Catheter ablation treatment in patients with drug-refractory atrial fibrillation: a prospective, multi-centre, randomized, controlled study (Catheter Ablation For The Cure Of Atrial Fibrillation Study). Eur Heart J 2006;27:216-221.
- Stavrakis S, Nakagawa H, Po SS, Scherlag BJ, Lazzara R, Jackman WM. The role of the autonomic ganglia in atrial fibrillation. JACC Clin Electrophysiol 2015;1:1-13.
- Steinbeck G, Sinner MF, Lutz M, Muller-Nurasyid M, Kaab S, Reinecke H. Incidence of complications related to catheter ablation of atrial fibrillation and atrial flutter: a nationwide in-hospital analysis of administrative data for Germany in 2014. Eur Heart J 2018;39:4020-4029.
- Straube F, Dorwarth U, Ammar-Busch S, Peter T, Noelker G, Massa T, Kuniss M, Ewertsen NC, Chun KR, Tebbenjohanns J, Tilz R, Kuck KH, Ouarrak T, Senges J, Hoffmann E; Freeze Cohort Investigators. First-line catheter ablation of paroxysmal atrial fibrillation: outcome of radiofrequency versus cryoballoon pulmonary vein isolation. Europace 2016;18:368-375.
- Szegedi N, Szeplaki G, Herczeg S, Tahin T, Sallo Z, Nagy VK, Osztheimer I, Ozcan EE, Merkely B, Geller L. Repeat procedure is a new independent predictor of complications of atrial fibrillation ablation. Europace 2019;21:732-737.
- Tamborero D, Mont L, Berruezo A, Matiello M, Benito B, Sitges M, Vidal B, de Caralt TM, Perea RJ, Vatasescu R, Brugada J. Left atrial posterior wall isolation does not improve the outcome of circumferential pulmonary vein ablation for atrial fibrillation: a prospective randomized study. Circ Arrhythm Electrophysiol 2009;2:35-40.
- Tang RB, Dong JZ, Liu XP, Long DY, Yu RH, Kalifa J, Ma CS. Metabolic syndrome and risk of recurrence of atrial fibrillation after catheter ablation. Circ J 2009;73:438-443.
- Teh AW, Kistler PM, Lee G, Medi C, Heck PM, Spence SJ, Sparks PB, Morton JB, Kalman JM. Electroanatomic remodeling of the left atrium in paroxysmal and persistent atrial fibrillation patients without structural heart disease. J Cardiovasc Electrophysiol 2012;23:232-238.
- Trines SA, Stabile G, Arbelo E, Dagres N, Brugada J, Kautzner J, Pokushalov E, Maggioni AP, Laroche C, Anselmino M, Beinart R, Traykov V, Blomstrom-Lundqvist C. Influence of risk factors in the ESC-EHRA EORP atrial fibrillation ablation long-term registry. Pacing Clin Electrophysiol 2019;42:1365-1373.
- Tripathi B, Arora S, Kumar V, Abdelrahman M, Lahewala S, Dave M, Shah M, Tan B, Savani S, Badheka A, Gopalan R, Shantha GPS, Viles-Gonzalez J, Deshmukh A. Temporal trends of in-hospital complications associated with catheter ablation of atrial fibrillation in the United States: an update from Nationwide Inpatient Sample database (20112014). J Cardiovasc Electrophysiol 2018;29:715-724.
- Ucer E, Janeczko Y, Seegers J, Fredersdorf S, Friemel S, Poschenrieder F, Maier LS, Jungbauer CG. A RAndomized Trial to compare the acute reconnection after pulmonary vein ISolation with Laser-BalloON versus radiofrequency Ablation: RATISBONA trial. J Cardiovasc Electrophysiol 2018;29:733-739.
- Ueberham L, Schuler E, Hindricks G, Kuhlen R, Bollmann A. SAFER. Eur Heart J 2018;39:2023-2024.
- Ullah W, McLean A, Tayebjee MH, Gupta D, Ginks MR, Haywood GA, O’Neill M, Lambiase PD, Earley MJ, Schilling RJ, Group UKMT. Randomized trial comparing pulmonary vein isolation using the SmartTouch catheter with or without real-time contact force data. Heart Rhythm 2016;13:1761-1767.
- Verma A, Jiang CY, Betts TR, Chen J, Deisenhofer I, Mantovan R, Macle L, Morillo CA, Haverkamp W, Weerasooriya R, Albenque JP, Nardi S, Menardi E, Novak P, Sanders P; STAR AF II Investigators. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med 2015;372:1812-1822.
- Verma A, Kilicaslan F, Pisano E, Marrouche NF, Fanelli R, Brachmann J, Geunther J, Potenza D, Martin DO, Cummings J, Burkhardt JD, Saliba W, Schweikert RA, Natale A. Response of atrial fibrillation to pulmonary vein antrum isolation is directly related to resumption and delay of pulmonary vein conduction. Circulation 2005;112:627-635.
- Vogler J, Willems S, Sultan A, Schreiber D, Luker J, Servatius H, Schaffer B, Moser J, Hoffmann BA, Steven D. Pulmonary vein isolation versus defragmentation: the CHASE-AF clinical trial. J Am Coll Cardiol 2015;66:2743-2752.
- Voskoboinik A, Sparks PB, Morton JB, Lee G, Joseph SA, Hawson JJ, Kistler PM, Kalman JM. Low rates of major complications for radiofrequency ablation of atrial fibrillation maintained over 14 years: a single centre experience of 2750 consecutive cases. Heart Lung Circ 2018;27:976-983.
- Walfridsson H, Walfridsson U, Nielsen JC, Johannessen A, Raatikainen P, Janzon M, Levin LA, Aronsson M, Hindricks G, Kongstad O, Pehrson S, Englund A, Hartikainen J, Mortensen LS, Hansen PS. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation: results on health-related quality of life and symptom burden. The MANTRA-PAF trial. Europace 2015;17:215-221.
- Wang YL, Liu X, Zhang Y, Jiang WF, Zhou L, Qin M, Zhang DL, Zhang XD, Wu SH, Xu K. Optimal endpoint for catheter ablation of longstanding persistent atrial fibrillation: a randomized clinical trial. Pacing Clin Electrophysiol 2018;41:172-178.
- Wazni O, Marrouche NF, Martin DO, Gillinov AM, Saliba W, Saad E, Klein A, Bhargava M, Bash D, Schweikert R, Erciyes D, Abdul-Karim A, Brachman J, Gunther J, Pisano E, Potenza D, Fanelli R, Natale A. Randomized study comparing combined pulmonary vein-left atrial junction disconnection and cavotricuspid isthmus ablation versus pulmonary vein-left atrial junction disconnection alone in patients presenting with typical atrial flutter and atrial fibrillation. Circulation 2003;108:2479-2483.
- Wazni OM, Marrouche NF, Martin DO, Verma A, Bhargava M, Saliba W, Bash D, Schweikert R, Brachmann J, Gunther J, Gutleben K, Pisano E, Potenza D, Fanelli R, Raviele A, Themistoclakis S, Rossillo A, Bonso A, Natale A. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA 2005;293:2634-2640.
- Weerasooriya R, Khairy P, Litalien J, Macle L, Hocini M, Sacher F, Lellouche N, Knecht S, Wright M, Nault I, Miyazaki S, Scavee C, Clementy J, Haissaguerre M, Jais P. Catheter ablation for atrial fibrillation: are results maintained at 5 years of follow-up?J Am Coll Cardiol 2011;57:160-166.
- Wilber DJ, Pappone C, Neuzil P, De Paola A, Marchlinski F, Natale A, Macle L, Daoud EG, Calkins H, Hall B, Reddy V, Augello G, Reynolds MR, Vinekar C, Liu CY, Berry SM, Berry DA; ThermoCool AF Trial Investigators. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA 2010;303:333-340.
- Winkle RA, Jarman JW, Mead RH, Engel G, Kong MH, Fleming W, Patrawala RA. Predicting atrial fibrillation ablation outcome: the CAAP-AF score. Heart Rhythm 2016;13:2119-2125.
- Winkle RA, Mead RH, Engel G, Kong MH, Fleming W, Salcedo J, Patrawala RA. Impact of obesity on atrial fibrillation ablation: patient characteristics, long-term outcomes, and complications. Heart Rhythm 2017;14:819-827.
- Wojcik M, Berkowitsch A, Greiss H, Zaltsberg S, Pajitnev D, Deubner N, Hamm CW, Pitschner HF, Kuniss M, Neumann T. Repeated catheter ablation of atrial fibrillation: how to predict outcome?Circ J 2013;77:2271-2279.
- Wokhlu A, Hodge DO, Monahan KH, Asirvatham SJ, Friedman PA, Munger TM, Cha YM, Shen WK, Brady PA, Bluhm CM, Haroldson JM, Hammill SC, Packer DL. Long-term outcome of atrial fibrillation ablation: impact and predictors of very late recurrence. J Cardiovasc Electrophysiol 2010;21:1071-1078.
- Wokhlu A, Monahan KH, Hodge DO, Asirvatham SJ, Friedman PA, Munger TM, Bradley DJ, Bluhm CM, Haroldson JM, Packer DL. Long-term quality of life after ablation of atrial fibrillation the impact of recurrence, symptom relief, and placebo effect. J Am Coll Cardiol 2010;55:2308-2316.
- Wong CX, Abed HS, Molaee P, Nelson AJ, Brooks AG, Sharma G, Leong DP, Lau DH, Middeldorp ME, Roberts-Thomson KC, Wittert GA, Abhayaratna WP, Worthley SG, Sanders P. Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J Am Coll Cardiol 2011;57:1745-1751.
- Wong CX, Sullivan T, Sun MT, Mahajan R, Pathak RK, Middeldorp M, Twomey D, Ganesan AN, Rangnekar G, Roberts-Thomson KC, Lau DH, Sanders P. Obesity and the risk of incident, post-operative, and post-ablation atrial fibrillation: a meta-analysis of 626,603 individuals in 51 studies. JACC Clin Electrophysiol 2015;1:139-152.
- Wong KC, Paisey JR, Sopher M, Balasubramaniam R, Jones M, Qureshi N, Hayes CR, Ginks MR, Rajappan K, Bashir Y, Betts TR. No benefit of complex fractionated atrial electrogram ablation in addition to circumferential pulmonary vein ablation and linear ablation: Benefit of Complex Ablation Study. Circ Arrhythm Electrophysiol 2015;8:1316-1324.
- Wynn GJ, Panikker S, Morgan M, Hall M, Waktare J, Markides V, Hussain W, Salukhe T, Modi S, Jarman J, Jones DG, Snowdon R, Todd D, Wong T, Gupta D. Biatrial linear ablation in sustained nonpermanent AF: results of the substrate modification with ablation and antiarrhythmic drugs in nonpermanent atrial fibrillation (SMAN-PAF) trial. Heart Rhythm 2016;13:399-406.
- Yang B, Jiang C, Lin Y, Yang G, Chu H, Cai H, Lu F, Zhan X, Xu J, Wang X, Ching CK, Singh B, Kim YH, Chen M; STABLE-SR Investigators. STABLE-SR (Electrophysiological Substrate Ablation in the Left Atrium During Sinus Rhythm) for the treatment of nonparoxysmal atrial fibrillation: a prospective, multicenter randomized clinical trial. Circ Arrhythm Electrophysiol 2017;10:pii: e005405.
- Yu HT, Shim J, Park J, Kim IS, Kim TH, Uhm JS, Joung B, Lee MH, Kim YH, Pak HN. Pulmonary vein isolation alone versus additional linear ablation in patients with persistent atrial fibrillation converted to paroxysmal type with antiarrhythmic drug therapy: a multicenter, prospective, randomized study. Circ Arrhythm Electrophysiol 2017;10:pii: e004915.
- Zhang Z, Letsas KP, Zhang N, Efremidis M, Xu G, Li G, Liu T. Linear ablation following pulmonary vein isolation in patients with atrial fibrillation: a meta-analysis. Pacing Clin Electrophysiol 2016;39:623-630.
- Zheng YR, Chen ZY, Ye LF, Wang LH. Long-term stroke rates after catheter ablation or antiarrhythmic drug therapy for atrial fibrillation: a meta-analysis of randomized trials. J Geriatr Cardiol 2015;12:507-514.
Verantwoording
Beoordelingsdatum en geldigheid
Publicatiedatum : 17-10-2022
Beoordeeld op geldigheid : 01-09-2022
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2018 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met atriumfibrilleren.
Werkgroep
- Prof. dr. N.M.S. (Natasja) de Groot, cardioloog, werkzaam in het Erasmus Medisch Centrum te Rotterdam, NVVC (voorzitter)
- P.H. (Pepijn) van der Voort, cardioloog, werkzaam in het Catharina Ziekenhuis te Eindhoven, NVVC
- Dr. M.E.W. (Martin) Hemels, cardioloog, werkzaam in het Rijnstate Ziekenhuis te Arnhem en RaboudUMC te Nijmegen, NVVC
- Dr. T.J. (Thomas) van Brakel, thoraxchirurg, werkzaam in het Catharina Ziekenhuis te Eindhoven, NVTNET
- Dr. M. (Michiel) Coppens, internist-vasculair geneeskundige, werkzaam in de Amsterdam Universitair Medische Centra te Amsterdam, NIV
- Dr. S. (Sander) van Doorn, huisarts, werkzaam in het Universitair Medisch Centrum Utrecht te Utrecht, NHG
- Prof. dr. M.K. (Kamran) Ikram, neuroloog, werkzaam in het Erasmus Medisch Centrum te Rotterdam, NVN
- H. (Hans) van Laarhoven, zelfstandig adviseur, werkzaam bij Laerhof Advies, Harteraad
Met ondersteuning van
- Dr. B.H. (Bernardine) Stegeman, senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Werkgroeplid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
De Groot (voorzitter) |
Cardioloog-elektrofysioloog, Erasmus Medisch Centrum, Rotterdam |
Mede-oprichter Stichting Atrial Fibrillation Innovation Platform |
Unrestricted grant voor AF bij Hartfalen, Pathofysiologische onderzoek (valt buiten de afbakening) |
Geen (valt buiten de afbakening) |
|
Brakel |
Cardio-thoracaal chirurg |
Verzorgen van trainingen voor chirurgische behandeling van AF (Trainingscontract met Medtronic; inkomsten voor de afdeling) |
Geen |
Geen |
|
Coppens |
Internist-vasculaire geneeskunde |
* Wetenschappelijke adviesraad Trombosestichting Nederland (onbetaald). |
Betaald adviseurschap of betaalde lezingen/nascholingen voor Bayer, Daiichi Investigator initiated studies met externe financiële ondersteuning en door industrie geïnitieerde studies Bayer, UniQure, Roche CSL Behring and Daiichi Sankyo |
Geen (valt buiten de afbakening, niet over AF-patiënten; onderzoek ging bijvoorbeeld over DOAC bij short bowel patiënten) |
|
Van der Voort |
Cardioloog-electrofysioloog Catharinaziekenhuis Eindhoven |
Bestuurslid van NHRA, onbetaald |
Geen |
Geen |
|
Laarhoven |
Zelfstandig adviseur voor de zorg |
Bestuurslid LAREB, vergoeding conform normering NTVZ Voorzitter Raad van Toezicht stichting Leefh, vergoeding conform NVTZ |
* Lid Patientenadviesraad Pfizer, vacatievergoeding * Adviesraad ‘NOAC’ (eenmalig 2019, vacatievergoeding) |
Geen |
|
Van Doorn |
* Assistant professor, Julius Centrum, UMC Utrecht |
Geen |
* Betrokken als co-PI van het ALL-IN onderzoek, naar de substitutie van AF zorg van de 2e lijn naar de huisarts, inclusief behandeling met anticoagulantia: doe 10.1093/eurheartj/ehaa055 (afgerond) * co-PI betrokken bij het FRAIL-AF onderzoek, een gerandomiseerd onderzoek naar de veiligheid en effectiviteit van DOAC’s bij kwetsbare ouderen: trialregister.nl NTR6721, doi 10.1136/bmjopen-2019-032488 (lopend) * Betrokken bij onderzoek met routine zorg data (CPRD) naar de veiligheid en effectiviteit van DOAC’s, en een systematische review naar DOAC doseringen. |
Geen |
|
Hemels |
* Cardioloog-elektrofysioloog Rijnstate ziekenhuis * Programmaleider NVVC Connect atriumfibrilleren |
* Associate editor van Netherlands Heart Journal, géén vergoeding * Onderwijsactiviteiten voor medisch specialisten, huisartsen, (ziekenhuis)apothekers en arts-assistenten/physician assisants, betreft urenvergoeding
|
* Principal investigator (samen met prof. M.V. Huisman) van het Dutch AF onderzoeks en registratieproject namens de NVVC en in opdracht van VWS/ZonMw. Er gaat een vergoeding naar de vakgroep cardiologie in het Rijnstate i.v.m. mijn werkzaamheden voor dit project, ook gefinancierd door FNT * Local principal investigator van diverse patiëntgebonden studies (hartritmestoornissen gerelateerd) in het Rijnstate ziekenhuis, géén persoonlijke vergoeding hiervoor |
Geen |
|
Ikram |
Hoogleraar Klinische Neuro-epidemiologie en neuroloog, Afdelingen Neurologie & Epidemiologie, Erasmus MC, Rotterdam |
Geen |
Geen |
Geen |
|
Stegeman |
Senior adviseur, Kennisinstituut van de Federatie Medisch Specialisten |
Geen |
Geen |
Geen |
|
Meelezer |
||||
|
Jakulj |
* Internist-nefroloog Amsterdam UMC en Dianet * Lid richtlijnencommissie Nederlandse Federatie voor Nefrologie |
Geen |
Geen |
Geen |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief door een afgevaardigde patiëntenvereniging in de werkgroep. De conceptrichtlijn is tevens voor commentaar voorgelegd aan Harteraad en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Wkkgz & Kwalitatieve raming van mogelijke substantiële financiële gevolgen
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijn is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling zijn richtlijnmodules op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Uit de kwalitatieve raming blijkt dat er waarschijnlijk geen substantiële financiële gevolgen zijn, zie onderstaande tabel.
|
Module |
Uitkomst raming |
Toelichting |
|
Module 1 Definitie en diagnose van atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 2 Atriumfibrilleren, subtype, burden en progressie |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 3 Screenen voor atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 4 Integrale behandeling voor patiënten met atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 5.1 Antitrombotisch beleid ter preventie van herseninfarct |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 5.2 Afsluiting of verwijdering van het linker hartoor |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.1 Frequentiecontrole |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.2 Ritmecontrole |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.2.1 Ritmecontrole met antiaritmische medicatie |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.3 Katheterablatie |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.4 Chirurgie voor atriumfibrilleren en concomitante chirurgie voor atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.5 Hybride katheter-/ chirurgische ablatie procedures |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 6.6 Peri-procedureel management ter preventie van herseninfarct |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 7 Cardiovasculaire risicofactoren en bijkomende ziekten |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.1 Atriumfibrilleren bij hemodynamische instabiliteit |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.2 Acute coronaire syndromen, chronisch coronairlijden, en percutane en chirurgische revascularisaties bij patiënten met atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.3 Acuut herseninfarct of hersnebloeding bij patiënten met atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.4 Bloeding ten tijde van antistolling |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.5 Atriumfibrilleren en valvulaire hartziekte |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.6 Atriumfibrilleren en chronische nierschade |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.7 De oudere en kwetsbare patiënt met atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.8 Atriumfibrilleren en aangeboren hartafwijkingen |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.9 Atriumfibrilleren bij erfelijke hartspierziekten |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.10 Atriumfibrilleren tijdens de zwangerschap |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.11 Atriumfibrilleren in professionele sporters |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 8.12 Postoperatief atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 9 Sekse-gerelateerde verschillen in atriumfibrilleren |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
|
Module 10 Epidemiologie, implicaties en behandeling van subklinisch AF/AHRE |
Geen financiële gevolgen |
Het overgrote deel voldoet aan de norm. |
Implementatie
De werkgroep is vooral inhoudelijk bezig geweest met het aanpassen van de ESC-richtlijn ‘Diagnosis and management of atrial fibrillation’ naar de Nederlandse praktijk. De werkgroep heeft een aantal suggesties gegeven voor het onder de aandacht brengen bij medische professionals van de nieuwe richtlijn. De verdere implementatie van de aanbevelingen uit de richtlijn valt buiten de expertise van de werkgroep.
Voorstel voor te ondernemen acties per partij
Hieronder wordt per partij toegelicht welke acties zij kunnen ondernemen om aandacht te geven aan de richtlijn.
Alle direct betrokken wetenschappelijk verenigingen/beroepsorganisaties
- Bekend maken van de richtlijn onder de leden.
- Publiciteit voor de richtlijn maken door over de richtlijn te publiceren in tijdschriften en te vertellen op congressen.
De lokale vakgroepen/individuele medisch professionals
- Het bespreken van de aanbevelingen in de vakgroepsvergadering en lokale werkgroepen.
- Het bespreken van de richtlijnen in de onderwijsuren van de medisch specialist in opleiding
- Het volgen van bijscholing die bij deze richtlijn ontwikkeld gaat worden.
- Afstemmen en afspraken maken met andere betrokken disciplines om de toepassing van de aanbevelingen in de praktijk te borgen.
Het Kennisinstituut van Medisch Specialisten
Toevoegen van de richtlijn aan de Richtlijnendatabase.
Werkwijze
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor patiënten met atriumfibrilleren. Tevens zijn er knelpunten aangedragen door het Zorginstituut Nederland, Zelfstandige Klinieken Nederland, Nederlandse Vereniging voor Neurologie, Vereniging Innovatieve Geneesmiddelen, Nederlandse Vereniging voor Cardiologie, Federatie voor Nederlandse Trombosediensten, Nederlandse Vereniging voor Hart- en Vaatverpleegkundigen, Nederland Huisartsen Genootschap en Inspectie Gezondheidszorg en Jeugd via Invitational conference. Een verslag hiervan is opgenomen onder aanverwante producten.
Overwegingen (van bewijs naar aanbevelingen)
De Engelse tekst uit de ESC-richtlijn Diagnosis and management of atrial fibrillation uit 2020 (Hindricks, 2020) is overgenomen, tenzij er argumenten voor de Nederlandse praktijk van belang zijn. De tekst is vervolgens aangepast en in het Nederlands opgesteld.
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. GRADE staat voor Grading Recommendations Assessment, Development and Evaluation (zie http://www.gradeworkinggroup.org/). Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Vertalen van aanbevelingen
De European Society of Cardiology gebruikt een standaardformulering voor de aanbevelingen op basis van de klasse en niveau van het bewijs. Deze standaardformulering met vertaling naar het Nederlands staat in de onderstaande tabel weergegeven.
|
Class of recommendations |
Suggested wording to use |
Nl’se vertaling, gehanteerd door onder andere de CVRM-richtlijn |
|
I |
Is recommended/is indicated |
Sterke aanbeveling met een actieve, directieve formulering, zoals behandel, streef naar, et cetera |
|
II |
|
|
|
IIa |
Should be considered |
Zwakke aanbeveling met een actieve, directieve formulering, zoals overweeg |
|
IIb |
May be considerd |
Zwakke aanbeveling met als formulering: kan worden overwogen |
|
III |
Is not recommended |
Sterke aanbeveling met een actieve, directieve formulering, zoals behandel niet, et cetera |
CVRM, CardioVasculair RisicoManagement
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijnmodule werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS) (published online ahead of print, 2020 Aug 29). Eur Heart J. 2020;ehaa612. doi:10.1093/eurheartj/ehaa612
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html.
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
