Preventie
Uitgangsvraag
Welke preventiestrategie is effectief voor acute hamstring-, lies-, quadriceps- en kuitblessures?
Aanbeveling
Bied een preventiestrategie aan bij sporters met een risico op acute hamstring-, lies-, quadriceps- en kuitblessures.
Bespreek de verwachtingen, tijdsinvesteringen en motivatie met de sporter bij het aanbieden van een preventiestrategie.
Overweeg bij het aanbieden van een preventiestrategie:
- Een graduele opbouw van belasting;
- Een warming-up waarin verschillende loop-vormen, (excentrische) krachtoefeningen, plyometrie, balans- en propriocepsistraining centraal staan;
- Voldoende hersteltijd tussen sportbelastingen (trainingen/wedstrijden);
- Spier-specifieke krachtoefeningen.
Wees terughoudend met passieve strategiëen ter preventie van spierblessures (e.g. massages, voedingssupplementen).
Overwegingen
Voor- en nadelen van de interventie en de kwaliteit van het bewijs
Er is literatuuronderzoek verricht naar preventiestrategieën bij sporters met een acute hamstring-, lies-, quadriceps- of kuitblessure. In totaal zijn er twaalf RCTs gevonden die preventiestrategieën vergeleken met standaard beleid of geen preventiestrategie. De RCTs hadden verschillende populaties, zoals patiënten met hamstring- (n=8), lies- (n=5), quadriceps- (n=1), kuitblessure (n=0) of cumulatieve (alle soorten) blessures (n=3).
In deze studies is sprake van een risico op bias, brede betrouwbaarheidsintervallen en er waren verschillen tussen de studie-interventies en controlegroepen op basis van de vooraf opgestelde PICO. De bewijskracht voor de cruciale uitkomstmaat incidentie van blessures was laag tot zeer laag, wat resulteert in een overall zeer lage bewijskracht. Het effect van preventiestrategieën blijft onzeker. Kortom, andere studies kunnen leiden tot nieuwe inzichten. Vooralsnog kunnen er op basis van de literatuur geen harde conclusies worden geformuleerd.
Ondanks het risico op bias acht de werkgroep het waardevol om (in het kader van de transitie van evidentie naar aanbevelingen) de beschikbare evidentie van de gerandomiseerde studies gericht op preventiestrategie nader te beschouwen. De studies met incidentie van acute hamstring-, lies- of quadricepsblessure als primaire uitkomstmaat onderzochten de effecten van de Copenhagen Adductie oefening, warm-up programma’s, FIFA11+, en de Nordic hamstring exercise. Wat betreft preventiestrategieën is het meeste bekend over hamstringblessures, met name door onderzoek bij voetballers. Er zijn geen studies gericht op preventiestrategieën van acute kuitblessures beschikbaar.
In alle beschikbare preventieve studies gebruikt men in alle protocollen een graduele opbouw om het lichaam gedoseerd aan de belasting bloot te stellen (Silvers, 2015; Soligard, 2008; Ali, 2022; Arnason, 2008; Petersen, 2011). Een uitgebreide warming up bestaande uit oefeningen gericht op kracht, plyometrie, neuromusculaire controle en balans verlaagt het risico op blessures van de onderste extremiteiten bij vrouwelijke voetballers (Soligard, 2008).
De FIFA heeft het FIFA 11(+) programma ontwikkeld (Silvers, 2015). Dit is een voetbalspecifieke warming up voor de onderste extremiteiten voor voetballers >14 jaar, bestaande uit:
- Sprintoefeningen inclusief snel wenden, draaien en keren;
- (Excentrische) krachtoefeningen, plyometrie en balans-/propriocepsistraining; en
- Afsluitende sprintoefeningen.
Dit is geschikt voor iedere voetballer op elk niveau en kost ca. 20 min zonder extra benodigdheden.
Acute hamstringblessure
De meeste studies zijn gedaan naar preventiestrategieën van acute hamstringblessures, veelal bij voetballers. Acute hamstringblessures ontstaan vaak, maar niet uitsluitend, op maximale snelheid (Nielsen & Yde, 1989; Arnason, 1996; Woods, 2004).
Spierzwakte, dysbalans tussen linker en rechter been en onvoldoende warming up (Arnason, 2008) zijn predisponerende factoren voor het ontstaan van een acute hamstringblessure. Met spierzwakte doelt de werkgroep op onvoldoende belastbaarheid in de excentrische fase (i.e. isometrische fase in verlengde positie).
Verschillende studies hebben aangetoond dat excentrische training effectief kan zijn om een acute hamstringblessure te voorkomen (Gabbe, 2006; Petersen, 2011; van der Horst, 2015). Een voorbeeld van een effectieve excentrische training is de Nordic Hamstring oefening (Raya-Gonzales, 2021). Raya-Gonzales (2021) stelt ook dat excentrisch trainen en propriocepsistraining de kans op een acute hamstringblessure nog meer verlaagt, in vergelijking met alleen excentrisch trainen. Hierbij worden de onderste extremiteiten en lumbale wervelkolom-/bekkenaansturing onder vermoeidheid getraind.
Van de Hoef (2019) heeft een preventief plyometrisch oefenprogramma onderzocht. Er was geen bewijs dat een plyometrische opbouw van concentrisch naar excentrisch naar plyometrie leidt tot minder hamstringblessures bij amateurvoetballers.
Samenvattend acht de werkgroep op basis van beschikbare literatuur en praktijk ervaring de excentrische oefentherapie (zoals bijvoorbeeld de Nordic Hamstring oefening) het meest effectief in het voorkomen van acute hamstringblessures. Echter, gezien het feit dat de beschikbare studies veelal zijn uitgevoerd bij jonge voetballers, is meer onderzoek nodig in verschillende populaties of die oefenvormen ook daar effectief zijn.
Acute liesblessure
Naast de acute hamstringblessure komt ook de (acute) liesblessure relatief frequent voor. De adductor longus is de meest aangedane spier in de liesregio. Fujisaki (2022) onderzocht de 'Copenhagen Adductor oefening' welke effectief bleek te zijn in het voorkomen van liesblessures bij voetabllers. Auteurs onderzochten ook de 'Copenhagen Adductor oefening' in combinatie met de Nordic Hamstring oefening, wat de kans op het ontstaan van een liesblessure nog meer verlaagde (Fujisaki, 2022)
De Copenhagen Adductor oefening wordt opgedeeld in drie verschillende moeilijkheidsgradaties afhankelijk van de mate van zwakte en uitvoering van de oefening (Harøy 2019). Dit kan een onderdeel zijn van een normale (dagelijkse) training:
- Heup adductie in zijlig,
- Copenhagen Adductor oefening met korte hefboom, of
- Copenhagen Adductor oefening met lange hefboom.
Acute quadriceps- en kuitblessure
Er zijn geen studies bekend over preventiestrategien van acute quadriceps- of kuitblessures. De werkgroep refereert in relatie tot deze blessures naar het FIFA 11+ programma. Dit programma omvat een specieke warming-up voor de preventie van blessures aan de onderste extremiteiten. De werkgroep verwacht dat het FIFA 11+ programma daarom ook waardevol is bij preventie van acute quadriceps- of kuitblessures bij sporters.
Preventiestrategie passieve interventies
Er zijn geen studies bekend over de preventieve werking van passieve interventies (zoals bijvoorbeeld massage, taping, bandages, schoeiselaanpassingen, voedingssupplementen). De werkgroep adviseert daarom zeer terughoudend te zijn met het toepassen van passieve preventiestrategieën.
Waarden en voorkeuren van patiënten (en evt. hun verzorgers)
De voor- en nadelen van de mogelijke preventiestrategieën dienen besproken te worden met de patiënt. Verwachtingsmanagement is hierbij van groot belang. Uit ervaring van de werkgroep blijkt dat het gezamenlijke besluitvormingsproces met daarbij behorende eigen input van patiënten als prettig wordt ervaren door patiënten. Hierbij is het belangrijk dat er voldoende persoonlijke aandacht is, dat de patiënt zich gehoord voelt en dat daar voldoende tijd voor is. Een vaste behandelaar of aanspreekpunt maakt dit gemakkelijker. De geschiedenis van een patiënt kan invloed hebben op de verwachting van een aankomend herstel/preventieproces. Een sporter die al een acute spierblessure heeft gehad zal gemotiveerder zijn om een preventiestrategie uit te voeren dan een patient die nog geen acute spierblessure heeft gehad. Door dit te overwegen en te bespreken met de patiënt zal hij/zij zich meer gehoord voelen en zijn/haar verwachting eventueel kunnen bijstellen.
Met adequate informatie kan de patiënt een weloverwogen keuze maken of een preventiestrategie past in zijn/haar situatie.
Kosten (middelenbeslag)
Er zijn bij de werkgroep geen kosten-effectiviteitsstudies bekend over preventiestrategieën bij acute hamstring-, lies-, quadriceps- en kuitblessures. De werkgroep voorziet dat de beschreven preventiestrategieën niet met extra kosten gepaard gaan. De kosten blijven eventueel beperkt tot de consultkosten van zorgverleners.
Aanvaardbaarheid, haalbaarheid en implementatie
Er is in deze richtlijn geen literatuuronderzoek gedaan naar de aanvaardbaarheid en haalbaarheid van de preventiestrategieën. Op basis van de beschikbare literatuur is de werkgroep van mening dat zowel de Nordic Hamstring oefening als de Copenhagen Adductor oefening in het trainingsschema kan worden toegepast. Deze oefeneningen kunnen overal door de sporter worden uitgevoerd. Het FIFA 11+ programma kan ook goed zelfstandig worden uitgevoerd. Toch is de ervaring vanuit de praktijk dat de implementatie erg lastig is. Persoonlijke motivatie van elke betrokken persoon van een team rondom de sporter is hierin cruciaal (van der Horst, 2018).
Persoonlijke motivatie van een sporter is van groot belang. Een sporter die al een acute spierblessure heeft gehad zal mogelijk gemotiveerder zijn om een preventiestrategie uit te voeren dan een sporter die nog geen acute spierblessure heeft gehad.
Rationale van de aanbeveling: weging van argumenten voor en tegen de interventies
Er is beperkt bewijs beschikbaar naar de toepassing van preventistrategiën bij acute spierblessures. De studies die beschikbaar zijn richten zich met name op acute hamstringblessure (in voetballers), waarbij het belang van een graduele opbouw om belasting te doseren wordt benadrukt. Dit wordt ondersteunt door de mening van de werkgroep. Er is geen literatuur beschikbaar over de effectiviteit van passieve interventies. Voor de patiënt zelf blijkt een persoonlijke benadering van belang bij de besluitvorming, waarin aandacht is voor het bespreken van de voor- en nadelen van de verschillende preventiestrategiën.
Onderbouwing
Achtergrond
Acute hamstring- lies, quadriceps- en kuitblessures komen bij sporters vaak voor. Aan deze blessures zit een bepaalde revalidatieduur vast en een risico op recidief met als gevolg uitval van sport. Dit kan gevolgen hebben voor (top)sporters, zoals bijvoorbeeld pijn, immobiliteit, mentale en financiële gevolgen. Hoewel het waarschijnlijk is dat (top)sporters baat hebben bij preventiestrategieën en er wel degelijk kennis over de effectiviteit van bepaalde preventiestrategieën bekend is bij de werkgroep, ontbreekt in de praktijk een uniforme aanpak en is onduidelijk welke preventiestrategieën zinvol zijn om acute hamstring-, lies-, quadriceps- en kuitblessures te voorkomen. De meeste preventie-studies onderzoeken de preventie van acute hamstring- en liesblessures bij zowel niet eerder geblesseerde sporters als sporters met recidiverende klachten. Deze module evalueert welke preventiestrategieën zinvol zijn bij hamstring-, lies-, quadriceps- en kuitblessures.
Conclusies / Summary of Findings
1. Cumulative (all types of) injuries
|
Low GRADE |
1a. Injury incidence (crucial) Injury prevention strategies may reduce (all type of) injury incidence in (amateur) athletes.
Source: Engebretsen (2008), Silvers (2015), Soligard (2009) |
|
Very low GRADE |
1b. Time loss (important) The evidence is very uncertain about the effect of injury prevention strategies on time absent from sports.
Source: Silvers (2015) |
2. Groin injuries
|
Low GRADE |
2a. Injury incidence (crucial) Injury prevention strategies (Copenhagen Adduction exercise, warm-up programs, FIFA11+, various) may reduce groin injury incidence in (amateur) athletes.
Source: Engebretsen (2008), Fujisaki (2022), Harøy (2019), Hölmich (2010), Silvers (2015) |
|
Very low GRADE |
2b. Time loss (important) The evidence is very uncertain about the effect of injury prevention strategies on time absent from sports due to groin injuries.
Source: Fujisaki (2022) |
3. Hamstring injuries
|
Low GRADE |
3a. Injury incidence (crucial) Injury prevention strategies (Nordic Hamstring Exercise, bounding or warm-up program, FIFA11+, various) may reduce hamstring injury incidence in (amateur) athletes.
Source: Ali (2022), Engebretsen (2008), Gabbe (2006), Petersen (2011), Raya-Gonzalez (2021), Silvers (2015), van de Hoef (2019), van der Horst (2015) |
|
Low GRADE |
3b. Time loss (important) Injury prevention strategies may increase time absent from sports due to hamstring injuries in (amateur) athletes.
Source: Petersen (2011), van de Hoef (2019), van der Horst (2015) |
4. Quadriceps injuries
|
Very low GRADE |
4a. Injury incidence (crucial) The evidence is very uncertain about the effect of injury prevention strategies on quadriceps injury incidence in (amateur) athletes.
Source: Silvers (2015) |
|
- GRADE |
4b. Time loss (important) The outcome time loss for quadriceps injuries was not reported and could not be graded. |
Samenvatting literatuur
Description of studies
As the PICO included several types of injuries, the included articles are analyzed for injury type:
- Cumulative (all types of) injuries
- Groin injuries
- Hamstring injuries
- Quadriceps injuries
No articles were found assessing calf injuries.
1. Cumulative (all types of) injuries
Three articles reported on multiple types of injury: Engebretsen (2008) on cumulative ankle, knee, groin and hamstring strains, Silvers (2015) on all types of injury, and Soligard (2009) on injuries to the lower extremity. Characteristics of the studies can be found in Table 1. Risk of bias assessments for the separate studies can be found under the heading Evidence Tables.
2. Groin injuries
Five articles were found reporting on groin injuries: three on groin injuries specifically, and two as part of a subanalysis. An overview of the articles’ characteristics can be found in Table 2.
3. Hamstring injuries
Eight articles were found reporting on hamstring injuries: six focusing on hamstring injuries specifically, and two as part of a subanalysis. An overview of the articles’ characteristics can be found in Table 3.
4. Quadriceps injuries
Only the article by Silvers (2015) performed a subanalysis for quadriceps injury, reported as injury incidence per 1000 exposure hours. The characteristics of the study by Silvers (2015) can be found in Table 1.
Table 1. Articles reporting on preventive programs for multiple injuries.
|
Study |
Population (size) |
Intervention and duration (n) |
Controls (n) |
Outcomes (including FU) |
Used definition of injury |
|
Engebretsen, 2008 |
Male soccer players in teams from the 1st, 2nd and top of 3rd division in the proximity of Oslo (508, 31 teams) |
Specific training program for the body part(s) assumed to be at high risk for injury, 3 times per week in the pre-season (10 weeks), and once per week during the competitive season (193) |
Regular team training (315), subdivided in high-risk of injury and low-risk group |
Injury incidence per 1000 hours exposure (1 season) |
any physical complaint to the ankle, knee, groin and hamstring sustained by a player that resulted from a soccer match or training, resulting in inability to play (time-loss injury) |
|
Silvers, 2015 |
Male student athletes participating in an NCAA Division I or II (1525, 65 teams) |
FIFA11+ injury prevention program, instructed to perform 3 times per week during 1 collegiate soccer season (775) |
No use of FIFA11+ injury prevention program (850) |
Injury incidence per 1000 athlete exposure (4 months) |
any physical complaint sustained by a player that resulted from a football match or training, irrespective of the need for medical attention or time loss from football |
|
Soligard, 2009 |
Female clubs from the 15-16 year divisions in the Norwegian Football Association that had at least 2 training sessions (2540, 125 clubs) |
Comprehensive warm-up program (approx. 20 minutes) for every training session throughout the season, consisting of slow running, exercises (strength, balance, jumping) and speed running (1320) |
Warm-up as usual (1220) |
Lower extremity injury incidence per 1000 playing hours (8 months) |
An injury to the foot, ankle, lower leg, knee, thigh, groin or hip during a scheduled match or training session, causing the player to be unable to fully take part in the next match or training session |
Table 2. Articles reporting on preventive programs for groin injuries: specifically groin (above marked line) or as part of subanalysis (below marked line).
|
Study |
Population (size) |
Intervention and duration (n) |
Controls (n) |
Outcomes (including FU) |
Used definition of injury |
|
Fujisaki, 2022 |
Male soccer players in the u18 soccer league (202, 7 schools) |
CAE 1 set for 1-3 times per week for 16 weeks (66)
CAE as above plus NHE 2-3 sets (73) |
Usual training (63) |
Injury incidence per 1000 competition hours (16 weeks) |
pain in the groin during sports activities, regardless of time loss or need for treatment |
|
Injury severity |
mean days lost to sports |
||||
|
Harøy, 2019 |
Semiprofessional Norwegian male football players (652, 35 teams) |
Adduction strengthening program (based on CAE) as part of warm-up, 3 times per week in the pre-season (6-8 weeks) and once per week during competitive season (28 weeks) (339) |
Training as normal (313) |
Weekly prevalence of groin pain (38 weeks) |
Groin problems registered using the OSTRC Overuse Injury Questionnaire |
|
Hölmich, 2010 |
Amateur football players training and playing at a competitive level (1211, 55 clubs) |
Exercise program with 6 exercises as part of warm-up (strengthening, coordination, core stability) performed 2-4 times per week (524) |
Training as usual (453) |
Time until first groin injury (42 weeks) |
any physical complaint that is the result of participating in football training or match incapacitating the player when playing football and/ or demanding special medical attention to be able to participate. |
|
Engebretsen |
Subanalysis for groin injuries (for characteristics see table 1) |
||||
|
Silvers, 2015 |
Subanalysis for groin injuries (for characteristics see table 1) |
||||
Abbreviations: CAE: Copenhagen Adduction Exercise, FU: follow-up, n: number, NHE: Nordic Hamstring Exercise, u18: under 18
Table 3. Articles reporting on preventive programs for hamstring injuries: specifically hamstring (above marked line) or as part of subanalysis (below marked line).
|
Study |
Population (size) |
Intervention and duration (n) |
Controls (n) |
Outcomes (including FU) |
Used definition of injury |
|
Gabbe, 2006 |
Adult, male football players in either senior or reserve grade teams during the 2004 season. (220, 7 clubs) |
Eccentric exercise (similar to NHE, 12x 6 repetitions) before cool-down, 5 sessions over a 12-week period (3 during pre-season and 2 during first 6 weeks of season) (114) |
Stretching and range of movement exercises (3x 30 seconds) before cool-down, 5 sessions over a 12-week period (same as intervention) (106) |
Injury incidence (1 season) |
defined by physical assessment including: sudden onset posterior thigh pain; tenderness on palpation; with or without pain on stretch of the hamstring muscles; and with or without pain on contraction of the hamstring muscles. |
|
Petersen, 2011 |
Male soccer players in the top 5 Danish soccer divisions. (942, 50 teams) |
10-weeks NHE (27 sessions) during the midseason break, followed by a weekly seasonal program (3 sets of 12-10-8 repetitions) (461) |
Usual training program (481) |
Occurrence of acute hamstring injury adjusted for player seasons at risk (12 months)s |
any acute-occurring physical complaint in the region of the posterior thigh sustained during a soccer match or training, irrespective of the need for medical attention or time loss from soccer activities |
|
Injury severity (12 months) |
Mean days of absence from soccer |
||||
|
Raya-Gonzalez, 2021 |
Male soccer players <19 years of age (61) |
Additional NHE and sprint training program once a week (15-20 minutes, for 14 weeks) (27) |
Regular weekly training program (34) |
Injury incidence per 1000 hours of exposure (14 weeks) |
an injury that occurred during a scheduled training session or match that caused absence from the next training session or match |
|
Van de Hoef, 2019 |
Adult male soccer players in the first-class amateur league aged 18-45 years (588, 32 teams) |
Bounding Exercise Program: in addition to regular soccer training 12-week program with build-up from concentric to eccentric to plyometric exercises (approx. 3-5 minutes) (305) |
Usual soccer training (283) |
Hamstring injury incidence per 1000 soccer hours (39 weeks) |
No definition of injury provided. Overuse injuries included. |
|
Injury severity (39 weeks) |
Mean days absent from soccer play |
||||
|
Van der Horst, 2015 |
Male soccer players in first-class amateur league (Eerste Klasse) aged 18 to 40 years (579, 40 teams) |
Supervised sessions (total of 25) of NHE in 13 weeks, before cooling down (292) |
Play soccer as usual (287) |
Number of players sustaining a hamstring injury (1 year) |
Any physical complaint affecting the posterior side of the upper leg irrespective of the need for medical attention or time loss from soccer activities |
|
Injury severity (1 year) |
Mean days absent from soccer play |
||||
|
Ali, 2022 |
Sprinters studying at Punjab university, aged 20 to 30 years. |
Warm-up exercises before sprinting events (3x/week for 3 months) (no protocol provided). (20) |
No warm-up exercise before training (20) |
Prevalence of hamstring injury (3 months) |
Pain, spasm or stiffness of hamstring muscle |
|
Engebretsen, 2008 |
Subanalysis for hamstring injuries (for characteristics see table 1) |
||||
|
Silvers, 2015 |
Subanalysis for hamstring injuries (for characteristics see table 1) |
||||
Results
None of the included articles reported on the outcome adaptation of sport activities.
1. Cumulative (all types of) injuries
The three articles from table 1 reported on multiple types of injury in soccer/football players (two studies with male, one with female participants); however, the used definitions for injury vary. Whereas Engebretsen (2008) classifies an injury as a complaint causing inability to play and Soligard (2009) as it preventing to fully take part, defines Silvers (2015) an injury as any complaint, irrespective of the need for medical attention or time loss from football.
1a. Injury incidence
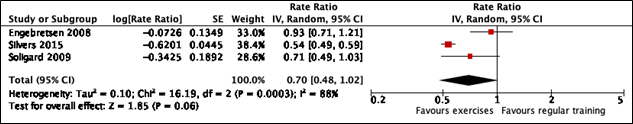
Three authors (Engebretsen 2008, Silvers 2015, and Soligard 2009) reported injury incidence per 1000 hours of exposure. The pooled incidence rate ratio (IRR) is 0.70 (95% CI 0.48 to 1.02) and is presented in figure 1. This finding is not statistically significant, but clinically relevant.
Figure 1. Forest plot of pooled incidence rate ratio of all types of injuries after preventive exercises compared to training as usual.
Engebretsen (2008) and Soligard (2009) additionally performed a subanalysis for acute injuries only (not including overuse injuries). Engebretsen (2008) found a risk ratio of 0.94 (95% CI 0.84 to 1.06), slightly favouring the intervention group (41% acute injuries) compared to the high-risk control group (43% acute injuries). Soligard (2009) found an IRR of 0.74 (95% CI 0.51 to 1.08) for acute injuries after a specific warm-up compared to regular warm-up. Both ratios are not statistically significant, but clinically relevant.
1b. Time loss
Only Silvers (2015) reported mean days lost to injury. A mean difference between the group receiving the FIFA11+ program and the group not receiving the program was -3.12 days (95% CI -5.19 to -1.05), meaning that the intervention group was less days absent from soccer play.
2. Groin injuries
All five included articles reporting groin injuries included male adolescent or adult football/soccer players.
2a. Injury incidence
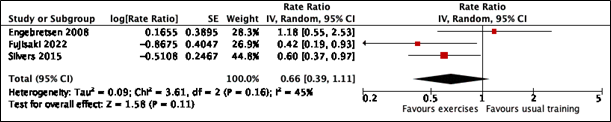
Three authors (Fujisaki 2022, Engebretsen 2008, and Silvers 2015) reported injury incidence per 1000 hours of exposure or competition hours, collected in follow-up times differing from 16 to 42 weeks. The pooled incidence rate ratio was 0.66 (95% CI 0.39 to 1.11) and is depicted in figure 2. The interventions used in the three studies are quite different, therefore the pooled result should be interpreted with caution.
Figure 2. Forest plot of pooled incidence rate ratio of groin injuries after preventive exercises compared to training as usual.
Two other authors reported injury occurrence differently: Harøy (2019) reported a weekly prevalence of groin injuries over a 38-week period through and odds ratio (OR 0.59, 95% CI 0.40 to 0.86). Hölmich (2010) took the factor time into account and reported through a hazard ratio (HR 0.80, 95% CI 0.46 to 1.40).
2b. Time loss
Fujisaki (2022) also reported on injury severity, defined as mean days lost from sport. In the group receiving Copenhagen Adduction Exercise (CAE), this number was 5.5 (SD 5.2), in the group receiving CAE plus Nordic Hamstring Exercise (NHE) it was 10.3 (SD 6.4) and in the control group it was 14.4 (SD 8.3). The mean differences were therefore -8.9 days (95% CI -12.0 to -5.8) and -4.1 days (95% CI -7.4 to -0.8) for CAE to control and CAE+NHE to control, respectively.
3. Hamstring injuries
All included articles reporting hamstring injuries included male adolescent or adult football/soccer players, except for Ali (2022) who included sprinters of both genders.
3a. Injury incidence
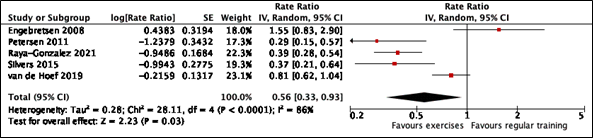
Five authors reported hamstring injuries through incidence rates adjusted for exposure. The pooled IRR can be found in figure 3. The RR was 0.56 (95%CI 0.33 to 0.93), which is considered statistically significant and clinically relevant.
Figure 3. Forest plot of pooled incidence rate ratio of hamstring injuries after preventive exercises compared to training as usual.
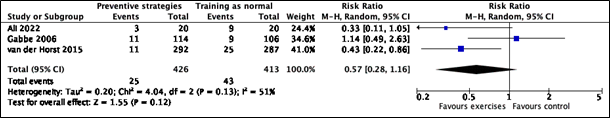
Three authors (Gabbe 2006, van der Horst 2015, and Ali 2022) reported injury occurrence through relative risks (not adjusted for player exposure), with varying follow-up times from 3 months to 1 year. The pooled risk ratio is depicted in figure 4. The pooled RR was 0.57 (95%CI 0.28 to 1.16), shows a clinically relevant effect, yet no statistical significance is reached, and a broad confidence interval implies different inferences.
Figure 4. Forest plot of pooled risk ratio of hamstring injuries after preventive exercises compared to control groups (usual training or stretching and range of movement exercises).
3b. Time loss
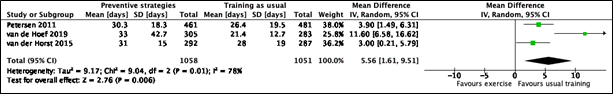
Three authors (Petersen 2011, van de Hoef 2019 and van der Horst 2015) reported injury severity as mean days absent from soccer play. The pooled mean difference can be found in figure 5: MD 5.56 days (95% CI 1.61 to 9.51). Despite being statistically significant, this difference is not clinically relevant.
Figure 5. Forest plot of pooled mean difference of days absent from soccer play after preventive exercises compared to training as usual.
4. Quadriceps injuries
4a. Injury incidence
The study by Silvers (2015) performed a subanalysis for quadriceps injury in male student athletes receiving the FIFA11+ injury prevention program. The found IRR compared to not receiving the program after 4 months was 0.72 (95% CI 0.44 to 1.16), a finding not statistically significant but clinically relevant.
Level of evidence of the literature
The level of evidence for all outcome measures started at high, as all were based on RCTs.
1. Cumulative (all types of) injuries
Downgrading for cumulative (all types of) injuries took place:
|
For 1a. Injury incidence by 2 levels because of:
|
For 1b. Time loss by 3 levels because of:
|
2. Groin injuries
Downgrading for groin injuries took place:
|
For 2a. Injury incidence by 2 levels because of:
|
For 2b. Time loss by 3 levels because of:
|
3. Hamstring injuries
Downgrading for hamstring injuries took place:
|
For 3a. Injury incidence by 2 levels because of:
|
For 3b. Time loss by 2 levels because of:
|
4. Quadriceps injuries
Downgrading for quadriceps injuries took place:
|
For 4a. Injury incidence by 3 levels because of:
|
For 4b. Time loss no results were reported, and therefore no grade assessment can be made. |
Zoeken en selecteren
A systematic review of the literature was performed to answer the following question:
What is the effectiveness of strategies to prevent acute hamstring, groin, quadriceps, and calf injuries in athletes without complaints?
P: Athletes without prevalent injuries or complaints
I: Strategies to prevent injuries (e.g. exercise programs, stretching and strengthening exercises, balance training)
C: Usual training or no use of a preventative strategy for injuries
O: Incidence of acute hamstring, groin, quadriceps, or calf injuries; time loss; adaption of sport activities
Relevant outcome measures
The guideline development group considered injury incidence as a critical outcome measure for decision making; and time loss and adaptation of sport activities as an important outcome measure for decision making.
Per outcome, the working group defined the following differences as a minimally clinically (patient) important difference:
- Adaptation of sport activities: RR>15%
- Injury incidence: RR>20%
- Time loss: 7 days or RR>5%
The working group defined the outcome measures as follows:
- Injury incidence: the occurrence of injuries per 1000 hours played (exposure hours) in training or matches;
- Time loss: mean days absent from play due to sustained injury;
- Adaptation of sport activities: the need to lower intensity or reduce training activities due to sustained injury.
Search and select (Methods)
The databases Medline (via OVID) and Embase (via Embase.com) were searched with relevant search terms from 2000 until September 20th, 2022. The detailed search strategy is available upon request. The systematic literature search resulted in 514 hits. Studies were selected based on the following criteria:
- A randomized controlled trial (RCT) as study design;
- Included adolescent or adult athletes (³14 years of age) without injuries;
- Described any injury prevention program as intervention;
- Described training as usual or no injury prevention program as comparison;
- Described injury incidence of groin, hamstring, quadriceps or calf as outcome;
- Reported results in English;
- Included ³ 20 participants (³10 per arm)
A total of 40 studies was initially selected based on title and abstract screening. After reading the full text, 28 studies were excluded (see the table with reasons for exclusion under the heading Evidence Tables), and 12 studies were included.
Results
Twelve RCTs were included in the analysis of the literature. Important study characteristics and results are summarized in the evidence tables. The assessment of the risk of bias is summarized in the risk of bias tables.
Referenties
- Ali S, Rafiq MT, ul-Hassan T, Sharif A. Role of warm-up exercise in preventing hamstring injury in sprinters. Rawal Medical Journal. 2022; 47(1): 238-240.
- Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008 Jun;36(6):1052-60. doi: 10.1177/0363546508314432. Epub 2008 Apr 3. PMID: 18390492.
- Fujisaki K, Akasaka K, Otsudo T, Hattori H, Hasebe Y, Hall T. Effects of a Groin Pain Prevention Program in Male High School Soccer Players: A Cluster-Randomized Controlled Trial. Int J Sports Phys Ther. 2022 Aug 1;17(5):841-850. doi: 10.26603/001c.36631. PMID: 35949380; PMCID: PMC9340824.
- Gabbe BJ, Branson R, Bennell KL. A pilot randomised controlled trial of eccentric exercise to prevent hamstring injuries in community-level Australian Football. J Sci Med Sport. 2006 May;9(1-2):103-9. doi: 10.1016/j.jsams.2006.02.001. Epub 2006 Mar 30. PMID: 16574482.
- Harøy J, Clarsen B, Wiger EG, Øyen MG, Serner A, Thorborg K, Hölmich P, Andersen TE, Bahr R. The Adductor Strengthening Programme prevents groin problems among male football players: a cluster-randomised controlled trial. Br J Sports Med. 2019 Feb;53(3):150-157. doi: 10.1136/bjsports-2017-098937. Epub 2018 Jun 10. PMID: 29891614.
- Hölmich P, Larsen K, Krogsgaard K, Gluud C. Exercise program for prevention of groin pain in football players: a cluster-randomized trial. Scand J Med Sci Sports. 2010 Dec;20(6):814-21. doi: 10.1111/j.1600-0838.2009.00998.x. PMID: 19883386.
- Petersen J, Thorborg K, Nielsen MB, Budtz-Jørgensen E, Hölmich P. Preventive effect of eccentric training on acute hamstring injuries in men's soccer: a cluster-randomized controlled trial. Am J Sports Med. 2011 Nov;39(11):2296-303. doi: 10.1177/0363546511419277. Epub 2011 Aug 8. PMID: 21825112.
- Raya-González J, Torres Martin L, Beato M, Rodríguez-Fernández A, Sanchez-Sanchez J. The effects of training based on Nordic hamstring and sprint exercises on measures of physical fitness and hamstring injury prevention in U19 male soccer players. Res Sports Med. 2021 Nov 27:1-16. doi: 10.1080/15438627.2021.2010206. Epub ahead of print. PMID: 34841995.
- Silvers-Granelli H, Mandelbaum B, Adeniji O, Insler S, Bizzini M, Pohlig R, Junge A, Snyder-Mackler L, Dvorak J. Efficacy of the FIFA 11+ Injury Prevention Program in the Collegiate Male Soccer Player. Am J Sports Med. 2015 Nov;43(11):2628-37. doi: 10.1177/0363546515602009. Epub 2015 Sep 16. PMID: 26378030; PMCID: PMC4839291.
- Soligard T, Myklebust G, Steffen K, Holme I, Silvers H, Bizzini M et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial BMJ 2008; 337 :a2469 doi:10.1136/bmj.a2469
- van de Hoef PA, Brink MS, Huisstede BMA, van Smeden M, de Vries N, Goedhart EA, Gouttebarge V, Backx FJG. Does a bounding exercise program prevent hamstring injuries in adult male soccer players? - A cluster-RCT. Scand J Med Sci Sports. 2019 Apr;29(4):515-523. doi: 10.1111/sms.13353. Epub 2019 Jan 24. PMID: 30536639; PMCID: PMC6850185.
- van der Horst N, Smits DW, Petersen J, Goedhart EA, Backx FJ. The preventive effect of the nordic hamstring exercise on hamstring injuries in amateur soccer players: a randomized controlled trial. Am J Sports Med. 2015 Jun;43(6):1316-23. doi: 10.1177/0363546515574057. Epub 2015 Mar 20. PMID: 25794868.
Evidence tabellen
Evidence table for intervention studies (randomized controlled trials and non-randomized observational studies [cohort studies, case-control studies, case series])
|
Study reference |
Study characteristics |
Patient characteristics |
Intervention (I) |
Comparison / control (C) |
Follow-up |
Outcome measures and effect size |
Comments |
|
Engebretsen, 2008 |
Type of study: RCT
Setting and country: Soccer teams, Norway
Funding and conflicts of interest: Several non-commercial and one commercial grant (not specified whether restricted). Conflict of interest not disclosed. |
Inclusion criteria: Soccer players in teams playing in the Norwegian 1st, 2nd or top of 3rd division in the proximity of Oslo.
Exclusion criteria: (1) declined invitation, (2) no show for baseline testing, (3) inability to speak Norwegian, (4) “other reasons”
N total at baseline: 508 (31 teams) Intervention: 193 Control – HR: 195 Control – LR: 120
Important prognostic factors: Not reported.
Groups comparable at baseline? Cannot be judged. Stratification within teams for high-risk players. |
Patients with high risk of injury (in case of acute injury to ankle, knee, hamstring or groin in the previous 12 months, or a reduced function (average score <80%) on body part-specific function questionnaires. Received a training program (including a folder) for the body parts to which they were assumed to have an increased risk of injury (ankle, knee, and/or groin training program) 3x/week for 10 weeks in separate training sessions in addition to regular team training during pre-season, and once per week for the rest of the season.
|
Control – HR: Patients with high risk of injury (in case of acute injury to ankle, knee, hamstring or groin in the previous 12 months, or a reduced function (average score <80%) on body part-specific function questionnaires. No specific training programs were prescribed in addition to regular team training.
Control – LR: Patients with low risk of injury (no acute injury in the past 12 months and normal function (average score >80%). No specific training programs were prescribed in addition to regular team training. |
Length of follow-up: 1 season
Loss-to-follow-up: None.
Incomplete outcome data: 1 team (3.1%) Intervention/ Control – HR: 13 (3.2%) Control – LR: 4 (3.2%) Reasons: the physiotherapist did not instruct the intervention group players nor record injuries.
|
Outcome measures and effect size (including 95%CI):
Injury incidence Defined as any physical complaint sustained by a player that resulted from a soccer match or training, resulting in inability to play (time-loss injury) (per 1000 hours exposure) IRR intervention to control – HR: 0.93 (95% CI 0.71 to 1.21) IRR: intervention to control – LR: 0.53 (95% CI 0.36 to 0.77)
Subanalysis: intervention to control – HR (95% CI): Hamstring IRR: 1.55 (0.83 to 2.90) Groin IRR: 1.18 (0.55 to 2.54)
Subanalysis acute Intervention: 41% Control – HR: 43% RR: 0.94 (95% CI 0.84 to 1.06) |
Authors’ conclusion: The introduction of individual specific preventive training programs did not affect the injury risk, most likely due to low compliance.
Remarks: No randomization procedure described. No baseline characteristics provided. No conflict of interest reported. Role of the commercial funding source unclear.
|
|
Fujisaki, 2022 [groin] |
Type of study: Cluster RCT
Setting and country: High schools, Japan
Funding and conflicts of interest: authors declare no conflicts of interest. Funding information not disclosed. |
Inclusion criteria: Soccer players (male) from 7 high schools in under-18 soccer league.
Exclusion criteria: Injury at inclusion preventing joining in club activities
N total at baseline: 202 (7 schools) CAE: 66 (3 schools) CAE + NHE: 73 (2 schools) Control: 63 (2 schools)
Important prognostic factors: age ± SD: CAE: 16.4 ± 0.9 CAE + NHE: 16.0 ± 0.7 Control: 16.1 ± 0.9
Weight ± SD CAE: 60.2 ± 7.1 CAE + NHE: 58.4 ± 7.2 Control: ± 0.9
Field position Attackers CAE 15% | +NHE 16% | C 17% Midfielders CAE 36% | +NHE 37% | C 37% Defenders CAE 39% | +NHE 32% | C 38% Goalkeepers CAE 9% | +NHE 15% | C 8%
Groups comparable at baseline? Yes |
CAE: Copenhagen adduction exercise, 1 set with 3 increasing to 15 repetitions, 1-3 times a week for 16 weeks as part of regular warm up.
CAE + NHE: CAE plus Nordic hamstring exercise; both exercises 1-3 times a week for 16 weeks as part of regular warm up. NHE 2 or 3 sets with 5 increasing to 10 repetitions.
|
No interventions other than continuing normal practice/ usual training.
|
Length of follow-up: 16 weeks
Loss-to-follow-up: CAE: 4 (6.1%) Reasons: low compliance (n = 1), injury (n = 1), left (n = 2)
CAE + NHE: 1 (1.4%) Reasons: injury (n = 1)
Control: 6 (9.5%) Reasons: injury (n = 3), left (n = 3)
Incomplete outcome data: See above.
|
Outcome measures and effect size (including 95%CI):
Injury incidence Defined as pain in the groin during sports activities, regardless of time loss or need for treatment (per 1000 competition hours) CAE: 0.64 | CAE + NHE: 0.25 C: 1.24 IRR CAE to C: 0.42 (95% CI 0.19 to 0.90) IRR CAE+NHE to C: 0.19 (0.07 to 0.54)
Groin injury severity: Defined as mean days lost to sports CAE: 5.5 ± 5.2 CAE +NHE: 10.3 ± 6.4 C: 14.4 ± 8.3 MD CEA to C: -8.9 (-12.0 to -5.8) MD CEA+NHE to C: -4.1 (-7.4 to -0.8)
|
Authors’ conclusion: Incorporating CAE in training sessions in high school soccer players reduced the incidence of groin pain and severity of injury according to time-lost to soccer. Addition of NHE might even be more effective.
|
|
Gabbe, 2006 [hamstring] |
Type of study: RCT
Setting and country: Football clubs, Australia
Funding and conflicts of interest: Non-commercial grants. Conflicts of interest described.
|
Inclusion criteria: Adult, male football players in either senior or reserve grade teams during the 2004 season.
Exclusion criteria: Injury at time of recruitment or study commencement
N total at baseline: 220 (7 clubs) Intervention: 114 Control: 106
Important prognostic factors: age (median, range): I: 23.4 (18 to 35) C: 23.9 (17.4 to 36)
Play experience (years ± SD) I: 11.8 ± 6.2| C: 12.4 ±4.9
Hamstring strain past 12mo I: 14% | C: 14%
Groups comparable at baseline? Yes, randomization stratified by past history of a hamstring strain. |
Eccentric exercise (similar to NHE, 12x 6 repetitions) before cool-down, 5 sessions over a 12-week period (3 during pre-season and 2 during first 6 weeks of season).
|
Stretching and range of movement exercises (3x 30 seconds) before cool-down, 5 sessions over a 12-week period (3 during pre-season and 2 during first 6 weeks of season).
|
Length of follow-up: 1 season.
Loss-to-follow-up: Not reported.
Incomplete outcome data: Poor compliance, yet no incomplete outcome data described.
|
Outcome measures and effect size (including 95%CI):
Injury incidence during season defined by physical assessment including: sudden onset posterior thigh pain; tenderness on palpation; with or without pain on stretch of the hamstring muscles; and with or without pain on contraction of the hamstring muscles. RR: 1.2 (95% 0.5 to 2.8)
|
Authors’ conclusion: A simple pre-season program might reduce the incidence of hamstring injuries; yet due to compliance issues, the program would have little widespread benefit to community-level Australian football.
Remarks:
|
|
Harøy, 2019 [groin] |
Type of study: Cluster RCT
Setting and country: Football teams, Norway
Funding and conflicts of interest: Several non-commercial and one commercial grant (not specified whether restricted). No conflict of interests. |
Inclusion criteria: Semiprofessional Norwegian male football players under contract with the team.
Exclusion criteria: Those not expected to train or play during the first 6-8 weeks of the season due to injury or illness.
N total at baseline: 652 (35 teams) Intervention: 339 (18 teams) Control: 313 (17 teams)
Important prognostic factors: age ± SD: I: 22.0 ± 4.3| C: 23.7 ± 4.3
Weight ± SD I: 75.7 ± 7.5| C: 78.0 ± 7.5
Prevalence of groin problems I: 32.8% | C: 32.6%
Field position Attackers I: 20% | C: 23% Midfielders I: 36% | C: 35% Defenders I: 31% | C: 30% Goalkeepers I: 13% | C: 11%
Groups comparable at baseline? Yes |
Adductor strengthening programme: one exercise (based on the Copenhagen adduction exercise) with three progression levels, performed 3x/week during the preseason during warm-up (6-8 weeks) and once per week during the competitive season (28 weeks), on both sides.
|
Training as normal.
|
Length of follow-up: 1 season (38 weeks)
Loss-to-follow-up: Intervention: 92 (27%) Reasons: insufficient weekly reports (<75% response rate)
Control: 71 (23%) Reasons: insufficient weekly reports (n = 51), withdrew from study (one team, n = 20)
Incomplete outcome data: See above. A per-protocol analysis was performed for 122 intervention players with sufficient compliance.
|
Outcome measures and effect size (including 95%CI):
Weekly prevalence of groin problems Registered using the OSTRC Overuse Injury Questionnaire OR: 0.59 (95% CI 0.40 to 0.86) |
Authors’ conclusion:
|
|
Hölmich, 2010 [groin] |
Type of study: Cluster RCT
Setting and country: Football clubs, Denmark
Funding and conflicts of interest: Not reported |
Inclusion criteria: Amateur football players training and playing at a competitive level.
Exclusion criteria: None reported.
N total at baseline: 1211 (55 clubs) Intervention: 39 clubs Control: 39 clubs
Important prognostic factors2: age (median): I: 24.5 | C: 24.6
Sex: not reported
Previous groin injury I: 38.4% | C: 47.2%
Field position Attackers I: 14.3% | C: 13.5% Midfielders I: 32.9% | C: 35.3% Defenders I: 25.2% | C: 23.7% Goalkeepers I: 8.8% | C: 7.4%
Groups comparable at baseline? Seemingly, yet only based on those with full datasets available (assumption MCAR not probable). Randomization stratified for level and geography. |
Exercise program with 6 exercises including strengthening (concentric and eccentric), coordination, core stability (for pelvis). Exercises formed an integrated part of the warmup before every regular football practice (2-4x/week). |
Training as usual.
|
Length of follow-up: 42 weeks (one season plus time off)
Loss-to-follow-up: Intervention: 17 clubs (43.5%) Control: 17 clubs (43.5%) Reasons: withdrew during study period.
Incomplete outcome data: See above. Eventually, 524 (intervention, 22 clubs) and 453 (control, 22 clubs) were included in the analysis.
|
Outcome measures and effect size (including 95%CI):
Time until first groin injury defined as any physical complaint that is the result of participating in football training or a football match incapacitating the player when playing football and/ or demanding special medical attention for the player to be able to participate or preventing him from participating in training or a match. HR: 0.80 (95% Ci 0.46 to 1.40)
|
Authors’ conclusion: The present cluster-randomized clinical trial ad- dressed a very common overuse injury using football players as the target group. The risk of sustaining a groin injury decreased, but this reduction was not significant.
Remarks: Authors report a 31% risk reduction, but it should be hazard (not risk). |
|
Petersen, 2011 [hamstring] |
Type of study: Cluster RCT
Setting and country: Soccer clubs, Denmark
Funding and conflicts of interest: No conflicts of interests. Funding information not disclosed. |
Inclusion criteria: Male soccer players in the top 5 Danish soccer divisions.
Exclusion criteria: (1) Use of eccentric hamstring exercises during recruitment, (2) players who joined a team after the start of the trial
N total at baseline: 942 (50 teams) Intervention: 461 (23 teams) Control: 481 (27 teams)
Important prognostic factors: age ± SD: I: 23.0 ± 4.0 C: 23.5 ± 4.0
Previous hamstring injury I: 10.6% | C: 11.2%
Field position Attackers I: 16.5% | C: 16.0% Midfielders I: 31.9% | C: 29.7% Defenders I: 29.1% | C: 28.9% Goalkeepers I: 8.2% | C: 8.5% Alternating I: 14.3% | C: 16.8%
Groups comparable at baseline? Yes, stratified according to playing level and geographical location. |
In addition to usual training program: 10-week progressive eccentric training program (Nordic Hamstring Exercise, 27 sessions) during the midseason break, followed by a weekly seasonal program (3 sets of 12-10-8 repetitions).
|
Usual training program.
|
Length of follow-up: 12 months
Loss-to-follow-up: Intervention: 36 (7.8%) Reasons: Discontinued intervention due to transfer or stop of career
Control: 44 (9.1%) Reasons: foreign transfer (n=1), discontinued due to transfer or stop of career (n = 43)
Incomplete outcome data: Intervention: 3 teams Control: 1 team Reasons: withdrew before start of study
|
Outcome measures and effect size (including 95%CI):
Occurrence of acute hamstring injury defined as any acute-occurring physical complaint in the region of the posterior thigh sustained during a soccer match or training, irrespective of the need for medical attention or time loss from soccer activities (adjusted for player seasons at risk) IRR (adjusted): 0.29 (0.15 to 0.57)
Injury severity Days of absence from soccer I: 30.3 days ± 18.3 C: 26.4 days ± 19.5 MD: 3.9 (95% CI 1.5 to 6.3) |
Authors’ conclusion: The training program is able to reduce the injury rate of new and recurrent injuries.
Remarks: Underpowered. |
|
Raya-Gonzalez, 2021 [hamstring] |
Type of study: RCT
Setting and country: Setting unclear, Spain
Funding and conflicts of interest: No conflicts of interest, no funding received. |
Inclusion criteria: Male soccer players <19 years of age
Exclusion criteria: (1) Players that participated in <80% of usual training sessions, (2) players with injury 2 months prior to the study, (3) goalkeepers
N total at baseline: 61 Intervention: 27 Control: 34
Important prognostic factors2: Not reported.
Groups comparable at baseline? Unclear, study only reports: “there were no baseline differences between-groups in any dependent variable.”
|
Regular weekly training program, complemented with Nordic Hamstring exercise and sprint training program once a week (15-20 minutes, for 14 weeks).
|
Regular weekly training program.
|
Length of follow-up: 14 weeks
Loss-to-follow-up: Intervention: 4 (14.8%) Reasons: <80% of training attendance
Control: 8 (23.5%) Reasons: injury (n = 3), <80% training attendance (n = 5)
Incomplete outcome data: See above.
|
Outcome measures and effect size (including 95%CI):
Injury incidence defined as an injury that occurred during a scheduled training session or match that caused absence from the next training session or match (per 1000 hours of exposure) I: 0.55 | C: 1.42 IRR: 0.39 (95% CI 0.28 to 0.54)
|
Authors’ conclusion: This study reported that the application of a training program based on NHE and sprint exercises is effective in improving sprint performance and reducing injury burden in U19 soccer players.
Remarks: Baseline characteristics mentioned in methods (should be results). Analysis of differences through SMD seems inappropriate. |
|
Silvers, 2015 |
Type of study: Cluster RCT
Setting and country: Universities, United States
Funding and conflicts of interest: Funding received from FIFA. Conflict of interest unclear. |
Inclusion criteria: Current student athletes (male) who were participating in an NCAA Division I or Division II member institution and who had not participated in an injury prevention program in the past 4 competitive seasons.
Exclusion criteria: None.
N total at baseline: 1525 (65 teams) Intervention: 775 (31 teams) Control: 850 (34 teams)
Important prognostic factors: Baseline characteristics not reported.
Groups comparable at baseline? Unclear. |
Information on DVD, an injury prevention manual and explanatory placards provided to perform the FIFA 11+ injury prevention program (ideally 3 times per week during 1 collegiate soccer season): A 20-minute program without additional equipment, consisting of 15 exercises divided into running exercises (8 minutes); strength, plyometrics and balance (10 minutes); and running exercises again (2 minutes)
|
No use of FIFA 11+ injury prevention program (not further described).
|
Length of follow-up: 4 months (August to December)
Loss-to-follow-up: Intervention: 100 (4 teams) Reasons: discontinuation of interventions due to time constraints
Control: 0
Incomplete outcome data: See above.
|
Outcome measures and effect size (including 95%CI):
Injury incidence defined as any physical complaint sustained by a player that resulted from a football match or football training, irrespective of the need for medical attention or time loss from football (per 1000 athlete exposure = participation in any team practice or game) I: 8.09 | C: 15.04 IRR: 0.53 (95% CI: 0.49 to 0.59)
Subanalysis: IRR (95% CI) Hamstring: 0.37 (0.21 to 0.63) Groin: 0.60 (0.37 to 0.98) Quadriceps: 0.72 (0.44 to 1.16)
Injury severity Mean days lost to injury I: 10.08 ± 14.68 C: 13.20 ± 26.6 MD: -3.12 (95% CI -5.19 to -1.05) |
Authors’ conclusion: The FIFA 11+ significantly reduced injury rates and decreased time loss to injury in the competitive male collegiate soccer player
Remarks: No supervision of adequate performance of the FIFA 11+ injury prevention program. |
|
Soligard, 2009 |
Type of study: Cluster RCT
Setting and country: Football clubs, Norway
Funding and conflicts of interest: Commercial (Norsk Tipping AS and FIFA Medical Assessment and Research Centre) and non-commercial funding. No conflicts of interest. |
Inclusion criteria: Female clubs from the 15-16 year divisions in the Norwegian Football Association that had at least 2 training sessions per week in addition to match play
Exclusion criteria: None.
N total at baseline: 2540 (125 clubs) Intervention: 1320 (65 clubs) Control: 1220 (60 clubs)
Important prognostic factors: Not reported.
Groups comparable at baseline? Cannot be judged.
|
Comprehensive warm-up programme (approx. 20 minutes) for every training session throughout the season, consisting of 3 parts (with instructional course + DVD + posters beforehand):
|
Warm up as usual during the season.
|
Length of follow-up: 8 months
Loss-to-follow-up: Not reported. Data on players who dropped out during the study period were included for the entire period of their participation.
Incomplete outcome data: Intervention: 265 (13 clubs, 20%) Reasons: did not start warm-up programme nor deliver any data on injury exposure
Control: 383 (19 clubs, 32%) Reasons: did not provide any data |
Outcome measures and effect size (including 95%CI):
Injury incidence to the lower extremity foot, ankle, lower leg, knee, thigh, groin and hip injuries (corrected for exposure time) IRR: 0.71 (95% CI 0.49 to 1.03)
Subanalysis: Acute injuries IRR: 0.74 (95% CI 0.51 to 1.08)
|
Authors’ conclusion: a structured warm- up programme in young female footballers can reduce risk of injury by about one third.
Remarks: Unclear whether groups were comparable at baseline. |
|
Van de Hoef, 2019 [hamstring] |
Type of study: Cluster RCT
Setting and country: Soccer clubs, the Netherlands
Funding and conflicts of interest: Funded by non-commercial grant distributor. No information disclosed on conflicts of interest. |
Inclusion criteria: Adult male soccer players in the first-class amateur league aged 18-45 years.
Exclusion criteria: Players who joined the team after the start of the season; player who were injured at the start participated from the moment they returned to play.
N total at baseline: 588 (32 teams) Intervention: 305 (16 teams) Control: 283 (16 teams)
Important prognostic factors: age ± SD: I: 23.8 ± 6.4 C:22.2 ± 3.1
Previous hamstring injury I: 21.8% | C: 26.9%
Field position Forwarder I: 24% | C: 21% Midfielders I: 32% | C: 35% Defenders I: 32% | C: 36% Goalkeepers I: 12% | C: 7%
Groups comparable at baseline? Yes |
Bounding Exercise Program: in addition to regular soccer training 12-week program with build-up from concentric to eccentric to plyometric exercises (approx. 3-5 minutes)
|
Usual soccer training
|
Length of follow-up: One season (39 weeks)
Loss-to-follow-up: Intervention: 76 (24.9%) Reasons: no baseline (n=53), no response weekly questions (n=15), severe injury (n=3), quit playing (n=5)
Control: 112 (39.6%) Reasons: no baseline (n=87), no response weekly questions (n=12), severe injury (n=4), quit playing (n=9)
Incomplete outcome data: average of around 50% of missing data points from the weekly self‐reports, for weekly match and training exposure |
Outcome measures and effect size (including 95%CI):
Hamstring injury incidence (per 1000 soccer hours) I: 1.12 | C: 1.39 IRR: 0.81 (95% CI: 0.62 to 1.04)
Hamstring injury severity: Defined as mean days absent from soccer play I: 33.0 days ± 42.7 C: 21.4 days ± 12.7 MD: 11.6 (95% CI 6.6 to 16.6) |
Authors’ conclusion: No evidence was found that a new functional injury prevention exercise pro- gram prevented hamstring injuries in adult male amateur soccer players.
Remarks:
|
|
Van der Horst, 2015 [hamstring] |
Type of study: Cluster RCT
Setting and country: Soccer teams, the Netherlands
Funding and conflicts of interest: Funded by non-commercial organisations. Conflict of interests not fully clearly reported. |
Inclusion criteria: Male soccer players in first-class amateur league (Eerste Klasse) aged 18 to 40 years.
Exclusion criteria: Players who joined a team after the start of the trial.
N total at baseline: (40 teams) Intervention: 292 (20 teams) Control: 287 (20 teams)
Important prognostic factors: age ± SD: I: 24.5 ± 3.6 C: 24.6 ± 4.1
Hamstring injury in previous year I: 24% | C: 20%
Field position Forwarder I: 28% | C: 27% Midfielders I: 35% | C: 36% Defenders I: 35% | C: 36% Goalkeepers I: 11% | C: 10%
Groups comparable at baseline? Yes |
Supervised sessions (total of 25) of Nordic Hamstring Exercise in 13 weeks, after the completion of the regular soccer training, before cooling down.
|
Play soccer as usual.
|
Length of follow-up: 1 year
Loss-to-follow-up: Intervention: 37 (2 teams, 11.2%) Reasons: discontinued intervention and registration
Control: 32 (2 teams, 10.0%) Reasons: loss to follow-up due to staff mutations)
Incomplete outcome data: In addition to above: Intervention: 2 teams Control: 2 teams Withdrew before start of study.
|
Outcome measures and effect size (including 95%CI):
Incidence of hamstring injuries ( Defined as any physical complaint affecting the posterior side of the upper leg irrespective of the need for medical attention or time loss from soccer activities Does not report for I and C separately I: 11 (3.8%) | C: 25 (8.7%) RR: 0.43 (95% CI 0.22 to 0.86)
Hamstring injury severity: Defined as mean days absent from soccer play I: 31 days ± 15 C: 28 days ± 19 MD: 3.0 (95% CI 0.21 to 5.79) |
Authors’ conclusion: Performing the NHE protocol in regular amateur soccer training results in a reduced risk of hamstring injury in male amateur soccer players. The NHE protocol did not reduce hamstring injury severity.
Remarks: Reference to protocol is wrong (NTR registration is correct though). |
|
Ali, 2022 [hamstring] |
Type of study: RCT
Setting and country: University, Pakistan
Funding and conflicts of interest: Not reported |
Inclusion criteria: Sprinters studying at Punjab university, aged 20 to 30 years.
Exclusion criteria: (1) known injury of hamstring muscle, lower limbs or spine, (2) cardiovascular disease, (3) smokers, (4) alcoholics
N total at baseline: 40 Intervention: 20 Control: 20
Important prognostic factors: age ± SD: I: 25.8 ± 1.8 C: 24.5 ± 2.2
Groups comparable at baseline? Insufficient information (gender distribution, confounders not reported) |
Warm-up exercises before sprinting events (3x/week for 3 months) (no protocol provided).
|
No warm-up exercises before sprinting events. (3x/week for 3 months)
|
Length of follow-up: 3 months
Loss-to-follow-up: None.
Incomplete outcome data: None. |
Outcome measures and effect size (including 95%CI):
Prevalence of hamstring injury Defined as pain, spasm or stiffness of hamstring muscle. I: 3 (15%) C: 9 (45%) RR: 0.33 (95% CI:0.11 to 1.05) |
Authors’ conclusion: Sprinters who did warm-up before sprinting events had less chances of hamstring injury than those who did not warm-up
Remarks: Very poor quality. Insufficient baseline characteristics, no sample size calculation, unclear statistical methods, no adjustment for confounders, no clear intervention. No information available on funding or competing interests. |
Abbreviations: CAE: Copenhagen Adduction Exercise, FIFA: Fédération Internationale de Football Association, HR: high-risk, LR: low-risk, MCAR: missing completely at random, NCAA: National Collegiate Athletic Association, NHE: Nordic Hamstring Exercise, RCT: randomized controlled trial, SD: standard deviation
Risk of bias table for intervention studies (randomized controlled trials; based on Cochrane risk of bias tool and suggestions by the CLARITY Group at McMaster University)
|
Study reference
|
Was the allocation sequence adequately generated?
|
Was the allocation adequately concealed?
|
Blinding:
|
Was loss to follow-up (missing outcome data) infrequent?
|
Are reports of the study free of selective outcome reporting?
|
Was the study apparently free of other problems that could put it at a risk of bias?
|
Overall risk of bias If applicable/necessary, per outcome measure
|
|
Engebretsen, 2008 |
Probably no
Reason: No information on the generation of the allocation sequence provided. |
Probably no
Reason: No information on the randomization process provided. |
Definitely no
Reason: Patients, physiotherapists (outcome assessors, data collectors and care providers) not blinded. Blinding of analysts not reported. |
Probably yes
Reason: Loss to follow-up not described, full intention-to-treat analysis. |
Probably yes
Reason: no protocol provided, yet all relevant outcomes were reported (including subanalyses) |
Definitely no
Reason: baseline characteristics not described, no information on conflict of interests reported by authors. |
HIGH
|
|
Fujisaki, 2022 |
Unclear
Reason: reported information: “Randomization using envelope method” |
Probably yes
Reason: sealed envelopes were opened by the principal investigator. |
Definitely no
Reason: Patients, outcome assessors, data collectors and care providers not blinded. Analysts were blinded. |
Probably yes
Reason: Loss to follow-up was infrequent (<10%) in intervention and control group. Intention-to-treat analysis performed. |
Probably yes
Reason: No protocol provided. Time loss first mentioned in results, yet follows naturally from analysis. |
No information |
Some concerns
|
|
Gabbe, 2006 |
Definitely yes
Reason: a computer-generated randomisation list for each club which included blocking in groups of four or six with the order of allocation varying within each block. |
Probably yes
Reason: Group allocation was performed by primary author, consequently reported to study personnel |
Definitely no
Reason: Patients, health care providers and outcome assessors not blinded. Blinding of analysts not reported. |
Unclear
Reason: Loss to follow-up was not reported. |
Probably yes
Reason: All relevant outcomes were reported, yet additional analysis of results for compliers. |
Probably no
Reason: Poor compliance to intervention, and active control group diluting results further. |
Some concerns
|
|
Harøy, 2019
|
Definitely yes
Reason: Statistician blinded to study protocol performed computer-generated block-randomization with block sizes of 4 and 6 in random order. |
Definitely yes
Reason: Principal investigator opened sealed envelope revealing group assignment. |
Definitely no
Reason: Patients (outcome assessors through self-assessment), health care providers were not blinded. Data collectors were blinded; analysts not reported. |
Probably no
Reason: Loss to follow-up was frequent (>20%) due to protocol excluding those with <75% response rate. Missing data were imputed by multiple imputation of those >75% response rate. |
Probably yes
Reason: All relevant outcomes (from prospectively registered protocol) were reported |
Probably yes
Reason: Possible recall bias due to retrospective registration of groin problems. No other problems noted |
Some concerns
|
|
Hölmich, 2010 |
Probably yes
Reason: Computer generated block randomization of block size two |
Definitely yes
Reason: Opaque, sealed envelopes were used and opened by physiotherapist and team coach. |
Probably no
Reason: Patients (outcome assessors through self-assessment), health care providers and data collectors were not blinded. Data analysts (data manager, statistician, authors) were blinded to allocation. |
Definitely no
Reason: Loss to follow-up was frequent in intervention and control group. No imputation methods were used (per protocol analysis). |
Probably yes
Reason: no protocol provided, yet all relevant outcomes were reported |
Definitely no
Reason: Funding information and conflict of interest not reported. |
High
|
|
Petersen, 2011 |
Probably yes
Reason: Envelopes with teams and envelopes with allocation randomly drawn and combined |
Definitely yes
Reason: Opaque, sealed envelopes were used and opened by an independent research assistant. |
Definitely no
Reason: Open trial with patients, health care providers and outcome assessors not blinded (blinding of data analysts not reported) |
Probably yes
Reason: Loss to follow-up was infrequent in intervention and control group. Results corrected for time at risk. |
Definitely no
Reason: registered secondary outcome measure (ACL-injury) not reported. Ultrasound not used for verification of injury. |
Probably yes
Reason: Limited generalizability to women and people of other age groups |
Some concerns
|
|
Raya-Gonzalez, 2021 |
Probably no
Reason: Study only reports that participants were allocated to either the intervention or control group. |
Probably no
Reason: No information on allocation concealment |
Probably no
Reason: no information on preventing participants obtaining knowledge of allocation. |
Definitely no
Reason: Loss to follow-up was frequent in both groups. No imputation methods were used. |
Probably yes
Reason: No protocol registered. All outcomes from methods mentioned in results. |
Probably no
Reason: Choice for use of SMD (Cohen’s d) unclear. Short follow-up time and limited generalizability. |
High
|
|
Silvers, 2015 |
Definitely yes
Reason: Utilizing a random number generator |
No information
Reason: Prevention of knowledge of allocation not described. |
Definitely no
Reason: Patients, health care providers, data collectors and outcome assessors not blinded (blinding of data analysts not reported) |
Probably no
Reason: Loss to follow-up was frequent in the intervention group (not in the control group). No imputation methods were used. |
Probably yes
Reason: No protocol registered. All outcomes from methods mentioned in results. |
Probably no
Reason: Conflict of interest information unclear. |
Some concerns
|
|
Soligard, 2009 |
Unclear
Reason: No information on randomization scheme provided |
Probably yes
Reason: The statistician who performed the randomization did not take part in the intervention. |
Probably no
Reason: No blinding of participants, coaches, outcome assessors. Data collectors were blinded; blinding of data analysts not reported. |
Definitely no
Reason: incomplete data was frequent in both groups. No imputation methods were used. |
Definitely yes
Reason: All relevant outcomes were reported (and defined in advance in the publicly available protocol) |
Definitely no
Reason: No baseline characteristics provided |
Some concerns
|
|
Van de Hoef, 2019 |
Probably yes
Reason: online randomizer was used. Unclear how equal numbers of assignment were guaranteed. |
Probably yes
Reason: Randomization performed independently. |
Probably no
Reason: Information on blinding not reported. Keeping in mind the type of intervention, blinding is unlikely. |
Definitely no
Reason: Loss to follow-up was frequent in both groups. Adequate imputation methods only used for exposure information |
Definitely yes
Reason: All relevant outcomes were reported conform publicly available protocol |
Probably yes
Reason: Protocol retrospectively registered; unclear original sample size calculation |
Some concerns:
|
|
Van der Horst, 2015 |
Definitely yes
Reason: Computer-generated random assignment of team numbers |
No information
Reason: Prevention of knowledge of allocation not described. |
Probably no
Reason: Information on blinding not reported. Keeping in mind the type of intervention, blinding is unlikely. |
Probably no
Reason: Loss to follow-up was reasonable in intervention and control group, yet no imputation methods were used. |
Probably no
Reason: Incidence per 1000 hours exposure not reported. Analysis of compliance not recorded in protocol |
Definitely no
Reason: Injury incidence was only calculated from players whose full training and match exposure during all 52 weeks of the study were registered. |
High
|
|
Ali, 2022 |
Probably yes
Reason: computer generated random number. |
No information
Reason: Prevention of knowledge of allocation not described. |
Probably no
Reason: Information on blinding not reported. |
Definitely yes
Reason: No loss to follow-up. |
Probably no
Reason: no protocol available. No description of intervention or control. Subjective outcome measures, without description of standardized measurement. |
Definitely no
Reason: Insufficient baseline characteristics, no sample size calculation, unclear statistical methods, no adjustment for confounders, no clear intervention. No information available on funding or competing interests. |
High |
Table of excluded studies
|
Reference |
Reason for exclusion |
|
Shadle IB, Cacolice PA. Eccentric Exercises Reduce Hamstring Strains in Elite Adult Male Soccer Players: A Critically Appraised Topic. J Sport Rehabil. 2017 Nov;26(6):573-577. doi: 10.1123/jsr.2015-0196. Epub 2016 Aug 24. PMID: 27632822. |
Wrong study type |
|
Al Attar WSA, Soomro N, Sinclair PJ, Pappas E, Sanders RH. Effect of Injury Prevention Programs that Include the Nordic Hamstring Exercise on Hamstring Injury Rates in Soccer Players: A Systematic Review and Meta-Analysis. Sports Med. 2017 May;47(5):907-916. doi: 10.1007/s40279-016-0638-2. PMID: 27752982. |
Wrong study type, unclear whether acute or overuse injury |
|
Biz C, Nicoletti P, Baldin G, Bragazzi NL, Crimì A, Ruggieri P. Hamstring Strain Injury (HSI) Prevention in Professional and Semi-Professional Football Teams: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Aug 4;18(16):8272. doi: 10.3390/ijerph18168272. PMID: 34444026; PMCID: PMC8394329. |
Wrong study type, unclear comparison |
|
Charlton PC, Drew MK, Mentiplay BF, Grimaldi A, Clark RA. Exercise Interventions for the Prevention and Treatment of Groin Pain and Injury in Athletes: A Critical and Systematic Review. Sports Med. 2017 Oct;47(10):2011-2026. doi: 10.1007/s40279-017-0742-y. PMID: 28497284. |
Wrong study type, no acute injury (chronic) |
|
Esteve E, Rathleff MS, Bagur-Calafat C, Urrútia G, Thorborg K. Prevention of groin injuries in sports: a systematic review with meta-analysis of randomised controlled trials. Br J Sports Med. 2015 Jun;49(12):785-91. doi: 10.1136/bjsports-2014-094162. Epub 2015 Feb 24. PMID: 25730819. |
Wrong study type, unclear whether acute or overuse injury |
|
Fanchini M, Steendahl IB, Impellizzeri FM, Pruna R, Dupont G, Coutts AJ, Meyer T, McCall A. Exercise-Based Strategies to Prevent Muscle Injury in Elite Footballers: A Systematic Review and Best Evidence Synthesis. Sports Med. 2020 Sep;50(9):1653-1666. doi: 10.1007/s40279-020-01282-z. PMID: 32185630. |
Wrong study type, unclear whether acute or overuse injury |
|
Goldman EF, Jones DE. Interventions for preventing hamstring injuries. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD006782. doi: 10.1002/14651858.CD006782.pub2. PMID: 20091605. |
Wrong study type |
|
Rosado-Portillo A, Chamorro-Moriana G, Gonzalez-Medina G, Perez-Cabezas V. Acute Hamstring Injury Prevention Programs in Eleven-a-Side Football Players Based on Physical Exercises: Systematic Review. J Clin Med. 2021 May 9;10(9):2029. doi: 10.3390/jcm10092029. PMID: 34065138; PMCID: PMC8125962. |
Wrong study type |
|
Rudisill SS, Varady NH, Kucharik MP, Eberlin CT, Martin SD. Evidence-Based Hamstring Injury Prevention and Risk Factor Management: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2022 Apr 6:3635465221083998. doi: 10.1177/03635465221083998. Epub ahead of print. PMID: 35384731. |
Wrong study type, unclear whether acute or overuse injury |
|
Vatovec R, Kozinc Z, Šarabon N. Exercise interventions to prevent hamstring injuries in athletes: A systematic review and meta-analysis. European Journal of Sport Science. 2020;20(7):992-1004. doi:10.1080/17461391.2019.1689300 |
Wrong study type |
|
Almeida MO, Maher CG, Saragiotto BT. Prevention programmes including Nordic exercises to prevent hamstring injuries in football players (PEDro synthesis). Br J Sports Med. 2018 Jul;52(13):877-878. doi: 10.1136/bjsports-2017-098862. Epub 2018 Mar 7. PMID: 29514817. |
Wrong study type |
|
Lutter C, Jacquet C, Verhagen E. Does prevention pay off? Economic aspects of sports injury prevention: a systematic review. British Journal of Sports Medicine 2022;56:470-476. |
Wrong outcome |
|
Andrew N, Gabbe BJ, Cook J, Lloyd DG, Donnelly CJ, Nash C, Finch CF. Could targeted exercise programmes prevent lower limb injury in community Australian football? Sports Med. 2013 Aug;43(8):751-63. doi: 10.1007/s40279-013-0056-7. PMID: 23681448. |
Wrong study type, unclear whether acute or overuse injury |
|
Chavarro-Nieto C, Beaven M, Gill N, Hébert-Losier K. Hamstrings injury incidence, risk factors, and prevention in Rugby Union players: a systematic review. Phys Sportsmed. 2023 Feb;51(1):1-19. doi: 10.1080/00913847.2021.1992601. Epub 2021 Oct 19. PMID: 34637371. |
Wrong study type |
|
Cornelissen M, Kemler E, Verhagen E, Gouttebarge V. A systematic review of injuries in recreational field hockey: From injury problem to prevention. J Sports Sci. 2020 Sep;38(17):1953-1974. doi: 10.1080/02640414.2020.1764898. Epub 2020 Jul 23. PMID: 32698730. |
Wrong study type, wrong outcome |
|
Crossley KM, Patterson BE, Culvenor AG. Making football safer for women: a systematic review and meta-analysis of injury prevention programmes in 11 773 female football (soccer) players. British Journal of Sports Medicine 2020;54:1089-1098. |
Wrong study type |
|
Goode AP, Reiman MP, Harris L, DeLisa L, Kauffman A, Beltramo D, Poole C, Ledbetter L, Taylor AB. Eccentric training for prevention of hamstring injuries may depend on intervention compliance: a systematic review and meta-analysis. Br J Sports Med. 2015 Mar;49(6):349-56. doi: 10.1136/bjsports-2014-093466. Epub 2014 Sep 16. PMID: 25227125. |
Wrong study type |
|
Impellizzeri FM, McCall A, van Smeden M. Why methods matter in a meta-analysis: a reappraisal showed inconclusive injury preventive effect of Nordic hamstring exercise. J Clin Epidemiol. 2021 Dec; 140:111-124.doi: 10.1016/j.jclinepi.2021.09.007 |
Wrong study type |
|
Kilic O, Kemler E, Gouttebarge V. The "sequence of prevention" for musculoskeletal injuries among adult recreational footballers: A systematic review of the scientific literature. Phys Ther Sport. 2018 Jul;32:308-322. doi: 10.1016/j.ptsp.2018.01.007. Epub 2018 Feb 2. PMID: 29655857. |
Wrong study type |
|
Okobi OE, Evbayekha EO, Ilechie E, Iroro J, Nwafor JN, Gandu Z, Shittu HO. A Meta-Analysis of Randomized Controlled Trials on the Effectiveness of Exercise Intervention in Preventing Sports Injuries. Cureus. 2022 Jun 20;14(6):e26123. doi: 10.7759/cureus.26123. PMID: 35875288; PMCID: PMC9298606. |
Wrong study type, wrong outcome data |
|
Porter T, Rushton A. The efficacy of exercise in preventing injury in adult male football: a systematic review of randomised controlled trials. Sports Med Open. 2015 Dec;1(1):4. doi: 10.1186/s40798-014-0004-6. Epub 2015 Jan 20. PMID: 27747841; PMCID: PMC4532702. |
Wrong study type |
|
Krist MR, van Beijsterveldt AM, Backx FJ, de Wit GA. Preventive exercises reduced injury-related costs among adult male amateur soccer players: a cluster-randomised trial. J Physiother. 2013 Mar;59(1):15-23. doi: 10.1016/S1836-9553(13)70142-5. PMID: 23419911. |
Wrong study type, wrong outcome |
|
Longo UG, Loppini M, Berton A, Marinozzi A, Maffulli N, Denaro V. The FIFA 11+ program is effective in preventing injuries in elite male basketball players: a cluster randomized controlled trial. Am J Sports Med. 2012 May;40(5):996-1005. doi: 10.1177/0363546512438761. Epub 2012 Mar 13. PMID: 22415208. |
Wrong study type, unclear whether acute or overuse injury, wrong outcome data |
|
Slauterbeck JR, Choquette R, Tourville TW, Krug M, Mandelbaum BR, Vacek P, Beynnon BD. Implementation of the FIFA 11+ Injury Prevention Program by High School Athletic Teams Did Not Reduce Lower Extremity Injuries: A Cluster Randomized Controlled Trial. Am J Sports Med. 2019 Oct;47(12):2844-2852. doi: 10.1177/0363546519873270. Epub 2019 Sep 17. PMID: 31526276. |
Wrong study type, unclear whether acute or overuse injury, wrong outcome data |
|
Toresdahl BG, McElheny K, Metzl J, Ammerman B, Chang B, Kinderknecht J. A Randomized Study of a Strength Training Program to Prevent Injuries in Runners of the New York City Marathon. Sports Health. 2020 Jan/Feb;12(1):74-79. doi: 10.1177/1941738119877180. Epub 2019 Oct 23. PMID: 31642726; PMCID: PMC6931177. |
Wrong study type, unclear whether acute or overuse injury, wrong outcome data |
|
van Beijsterveldt AM, van de Port IG, Krist MR, Schmikli SL, Stubbe JH, Frederiks JE, Backx FJ. Effectiveness of an injury prevention programme for adult male amateur soccer players: a cluster-randomised controlled trial. Br J Sports Med. 2012 Dec;46(16):1114-8. doi: 10.1136/bjsports-2012-091277. Epub 2012 Aug 9. PMID: 22878257; PMCID: PMC3596860. |
Wrong study type, unclear whether acute or overuse injury, wrong outcome data |
|
Hölmich P, Nyvold P, Larsen K. Continued significant effect of physical training as treatment for overuse injury: 8- to 12-year outcome of a randomized clinical trial. Am J Sports Med. 2011 Nov;39(11):2447-51. doi: 10.1177/0363546511416075. Epub 2011 Aug 3. PMID: 21813441. |
Wrong outcome (no acute injuries) |
|
Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008 Feb;18(1):40-8. doi: 10.1111/j.1600-0838.2006.00634.x. Epub 2007 Mar 12. PMID: 17355322. |
Wrong study design (no RCT) |
Verantwoording
Beoordelingsdatum en geldigheid
Laatst beoordeeld : 12-06-2024
Algemene gegevens
De ontwikkeling/herziening van deze richtlijnmodule werd ondersteund door het Kennisinstituut van de Federatie Medisch Specialisten (www.demedischspecialist.nl/kennisinstituut) en werd gefinancierd uit de Kwaliteitsgelden Medisch Specialisten (SKMS). Patiëntenparticipatie bij deze richtlijn werd medegefinancierd uit de Kwaliteitsgelden Patiënten Consumenten (SKPC) binnen het programma KIDZ.
De financier heeft geen enkele invloed gehad op de inhoud van de richtlijnmodule.
Samenstelling werkgroep
Voor het ontwikkelen van de richtlijnmodule is in 2022 een multidisciplinaire werkgroep ingesteld, bestaande uit vertegenwoordigers van alle relevante specialismen (zie hiervoor de Samenstelling van de werkgroep) die betrokken zijn bij de zorg voor patiënten met acute spierblessures van de onderste ledematen.
Werkgroep
- dr. G. (Guus) Reurink (voorzitter), sportarts, VSG
- drs. H.E. (Nadine) Bruineberg, AIOS spoedeisende geneeskunde, NVSHA
- drs. P. (Petra) Groenenboom, sportarts, VSG
- dr. N. (Nick) van der Horst, sportfysiotherapeut, KNGF
- prof. dr. G.M.M.J. (Gino) Kerkhoffs, hoogleraar/orthopedisch chirurg, NOV
- drs. A.D. (Anne) van der Made, AIOS orthopedie, NOV
- drs. M.E.F. (Mariëlle) Olsthoorn, radioloog, NVvR
- dr. K.W. (Kostan) Reisinger, traumachirurg, NVvH
- dr. I.J.R. (Igor) Tak, sportfysiotherapeut, KNGF
- drs. A. (Adam) Weir, sportarts, VSG
- dr. M. (Marinus) Winters, sportfysiotherapeut, KNGF
- T. (Thomas) Jonkergouw, junior adviseur patiëntbelang, PFNL (t/m april 2023)
- M. (Maike) Broere, adviseur patiëntbelang, PFNL (vanaf april 2023)
Meelezer:
- Drs. R.J.E. (Rob) Riksen, revalidatiearts, VRA
Klankbordgroep patiënten:
- L. (Luxman) Logathasan
- B. (Bart) Deprez
- E. (Eline) van Oord – Jansen Venneboer
- W. (Wim) van Tongeren
Met ondersteuning van
- dr. C.T.J. (Charlotte) Michels, adviseur, Kennisinstituut van Medisch Specialisten
- drs. F. (Florien) Ham, adviseur, Kennisinstituut van Medisch Specialisten
Belangenverklaringen
De Code ter voorkoming van oneigenlijke beïnvloeding door belangenverstrengeling is gevolgd. Alle werkgroepleden hebben schriftelijk verklaard of zij in de laatste drie jaar directe financiële belangen (betrekking bij een commercieel bedrijf, persoonlijke financiële belangen, onderzoeksfinanciering) of indirecte belangen (persoonlijke relaties, reputatiemanagement) hebben gehad. Gedurende de ontwikkeling of herziening van een module worden wijzigingen in belangen aan de voorzitter doorgegeven. De belangenverklaring wordt opnieuw bevestigd tijdens de commentaarfase.
Een overzicht van de belangen van werkgroepleden en het oordeel over het omgaan met eventuele belangen vindt u in onderstaande tabel. De ondertekende belangenverklaringen zijn op te vragen bij het secretariaat van het Kennisinstituut van de Federatie Medisch Specialisten.
|
Lid |
Functie |
Nevenfuncties |
Gemelde belangen |
Ondernomen actie |
|
Werkgroep |
||||
|
dr. G. (Guus) Reurink (vz.) |
Sportarts (medisch specialist) |
*Lid werkgroep richtlijnen van de Vereniging voor Sportgeneeskunde (VSG) (onbetaald) |
* Betrokken bij wetenschappelijk onderzoek naar blessurepreventie in judo, gefinancierd door ZonMw. * Betrokken bij wetenschappelijk onderzoek naar Plaatjes-Rijk-Plasma injecties bij enkel arthrose, gefinancierd door Reuma fonds Nederland. * Betrokken bij wetenschappelijk onderzoek naar effect van preventieve hamstringoefeningen op hamstrings spier karakteristieken verkregen met DTI MRI, National Basketball Association grant gefinancierd door GE Healthcare. * Positieve bijdrage aan mijn reputatie als sportarts en (wetenschappelijk) expert op het gebied van acute spierblessures bij sporters. |
Geen restricties. |
|
drs. H.E. (Nadine) Bruineberg |
* Militair AIOS Spoedeisende geneeskunde, * Opleidingsregio NWN - OLVG |
Geen. |
Geen. |
Geen restricties. |
|
drs. P. (Petra) Groenenboom |
Sportarts, Ziekenhuis Gelderse Vallei, Ede |
TeamNL Papendal (vanuit Gelderse Vallei) |
Geen.
|
Geen restricties. |
|
dr. N. (Nick) van der Horst |
Sportfysiotherapeut PSV Eindhoven 1 |
*SoccerDoc scholingsinstituut CEO (geaccrediteerde scholing voor fysiotherapeuten; cursus over hamstringblessures met werkgroepleden). |
Geen.
|
Geen restricties. |
|
prof. dr. G.M.M.J. (Gino) Kerkhoffs |
Hoogleraar en afdelingshoofd Orthopedische chirurgie Amsterdam UMC |
* Consultant fa. Arthrex (www.arthrex.nl) (betaald wereldwijd bedrijf in medische apparatuur en leider in de ontwikkeling van nieuwe producten en het medisch onderwijs in de orthopedie. Gino is betaald consultant, in het kader van onderwijs en onderzoek). |
* Geen, behoudens het algemene gezondheidsbelang van preventieve maatregelen ter voorkoming van acute spierletsels en revalidatie van opgelopen spierletsels. * Aantal projecten, zie o.a. onderstaand: Rol als PI bij contractonderzoeken, deze onderzoeken zijn ook gericht op de enkel en artroscopie. Geen externe subsidies. * Opinieleider op het gebied van acute spierblessures. |
Geen restricties. |
|
drs. A.D. (Anne) van der Made |
Amsterdam UMC - AIOS Orthopedie |
Amsterdam UMC – Onderzoeker (onbetaald) |
* PhD-traject wordt betaald vanuit een PhD-beurs van het Amsterdam UMC.
|
Geen restricties. |
|
drs. M.E.F. (Mariëlle) Olsthoorn |
Radioloog, Erasmus MC, Rotterdam |
Geen. |
Geen. |
Geen restricties. |
|
dr. K.W. (Kostan) Reisinger |
Chirurg, Zuyderland MC, Heerlen |
Dienstverband bij Zuyderland, wij voeren dergelijke operaties uit. |
Geen.
|
Geen restricties. |
|
dr. I.J.R. (Igor) Tak |
Sportfysiotherapeut en mede-eigenaar |
* Post-doc onderzoeker Amsterdam * Lid congrescommissie Sportmedisch * Docent (para-)medisch Beroepsonderwijs (betaald en onbetaald) |
Geen.
|
Geen restricties. |
|
dr. A. (Adam) Weir |
* Sportarts - Afdeling orthopedie en sportgeneeskunde, ErasmusMC, Rotterdam (0.4fte) |
* Lid congrescommissie Sportmedisch Wetenschappelijk Jaarcongres VSG (onbetaald) * Spreker op congressen (veelal onbetaald soms wel tegen een vergoeding). |
Geen.
|
Geen restricties. |
|
dr. M. (Marinus) Winters |
Sportfysio- en manueel therapeut en eigenaar Onder de Knie Sportfysiotherapie en Manuele Therapie, Haarlem |
* Spreker op congressen (veelal onbetaald/tegen een minimale vergoeding). |
* Eigenaar 'Onder de Knie' een gespecialiseerde sportfysiotherapie praktijk voor mensen met klachten in het onderbeen. Dit betreft een net opgestarte praktijk in Haarlem. De richtlijn zouden mij een financieel voordeel kunnen opleveren als er meer dan al gangbaar is bij acute spierblessures - wordt geadviseerd een gespecialiseerde sportfysiotherapeut te raadplegen. * Anders dan bovengenoemde belang, heb ik geen betaald adviseurschap, of andere financiële belangen. * Er zijn geen familie, partner, vrienden en naaste collega's die opereren in dit specifieke aandachtsgebied in de gezondheidszorg. * Als sportfysiotherapeut, incidenteel spreker en onderzoeker zou het meewerken aan de richtlijn mijn reputatie op het gebied blessures in de onderste extremiteiten kunnen versterken. |
Geen restricties. |
|
T. (Thomas) Jonkergouw |
Adviseur Patiëntbelang Patiëntenfederatie Nederland |
*Thoracale letsels na trauma |
Geen. |
Geen restricties. |
|
M. (Maike) Broere |
Adviseur patiëntenbelang - Patiëntenfederatie Nederland |
Geen. |
Geen. |
Geen restricties. |
|
Meelezer |
||||
|
R.J.E. (Rob) Riksen |
Deelname als afgevaardigde van VRA, lid van werkgroep Bewegen en Sport. |
Geen. |
Geen. |
Geen restricties. |
|
Klankbordgroep patiënten |
||||
|
L. (Luxman) Logathasan |
N.v.t. |
Onbetaald, ervaringen delen als sporter/cricket |
Vrienden die ook sporten |
Geen restricties. |
|
B. (Bart) Deprez |
Finance Manager Eveon Containers - 100% |
(ex) voetballer (betaald) |
Geen. |
Geen restricties. |
|
E. (Eline) van Oord – Jansen Venneboer |
Communicatieadviseur bij Stichting Taal aan Zee in Den Haag. |
Lid College van Bestuur van Nieuwe of Littéraire Sociëteit De Witte (onbetaald). |
Geen. |
Geen restricties. |
|
W. (Wim) van Tongeren |
*Fysiotherapeut OREC |
Geen. |
Geen. |
Geen restricties. |
Inbreng patiëntenperspectief
Er werd aandacht besteed aan het patiëntenperspectief middels het instellen van een patiënten-klankbordgroep, in samenwerking met de Nederlandse Patiëntenfederatie . Vier patienten zijn hiervoor uitgenodigd binnen hetnetwerk van de werkgroep. Er zijn vier bijeenkomsten georganiseerd met de patiënten klankbordgroep gedurende de richtlijnontwikkeling. Hierbij is specifiek vanuit patiënten perspectief input gevraagd bij de keuze en prioritering van uitkomstmaten, het formuleren van waarden en voorkeuren voor patiënten per module, het implementatieplan per module en de ontwikkeling van patiënten informatie op https://www.thuisarts.nl/. Resultaten van deze bijeenkomsten (zie aanverwante producten: Verslagen klankbordgroep bijeenkomsten) zijn besproken in de werkgroep. De verkregen input is meegenomen bij de keuze voor de uitkomstmaten, het opstellen van de overwegingen (zie kop Waarden en voorkeuren van patiënten en verzorgers) en het schrijven van de module over preventie. De conceptrichtlijn is tevens voor commentaar voorgelegd aan de deelnemers van de klankbordgroep en de eventueel aangeleverde commentaren zijn bekeken en verwerkt.
Kwalitatieve raming van mogelijke financiële gevolgen in het kader van de Wkkgz
Bij de richtlijn is conform de Wet kwaliteit, klachten en geschillen zorg (Wkkgz) een kwalitatieve raming uitgevoerd of de aanbevelingen mogelijk leiden tot substantiële financiële gevolgen. Bij het uitvoeren van deze beoordeling zijn richtlijnmodules op verschillende domeinen getoetst (zie het stroomschema op de Richtlijnendatabase).
Uit de kwalitatieve raming blijkt dat er waarschijnlijk geen substantiële financiële gevolgen zijn, zie onderstaande tabel.
|
Module |
Uitkomst raming |
Toelichting |
|
Preventie |
Geen financiële gevolgen |
Hoewel uit de toetsing volgt dat de aanbeveling(en) breed toepasbaar zijn, volgt uit de toetsing dat [het overgrote deel (±90%) van de zorgaanbieders en zorgverleners al aan de norm voldoet of het geen nieuwe manier van zorgverlening of andere organisatie van zorgverlening betreft, het geen toename in het aantal in te zetten voltijdsequivalenten aan zorgverleners betreft en het geen wijziging in het opleidingsniveau van zorgpersoneel betreft. Er worden daarom geen substantiele financiële gevolgen verwacht wegens deze modules. |
Werkwijze
AGREE
Deze richtlijnmodule is opgesteld conform de eisen vermeld in het rapport Medisch Specialistische Richtlijnen 2.0 van de adviescommissie Richtlijnen van de Raad Kwaliteit. Dit rapport is gebaseerd op het AGREE II instrument (Appraisal of Guidelines for Research & Evaluation II; Brouwers, 2010).
Knelpuntenanalyse en uitgangsvragen
Tijdens de voorbereidende fase inventariseerde de werkgroep de knelpunten in de zorg voor patiënten met acute spierblessures van de onderste ledematen. Tevens zijn er knelpunten aangedragen door Ergotherapie Nederland, Inspectie Gezondheidszorg en Jeugd, Nederlandse Vereniging van Ziekenhuizen, Patiëntenfederatie Nederland, Revalidatie Nederland, Verpleegkundigen & Verzorgenden Nederland, Nederlandse Vereniging van Revalidatieartsen, Vereniging van Oefentherapeuten Cesar en Mensendieck, Zorginstituut Nederland, Zelfstandige Klinieken Nederland en Zorgverzekeraars Nederland via een schriftelijke knelpuntenanalyse. Op basis van de uitkomsten van de schriftelijke knelpuntenanalyse zijn door de werkgroep concept-uitgangsvragen opgesteld en definitief vastgesteld.
Uitkomstmaten
Na het opstellen van de zoekvraag behorende bij de uitgangsvraag inventariseerde de werkgroep welke uitkomstmaten voor de patiënt relevant zijn, waarbij zowel naar gewenste als ongewenste effecten werd gekeken. Hierbij werd een maximum van acht uitkomstmaten gehanteerd. De werkgroep waardeerde deze uitkomstmaten volgens hun relatieve belang bij de besluitvorming rondom aanbevelingen, als cruciaal (kritiek voor de besluitvorming), belangrijk (maar niet cruciaal) en onbelangrijk. Tevens definieerde de werkgroep tenminste voor de cruciale uitkomstmaten welke verschillen zij klinisch (patiënt) relevant vonden.
Methode literatuursamenvatting
Een uitgebreide beschrijving van de strategie voor zoeken en selecteren van literatuur is te vinden onder ‘Zoeken en selecteren’ onder Onderbouwing. Indien mogelijk werd de data uit verschillende studies gepoold in een random-effects model. Review Manager 5.4 werd gebruikt voor de statistische analyses. De beoordeling van de kracht van het wetenschappelijke bewijs wordt hieronder toegelicht.
Beoordelen van de kracht van het wetenschappelijke bewijs
De kracht van het wetenschappelijke bewijs werd bepaald volgens de GRADE-methode. GRADE staat voor ‘Grading Recommendations Assessment, Development and Evaluation’ (zie http://www.gradeworkinggroup.org/). De basisprincipes van de GRADE-methodiek zijn: het benoemen en prioriteren van de klinisch (patiënt) relevante uitkomstmaten, een systematische review per uitkomstmaat, en een beoordeling van de bewijskracht per uitkomstmaat op basis van de acht GRADE-domeinen (domeinen voor downgraden: risk of bias, inconsistentie, indirectheid, imprecisie, en publicatiebias; domeinen voor upgraden: dosis-effect relatie, groot effect, en residuele plausibele confounding).
GRADE onderscheidt vier gradaties voor de kwaliteit van het wetenschappelijk bewijs: hoog, redelijk, laag en zeer laag. Deze gradaties verwijzen naar de mate van zekerheid die er bestaat over de literatuurconclusie, in het bijzonder de mate van zekerheid dat de literatuurconclusie de aanbeveling adequaat ondersteunt (Schünemann, 2013; Hultcrantz, 2017).
|
GRADE |
Definitie |
|
Hoog |
|
|
Redelijk |
|
|
Laag |
|
|
Zeer laag |
|
Bij het beoordelen (graderen) van de kracht van het wetenschappelijk bewijs in richtlijnen volgens de GRADE-methodiek spelen grenzen voor klinische besluitvorming een belangrijke rol (Hultcrantz, 2017). Dit zijn de grenzen die bij overschrijding aanleiding zouden geven tot een aanpassing van de aanbeveling. Om de grenzen voor klinische besluitvorming te bepalen moeten alle relevante uitkomstmaten en overwegingen worden meegewogen. De grenzen voor klinische besluitvorming zijn daarmee niet één op één vergelijkbaar met het minimaal klinisch relevant verschil (Minimal Clinically Important Difference, MCID). Met name in situaties waarin een interventie geen belangrijke nadelen heeft en de kosten relatief laag zijn, kan de grens voor klinische besluitvorming met betrekking tot de effectiviteit van de interventie bij een lagere waarde (dichter bij het nuleffect) liggen dan de MCID (Hultcrantz, 2017).
Overwegingen (van bewijs naar aanbeveling)
Om te komen tot een aanbeveling zijn naast (de kwaliteit van) het wetenschappelijke bewijs ook andere aspecten belangrijk en worden meegewogen, zoals aanvullende argumenten uit bijvoorbeeld de biomechanica of fysiologie, waarden en voorkeuren van patiënten, kosten (middelenbeslag), aanvaardbaarheid, haalbaarheid en implementatie. Deze aspecten zijn systematisch vermeld en beoordeeld (gewogen) onder het kopje ‘Overwegingen’ en kunnen (mede) gebaseerd zijn op expert opinion. Hierbij is gebruik gemaakt van een gestructureerd format gebaseerd op het evidence-to-decision framework van de internationale GRADE Working Group (Alonso-Coello, 2016a; Alonso-Coello 2016b). Dit evidence-to-decision framework is een integraal onderdeel van de GRADE methodiek.
Formuleren van aanbevelingen
De aanbevelingen geven antwoord op de uitgangsvraag en zijn gebaseerd op het beschikbare wetenschappelijke bewijs en de belangrijkste overwegingen, en een weging van de gunstige en ongunstige effecten van de relevante interventies. De kracht van het wetenschappelijk bewijs en het gewicht dat door de werkgroep wordt toegekend aan de overwegingen, bepalen samen de sterkte van de aanbeveling. Conform de GRADE-methodiek sluit een lage bewijskracht van conclusies in de systematische literatuuranalyse een sterke aanbeveling niet a priori uit, en zijn bij een hoge bewijskracht ook zwakke aanbevelingen mogelijk (Agoritsas, 2017; Neumann, 2016). De sterkte van de aanbeveling wordt altijd bepaald door weging van alle relevante argumenten tezamen. De werkgroep heeft bij elke aanbeveling opgenomen hoe zij tot de richting en sterkte van de aanbeveling zijn gekomen.
In de GRADE-methodiek wordt onderscheid gemaakt tussen sterke en zwakke (of conditionele) aanbevelingen. De sterkte van een aanbeveling verwijst naar de mate van zekerheid dat de voordelen van de interventie opwegen tegen de nadelen (of vice versa), gezien over het hele spectrum van patiënten waarvoor de aanbeveling is bedoeld. De sterkte van een aanbeveling heeft duidelijke implicaties voor patiënten, behandelaars en beleidsmakers (zie onderstaande tabel). Een aanbeveling is geen dictaat, zelfs een sterke aanbeveling gebaseerd op bewijs van hoge kwaliteit (GRADE gradering HOOG) zal niet altijd van toepassing zijn, onder alle mogelijke omstandigheden en voor elke individuele patiënt.
|
Implicaties van sterke en zwakke aanbevelingen voor verschillende richtlijngebruikers |
||
|
|
Sterke aanbeveling |
Zwakke (conditionele) aanbeveling |
|
Voor patiënten |
De meeste patiënten zouden de aanbevolen interventie of aanpak kiezen en slechts een klein aantal niet. |
Een aanzienlijk deel van de patiënten zouden de aanbevolen interventie of aanpak kiezen, maar veel patiënten ook niet. |
|
Voor behandelaars |
De meeste patiënten zouden de aanbevolen interventie of aanpak moeten ontvangen. |
Er zijn meerdere geschikte interventies of aanpakken. De patiënt moet worden ondersteund bij de keuze voor de interventie of aanpak die het beste aansluit bij zijn of haar waarden en voorkeuren. |
|
Voor beleidsmakers |
De aanbevolen interventie of aanpak kan worden gezien als standaardbeleid. |
Beleidsbepaling vereist uitvoerige discussie met betrokkenheid van veel stakeholders. Er is een grotere kans op lokale beleidsverschillen. |
Organisatie van zorg
In de knelpuntenanalyse en bij de ontwikkeling van de richtlijnmodule is expliciet aandacht geweest voor de organisatie van zorg: alle aspecten die randvoorwaardelijk zijn voor het verlenen van zorg (zoals coördinatie, communicatie, (financiële) middelen, mankracht en infrastructuur). Randvoorwaarden die relevant zijn voor het beantwoorden van deze specifieke uitgangsvraag zijn genoemd bij de overwegingen. Meer algemene, overkoepelende, of bijkomende aspecten van de organisatie van zorg worden behandeld in de module Organisatie van zorg.
Commentaar- en autorisatiefase
De conceptrichtlijnmodule werd aan de betrokken (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd ter commentaar. De commentaren werden verzameld en besproken met de werkgroep. Naar aanleiding van de commentaren werd de conceptrichtlijnmodule aangepast en definitief vastgesteld door de werkgroep. De definitieve richtlijn werd aan de deelnemende (wetenschappelijke) verenigingen en (patiënt) organisaties voorgelegd voor autorisatie en door hen geautoriseerd dan wel geaccordeerd.
Literatuur
Agoritsas T, Merglen A, Heen AF, Kristiansen A, Neumann I, Brito JP, Brignardello-Petersen R, Alexander PE, Rind DM, Vandvik PO, Guyatt GH. UpToDate adherence to GRADE criteria for strong recommendations: an analytical survey. BMJ Open. 2017 Nov 16;7(11):e018593. doi: 10.1136/bmjopen-2017-018593. PubMed PMID: 29150475; PubMed Central PMCID: PMC5701989.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016 Jun 28;353:i2016. doi: 10.1136/bmj.i2016. PubMed PMID: 27353417.
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ; GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ. 2016 Jun 30;353:i2089. doi: 10.1136/bmj.i2089. PubMed PMID: 27365494.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010 Dec 14;182(18):E839-42. doi: 10.1503/cmaj.090449. Epub 2010 Jul 5. Review. PubMed PMID: 20603348; PubMed Central PMCID: PMC3001530.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017 Jul;87:4-13. doi: 10.1016/j.jclinepi.2017.05.006. Epub 2017 May 18. PubMed PMID: 28529184; PubMed Central PMCID: PMC6542664.
Medisch Specialistische Richtlijnen 2.0 (2012). Adviescommissie Richtlijnen van de Raad Kwalitieit. http://richtlijnendatabase.nl/over_deze_site/over_richtlijnontwikkeling.html
Neumann I, Santesso N, Akl EA, Rind DM, Vandvik PO, Alonso-Coello P, Agoritsas T, Mustafa RA, Alexander PE, Schünemann H, Guyatt GH. A guide for health professionals to interpret and use recommendations in guidelines developed with the GRADE approach. J Clin Epidemiol. 2016 Apr;72:45-55. doi: 10.1016/j.jclinepi.2015.11.017. Epub 2016 Jan 6. Review. PubMed PMID: 26772609.
Schünemann H, Brożek J, Guyatt G, et al. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. Available from http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
Zoekverantwoording
Zoekacties zijn opvraagbaar. Neem hiervoor contact op met de Richtlijnendatabase.